Abstract
Despite the increased use of nursing homes by minority residents, nursing home care remains highly segregated. Compared to whites, racial/ethnic minorities tend to be cared for in facilities with limited clinical and financial resources, low nurse staffing levels, and a relatively high number of care deficiency citations. We assessed the trends from 2006 to 2011 in those citations and in disparities across facilities with four different concentrations of racial/ethnic minority residents. We found that the number of health care–related deficiencies and the percentage of facilities with serious deficiencies decreased over time for all four facility groups. From 2006 to 2011, the average annual number of health care–related deficiencies declined from 7.4 to 6.8 for facilities with low minority concentrations (< 5 percent) and from 10.6 to 9.4 for facilities with high minority concentrations (≥ 35 percent). In multivariable analyses, across-site disparities in health care-related deficiencies and in life-safety deficiencies narrowed over time. We also found that increasing the Medicaid payment rate might help improve both overall quality and disparities, but state case-mix payment approaches might worsen both. These results suggest the need to reevaluate quality improvement and cost containment efforts to better foster quality and equity of nursing home care.
Racial and ethnic disparities in quality of care have long been documented in nursing homes.[1–6] Approximately 1.3 million older and disabled Americans receive nursing home care in 15,000 facilities.[6] In the past two decades, the racial/ethnic composition of nursing home residents has changed continuously, with declining numbers of non-Hispanic white residents and dramatically increasing numbers of minority residents (such as African Americans, Hispanics, and Asian Americans).[6] In 2012 nearly 20 percent of the nursing home population nationally were members of racial/ethnic minority groups (authors' calculation, based on the Minimum Data Set).
Despite the increased use of nursing homes by minority residents, nursing home care remains highly segregated.[1–3] Compared to whites, racial/ethnic minorities tend to be cared for in facilities with limited clinical and financial resources, low nurse staffing, and high care deficiencies.[1–3] Thus, widespread racial/ethnic disparities in quality are largely due to differences across sites instead of differences in care provided to residents within the same facility.[1–5]
Over the past several decades, the quality of care in both minority-concentrated and majority-concentrated nursing homes may have improved, at least partially as a result of such quality-improvement efforts as strengthened state oversights after the Omnibus Budget Reconciliation Act of 1987[7] and increased market competition.[8] Despite the industrywide trend of improvements, recent literature suggests little or no improvements of disparities across sites over time in terms of several quality indicators,[4,5] such as family-reported experiences with care.
State Medicaid programs are the dominant payer of long-term nursing home care, paying for roughly half of its total expenditures.[9,10] States have considerable discretion in setting Medicaid payment rates and methods.[10–13]
Vincent Mor and colleagues[10] reported that state Medicaid payment rates ranged from $91 to $189 per diem in 2004. From 1998 to 2004 the number of states adopting case-mix adjusted payment, or payment adjusted for estimated resource utilization of resident groups, increased from twenty-six to thirty-five, and the average inflation-adjusted state Medicaid per diem rate increased from $109 to $131. The increased payment rate appeared to be associated with improved quality and resident outcomes in nursing homes.[10–13]
This study was intended to provide an updated assessment of the longitudinal trend in nursing home quality and site-of-care disparities from 2006 to 2011. Instead of focusing on individual quality indicators, we assessed government-issued deficiency citations, which cover a comprehensive list of federal standards in clinical and personal care.[7] Given the indisputable role of state Medicaid reimbursement policies in determining nursing home care, we also examined the associations of Medicaid payment rate and use of case-mix payment with site-of-care disparities in deficiencies. Our aim was to inform state policy makers of potential levers with which to improve both the global quality and the equity of nursing home care.
Study Data And Methods
Data and Sample
We linked the 2005–11 Online Survey Certification and Reporting (OSCAR) System files to the 2005–10 LTCFocus databases that are publicly available from Brown University.[14], OSCAR, a facility-level database, is updated annually by the Centers for Medicare and Medicaid Services (CMS).[15] OSCAR contains rich information about nursing home organizational characteristics and deficiency citation measures, which have been widely used for quality evaluations and policy analyses.[1–6] The LTCFocus databases were created by the Center for Gerontology and Healthcare Research at Brown University using multiple data sources, including the Minimum Data Set, Medicare insurance files, OSCAR, and results of state policy surveys.
Our sample included all freestanding nursing homes in the United States, except for the roughly 8 percent of the facilities that are affiliated with hospitals. We excluded those homes because their patterns of care and patient mix are different from those of the majority of other facilities. We also excluded a small number of facilities (less than 5 percent of the total) with missing information about concentrations of minority residents.
Our analytic sample included 85,941 facility-years (14,000–14,600 facilities annually) and their deficiency measures for 2006–11 and other characteristics lagged by one year (2005–10). We included lagged independent variables to temper concerns about potential endogeneity.[10]
Deficiency Citations
All US nursing homes certified by Medicare, Medicaid, or both are inspected annually for compliance with a set of approximately 180 federal quality standards. These standards encompass all aspects of care, including clinical and personal care, patient safety, quality of life, patient rights, physical environment, and administration.[7]
Under contracts with CMS, states perform on-site surveys every nine to fifteen months using trained surveyors whose tasks include examining facility operations, reviewing medical records, and interviewing residents and staff. State surveyors issue deficiency citations (coded as 1 for a deficiency and 0 for no deficiency) if they determine that service standards for a particular domain are not met. Therefore, the number of deficiencies a facility receives each year represents an external evaluation of its existing quality problems. Depending on the severity and scope of identified deficiencies, facilities may face intermediate sanctions, such as civil monetary penalties, or even termination of Medicare or Medicaid reimbursement.[7]
In this study, we analyzed three deficiency measures publicly reported on the Nursing Home Compare website.[16] They were the number of deficiencies directly related to clinical or personal care processes and outcomes of patients (health care–related deficiencies), the number of deficiencies related to life and fire safety issues of the facility (life-safety deficiencies), and whether or not the nursing home had received any deficiency at G-level or higher (i.e. deficiency causing immediate jeopardy or actual harm to resident) as a measure of the severity of identified care problems.
Independent Variables
The key independent variable was the percentage of racial/ethnic minority residents (African Americans, Hispanics, Asians or Pacific Islanders, and American Indians or Alaskan Natives) in a nursing home on the first Thursday in April of each year in 2005–10. This information was obtained from the LTCFocus databases, using the race and ethnicity information in the Minimum Data Set and Medicare enrollment databases.
After preliminary analyses of the associations of facility racial/ethnic composition with deficiency measures, we categorized facilities into the following site-of-care groups:[4] facilities with low concentrations of minority residents (less than 5 percent), medium concentrations (5–14.9 percent), medium-high concentrations (15–34.9 percent), and high concentrations (35 percent or more). We examined alternative cutoff points in sensitivity analyses; the results were similar and thus are not presented here.
We obtained the following covariates for 2005–10 from OSCAR that, according to previous studies,[1–6,10,11] may be associated with nursing home quality: number of beds (or bed size); affiliation with a chain (yes or no); ownership type (for-profit, nonprofit, or government-owned); occupancy rate; percentages of residents insured by Medicare, insured by Medicaid, and with behavioral symptoms; and staffing levels (hours per resident per day) for registered nurses, licensed practical nurses, and certified nursing assistants.
We obtained additional facility covariates for 2005–10 from the LTCFocus files that included percentage of female residents, average age of residents, and a facility-level case-mix index derived from the resource utilization group III classification based on Minimum Data Set assessments.[17] The case-mix index was calculated as the average of the resource utilization group III scores of all residents in the facility, with a higher value indicating higher average complexity of resident population.
We also defined a market competition measure based on the Herfindahl-Hirschman Index, calculated using nursing home beds available in the county annually. Finally, using the LTCFocus databases, we defined variables for state Medicaid average per diem payment rate and whether or not the state used a case-mix payment system each year during 2005–09 (2010 data were not available). All payment rates were inflation adjusted to 2009 dollars.
Statistical Analyses
In bivariate analyses separately performed for each year, we compared deficiency measures, nursing home covariates, and market competition across the four site-of-care groups. Comparisons were based on analyses of variance for continuous variables and on chi-square tests for categorical variables.
In analyses of the trend of disparities in health care–related and life-safety deficiencies during 2006–11, we estimated separate multivariable Poisson regressions that modeled the number of deficiencies as a function of site-of-care dummies (omitting sites with low minority concentration), year dummies (omitting 2006), site-year interactions, facility covariates, market competition, and state dummies.
We used facility random effects to control for repeated observations of facilities and potential overdispersion of the count data (that is, the deficiency numbers).[18] We did not estimate models with fixed effects because of our focus on across-site, instead of within-site, disparities and because our key independent variable—site-of-care groups—was essentially time invariant. We similarly estimated a random-effects logistic regression for whether or not each nursing home received any citation at levels G–L.
To explore the potential role of Medicaid payment policies implemented during the period 2005–09 in addressing site-of-care disparities in 2006–10, we first performed a state-level analysis for each year to illustrate state variations in site-of-care disparities. We further estimated longitudinal random-effects Poisson regressions (for numbers of deficiencies) and logistic regressions (for any G–L level deficiencies), with the unit of the analyses being the facility-year. In each regression, the deficiency measure was modeled as a function of site-of-care groups, year dummies, site-year interactions, Medicaid per diem rate and its interactions with site groups, state use of the case-mix payment method and its interactions with site groups, facility covariates, market completion, and state dummies.
Limitations
The study had several limitations. First, we examined deficiency citations as quality indicators but did not analyze other Minimum Data Set–based indicators that might directly measure resident outcomes, such as the development of high-stage pressure ulcers. Future research is needed to study other indicators.
Second, our state policy analyses focused on Medicaid's payment rate and state use of the case-mix reimbursement method, given their critical role in driving the delivery of nursing home care. Other state variables, such as the stringency of regulations of nursing home quality, might have confounded the associations between state payment policies and deficiencies. However, the use of state dummies should largely control for such confounding.
Finally, many variables in the OSCAR data are self-reported by nursing homes, which might bias our results. Nonetheless, we do not believe that such bias would change the major conclusions of our study.
Study Results
Of the freestanding nursing homes in our study in 2010, 5,925 (43 percent) had low minority concentrations, 3,027 (22 percent) had medium concentrations, 2,547 (18 percent) had medium-high concentrations, and 2,363 (17 percent) had high concentrations (online Appendix Exhibit A1).[19] The average shares of minority residents ranged from less than 2 percent in facilities with low concentrations to more than 50 percent in facilities with high concentrations. Compared to nursing homes with lower minority concentrations, those with higher concentrations tended to be larger, for-profit, and located in more competitive markets. They also tended to have more Medicaid-funded residents and less appropriate nurse staffing patterns. These differences were similar in other years in the study period.
The average number of health care–related deficiencies fell during the study period for all groups of nursing homes (Exhibit 1), as did the rate of having any G–L level deficiencies (Appendix Exhibit A2).[19] The average number of health care–related deficiencies declined from 7.4 in 2006 to 6.8 in 2011 for facilities with low minority concentrations and from 10.6 to 9.4 for facilities with high minority concentrations (p < 0.001 for trends; Exhibit 2). Similarly, the percentage of facilities that had any G–L level deficiencies declined from 26.9 percent in 2006 to 20.2 percent in 2011 for facilities with low minority concentrations and from 27.6 percent to 19.4 percent for the group with high concentrations (p < 0.001 for trends; Appendix Exhibit A2).[19]
EXHIBIT 1.
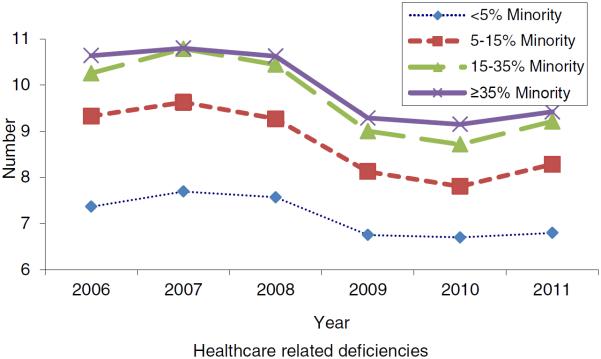
Caption: Trend In The Average Number Of Health Care–Related Deficiencies In Freestanding Nursing Homes By Concentration Of Racial/Ethnic Minority Residents, 2006–11
Source/Notes: SOURCE Authors' analysis of data for 2006–11 from the Online Survey Certification and Reporting (OSCAR) files and the LTCFocus files.
Exhibit 2.
Average Number Of Health Care–Related Deficiencies By Nursing Home Concentration Of Racial/Ethnic Minority Residents, 2006 And 2011
| Concentration | 2006 | 2011 | Change in adjusted disparityb | ||||
|---|---|---|---|---|---|---|---|
| Number | Unadjusted disparity | Adjusted disparitya | Number | Unadjusted disparity | Adjusted disparitya | ||
| Low (<5%) | 7.37 | — c | — c | 6.80 | -- | — c | — c |
| Medium (5–14.9%) | 9.33 | 1.96 | 0.57**** | 8.28 | 1.48 | 0.35**** | −0.22** |
| Medium-high (15–34.9%) | 10.26 | 2.89 | 0.74**** | 9.21 | 2.41 | 0.05**** | −0.69**** |
| High (≥35%) | 10.64 | 3.27 | 1.04**** | 9.42 | 2.62 | 0.18**** | −0.86**** |
SOURCE Authors' analysis of data for 2006–11 from the Online Survey Certification and Reporting (OSCAR) files and the LTCFocus files.
Calculated as Def multiplied by (IRR – 1), where Def is the mean number of health care related deficiencies for nursing homes with low concentrations of minority residents in the year, and IRR is the adjusted incidence rate ratio of each other concentration group estimated from a multivariable random-effects Poisson regression that modeled deficiency number as a function of minority concentration groups, year dummies, the interactions of minority concentration groups and year dummies, bed size, chain affiliation, nonprofit ownership, government ownership, occupancy rate, percentage of Medicare residents, percentage of Medicaid residents, case-mix, percentage of residents with behavioral symptoms, percentage of female residents, average age of residents, staffing levels for registered nurses, staffing levels for licensed practical nurses, staffing levels for certified nursing assistants, market completion, and state dummies.
Adjusted disparity of 2011 minus adjusted disparity of 2006.
The reference group.
p < 0.05
p < 0.001
In contrast, the average number of life-safety deficiencies increased slightly over time for all groups of facilities (Appendix Exhibit A2).[19] The averages rose from 2.8 in 2006 to 3.4 in 2011 for facilities with low minority concentrations and from 3.5 to 4.1 for the group with high concentrations.
Across-site disparities in both health care–related and life-safety deficiencies narrowed but did not disappear from 2006 to 2011. Multivariable Poisson analyses suggested that for health care–related deficiencies, adjusted disparities between facilities with high and low minority concentrations were 1.04 deficiencies in 2006 and 0.18 deficiency in 2011 (p < 0.001 in both cases; Exhibit 2). The analyses also show reduced adjusted disparities over time by 0.86 deficiency (i.e. from 1.04 in 2006 to 0.18 in 2011; p < 0.001). Similarly, the adjusted disparities in life-safety deficiencies between the two groups were 0.37 in 2006 and 0.19 in 2011 (p < 0.001 in both cases), showing reduced adjusted disparities by 0.18 deficiency (i.e. from 0.37 in 2006 to 0.19 in 2011; p < 0.01; Appendix Exhibit A3).[19]
In unadjusted analyses, no significant site-of-care disparities were found for the rate of facilities that had any G–L level deficiencies. However, adjusted analyses found that significant across-site disparities might exist for this measure (Appendix Exhibit A3).[19]
The unadjusted disparities in 2010 health care–related deficiencies between facilities with high versus low minority concentrations varied substantially across states (Exhibit 3). Similar variations were found for life-safety deficiencies and severity of deficiencies (Appendix Exhibit A4).[19]
EXHIBIT 3.

Caption: Difference In Average Number Of Health Care–Related Deficiencies Between Nursing Homes With High Concentrations Of Racial/Ethnic Minority Residents And Those With Low Concentrations By State
Source/Notes: SOURCE Authors' analysis of data for 2010 from the Online Survey Certification and Reporting (OSCAR) file and the LTCFocus file. NOTES States were not included if in 2010 they had fewer than five nursing homes in the group with low (< 5 percent) minority concentrations (HI and NM) or fewer than five nursing homes in the group with high (≥ 35 percent) minority concentrations (AK, IA, ID, ME, MN, MT, ND, NE, NH, NV, OR, RI, SD, UT, VT, WV, and WY). The District of Columbia was also excluded because in 2010 it had fewer than five nursing homes in the high-concentration group.
Multivariable analyses found that increasing the Medicaid per diem payment rate by $10 was associated with small but significant reductions in health care–related deficiencies (adjusted incidence rate ratio 0.987; Exhibit 4). However, increasing the payment rate was not associated with reductions in life-safety deficiencies or with changes in the rate of having any G–L level deficiencies (Appendix Exhibit A5).[19] Increased per diem payment rates might also be associated with slightly but significantly reduced disparities in health care–related deficiencies and rate of having any G–L level deficiencies.
Exhibit 4.
Effects Of Medicaid Payment Rates And Case-Mix Payment On Nursing Home Health Care–Related Deficiencies And Racial/Ethnic Disparities
| Medicaid payment | Adjusted IRRa | Effect on deficiencies (main effects) | |
|---|---|---|---|
| Effectb | p | ||
| Payment rate (in $10) | 0.987 | −0.11 | 0.005 |
| Case-mix payment | 1.383 | 3.27 | 0.000 |
| Effect on disparities (effects of interaction) | |||
|---|---|---|---|
| Nursing home concentration of minorities | Adjusted IRRa | Effectb | p |
| Payment rate (in $10) interacted with: | |||
| Low (<5%) | — c | — c | — c |
| Medium (5–14.9%) | 1.001 | 0.01 | 0.731 |
| Medium-high (15–34.9%) | 0.998 | −0.01 | 0.469 |
| High (≥35%) | 0.984 | −0.11 | 0.000 |
| Case-mix payment interacted with: | |||
| Low (<5%) | — c | — c | — c |
| Medium (5–14.9%) | 0.990 | −0.07 | 0.455 |
| Medium-high (15–34.9%) | 1.048 | 0.34 | 0.009 |
| High (≥35%) | 1.072 | 0.51 | 0.002 |
SOURCE Authors' analysis of data for 2006–10 from the Online Survey Certification and Reporting (OSCAR) files and the LTCFocus files.
Multivariable longitudinal (2006–10) random-effects Poisson regression modeled deficiencies as a function of minority concentration groups, year dummies, the interactions of minority concentration groups and year dummies, Medicaid payment rate and its interactions with minority groups, case-mix payment method and its interactions with minority groups, bed size, chain affiliation, nonprofit ownership, government ownership, occupancy rate, percentage of Medicare residents, percentage of Medicaid residents, case-mix, percentage of residents with behavioral symptoms, percentage of female residents, average age of residents, staffing levels for registered nurses, staffing levels for licensed practical nurses, staffing levels for certified nursing assistants, market completion, and state dummies.
Calculated as Def multiplied by (IRR – 1), where Def is the mean number of health care related deficiencies of all nursing homes in the sample (for main effects) or of nursing homes with low concentrations of minority residents (for effects of interaction) and IRR is the adjusted incidence rate ratio estimated from the Poisson regression for the corresponding main effects or effects of interaction.
The reference group.
In contrast, a state's use of the case-mix payment system was associated with an increase in the number of health care–related deficiencies (adjusted IRR: 1.383; Exhibit 4), increased likelihood of having any G–L level deficiencies (Appendix Exhibit A5),[19] and slightly but significantly increased site-of-care disparities in both health care–related and life-safety deficiencies.
Discussion
We found that during 2006–11 the average number of health care–related deficiencies and the severity of deficiencies (measured by having any G–L level deficiencies) decreased for freestanding nursing homes in all groups of racial/ethnic minority concentrations. Meanwhile, disparities in health care–related deficiencies between facilities with higher and lower minority concentrations narrowed but did not disappear over time. The average number of life-safety deficiencies increased slightly, but across-facility disparities in these deficiencies narrowed.
Moreover, disparities in all deficiency measures varied substantially across states. Increased Medicaid nursing home per diem payment rates were associated with overall decreases in the number of health care–related deficiencies and slight reductions in across-site disparities. State use of the case-mix payment system was associated with increased health care–related deficiencies and slightly increased site-of-care disparities. These findings are clinically relevant, given the critical implications of care deficiencies for resident outcomes and experiences with care.[3–5]
The poor quality of nursing home care has been a concern for several decades, with deficits found in numerous clinical and personal care areas such as the prevention of high-stage pressure ulcers[4] and management of chronic pain.[10] In the context of continued care problems at nursing homes, previous studies also indicated that nursing home care in certain areas might have improved, possibly due to stronger government enforcement after the 1987 Omnibus Budget Reconciliation Act,[7] market-based quality improvement efforts such as public reporting,[8] and increased Medicaid payment,[10] among other factors. Nevertheless, a series of U.S. Government Accountability Office reports[20–22] throughout the past decade and more recent studies[23,24] expressed continuing concerns about the serious care problems in nursing homes and about the fact that state surveyors tend to underidentify nursing home violations of minimum care standards and underrate serious violations.
This study updated the literature with more recent data that showed decreases in the number and severity of health care–related deficiencies, but slight increases for the number of life-safety deficiencies over time. These trends suggest that nursing homes may have improved performance in various clinical and nursing areas but have paid less attention to potential life-safety issues (for instance, inadequate maintenance or testing of sprinkler systems). It is also possible that the reduced number and severity of health care–related deficiencies indicate gradually weakened state oversight and enforcement, with state surveyors becoming more lenient in issuing and rating citations. However, strong evidence does not exist to support either of the possible explanations. Further investigation is necessary to determine which factors (changes in regulatory inspections, actual changes in quality, or both) underlie these trends.
Despite the divergent trends in health care–related and life-safety deficiencies, this study further found that site-of-care disparities in deficiencies narrowed over time. Nursing homes may have tried to improve their performance in care in response to the above-mentioned regulatory, market-oriented, and financial drivers of quality. However, concerns exist that these efforts may not lead to equally improved care for all subgroups of residents or in all nursing facilities.[4,5] In other words, these broadly targeted efforts may help stimulate overall quality improvement, but it is uncertain whether and how they may help reduce disparities in performance.[25]
To our knowledge, national initiatives targeting racial/ethnic or site-of-care disparities in nursing homes do not exist. Thus, our findings of narrowed disparities in deficiencies may suggest that, in aggregate and over time, these global quality improvement efforts helped reduce disparities as well. It is also possible that narrowed disparities were due to state inspectors' underreporting and underrating of deficiencies for minority-concentrated facilities relative to other facilities. As noted above, however, there is no firm evidence to support this possibility.
In an attempt to better understand the impact of individual quality approaches on racial/ethnic disparities, this study took the first step to focus on Medicaid payment policies. This was a logical first step because of the dominating role of Medicaid payment policies in determining the levels of nursing home financial resources and because of their readily available data. Our findings that overall reduced health care–related deficiencies were associated with higher payment rates confirmed the positive impact of Medicaid payment on nursing home quality that has been reported in the literature.[10–13] The associations of higher payment rate with reduced site-of-care disparities in the number and severity of health care–related deficiencies, although small in magnitude, may suggest that increased generosity on Medicaid's part would be of higher benefit to minority-concentrated facilities, given that these facilities also have relatively higher concentrations of Medicaid residents. Thus, that increased generosity would not only have an impact on all nursing homes, but it would also help reduce disparities across sites.
Our estimated associations of state use of the case-mix payment system with increased number and severity of health care–related deficiencies are also largely consistent with previous findings.[10–13] Previous studies reported either no association between use of case-mix payment and specific quality indicators or worse resident outcomes and reduced nurse staffing after a state's shift to case-mix payment. This study further revealed small but significant associations of the use of case-mix payment with increased site-of-care disparities in both health care–related and life-safety deficiencies. These and previous findings together raise important concerns about the unintended consequences of case-mix reimbursement on both overall quality and equity of nursing home care.
The results of our study have important policy implications. The recent trend of reduced disparities in deficiency citations are encouraging. Nonetheless, it is imperative that future efforts develop a better evidence base to help clarify the ways in which major quality initiatives affect the equity of nursing home care. We found that although increasing the Medicaid payment rate might help improve both overall quality and disparities, state case-mix payment approaches might worsen both. These results provide a rationale for possible reconsiderations of existing Medicaid—and, more broadly, non-Medicaid—quality improvement and cost containment efforts to better foster the quality and equity of nursing home care.
Conclusion
Several previous studies found persistent racial/ethnic disparities in individual nursing home quality indicators.[4,5] In contrast, our study—which used more recent data, for the period 2006–11—suggested narrowed site-of-care disparities in health care–related and life-safety deficiency citations over time. Further research is necessary to determine how Medicaid and non-Medicaid policies might affect the care in nursing homes with high concentrations of minority residents versus other nursing homes so that best policies can be developed to achieve the dual goal of high quality and equity of care.
Acknowledgments
This study was funded by the National Institute on Minority Health and Health Disparities (NIMHD; Grant No. R01MD007662). The views expressed in this article are those of the authors and do not necessarily represent the views of the NIMHD.
Notes
- 1.Smith DB, Feng Z, Fennell ML, Zinn J, Mor V. Racial disparities in access to long-term care: the illusive pursuit of equity. J Health Polit Policy Law. 2008;33(5):861–81. doi: 10.1215/03616878-2008-022. [DOI] [PubMed] [Google Scholar]
- 2.Fennell ML, Feng Z, Clark MA, Mor V. Elderly Hispanics more likely to reside in poor-quality nursing homes. Health Aff (Millwood) 2010;29(1):65–73. doi: 10.1377/hlthaff.2009.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82(2):227–56. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Y, Yin J, Cai X, Temkin-Greener J, Mukamel DB. Association of race and sites of care with pressure ulcers in high-risk nursing home residents. JAMA. 2011;306(2):179–86. doi: 10.1001/jama.2011.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Y, Ye Z, Glance LG, Temkin-Greener H. Trends in family ratings of experience with care and racial disparities among Maryland nursing homes. Med Care. 2014;52(7):641–8. doi: 10.1097/MLR.0000000000000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feng Z, Fennell ML, Tyler DA, Clark M, Mor V. Growth of racial and ethnic minorities in US nursing homes driven by demographics and possible disparities in options. Health Aff (Millwood) 2011;30(7):1358–65. doi: 10.1377/hlthaff.2011.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harrington C, Carrillo H. The regulation and enforcement of federal nursing home standards, 1991–1997. Med Care Res Rev. 1999;56(4):471–94. doi: 10.1177/107755879905600405. [DOI] [PubMed] [Google Scholar]
- 8.Mukamel DB, Weimer DL, Mushlin AI. Interpreting market share changes as evidence for effectiveness of quality report cards. Med Care. 2007;45(12):1227–32. doi: 10.1097/MLR.0b013e31812f56bb. [DOI] [PubMed] [Google Scholar]
- 9.Ng T, Harrington C, Musumeci M, Reaves EL. Medicaid home and community-based services programs: 2010 data update [Internet] Kaiser Commission on Medicaid and the Uninsured; Washington (DC): Dec 22, 2014. [cited 2015 May 7]. Available from: http://kff.org/medicaid/report/medicaid-home-and-community-based-services-programs-2011-data-update/ [Google Scholar]
- 10.Mor V, Gruneir A, Feng Z, Grabowski DC, Intrator O, Zinn J. The effect of state policies on nursing home resident outcomes. J Am Geriatr Soc. 2011;59(1):3–9. doi: 10.1111/j.1532-5415.2010.03230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harrington C, Swan JH, Carrillo H. Nurse staffing levels and Medicaid reimbursement rates in nursing facilities. Health Serv Res. 2007;42(3 Pt 1):1105–29. doi: 10.1111/j.1475-6773.2006.00641.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grabowski DC, Angelelli JJ, Mor V. Medicaid payment and risk-adjusted nursing home quality measures. Health Aff (Millwood) 2004;23(5):243–52. doi: 10.1377/hlthaff.23.5.243. [DOI] [PubMed] [Google Scholar]
- 13.Feng Z, Grabowski DC, Intrator O, Zinn J, Mor V. Medicaid payment rates, case-mix reimbursement, and nursing home staffing—1996–2004. Med Care. 2008;46(1):33–40. doi: 10.1097/MLR.0b013e3181484197. [DOI] [PubMed] [Google Scholar]
- 14.LTCfocus . Create custom reports on long-term care [Internet] Brown School of Public Health; Providence (RI): [cited 2015 May 7]. Available from: http://ltcfocus.org/ [Google Scholar]
- 15. CMS.gov . Provider of Services current files [Internet] Centers for Medicare and Medicaid Services; Baltimore (MD): CMS.gov [last modified 2015 Apr 29; cited 2015 May 7]. Available from: http://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Provider-of-Services/ [Google Scholar]
- 16. Medicare.gov . Nursing Home Compare [Internet] Centers for Medicare and Medicaid Services; Baltimore (MD): Medicare.gov [cited 2015 May 7]. Available from: http://www.medicare.gov/nursinghomecompare/search.html. [Google Scholar]
- 17.Fries BE, Schneider DP, Foley WJ, Gavazzi M, Burke R, Cornelius E. Refining a case-mix measure for nursing homes: Resource Utilization Groups (RUG-III) Med Care. 1994;32(7):668–85. doi: 10.1097/00005650-199407000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Greene WH. Econometric analysis, 5th version. Prentice Hall; Upper Saddle River (NJ): 2002. [Google Scholar]
- 19.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 20.General Accountability Office . Nursing home quality: prevalence of serious problems, while declining, reinforces importance of enhanced oversight [Internet] GAO; Washington (DC): Jul, 2003. [cited 2015 May 7]. (Report No. GAO-03-561). Available from: http://www.gao.gov/assets/240/238941.pdf. [Google Scholar]
- 21.Government Accountability Office . Nursing homes: efforts to strengthen federal enforcement have not deterred some homes from repeatedly harming residents [Internet] GAO; Washington (DC): Mar, 2007. [cited 2015 May 7]. (Report No. GAO-07-241). Available from: http://www.gao.gov/assets/260/258016.pdf. [Google Scholar]
- 22.Government Accountability Office . Nursing homes: CMS's special focus facility methodology should better target the most poorly performing homes, which tended to be chain affiliated and for-profit [Internet] GAO; Washington (DC): Aug, 2009. [cited 2015 May 7]. (Report No. GAO-09-689). Available from: http://www.gao.gov/new.items/d09689.pdf. [Google Scholar]
- 23.Harrington C, Stockton J, Hooper S. The effects of regulation and litigation on a large for-profit nursing home chain. J Health Polit Policy Law. 2014;39(4):781–809. doi: 10.1215/03616878-2743039. [DOI] [PubMed] [Google Scholar]
- 24.Department of Health and Human Services Office of Inspector General . Adverse events in skilled nursing facilities: national incidence among Medicare beneficiaries [Internet] HHS; Washington (DC): Feb, 2014. [cited 2015 May 8]. (Report No. OEI-06-11-00370). Available from: http://oig.hhs.gov/oei/reports/oei-06-11-00370.pdf. [Google Scholar]
- 25.Weinick RM, Hasnain-Wynia R. Quality improvement efforts under health reform: how to ensure that they help reduce disparities—not increase them. Health Aff (Millwood) 2011;30(10):1837–43. doi: 10.1377/hlthaff.2011.0617. [DOI] [PubMed] [Google Scholar]


