Abstract
Background
Estimates of population-based incidence for rotavirus inpatient and outpatient visits, as well as their associated medical costs, can provide valuable information to assess the potential benefits of rotavirus vaccination.
Methods
We conducted active surveillance for rotavirus gastroenteritis at 6 medical institutions for children younger than 5 years from July 2012 to June 2013 in Beijing Municipality and Gansu Province. We collected stool samples of diarrhea patients for testing rotavirus, and epidemiological, clinical and cost data.
Results
The proportion of rotavirus-positive for inpatient and outpatient visits from Beijing was 28.7% (138/481) and 19.4% (133/687); a statistically lower proportion than observed in Gansu among inpatient visits (45.2%, 245/542, P < 0.001) and among outpatient visits (28.8%, 66/229, P = 0.003), respectively. The G9P[8] genotype was most prevalent in Beijing (60.6%) and in Gansu (77.6%). The median Vesikari scale value was 16 for rotavirus inpatients and 15 for nonrotavirus inpatients. Population-based estimated rates of rotavirus-related hospitalizations were 14.4 (95% CI, 13–16) per 10,000 children, and the rate of rotavirus gastroenteritis in the outpatient setting was 149 (95% CI, 145–153) per 10,000 children younger than 5 years. The estimated total number of rotavirus-related inpatient visits were 3790 (95% CI, 2488–3827) cases and 29,101 (95% CI: 27,748–29,279) outpatient visits. The total cost of rotavirus infection was $1.4 million (95% CI, $0.9–1.4 million) for hospitalizations and $4.2 million (95% CI, $4.0–4.2 million) for outpatient visits per year in Beijing and Gansu.
Conclusion
Rotavirus gastroenteritis is associated with a large disease burden in Chinese children younger than 5 years in Beijing and Gansu. Rotavirus is the most common cause of severe acute gastroenteritis (AGE) in children younger than 5 years worldwide, accounting for an estimated 25 million clinic visits, 2 million hospitalizations and 453,000 deaths each year.1,2 In China, the world’s most populous nation, surveillance at sentinel hospitals showed that approximately 48% of AGE hospitalizations among children younger than 5 years were attributed to rotavirus from 2003 to 2007, and 13,387 rotavirus deaths were estimated in China in 2002 alone.3,4 The Lanzhou lamb rotavirus vaccine, consisting of serotype G10P[12], was licensed in 2000 but is not included in the National Expanded Program of Immunization vaccine recommendations for Chinese children.5 License applications for new rotavirus vaccines (Rotarix, produced by GlaxoSmithKline Biologicals, and RotaTeq, produced by Merck and Company) have been submitted for administering these vaccines to Chinese infants.
Keywords: rotavirus, child, population-based surveillance, hospitalization rate, medical-related cost
Chinese laboratory-based and hospitalized-based surveillance capacity includes monitoring rotavirus test-positive rates and strain genotypes since 19983,6,7 among inpatients younger than 5 years with diarrhea in selected sentinel hospitals. However, active, population-based surveillance to understand the epidemiology and estimate the burden of rotavirus gastroenteritis among Chinese children has only recently been established by the Chinese Center for Disease Control and Prevention in China’s Beijing Municipality and Gansu Province. This surveillance provides the information on the incidence of rotavirus inpatient and outpatient visits, as well as their associated medical costs, thereby providing valuable information to assess the potential benefits of rotavirus vaccination in China.
MATERIALS AND METHODS
Surveillance Sites and Population
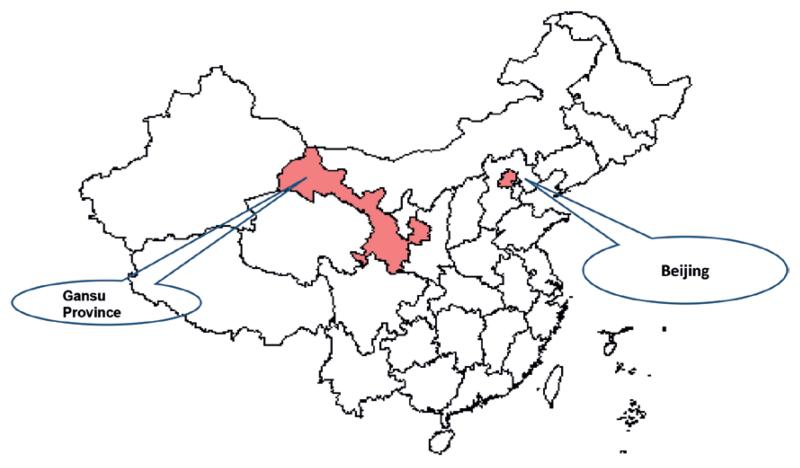
Active, prospective, population-based surveillance was conducted from July 2012 to June 2013 in Beijing Municipality and Gansu Province (Fig. 1). Beijing Municipality holds one of the largest metropolitan populations in the world and is among the most socioeconomically developed cities throughout China. Gansu Province is located in the north-west region of China and has a lower socioeconomic status. Surveillance was conducted in the 3 districts (Xicheng district, Chao yang district and Tong Zhou district) of Beijing Municipality, and in Gansu Province’s Liang Zhou district which includes Wuwei city and Lanzhou city. Six medical institutions participated in this surveillance. Four hospitals were selected in Beijing Municipality: Beijing Children’s Hospital, Peking University First Hospital, Capital Pediatric Research Institute, and Tong Zhou District Women and Children’s Medical Center. Two medical institutions in Gansu Province participated: Lanzhou University Hospital and Liangzhou District Hospital of Wuwei city. On the basis of national infectious disease reporting demographic statistics data in 2012,8 the total population of children younger than 5 years in these surveillance areas was 399,484.
FIGURE 1.
Geographic map of surveillance areas, China.
Case Definition and Enrollment of Patients
Children 14 days to 59 months old were considered eligible for enrollment if they presented to the surveillance hospitals with symptoms of AGE, defined as ≥3 loose stools and /or ≥1 episode of vomiting within 24 hours. Confirmed rotavirus case-patients were those whose stools had rotavirus detected by enzyme-linked immunoassay (EIA). AGE patients were divided into mild cases (Vesikari scale score <11), moderate cases (Vesikari scale score of 11–14) and severe cases (Vesikari scale scores ≥15).9 Hospitalized AGE case-patients were those admitted as inpatients for a stay lasting ≥24 hours or having intravenous rehydration therapy for >2 days in the outpatient clinic.
The enrolled patients with AGE symptom both in inpatient and outpatient sites have informed consent from a parent or guardian. Inpatient surveillance enrollment of all eligible inpatients occurred systematically through the study period. Outpatient surveillance enrollment occurred for all eligible AGE subjects visiting the medical institution 2 days per week in Beijing Municipality and on 3 days per week in Gansu Province.
Data Collection and Analysis
A standardized questionnaire to consenting parents/guardians that collected demographic, medical history, socioeconomic data, clinical data, rotavirus vaccination status and medically related economic costs. The direct medical care costs of hospitalizations was examined from a hospital administrative database, and direct nonmedical costs (eg, travel costs, nonprescription medications) and indirect costs (eg, lost work days for parents) were collected during follow-up interviews. The cost of lost work days was estimated using cost per person/work day of Beijing and Gansu in the Chinese Statistics Yearbook, 2012.8 All enrolled patients follow-up visits finished within approximately 14 days after discharge.
We attempted to collect a whole stool sample from each case-patient within 7 days of AGE symptom onset. Each specimen was immediately stored at −20°C, and tested for rotavirus antigen by EIA using the group A rotavirus detection kit (IDEIA Rotavirus, Dako). Rotavirus EIA-positive specimens were analyzed for rotavirus serotype and genotype detection by multiplex, reverse transcription-polymerase chain reaction methods and nucleotide sequencing according to the guideline for rotavirus laboratory detection provided by Chinese Center for Disease Control and Prevention.
Statistical analyses were conducted by using SPSS 16.0 software and Microsoft Excel. Comparisons were made by using Pearson’s χ2 test and Kruskal–Wallis test. Population-based hospitalization and outpatient visit rates were calculated as the weighted number of children enrolled with AGE with laboratory-confirmed rotavirus infections among inpatient and outpatient subjects, divided by the childhood population8 multiplied by 10,000. Weights were calculated to account for the proportion of patients who were eligible and enrolled in the study, and the proportion of eligible children who resided within the catchment area for the medical institutions conducting surveillance. The surveillance capture rates of eligible children was estimated to be 98%, according to an enteric disease clinic database in Beijing Municipality, and 60% of inpatient visits and 50% of outpatient visits based on infectious diarrhea disease reporting surveillance areas in Gansu Province according to Gansu provincial health resource information. The costs attributable to rotavirus in Beijing Municipality and Gansu Province were estimated using the population-based hospitalization and outpatient visit rates, multiplied by the total number of resident children younger than 5 years in each surveillance area.
RESULTS
In total, 28,153 AGE case-patients (including 1176 inpatient and 26,977 outpatient visits) were identified as eligible patients in Beijing Municipality and Gansu Province. A total of 1939 AGE patients were enrolled; 1023 and 916 from the inpatient and outpatient clinical settings, respectively. From Beijing Municipality, we collected stool samples from 481 (94%) of 511 eligible hospitalized patients and from a sample of 687 (3.2%) of 21,513 eligible outpatient visits. From Gansu Province, we collected stool samples from 542 (82%) of 665 eligible hospitalized AGE patients and from 229 (4.2%) of 5464 eligible AGE outpatient visits in Gansu Province. Rotavirus vaccination was self-reported and just 48 (2.5%) of the 1939 AGE patients were reported to have received any rotavirus vaccination. No deaths were observed among our enrolled AGE patients.
Epidemiologic Characteristics of Rotavirus-related AGE
Overall, 30.0% (582/1939) of children in this surveillance assessment were confirmed rotavirus-positive. Among the 1023 inpatient children, 383 (37.4%) were rotavirus-positive, and of 916 outpatient patients, 199 (21.7%) were rotavirus-positive (P < 0.001) (Table 1). The proportion of rotavirus-positive patients from inpatient settings and outpatient settings from Beijing Municipality was 28.7% (138/481) and 19.4% (133/687); a statistically lower proportion than observed in Gansu Province (45.2%, 245/542, P = 0.001) among inpatient visits and 28.8% (66/229, P = 0.003) among outpatient visits, respectively. Rotavirus positivity in Gansu Province was higher than Beijing Municipality across each strata (gender, race, urban/rural residence, insurance and vaccination) (Table 1).
TABLE 1.
Rotavirus Laboratory Results by Patient Characteristics and by Surveillance Sites
| Beijing Municipality (n = 1168) |
Gansu Province (n = 771) |
||||||
|---|---|---|---|---|---|---|---|
| RV neg. | RV pos. | RV pos. (%) | RV neg. | RV pos. | RV pos. (%) | P Value | |
| Total | 897 | 271 | 23.2 | 460 | 311 | 40.3 | <0.001 |
| Setting type | |||||||
| Inpatient | 343 | 138 | 28.7 | 297 | 245 | 45.2 | <0.001 |
| Outpatient | 554 | 133 | 19.4 | 163 | 66 | 28.8 | 0.003 |
| Age group (mo) | |||||||
| 0–2 | 72 | 7 | 8.9 | 28 | 21 | 42.9 | <0.001 |
| 3–5 | 144 | 11 | 7.1 | 104 | 45 | 30.2 | <0.001 |
| 6–11 | 360 | 110 | 23.4 | 214 | 172 | 44.6 | <0.001 |
| 12–17 | 138 | 92 | 40.0 | 69 | 51 | 42.5 | 0.652 |
| 18–23 | 81 | 23 | 22.1 | 29 | 13 | 31.0 | 0.262 |
| 24–35 | 48 | 14 | 25.8 | 9 | 6 | 27.3 | 0.924 |
| 36–47 | 33 | 7 | 17.5 | 4 | 1 | 20.0 | 1.000 |
| 48–59 | 21 | 7 | 25.0 | 3 | 2 | 40.0 | 0.597 |
| Gender | |||||||
| Male | 557 | 161 | 22.4 | 291 | 199 | 40.6 | <0.001 |
| Female | 340 | 110 | 24.4 | 169 | 112 | 39.9 | <0.001 |
| Registration type | |||||||
| Urban | 625 | 164 | 20.8 | 147 | 99 | 40.2 | <0.001 |
| Rural | 272 | 107 | 28.2 | 313 | 212 | 40.4 | <0.001 |
| Insurance | |||||||
| Yes | 160 | 62 | 27.9 | 172 | 105 | 37.9 | 0.019 |
| No | 737 | 209 | 22.1 | 288 | 206 | 41.7 | <0.001 |
| Rotavirus vaccination | |||||||
| Yes | 13 | 5 | 27.8 | 21 | 9 | 30.0 | 0.870 |
| No | 884 | 266 | 23.1 | 439 | 302 | 40.8 | <0.001 |
RV indicates Rotavirus.
Infants in Gansu Province had higher proportions of rotavirus positivity compared with Beijing Municipality (P < 0.001). In Gansu Province, rotavirus was detected in high proportions even among the youngest infants, including 0–2 month olds (42.9%, n = 21 of 49), 3–5 month olds (30.2%, n = 45 of 149) and 6–11 month olds (44.6%, n = 172 of 386).
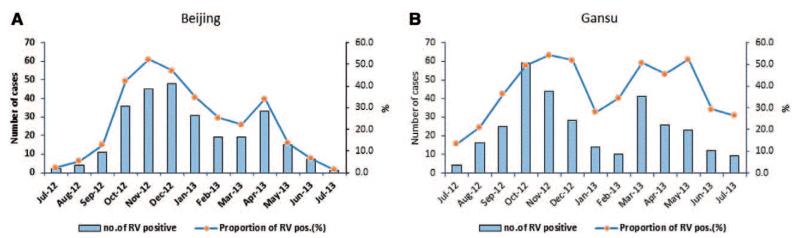
Dual rotavirus seasonal peaks were observed in Beijing Municipality from October to December and in April, and dual seasonal peaks were also observed in Gansu Province from October to December and from March to May (Fig. 2A, B).
FIGURE 2.
(A) Rotavirus test-positive proportions in AGE patients younger than 5 years by month in Beijing. (B) Rotavirus test-positive proportions in AGE patients younger than 5 years by month in Gansu Province.
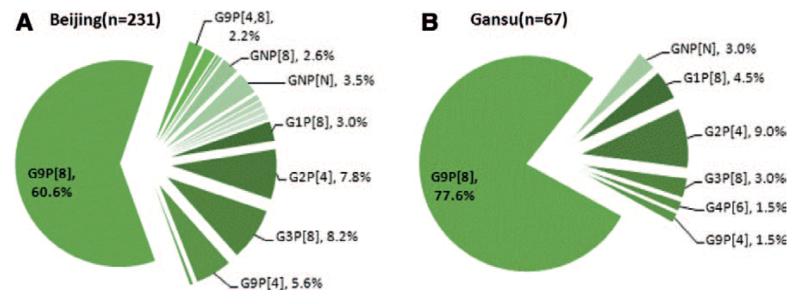
Rotavirus Strain Characterization
A sample of 298 rotavirus positive specimens were genotyped by reverse transcription-polymerase chain reaction (231 from Beijing Municipality and 67 from Gansu Province) and sequenced to determine their G and P genotypes (Fig. 3A, B). Overall, G9P[8] rotavirus infections were most prevalent both in Beijing Municipality (60.6%) and in Gansu Province (77.6%), followed by G3P[8] (8.2%) and G2P[4] (7.8%) in Beijing Municipality, and G2P[4] (9.0%) and G1P[8] (4.5%) genotypes in Gansu Province, respectively.
FIGURE 3.
(A) Rotavirus strains genotyping in children diarrhea patients in Beijing. (B) Rotavirus strains genotyping in children diarrhea patients in Gansu.
Clinical Severity
Of 582 rotavirus AGE patients, 63.6% (n = 370 of 582) were classified as severe cases, having Vesikari scale scores ≥15. Among the 1357 rotavirus-negative patients, only 40.4% were classified as severe infections according to this scale (Table 2). The difference between these Vesikari scale values for rotavirus AGE (median scores, hospitalized = 16, outpatient = 14) compared with values for nonrotavirus AGE (median scores, hospitalized = 15, outpatient = 13) were statistically significant (P < 0.001).
TABLE 2.
Clinical Characteristics and Severity for Rotavirus (RV AGE) Positive and Negative Patients (non-RV AGE)
| Clinical Characteristics | Children With RV AGE (n = 582) |
Children with non-RV AGE (n = 1357) |
P Value | ||
|---|---|---|---|---|---|
| Vesikari scale score | <0.001 | ||||
| <11 | 44 | (7.6) | 150 | 11.1 | |
| 11–14 | 168 | (28.9) | 659 | 48.6 | |
| ≥15 | 370 | (63.6) | 548 | 40.4 | |
| Diarrhea duration (days) | 0.003 | ||||
| <4 days | 359 | (61.7) | 845 | (62.3) | |
| 4–5 days | 105 | (18.0) | 173 | (12.7) | |
| 6 days and above | 113 | (19.4) | 326 | (24.0) | |
| Maximum diarrhea episodes | <0.001 | ||||
| <4 | 95 | (16.3) | 395 | (29.1) | |
| 4–5 | 167 | (28.7) | 427 | (31.5) | |
| ≥6 | 320 | (55.0) | 527 | (38.8) | |
| Maximum body temperature | <0.001 | ||||
| <38.5°C | 261 | (44.8) | 539 | 39.7 | |
| 38.5–38.9°C | 65 | (11.2) | 68 | 5.0 | |
| ≥39°C | 79 | (13.6) | 75 | 5.5 | |
| Maximum vomiting episodes | 0.028 | ||||
| 1 | 66 | (11.3) | 114 | 8.4 | |
| 2–4 | 171 | (29.4) | 207 | 15.3 | |
| 5 and above | 39 | (6.7) | 33 | 2.4 | |
| Behavioral Status | <0.001 | ||||
| Normal behavior | 526 | (90.4) | 1316 | 97.0 | |
| Restless/Irritable | 23 | (4.0) | 19 | 1.4 | |
| Lethargic | 32 | (5.5) | 21 | 1.5 | |
| Dehydration | 0.912 | ||||
| Sunken eyes | 176 | (30.2) | 234 | 17.2 | |
| Dry mouth/tongue | 231 | (39.7) | 323 | 23.8 | |
| Retraction of skin ≥2 seconds | 20 | (3.4) | 29 | 2.1 | |
RV indicates Rotavirus.
Rotavirus-related Inpatient Rate
The proportion of rotavirus-positive AGE hospitalizations among children younger than 5 years accounted for 27.8% (142 of 511) of all AGE hospitalizations in Beijing Municipality and 45.0% (299 of 665) in Gansu Province (P < 0.001).
Population-based rates of rotavirus-related hospitalizations were 14.4 (95% CI, 13–16) per 10,000 children younger than 5 years, corresponding to 1 in 694 children below 5 being hospitalized for rotavirus each year. The hospitalization rate associated with rotavirus AGE in children younger than 3 years was 24.0 (95% CI, 22–26) admissions per 10,000 children in our surveillance area.
Rotavirus AGE hospitalization rates were lower in Beijing Municipality (4.4 per 10,000, 95% CI: 3.5–5.4 per 10,000) compared with Gansu Province (23.8 per 10,000, 95% CI: 22–26 per 10,000) in children younger than 5 years. Infants <1 year old in Gansu Province had a significantly higher rotavirus AGE hospitalization rate (99.4 per 10,000, 95% CI: 90–109 per 10,000) compared with Beijing Municipality (13.5 per 10,000, 95% CI: 10–18 per 10,000). The rate in 1-year old (21.7 per 10,000) in Gansu Province was also significant higher than the rate in Beijing Municipality (8.8 per 10,000). But the hospitalization rates of 2-year old (1.4 per 10,000), 3-year old (0 per 10,000) and 4-year old (0.5 per 10,000) children in Gansu Province were similar between Beijing Municipality (0.4 per 10,000; 0.3 per 10,000 and 0.5 per 10,000), respectively.
Rotavirus-related Outpatient Visit Rate
The population-based rate of rotavirus AGE in the outpatient clinical setting was 149 (95% CI = 145–153) per 10,000 children younger than 5 years, corresponding to 1 in 67 children below 5 having an outpatient visit for rotavirus each year. In Beijing Municipality, the population-based outpatient visit rate was 147.5 (95% CI, 112–153) per 10,000 children. In Gansu Province, the outpatient visit rate was 150.4 (95% CI, 145–156) per 10,000 children. For infants <1-year old, the rotavirus outpatient rate in Beijing Municipality (379.7 per 10,000) was lower than in Gansu Province (513.7 per 10,000) (P < 0.001). But the rates of rotavirus outpatient visits among 1-year olds (292.2 per 10,000), 2-year olds (57.1 per 10,000), 3-year olds (27.0 per 10,000) and 4-year olds (22.0 per 10,1000) in Beijing Municipality were all higher than outpatient visit rates in Gansu Province (198.8 per 10,000, 33.5 per 10,000, 11.3 per 10,000 and 11.6 per 10,000).
Estimated Disease Burden and Economic Cost of Rotavirus-related AGE
Summed medical-related costs including direct and indirect medical costs per rotavirus AGE outpatient visit amounted to $144.90, derived from a sample of 199 rotavirus-positive AGE outpatient children (Table 3). The total cost per rotavirus AGE-hospitalized patient was $372.30, based on the cost of 323 patients with rotavirus-positive AGE in inpatient settings. If applied to the estimated number of patients with rotavirus-related AGE 3790 (95% CI: 2488–3827) hospitalized patients and 29,101 (95% CI: 27,748–29,279) outpatient visits per year, the total cost of rotavirus in children younger than 5 years was $1.4 million (95% CI: $0.9–1.4 million) for hospitalizations and $4.2 million (95% CI: $4.0–4.2 million) for outpatient visits per year.
TABLE 3.
Municipality/Provincial Estimated Burden and Cost (US $) for Rotavirus AGE
| Cost per patient(US$) |
Municipality/Provincial Total Estimated Burden per Year |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Area | Setting | Direct Medical Cost |
Direct Nonmedical Cost |
Indirect Cost | Total Cost | Number of Rotavirus AGE Patients (95% CI) |
Total Cost (95% CI) (million) |
||
| Beijing | Outpatient | 55.4 | 14.3 | 74.6 | 144.3 | 7929 | (7799–8153) | 1.1 | (1.1–1.2) |
| Inpatient | 78.1 | 28.4 | 101.6 | 208.1 | 241 | (177–273) | 0.1 | (0.08–0.1) | |
| Gansu | Outpatient | 60.5 | 23.2 | 61.6 | 145.3 | 21172 | (20405–21953) | 3.1 | (3.0–3.2) |
| Inpatient | 330.9 | 50.7 | 154.7 | 536.3 | 3549 | (3096–3659) | 1.9 | (1.7–2.0) | |
| Beijing and Gansu |
Outpatient | 58.0 | 18.8 | 68.1 | 144.9 | 29101 | (27748–29279) | 4.2 | (4.0–4.2) |
| Inpatient | 204.5 | 39.6 | 128.2 | 372.3 | 3790 | (2488–3827) | 1.4 | (0.9–1.4) | |
DISCUSSION
Our assessment of the epidemiology of rotavirus AGE in Chinese children clearly demonstrates the substantial disease burden from rotavirus and the potential for large benefits from vaccination in the future. Almost one-fourth (22%) of outpatient AGE visits and 37% of AGE hospitalizations were determined by laboratory confirmation to have been caused by rotavirus among children younger than 5 years from July 2012 to June 2013 in Beijing Municipality and Gansu Province. Population-based inpatient and outpatient visit rate estimates due to rotavirus gastroenteritis were similar to those among children younger than 5 years between 2000 and 2006 in the United States,10 and to those in Honjo city and surroundings in northern Japan (13/10,000).11 Our rotavirus rates are higher than the rates in 2008 (4/10,000) and in 2009 (6/10,000) reported in the United States.10 Our rates were lower than Hangzhou of China (21/10,000) during 2007–2008 from a hospital-based study,12 and lower than Hong Kong of China (20/10,000) during 1987–1996.13 The inpatient rate (24/10,000) associated with rotavirus AGE in the subset of children younger than 3 years in our study was similar (22.5/10,000) to that found for children of this age in the United States during the last year before widespread use of rotavirus vaccines there, 2006.9
The overall proportion (37%) of rotavirus-associated hospitalizations among children with AGE younger than 5 years decreased 21% and 24% compared with previously published rates during 2001–2003 and 2003–2007 in 11 Chinese sentinel sites, respectively, and this variability may be due to secular trends, differences in vaccination, study design factors, subject ages and hospital utilization practices.3,7 The rotavirus test-positive proportion (28.2%) of hospitalized children in Beijing Municipality decreased 20% compared with 36% during 2003–20073 and this was lower than the prevalence found in Morocco and Japan (44–56%)14,15 and was higher than that observed in Hong Kong.13
Our study found that medically attended rotavirus infections varied by surveillance location, particularly among the youngest subjects. The 0 to 2 and 3 to 5-month age groups in Beijing Municipality had a lower proportion of rotavirus positivity compared with those in Gansu Province. Seven percent (7%) of the enrolled subjects in Beijing Municipality were younger than 6 months, compared with 21% of those in Gansu Province. These youngest age groups are often considered to be protected through passive immunity via maternal antirotavirus antibodies; therefore, the relatively high rate of rotavirus hospitalizations and outpatient visits among this age group observed in Gansu Province is striking and warrants further investigation. We found 21 infants 0–2 months old hospitalized with rotavirus infection in Gansu Province, and 16 (76%) had diagnosed co-morbidities. Among the 36 infants 3–5 months old and hospitalized with rotavirus in Gansu Province, 12 (33.3%) had comorbidities. None of them had a reported history of receiving any rotavirus vaccinations. Rotavirus AGE may pose a sizeable threat for young infants suffering from other comorbidities, such as respiratory diseases and neonatal disorders.
Rotavirus-related AGE was characterized by fever, a long duration of diarrhea, vomiting and watery stool in our subjects, similar to other research.3,16-20 But nearly all (92.5%) rotavirus AGE patients were classified as having either moderate or severe classifications by Vesikari severity scale; higher than in hospitalized AGE patients in Greece (58.7%).17
Gansu Province and Beijing Municipality are situated in northern China. In our study, rotavirus infection occurred with similar seasonal patterns in Beijing Municipality and Gansu Province overall, with a first peak from October to December and a second peak from March to May. A double-peak pattern was also reported in Beijing Municipality during 2001–2003, as well as in China’s Kunming City and Suzhou City.7 During 2001–2003 and 2003–2007, southern China and northern China had no significant differences in peak seasonality.3,7 In the United States, the rotavirus epidemic peaked in the winter months during the period before widespread rotavirus vaccination,21 but now occurs for a delayed, truncated period.9 Further studies on rotavirus seasonality need to be conducted so as to understand geographic differences and other contributing factors.
We found that the rotavirus hospitalization rate and outpatient visit rate of patients <1-year old in Gansu Province was both higher than patients <1-year old in Beijing. The possible reasons involved in higher proportion of rotavirus positive in Gansu (45%, 195/436) than Beijing (25%, 71/280) in inpatient patients under 1 year old and higher severe cases’ percentage in Gansu (81%, 354/436) than Beijing (34%, 95/280). Our results also showed the higher visiting proportions in the outpatient settings in patients of 1-4-years old was found in Beijing than Gansu. This related to more proportions on patients >1-year old, mild patients and lower proportions of rotavirus positive in Beijing than Gansu.
Our study results showed that the average direct medical cost for outpatient visit and hospitalized patient was US $ 58.00 and was higher than the average cost (US $ 13.99) of rotavirus outpatient visits in 2006–2007 and the cost (US $ 13.51) in 2004 in China.22,23 The direct medical cost (US $ 204.5) of hospitalization for rotavirus AGE is lower than previous funding of US $ 459.83 in 2006–2007, but is higher than the cost (US $108.96) in 2004 in China.22,23 The total social cost (US $ 144.9) of outpatient visit per patient is higher than previous study (US $ 61.64), but the total health care cost of hospitalized patient per patient (US $ 372.3) is lower than previous study (US $ 684.15) in 2006–2007 in China.22 Health care costs arising from outpatient visits are higher (300% increase) compared with these costs during 2006–2007 in China.
Our finding of G and P types circulating in Beijing and Gansu were predominated by G9P[8] was similar with Kenya (35%),24 but different from circulating strains of G3P8 (32.1%) before 2011 in China.25 G9 was also detected in Hebei province which is nearby Beijing from 2009.26 New rotavirus vaccines indicated for the prevention of rotavirus gastroenteritis caused by G1 and non-G1 types (G3, G4 and G9) in infants and children,27 but have not been introduced to China. The Lanzhou Lamb rotavirus vaccine is currently approved for use in China, but is not part of the Expanded Program of Immunization and its cost is not covered by the national vaccination program. In our study, whereupon parents were asked for vaccination status during an interview, only a small proportion (2.5%) of children with diarrhea illness were reported to have received at least 1 vaccine dose. This is a lower proportion than observed in Guangzhou, China in 2009–2011, where 14.4% reportedly received at least 1 dose and 0.4% were vaccinated with a full course of 2 doses.28,29 Increased use of effective rotavirus vaccines could dramatically decrease the disease burden due to rotavirus that we observed.
Extrapolating from our population-based findings to the Chinese population, we estimate 110,000 (100,000–120,000) rotavirus hospitalizations and 1.2 million (1.1–1.2 million) outpatient visits occur per year in China in young children. The estimated social cost for rotavirus infection younger than 5 years is US $ 42 million per year for hospitalizations and US $ 168 million cost for outpatient visits per year in China. This disease burden baseline in children younger than 5 years during an era before widespread use of rotavirus vaccines could be helpful for assessing rotavirus vaccination policies.
Some limitations should be considered in the study. Including medical institutions in Beijing Municipality and Gansu Province provided differences in socioeconomic levels and health care access that may have been important to observed differences between these locations. Two areas belong to northern China through previous studies showed no significant different on seasonality. Another limitation is that we had low enrollment among outpatient AGE visits, due in part to the large number of children attending these outpatient settings, and this may have affected the representativeness of our outpatient estimates. We estimated the sample size with 20–30% positive rate and 10% lost visit rate after main visit for keeping the study samples for enrolling. We used the proportions of diarrhea cases in selected hospitals out of total reported diarrhea cases in surveillance areas of Gansu province for estimating capture rates, but it has limitation due to under-reporting. The daily and monthly statistics for all inpatient and outpatient visits for diarrhea or AGE were conducted but the detail information is limited for analysis. Although 1-year round active surveillance provides some seasonal pattern, but the epidemic strains changes and seasonality change cannot be captured.
China is the most populous nation in the world, with a large childhood population. Our study highlights that rotavirus infections bring large disease burden and economic social costs in children younger than 5 years. Further surveillance to document these burdens and to describe the potential benefits from rotavirus vaccines to reduce these burdens is needed in China.
ACKNOWLEDGMENTS
We thank the participation of all enrollees in 6 hospitals (Beijing Children’s Hospital, Peking University First Hospital, Capital Pediatric Research Institute, and Tong Zhou District Women and Children’s Medical Center, Lanzhou University Hospital and Liangzhou District Hospital of Wuwei city) and local Center for Disease Control and Prevention (CDC) including Beijing Municipality CDC, CDC of Chaoyang district of Beijing, Xicheng district of Beijing and Tongzhou district of Beijing; Gansu Provincial CDC and CDC of Liangzhou district of Wuwei city in Gansu in this study. We thank the support by the fund for annual disease surveillance of Chinese Center for Disease Control and Prevention.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the US Centers for Disease Control and Prevention.
Footnotes
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Parashar UD, Hummelman EG, Bresee JS, et al. Global illness and deaths caused by rotavirus disease in Children. Emerg Infect Dis. 2003;9:565–572. doi: 10.3201/eid0905.020562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tate JE, Burton AH, Boschi-Pinto C, et al. estimate of worldwide rotavirus-associated mortality in children younger than 5 years before the introduction of universal rotavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis. 2008;2012;12:136–141. doi: 10.1016/S1473-3099(11)70253-5. [DOI] [PubMed] [Google Scholar]
- 3.Duan Z-J, Liu N, Yang S-H, et al. Hospital-based surveillance of rotavirus diarrhea in the People’s Republic of China, August 2003-July 2007. J Infect Dis. 2009;200:S167–173. doi: 10.1086/605039. [DOI] [PubMed] [Google Scholar]
- 4.Yee EL, Fang Z-Y, Liu N, et al. Importance and challenge of accurately counting rotavirus deaths in China, 2002. Vaccine. 2009;27S:46–49. doi: 10.1016/j.vaccine.2009.08.065. [DOI] [PubMed] [Google Scholar]
- 5.Fu C, He Q, Xu J, et al. Effectiveness of the Lanzhou lamp rotavirus vaccine against gastroenteritis among children. Vaccine. 2012;31:154–158. doi: 10.1016/j.vaccine.2012.10.078. [DOI] [PubMed] [Google Scholar]
- 6.Zhao-Y F, Yang H. Diversity of rotavirus strains among children with acute diarrhea in China: 1998–2000 surveillance study. J Clin Microbiol. 2002;40:1875–1878. doi: 10.1128/JCM.40.5.1875-1878.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fang Z-Y, Wang B, Kilgore PE, et al. Sentinel hospital surveillance for rotavirus diarrhea in the People’s Republic of China, August 2001-July 2003. J Infect Dis. 2005;192:S94–S99. doi: 10.1086/431505. [DOI] [PubMed] [Google Scholar]
- 8.Ministry of health of the people’s Republic of China . China Health Statistical Yearbook (2012) Peking Union Medical College Press; Beijing, China: 2012. [Google Scholar]
- 9.Ruuska T, Vesikari T. A prospective study of acted diarrhea in Finnish children. Acta Padiatr Scand. 1991;80:500–507. doi: 10.1111/j.1651-2227.1991.tb11893.x. [DOI] [PubMed] [Google Scholar]
- 10.Payne D, Staat MA, Edwards KM, et al. Active, population-based surveillance for severe rotavirus gastroenteritis in children in the United States. Pediatrics. 2008;122:1235–1243. doi: 10.1542/peds.2007-3378. [DOI] [PubMed] [Google Scholar]
- 11.Desai R, Curns AT, Steiner CA, et al. All-cause gastroenteritis and rotavirus-coded hospitalization among US children, 2000–2009. Clin Infect Dis. 2012;55:e28–e34. doi: 10.1093/cid/cis443. [DOI] [PubMed] [Google Scholar]
- 12.Nakagomi T, Nakagomi O, Takahashi Y, et al. Incidence and burden of rotavirus gastroenteritis in Japan, as estimated from a prospective sentinel hospital study. J Infect Dis. 2005;192(suppl 1):S106–S110. doi: 10.1086/431503. [DOI] [PubMed] [Google Scholar]
- 13.Lou J-T, Xu X-J, Wu Y-D, et al. Epidemiology and burden of rotavirus infection among children in Hangzhou, China. J Clin Virol. 2011;50:84–87. doi: 10.1016/j.jcv.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Chen PKS, Tam JS, Nelson EAS, et al. Rotavirus infection in Hong Kong: epidemiology and estimates of disease burden. Epidemiol Infect. 1998;120:321–325. doi: 10.1017/s0950268898008747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Behafid M, Rguigh A, Trivedi T, et al. Monitoring of rotavirus vaccine in Morocco: establishing the baseline burden of rotavirus disease. Vaccine. 2012;30:6515–6520. doi: 10.1016/j.vaccine.2012.08.058. [DOI] [PubMed] [Google Scholar]
- 16.Ito H, Otabe O, Katsumi Y, et al. The incidence and direct medical cost of hospitalization due to rotavirus gastroenteritis in Kyoto, Japan, as estimated from a retrospective hospital study. Vaccine. 2011;29:7807–7810. doi: 10.1016/j.vaccine.2011.07.105. [DOI] [PubMed] [Google Scholar]
- 17.Onstantopoulos A, Tragiannidis A, SFouzas A, et al. Burden of rotavirus gastroenteritis in children <5 years of age in Greece: hospital-based prospective surveillance (2008–2010) BMJ Open. 2013;3:e003579. doi: 10.1136/bmjopen-2013-003570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sowmyanarayanan TV, Ramani S, Sarkar R, et al. Severity of rotavirus gastroenteritis in Indian children requiring hospitalization. Vaccine. 2012;305:A167–A172. doi: 10.1016/j.vaccine.2011.07.145. [DOI] [PubMed] [Google Scholar]
- 19.Giaquinto C, Van Damme P, Huet F, et al. Clinical consequences of rotavirus acute gastroenteritis in Europ. 2004–2005: the REVEAL study. J Infect Dis. 2007;195:S26–35. doi: 10.1086/516717. [DOI] [PubMed] [Google Scholar]
- 20.Steele AD, Bos P, Alexander JJ. Clinical features of acute infantile gastroenteritis associated with human rotavirus subgroups I and II. J Clin Microbiol. 1988;26:2647–2649. doi: 10.1128/jcm.26.12.2647-2649.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pitzer VE, Viboud C, Simonsen L, et al. Demographic variability, vaccination, and the spatiotemporal dynamics of rotavirus epidemics. Science. 2009;325:290–294. doi: 10.1126/science.1172330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jin H, Wang B, Fang Z, et al. Hospital-based study of the economic burden associated with rotavirus diarrhea in eastern China. Vaccine. 2011;29:7801–7806. doi: 10.1016/j.vaccine.2011.07.104. [DOI] [PubMed] [Google Scholar]
- 23.Wang B, Fang ZY, Gao Q, et al. the study of disease burden on rotavirus diarrhea in China. Chin J Vaccines Immunization. 2005;11(suppl.):15–17. [Google Scholar]
- 24.Kiulia NM, Nyaga MM, Seheri ML, et al. Rotavirus G and P types circulating in the eastern region of Kenya: predominance of G9 and emergence of G12 genotypes. Pediatr Infect Dis J. 2014;33(suppl 1):85–88. doi: 10.1097/INF.0000000000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu N, Xu Z, Li D, et al. Update on the disease burden and circulating strains of rotavirus in China: a systematic review and meta-analysis. Vaccine. 2014;32:4369–4375. doi: 10.1016/j.vaccine.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 26.Ma X, Li DD, Guo YQ, et al. Whole genome analysis of human group A rotavirus G9p[8] strains in Hebei Lulong region,2009–2011. Bing Du Xue Bao. 2014;30:119–127. in Chinese. [PubMed] [Google Scholar]
- 27.O’Ryan M. Rotarix (RIX4414): an oral human rotavirus vaccine. Expert Rev Vaccines. 2007;6:11–19. doi: 10.1586/14760584.6.1.11. [DOI] [PubMed] [Google Scholar]
- 28.Fu C, He Q, Xu J, et al. Effectiveness of the Lanzhou lamb rotavirus vaccine against gastroenteritis among children. Vaccine. 2012;31:154–158. doi: 10.1016/j.vaccine.2012.10.078. [DOI] [PubMed] [Google Scholar]
- 29.Fu C, Tate JE, Jiang B. Effectiveness of the Lanzhou lamb rotavirus vaccine against hospitalized gastroenteritis. Human Vaccine. 2010;6:11. doi: 10.4161/hv.6.11.12847. [DOI] [PubMed] [Google Scholar]