Abstract
Hyperoxic and hypercapnic hyperoxic gas challenges are increasingly being used in cerebrovascular reactivity (CVR) and calibrated fMRI experiments. The longitudinal arterial blood-water relaxation time (T1a) change with hyperoxia will influence signal quantification through mechanisms relating to elevated partial pressure of plasma-dissolved O2 (pO2) and increased oxygen bound to hemoglobin in arteries (Ya) and veins (Yv). The dependence of T1a on Ya and Yv has been elegantly characterized ex vivo, however the combined influence of pO2, Ya and Yv on T1a in vivo under normal ventilation have not been reported. Here, T1a is calculated during hyperoxia in vivo by a heuristic approach that evaluates T1-dependent arterial spin labeling (ASL) signal changes to varying gas stimuli. Healthy volunteers (n=14; age=31.5±7.2yrs) were scanned using pseudo-continuous ASL in combination with room air (RA;21%O2/79%N2), hypercapnic-normoxic (HN; 5%CO2/21%O2/74%N2), and hypercapnic-hyperoxic (HH; 5%CO2/95%O2) gas administration. HH T1a was calculated by requiring that the HN and HH CBF change be identical. The HH protocol was then repeated in patients (n=10; age=61.4±13.3yrs) with intracranial stenosis to assess whether a HH T1a decrease prohibited ASL from being performed in subjects with known delayed blood arrival times. Arterial blood T1a decreased from 1.65s at baseline to 1.49±0.07s during HH. In patients, CBF values in the affected flow territory for the HH condition were increased relative to baseline CBF values and were within physiological range (RA-CBF=36.6±8.2ml/100g/min;HH-CBF=45.2±13.9ml/100g/min).
Conclusion
Hyperoxic (95% O2) 3T arterial blood T1aHH =1.49±0.07s relative to a normoxic T1a of 1.65s.
Keywords: carbogen, arterial spin labeling, blood, hypercapnia, cerebrovascular reactivity, hyperoxia, T1
Graphical Abstract
We calculate in vivo arterial blood T1 changes at 3T during hyperoxic hypercapnic (carbogen) gas challenges.
A heuristic approach was used to compute T1-dependent ASL signal changes to varying gas stimuli.
Arterial blood T1 decreased from 1.65s at baseline to 1.49 ± 0.07s during carbogen.
The T1 correction was applied to ASL data in intracranial stenosis patients using a carbogen protocol.
The calculated T1 value should provide reference for future calibrated fMRI, ASL and VASO experiments using hyperoxic gas mixtures.
Introduction
Cerebrovascular reactivity (CVR) can be defined as the change in cerebral blood flow (CBF) and volume (CBV) in response to a vascular stimulus, and can be used to examine vascular reserve capacity or iso-metabolic reactivity mechanisms. Breathing hypercapnic gas mixtures causes relaxation of arteriolar smooth muscles through mechanisms related to reductions in pH, which in turn cause global increases in CVR in gray and white matter parenchyma (1,2). As such, a non-invasive method for eliciting CVR changes is with the administration of hypercapnic gas mixtures (e.g., CO2 in air: 5% CO2/21% O2/74% N2 or carbogen-5: 5% CO2/95% O2), which both allow for evaluation of vascular compliance in health and disease (3–8).
The elicited changes in CVR can be measured with non-invasive MRI techniques, the most common being blood-oxygenation-level-dependent (BOLD) MRI. However, the BOLD signal is nonspecific, influenced by CBF, CBV and cerebral metabolic rate of oxygen consumption (CMRO2), and deciphering the contributions of each is non-trivial. An alternative MRI technique is arterial spin labeling (ASL) (9). ASL MRI is more specific to CBF by magnetically labeling the arterial blood water proximal to the imaging region and acquiring an image after a post-labeling delay (PLD) time. This labeled image is subtracted from a non-labeled or “control” image, resulting in a CBF-weighted image. One difficulty with ASL and hyperoxia is that the label decays with the arterial blood water T1a. The T1a is highly dependent on blood oxygenation status, which will influence the measured CBF if not incorporated correctly into quantification models.
T1a values for different O2 saturation (fraction of O2 bound to hemoglobin) levels have been estimated ex vivo in bovine blood at 3T (10,11), 4.7T (12) and 7T (13), and human blood (14). The disadvantage of ex vivo experiments is that anti-coagulants added to the blood mixtures may influence relaxation mechanisms while it is also difficult to precisely control for temperature, O2 saturation, and pO2 at physiological levels in all experiments. In vivo estimation of T1a is likewise challenging due to both practical issues and two competing physiological effects that influence blood water T1 during hyperoxia (12,15). First, hyperoxia increases arterial and venous O2 saturation (Ya and Yv, respectively) which will increase blood water T1 due to paramagnetic effects from decreased deoxyhemoglobin content. Previous ex vivo work has shown that blood water R1 = 1/T1 decreases linearly with increasing hemoglobin O2 saturation (12,13). Second, hyperoxia also increases the arterial and venous partial pressure of O2 (PaO2 and PvO2, respectively) and thus the amount of plasma dissolved O2, resulting in a decrease in blood water T1. Previous ex vivo work has shown that R1 = 1/T1 increases linearly with plasma dissolved O2 concentration (11,12).
A practical drawback of in vivo T1a estimation using multi-recovery or multi-flip angle approaches is primarily that it is difficult to localize pure blood voxels, especially arterial blood voxels, and additionally that blood may flow in or out of the inversion/excitation volume over the experiment, thereby complicating steady state assumptions (16–20). Additionally, the presence of inhomogeneous B0 and B1 fields can complicate quantification. Previous in vivo studies have focused mainly on measuring venous blood water T1v to circumvent the issues, as venous blood water in the superior sagittal sinus can be inverted over a larger spatial range of homogenous B0 and B1 and also the sagittal sinus is large enough to enable blood voxels to be isolated with minimal partial volume effects (16–20). Using T1v as a proxy for studying the effect of hyperoxia on T1a is complicated by the previously mentioned two effects that influence blood water T1. During hyperoxia, venous blood undergoes a more complicated process as it will see a substantial increase in Yv (as compared to Ya) and thus an increase in T1v. This effect is known to be the dominant effect compared to the decrease in T1v due to the small increase in plasma-dissolved O2 (PvO2) (21).
In general, ex vivo and in vivo studies indicate that the prominent T1a effect of hyperoxia occurs from increases in plasma dissolved O2 resulting in an overall decreased T1a (12–15,18). One study investigated the CBF response in humans to hyperoxia using ASL MRI at 3T (15) and obtained T1a values using extrapolation of ex vivo literature values (10) for a range of O2 saturation levels. To our knowledge, the T1a value at 3T for hyperoxic blood conditions has not been experimentally quantified in vivo. As the T1a affects the decay of the label and thus the CBF quantification, the issue is fundamental to CBF measurements using hyperoxia in basic science (10,15,22–26) but also in clinical studies, for example CVR evaluations in steno-occlusion patients (5,27,28). In the latter, a hyperoxic component may be incorporated to increase tissue or blood oxygenation for the purposes of extracting additional information regarding blood arrival times, blood volume, and/or metabolism (1,3,29–33). Knowledge of T1a is equally important in calibrated fMRI experiments. These incorporate ASL and BOLD imaging to estimate neuronal induced CMRO2 changes using hybrid (hypercapnic and hyperoxic) gas challenges (8). Furthermore, for studies using vascular space occupancy (VASO) MRI (34,35) combined with hypercapnic/hyperoxic gas challenges, accurate knowledge of T1a for different conditions is crucial for precise nulling of arterial blood and thus quantification of CBV changes.
Here, we utilize quantification principles of ASL and the dependence of this contrast on T1a to quantify T1a in vivo. To achieve this, we apply hypercapnic normoxia (5%CO2/21%O2/74%N2, abbreviated as HN) and hypercapnic hyperoxia (5%CO2/95%O2, i.e. carbogen-5, abbreviated as HH) stimuli sequentially in healthy volunteers in conjunction with ASL MRI. The hypothesis to be investigated is that when there is a small-to-negligible effect on CBF of breathing hyperoxia for short durations (33,36,37), it is possible to quantify the T1a change during carbogen administration. Here the assumption is that the identical hypercapnic fraction (i.e., 5% CO2) is the predominant contributor to CBF changes in both stimuli types, HN and HH, and thus CBF changes should be similar between these two stimuli after controlling for T1a changes. Nonetheless, to accommodate any potential CBF changes of hyperoxia, we also computed the T1a,HH for a range of simulated hyperoxia induced CBF changes.
Finally, we assess the clinical feasibility of ASL in the presence of hyperoxia by applying the calculated hyperoxic T1a to ASL data acquired during HH administration in patients with angiographically-confirmed stenosis with delayed blood water transit times (38,39). The purpose of this component of the study was to evaluate whether decreases in T1a,HH prohibited pCASL data from being interpretable during HH administration at typical PLD times. This possibility exists owing to the faster recovery of the longitudinal component of blood water magnetization following inversion in the presence of hyperoxia, which may lead to insufficient SNR at typical PLDs in patients with delayed bolus arrival time, thereby providing non-physiological CBF values and/or CBF reactivity measures.
Materials and Methods
Participants
Healthy volunteers (n = 14; 8M/6F; age = 31.5 ± 7.2 yrs) with no history of cerebrovascular disease or stroke and subjects (n = 10; 6M/4F; age = 61.4 ± 13.3 yrs) with angiographically-confirmed intracranial (IC) stenosis provided informed, written consent. The study was approved by the Institutional Review Board and in compliance with the Helsinki Declaration.
Arterial blood water T1 quantification procedure
Healthy volunteers were scanned on a 3T Philips Achieva system (Philips Healthcare, Best, The Netherlands) using body coil transmission and 8-channel SENSE head coil reception. Participants were closely fitted with a non-rebreathing oxygen mask and a nasal cannula. Gas was delivered to the mask at 12L/min during a breathing protocol of baseline period (room air, RA) followed by hypercapnic gas mixture period (either 5% CO2 in air, HN; or carbogen-5, HH). Stimulus order was randomized across participants, and heart rate, Ya, and end-tidal CO2 (EtCO2) were required to return to baseline before beginning the next scanning block presentation (approximately 3 min). CBF changes were assessed using pseudo-continuous ASL (pCASL) with a multi-slice single-shot EPI readout. Healthy volunteers were split in two groups (n1 = 7 and n2 = 7) and scanned with two different gas administration period durations and PLD times to evaluate whether small variations in blood transit time between gas stimuli did not contribute substantially to the T1a,HH measurement.
Group 1 (n1 = 7, 4M/3F; age = 33.6 ± 9.4 years) was subjected to a 272.5s baseline RA period followed by a 272.5s gas mixture (HN or HH) period. Group 1 pCASL scan parameters were: TR=3900ms, TE=13ms, PLD=1525ms, background suppression was enabled, spatial resolution=3.5×3.5×7mm3, inter-slice gap=0.5 mm, slices=17, volumes=27 (RA + HH/HN), scan duration=545s. Spin labeling was performed using a label-duration of 1.5s consisting of 0.5 ms Hanning-windowed pulses. Group 2 (n2 = 7, 4M/3F; age = 29 ± 3.7 years) was subjected to a 240s baseline RA period followed by a 240s gas mixture (HN or HH) period. Group 2 pCASL scan parameters were identical to group 1 except: PLD=1700ms; spatial resolution = 3.5×3.5×7mm3, inter-slice gap=0.5 mm, volumes = 13 (for both RA and HH/HN), scan duration = 109s.
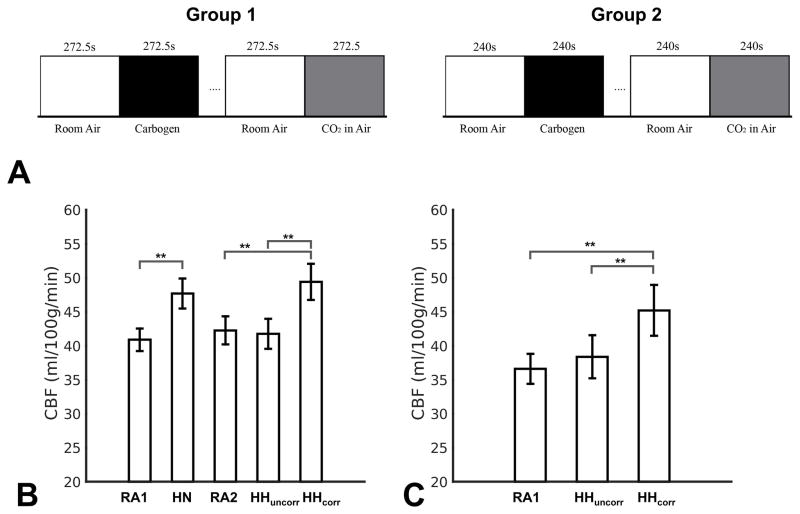
The pCASL scans were started when the observed EtCO2 level plateaued. The experimental design is shown in Figure 1A.
Figure 1.
(A) Experimental paradigm. Each 272.5s (group1, left) and 240s (group2, right) presentation of a gas mixture (e.g., room air, carbogen or CO2 in air) was a stimulus block. The presentation order of the scanning blocks (e.g., Room air + hypercarbic stimulus block) was randomized across healthy participants, where the space between scanning blocks signifies monitored time for the participant’s heart rate, Ya, and EtCO2 to return to baseline. Mean CBF values for healthy participants (B) and patients (C) for different gas mixtures: room air (RA1) before 5%CO2 in air (HN), room air (RA2) before carbogen-5 (HH). HHuncorr and HHcorr are the CBF values for HH condition using a normoxic T1a,RA (1.65s) and hyperoxic T1a,HH (1.49s) obtained from the fitting procedure. Error bars denote the s.e.m. (n=14 control volunteers and n=10 steno-occlusive disease patients). ** denotes significant differences (p < 0.025) for a paired Student’s t-test.
Additionally, an M0 scan was acquired for both groups for CBF quantification, using identical acquisition geometry as the pCASL scan but with a TR=20s and 15s for group 1 and group 2, respectively, and the spin labeling pulse-train turned off.
Data were corrected for motion using standard routines from the FMRIB Software Library (FSL (40)). CBF in both RA conditions and both HN and HH stimulus blocks was quantified by applying a simplified single-compartment pCASL kinetic model as recently suggested by the ISMRM perfusion study group and ASL white paper (41) to the average difference magnetization (ΔM). The ΔM data was obtained using a surround-subtraction approach that also realizes baseline drift removal. CBF was quantified according to
| [1] |
for i = RA, HN, or HH,
where CBF is in ml/100g/min, α = 0.85 is the pCASL labeling efficiency, τ = 1.5s is the labeling duration, T1a is the arterial blood water T1 (in seconds), and λ = 0.9ml/g is the tissue/blood partition coefficient of water. M0, the equilibrium brain magnetization signal, was obtained from the equilibrium M0 scan after spatial smoothing using a 3-dimensional Gaussian kernel (full-width-half-at-maximum = 7mm). PLD is 1.525s and 1.700s for group 1 and group 2, respectively. The slice dependency of the PLD was taken into account using the slice time of the pCASL scan.
CBF in the RA, HN and HH conditions was initially quantified using Eq. 1 assuming a T1a,RA = T1a,HN = T1a,HH,initial = 1.65s measured ex vivo under normoxic conditions from bovine blood water (10). Also, this value is recommended by the ISMRM perfusion study group and ASL white paper (41), and therefore expected to be used abundantly in future ASL-based CBF studies as reference T1a,RA value. CBF data were spatially smoothed using a 3-dimensional Gaussian smoothing kernel (full-width-half-at-maximum=7 mm) and registered to MNI standard space using the FLIRT tool from FSL (40). Subsequent processing was done in MATLAB (Mathworks, Natick, MA). We focused on cortical gray matter CBF (using a cortical gray matter MNI mask) as white matter CBF transit time is 2–3 times longer than gray matter and thus could not be accurately sampled at our PLD (42).
To determine the T1a,HH, the parameter of interest, we required that the mean HN and HH cortical CBF change, ΔCBF, relative to RA be identical. This heuristic approach assumes that the vasodilatory effect from hypercapnia is much greater than any small vasoconstrictive effects that may occur during a short period of hyperoxia. The CBF for the HH condition was recomputed for a range of T1a,HH values; 1.3s to 1.62s in steps of 0.004s, yielding a calibration curve of the ΔCBF dependency on T1a,HH. Also, to accommodate different assumed normoxic T1a,RA values in future studies we repeated the above simulation for a range of different normoxic T1a,RA (and thus T1a,HN) values: 1.6 to 1.75s in steps of 0.01s.
Lastly, to investigate potential hyperoxic vasoconstrictive effects, we simulated how the calculated T1a,HH values would change for small reductions (0%–20%) in HH CBF relative to HN CBF. The following model was used:
| [2] |
where c is the fractional reduction, ranging from 0 to 0.2, in baseline (RA) CBF due to hyperoxic vasoconstriction, and ΔCBFHH the absolute increase in CBF due to hypercapnic vasodilation (assumed to be identical for both HN and HH conditions).
A T1a,HH value for each participant and each normoxic T1a,RA was computed, and averaged to arrive at a group mean T1a,HH value, for group 1 and group 2 respectively, and a total mean T1a,HH across both groups. Using the total mean T1a,HH, the HH CBF was quantified again for each volunteer. Comparisons were made between the CBF values for the two baseline RA conditions, and between the corrected CBF values in the HH condition vs CBF values in the HN condition, using two-tailed Student’s t-tests with Bonferroni correction for two comparisons (uncorrected p = 0.05; corrected p = 0.025).
Intracranial stenosis study
Patients with flow-limiting IC stenosis of at least one major IC vessel (e.g., middle cerebral artery, MCA; posterior cerebral artery, PCA; anterior cerebral artery, ACA; or intracranial segments of the internal carotid artery, ICA) received an identical HH protocol as in the healthy volunteer study outlined above.
Data were collected and managed using REDCap electronic data capture tools (16). Stenoses were measured by board-certified neuroradiologist (MKS; experience = 11 years) from clinically acquired computerized tomography angiography (CTA), digital subtraction angiography (DSA), or magnetic resonance angiography (MRA) according to criteria in Samuels et al. (43) for IC stenosis, and according to the North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria in the case of extracranial stenosis (44). Inclusion criteria were that patients had intracranial stenosis greater than 50%. The T1a,HH correction of the CBF HH patient data was performed using the T1a,HH estimated from the healthy volunteers. CBF data were averaged for each condition (RA, T1a,HH corrected HH and uncorrected HH), and CBF values were compared (corrected HH vs RA; corrected HH vs uncorrected HH) using two-tailed Student’s t-tests with Bonferroni correction for two comparisons (uncorrected p = 0.05; corrected p = 0.025).
Results
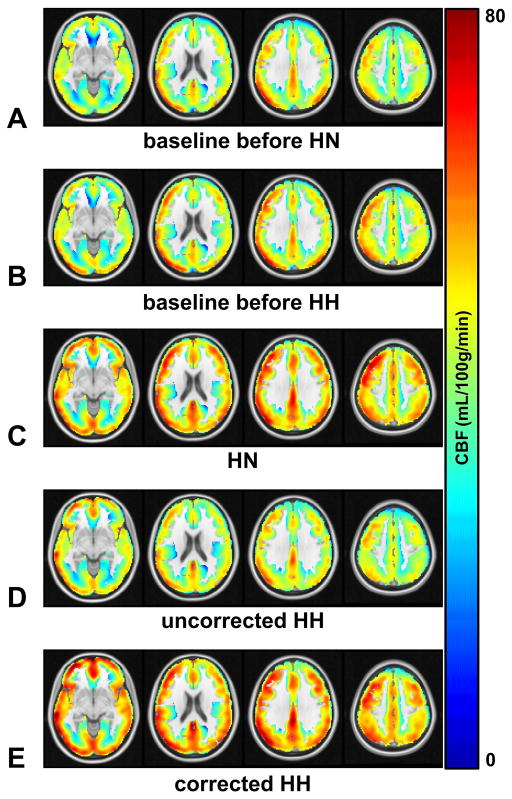
In healthy controls (Figure 1B) cortical CBF values for RA conditions before HN (mean±s.d. = 40.9 ± 6.1 ml/100g/min) and before HH (mean±s.d. = 42.3 ± 7.7 ml/100g/min) did not significantly differ (p = 0.17). As expected by the current approach for computing the T1a,HH values, the corrected CBF values for the HH condition (mean±s.d. = 49.3 ± 9.5 ml/100g/min) did not significantly differ from the CBF values for the HN condition (mean±s.d. = 47.7 ± 8.2 ml/100g/min; p = 0.25). Similarly, a significant correlation was found between corrected ΔCBFHH and ΔCBFHN (Pearson R2 = 0.51, p = 0.0046). No significant difference was found between end-tidal CO2 changes (p = 0.17, two-tailed paired Student’s t-test) for the HN and HH condition between subjects (mean ± s.d. ΔEtCO2 = 6.8 ± 2.0 and 5.6 ± 3.4 mmHg for the HN and HH condition respectively). Note that the uncorrected HH CBF (mean±s.d. = 41.8 ± 8.2 ml/100g/min) was not significantly different (p = 0.67) from the RA condition, demonstrating that the T1a,HH has a large effect on CBF quantification. Group CBF maps for healthy volunteers are shown in Figure 2.
Figure 2.
Mean CBF maps (ml/100g tissue/min) for healthy participants during (A) baseline before 5%CO2 in air (HN), (B) baseline before carbogen-5 (HH), (C) 5%CO2 in air (HN), (D) uncorrected carbogen-5 (HH), T1a,HH = T1a,RA = 1.65s, and (E) corrected carbogen-5 (HH), calculated T1a,HH = 1.49s.
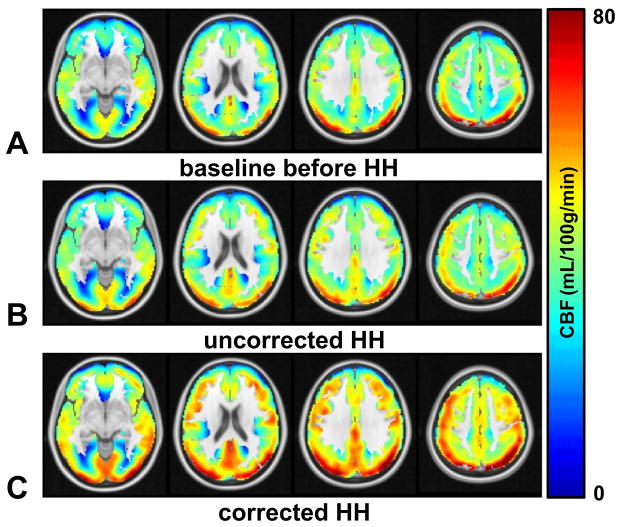
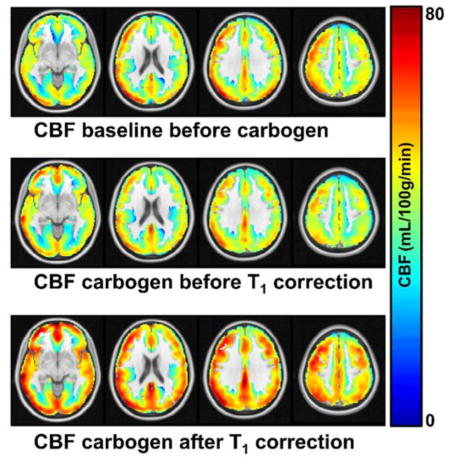
In patients (Figure 1C, Table 1), the corrected HH CBF values (mean±s.d.= 45.2 ± 13.9 ml/100g/min) did significantly differ (p < 0.005) from both the RA condition (mean±s.d.= 36.6 ± 8.2 ml/100g/min) and the uncorrected HH condition (mean±s.d.= 38.4 ± 11.8 ml/100g/min). Note that the uncorrected HH and RA CBF values did not significantly differ (p = 0.32). Group CBF maps for patients are shown in Figure 3.
Table 1.
Summary of All Data from Patients
| Patient ID | Age (yrs) | Sex | Stenosis Location (% stenosis) | Room Air CBF (ml/100g tissue/min) | Carbogen-5 CBF (ml/100g tissue/min) Uncorrected (T1a = 1.65s) | Carbogen-5 CBF (ml/100g tissue/min) Corrected (T1a = 1.49s) |
|---|---|---|---|---|---|---|
| 1 | 72 | M | Right Paraclinoid ICA (53%); Right IC vertebral (67%) | 48.1 ± 19.5 | 52.1 ± 22.2 | 61.4 ± 26.2 |
| 2 | 66 | M | Right MCA (28%); Left MCA (59%); Right IC vertebral (57%) | 32.2 ± 15.7 | 34.8 ± 16.5 | 41.0 ± 19.5 |
| 3 | 82 | F | Left MCA (33%); Right MCA (65%) | 26.4 ± 15.3 | 31.1 ± 14.6 | 36.7 ± 17.3 |
| 4 | 64 | M | Left Paraclinoid ICA (33%); Right cervical vertebral (68%) | 31.0 ± 10.5 | 27.7 ± 10.9 | 32.6 ± 12.8 |
| 5 | 72 | F | Right MCA (67%) | 35.3 ± 12.4 | 37.1 ± 13.0 | 43.8 ± 15.4 |
| 6 | 73 | F | Right MCA (73%); Left MCA (46%) | 44.6 ± 14.4 | 42.8 ± 17.1 | 50.3 ± 20.2 |
| 7 | 38 | F | Left MCA (68%) | 49.7 ± 21.1 | 64.1 ± 25.4 | 75.6 ± 30.1 |
| 8 | 62 | M | Left ICA (100%); Right cervical vertebral (80%) | 30.9 ± 18.2 | 26.5 ± 15.4 | 31.2 ± 18.1 |
| 9 | 51 | M | Right MCA (79%) | 29.4 ± 11.5 | 30.1 ± 11.5 | 35.5 ± 13.6 |
| 10 | 69 | M | Right MCA (99%); Right ICA (99%); Right cervical vertebral (76%) | 38.6 ± 13.0 | 37.4 ± 13.9 | 44.0 ± 16.3 |
|
| ||||||
| Mean | 61.4±13.3 | 36.6 ± 8.3 | 38.4 ± 11.8 | 45.2 ± 13.9 | ||
Figure 3.
Mean CBF maps (ml/100g tissue/min) for patients during (A) baseline before carbogen-5 (HH), (B) uncorrected carbogen-5 (HH), T1a,HH = T1a,RA = 1.65s, and (C) corrected carbogen-5 (HH), calculated T1a,HH = 1.49s. Owing to multiple vessels with steno-occlusive disease, patients have not been oriented by flow-limiting hemisphere.
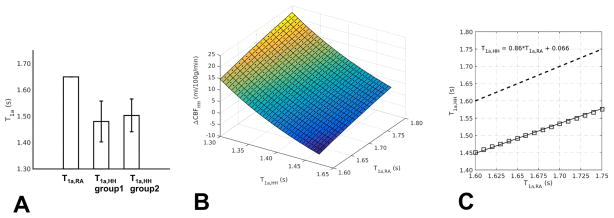
The mean T1a,HH value (Figure 4A) calculated in the HH condition across both groups was 1.49 ± 0.07s (with mean±s.d 1.48 ± 0.08s and 1.50 ± 0.06s for group 1 and group 2, respectively). The T1a,HH value between the two groups did not differ significantly (p = 0.6). The dependency of ΔCBFHH (CBFHH – CBFRA) is well approximated by a quadratic decreasing function with respect to T1a,HH and a quadratically increasing function with respect to assumed normoxic T1a,RA (Figure 4B). The reduction of the calculated T1a,HH for different assumed normoxic T1a,RA is fairly constant; a mean±s.d. T1 reduction of 162 ± 8ms across a range, 1.60 – 1.75s, of T1a,RA values was computed (Figure 4C).
Figure 4.
T1a,HH calculation results. (A) Reduced T1a,HH was found for both groups as compared to the normoxic condition (left bar, T1a,RA = 1.65s); 1.48s and 1.50s for group 1 and group 2, respectively, yielding a combined result of T1a,HH = 1.49s. No significant difference in T1a,HH was found between group 1 and group 2. Error bars denote the s.d. (B) Dependency of ΔCBFHH (CBFHH – CBFRA) for different calculated hyperoxic T1a,HH and assumed normoxic T1a,RA values. (C) Dependency of the calculated T1a,HH for different assumed normoxic T1a,RA values.
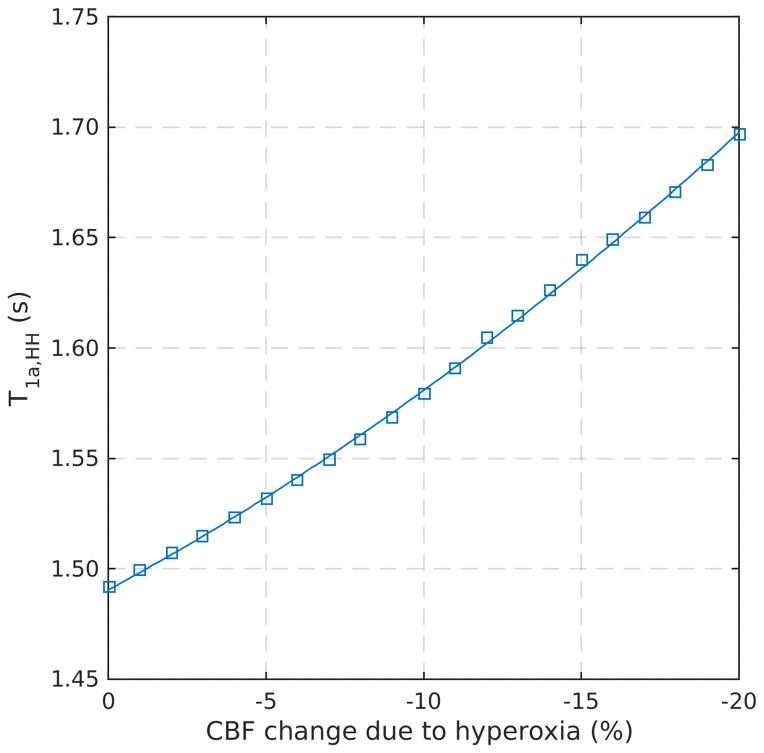
Figure 5 shows how the T1a,HH would change if the hyperoxic component of the HH mixture had a small-to-moderate (0 – 20%) vasoconstrictive effect on reducing baseline CBF. To completely attribute the reduced CBF in the HH condition to vasoconstrictive effects, thus no hyperoxic T1 effect (T1a,HH = T1a,RA = 1.65s), a ~16% CBF reduction is necessary. This is approximately the same percentage difference between the uncorrected and corrected HH CBF values (Figure 1B), as expected.
Figure 5.
Simulation demonstrating the effect of small hyperoxic-induced vasoconstriction (0 – 20% CBF reduction) on the arterial blood T1a,HH calculations. Note that for 0% CBF reduction due to hyperoxia the calculated T1a,HH = 1.49s as shown in Figure 4A. For larger potential vasoconstrictive effects due to hyperoxia (more CBF reduction) the calculated T1a,HH will increase accordingly. For a CBF reduction of ~16% the T1a,HH approaches the normoxic value T1a,RA = 1.65s, which is the same percentage difference between the corrected and uncorrected carbogen-5 (HH) CBF values in Figure 1A as expected.
Discussion
The overall finding from this work is that carbogen-5 (hypercapnic hyperoxia, HH) results in a T1a,HH of approximately 1.49s in humans, relative to a normoxic baseline T1a,RA of 1.65s. This value may be useful for quantitative ASL experiments that implement hyperoxic gas challenges such as the recently proposed calibrated BOLD model using hybrid gas challenges (8). Also other functional imaging approaches using hyperoxic gas challenges, such as vascular space occupancy (VASO) MRI (34) will benefit from accurate knowledge of T1a,HH to more precise blood nulling. The T1a,HH results presented in this work are valid for hypercapnic gas mixtures containing 95% O2 content. As previous ex-vivo studies have shown a linear dependency of R1,a = 1/T1,a with O2 concentration (pO2) (11,12), we suggest that extra- and interpolation of our results can be used for other amounts of O2 content.
Not surprisingly, subject variability of the T1a,HH value was observed. Our fitting approach is likely affected by the relatively large spatial resolution which can introduce partial volume effects between white and gray matter, CSF, and vascular compartment (e.g., arteriole vs. venules), and as such different voxels are anticipated to respond differently to vasoactive stimuli. However this bias is similar between all subjects in both groups studied as evidenced by the relatively similar calculated T1a,HH between subjects of the two groups (Figure 4A).
Analysis of the patient data supports the clinical feasibility of using hyperoxic gas challenges with ASL sequences, even in patients with known steno-occlusive disease. It is well-known that CBF increases after carbogen-5 (HH) administration (6,33). This change is only present when incorporating appropriate T1a,HH values in the quantification model (Figure 3). Due to the complicated nature of CBF in patients with atherosclerosis and the heterogeneity of stenosis locations in this patient group, changes in CBF across affected and unaffected regions were not evaluated. With a larger patient cohort, CBF reactivity comparisons across affected and unaffected regions could be of interest for future research.
A confounding factor of the analysis could be the interplay of hypercapnia and hyperoxia (vasodilation vs. vasoconstriction) and the resulting influence on CBF, as we assume here that short durations of hyperoxia have a negligible effect on CBF relative to the accuracy of the ASL measurement and relative to hypercapnia. The effect of hyperoxia on CBF remains a controversial topic as contradicting results have been reported (15,22,36,37,45–47) and thus it becomes difficult to confidently argue that there is indeed a small-to-negligible effect on CBF. Reasons for a reduction in CBF are a potential direct vasoconstrictive effect of O2 and hyperventilation (increased expired ventilation volume per minute) that causes PaCO2 to decrease (22). Several ASL-based studies have observed a slight reduction in CBF when breathing hyperoxic gasses (on the order of 2–10% reduction upon 5–12 min. of 100% O2) (15,29,37,45). For instance, a very small CBF decrease (~2% for gray matter) was reported using ASL at 1.5T, however this was not significantly different from zero (37) when using a corrected T1a,HH measured in non-cerebral body regions(18,21). Other ASL studies did find a significant decrease in CBF of ~10% at 3T (15) and ~30% at 1.5 T (22). The latter study however used a fixed T1a for both room air and hyperoxic conditions. Independent [15O]-H2O PET work in humans has revealed a non-significant but trending decrease in CBF during much longer durations (10 min) of hyperoxia (100% O2) for healthy volunteers of about 3 mL/100g tissue/min, and non-significant mean CBF changes in steno-occlusive patients (33). Phase-contrast based MRI studies also reported a slight CBF reduction during hyperoxia (46,47), however a correction for the confounding decrease in PaCO2 due to hyperventilation of hyperoxia was not performed. A more recent phase-contrast MRI study by Xu et al. did correct for PaCO2 changes during hyperoxia which resulted in a non-significant CBF decrease (36). In this study, to accommodate any possible CBF changes of hyperoxia, we therefore computed the T1a,HH for a range of simulated hyperoxia induced CBF changes. Figure 5 demonstrates how the calculation of T1a,HH would change if transient hyperoxia reduced CBF. The T1a,HH value calculated here (1.49s at 95%O2, assuming a normoxic T1a,RA of 1.65s) may be underestimated if hyperoxia leads to substantial CBF decreases. In general, more work is needed to elucidate the effect of hyperoxia on cerebral blood flow using either stable direct T1a measurements or T1 independent methods such as phase-contrast MRI or PET. Dynamic susceptibility contrast MRI using a multi-echo readout to isolate T2* changes might also be an option, however, this would require injection of an exogenous contrast agent (gadolinium). Of importance is also to study the effect of the O2 content amount and stimulus duration in order to give an exemplar for an optimal hyperoxic-stimulus protocol where hyperoxic induced CBF changes are minimal.
Another confound is that our approach relies on the single-compartment kinetic model (41). Here a single T1 value (arterial blood with a single PaO2 value) is used to describe the ASL signal in a voxel, and it assumes that the blood-tissue water exchange is almost instantaneous. A more likely scenario is that the labeled blood experiences a range of PaO2 values and may even reach the more venous side in the capillary bed. Therefore, a continuum of T1a values is experienced which should ideally be incorporated in the ASL signal model. Furthermore, bolus arrival times are regionally dependent and, like the pCASL labelling efficiency, dependent on hypercapnic state (26,48). This will also affect the CBF quantification and the continuum of T1a values the blood experiences in the cerebral vasculature. Another matter is the complex biochemistry of carbogen as it affects both the O2 and CO2 hemoglobin dissociation curves through the Bohr and Haldane effects (25). Hyperoxia will facilitate CO2 unloading (Haldane effect), thus increasing local PaCO2, whereas hypercapnia will facilitate O2 unloading (Bohr effect), thus increasing local PaO2. However, due to the combined hypercapnic and hyperoxic state it is not unlikely that the Bohr and Haldane effects are partially negated. For example, the increased hemoglobin O2 unloading due to hypercapnia (Bohr effect) can be partially restored by the increased PaO2 due to hyperoxia, and vice versa for the Haldane effect. These effects have recently been simulated by Faraco et al (49).
In conclusion, while the calculated T1a,HH could be adjusted for slight vasoconstrictive effects of hyperoxia, this value is slightly longer than previously computed T1a,HH values at 3T using extrapolation (~1.38s) (15) and ex vivo estimation using bovine blood (~1.45s, for 95% O2) (11), and therefore suggests a slower recovery of the labelled blood under hyperoxic conditions than may have been assumed previously. Only after incorporating the adjusted T1a,HH value in a ASL CBF quantification model, hypercapnic induced CBF changes were observed in patients with known steno-occlusive disease. This shows the feasibility of using hypercapnic-hyperoxic gas mixtures in ASL-based CBF studies. The T1a,HH value reported here (in-vivo at 3T for 95% O2) together with a ‘calibration curve’ for different assumed normoxic T1a and vasoconstrictive effects can be of significance for future studies. More work, however, is warranted to thoroughly characterize the dependence of CBF changes for different hyperoxic stimulation durations and inspired O2 content. The T1a,HH value calculated here should provide a reference for future calibrated BOLD fMRI, VASO and ASL-based CVR experiments using hyperoxic gas mixtures.
Acknowledgments
Funding: The authors would like to thank Dave Pennel, Lindsey Dethrage, Leslie McIntosh, Kristen George-Durrett, Paul Clemmons, and Diane Brown for experimental support, as well as the National Institute of Neurological Disorders and Stroke (NINDS) for funding (NIH/NINDS 5RO1NS078828) and the American Heart Association (14CSA20380466). Jeroen Hendrikse was supported by European Research Council (ERC) grant number: ERC-2014-StG - 637024_HEARTOFSTROKE.
List of Abbreviations
- ΔM
difference magnetization
- ACA
anterior cerebral artery
- ASL
arterial spin labeling
- BOLD
blood oxygenation level-dependent
- CBF
cerebral blood flow
- CBV
cerebral blood volume
- CTA
computerized tomography angiography
- CVR
cerebrovascular reactivity
- DSA
digital subtraction angiography
- EtCO2
end-tidal CO2
- FLIRT
FMRIB’s Linear Image Registration Tool
- FMRIB
Functional MRI of the Brain Centre
- FSL
FMRIB Software Library
- Hct
Hematocrit
- HH
hypercapnic hyperoxia
- HN
hypercapnic normoxia
- IC
intracranial
- ICA
internal carotid artery
- ISMRM
International Society for Magnetic Resonance in Medicine
- MCA
middle cerebral artery
- MNI
Montreal Neurological Institute
- MRA
magnetic resonance angiography
- NASCET
North American Symptomatic Carotid Endarterectomy Trial
- PaO2
arterial partial pressure of oxygen
- PCA
posterior cerebral artery
- pCASL
pseudo-continuous arterial spin labeling
- PET
positron emission tomography
- PLD
post-labeling delay
- pO2
partial pressure of oxygen
- PvO2
partial pressure of venous oxygen
- RA
room air
- SNR
signal to noise ratio
- VASO
vascular space occupancy
- Ya
arterial oxygen saturation fraction
- Yv
venous oxygen saturation fraction
Footnotes
Declaration of conflict of interest: The authors declare that no conflict of interest exists
References
- 1.Ashkanian M, Borghammer P, Gjedde A, Østergaard L, Vafaee M. Improvement of brain tissue oxygenation by inhalation of carbogen. Neuroscience. 2008;156:932–938. doi: 10.1016/j.neuroscience.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 2.Ito H, Kanno I, Ibaraki M, Hatazawa J, Miura S. Changes in human cerebral blood flow and cerebral blood volume during hypercapnia and hypocapnia measured by positron emission tomography. J Cereb Blood Flow Metab. 2003;23:665–70. doi: 10.1097/01.WCB.0000067721.64998.F5. [DOI] [PubMed] [Google Scholar]
- 3.Wise RG, Harris AD, Stone AJ, Murphy K. Measurement of OEF and absolute CMRO2: MRI-based methods using interleaved and combined hypercapnia and hyperoxia. In. Neuroimage. 2013:135–147. doi: 10.1016/j.neuroimage.2013.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blockley NP, Griffeth VEM, Simon AB, Buxton RB. A review of calibrated blood oxygenation level-dependent ( BOLD ) methods for the measurement of task-induced changes in brain oxygen metabolism. 2012 doi: 10.1002/nbm.2847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donahue MJ, Dethrage LM, Faraco CC, Jordan LC, Clemmons P, Singer R, Mocco J, Shyr Y, Desai A, O’Duffy A, Riebau D, Hermann L, Connors J, Kirshner H, Strother MK. Routine clinical evaluation of cerebrovascular reserve capacity using carbogen in patients with intracranial stenosis. Stroke. 2014;45:2335–41. doi: 10.1161/STROKEAHA.114.005975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donahue MJ, Ayad M, Moore R, van Osch M, Singer R, Clemmons P, Strother M. Relationships between hypercarbic reactivity, cerebral blood flow, and arterial circulation times in patients with moyamoya disease. J Magn Reson Imaging. 2013;38:1129–39. doi: 10.1002/jmri.24070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jane Taylor N, Baddeley H, Goodchild KA, Powell MEB, Thoumine M, Culver LA, James Stirling J, Saunders MI, Hoskin PJ, Phillips H, Padhani AR, Griffiths JR. BOLD MRI of human tumor oxygenation during carbogen breathing. J Magn Reson Imaging. 2001;14:156–163. doi: 10.1002/jmri.1166. [DOI] [PubMed] [Google Scholar]
- 8.Gauthier CJ, Hoge RD. A generalized procedure for calibrated MRI incorporating hyperoxia and hypercapnia. Hum Brain Mapp. 2013;34:1053–1069. doi: 10.1002/hbm.21495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams DS, Detre JA, Leigh JS, Koretsky AP. Magnetic resonance imaging of perfusion using spin inversion of arterial water. Proc Natl Acad Sci U S A. 1992;89:212–216. doi: 10.1073/pnas.89.1.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lu H, Clingman C, Golay X, van Zijl PCM. Determining the longitudinal relaxation time (T1) of blood at 3.0 Tesla. Magn Reson Med. 2004;52:679–82. doi: 10.1002/mrm.20178. [DOI] [PubMed] [Google Scholar]
- 11.Ma Y, Berman AJL, Pike GB. The Effect of Dissolved Oxygen on Relaxation Rates of Blood Plasma. Proceedings 22nd Scientific Meeting International Society for Magnetic Resonance in Medicine; 2014; p. 3099. [Google Scholar]
- 12.Silvennoinen MJ, Kettunen MI, Kauppinen Ra. Effects of hematocrit and oxygen saturation level on blood spin-lattice relaxation. Magn Reson Med. 2003;49:568–71. doi: 10.1002/mrm.10370. [DOI] [PubMed] [Google Scholar]
- 13.Grgac K, van Zijl PCM, Qin Q. Hematocrit and oxygenation dependence of blood (1)H(2)O T(1) at 7 Tesla. Magn Reson Med. 2013;70:1153–9. doi: 10.1002/mrm.24547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.d’Othée B, Rachmuth G, Munasinghe J, Lang E. The effect of hyperoxygenation on T1 relaxation time in vitro 1. Acad Radiol. 2003 doi: 10.1016/s1076-6332(03)00004-7. [DOI] [PubMed] [Google Scholar]
- 15.Bulte DP, Chiarelli Pa, Wise RG, Jezzard P. Cerebral perfusion response to hyperoxia. J Cereb Blood Flow Metab. 2007;27:69–75. doi: 10.1038/sj.jcbfm.9600319. [DOI] [PubMed] [Google Scholar]
- 16.Zhang X, Petersen ET, Ghariq E, De Vis JB, Webb AG, Teeuwisse WM, Hendrikse J, van Osch MJP. In vivo blood T(1) measurements at 1.5 T, 3 T, and 7 T. Magn Reson Med. 2013;70:1082–6. doi: 10.1002/mrm.24550. [DOI] [PubMed] [Google Scholar]
- 17.Varela M, Hajnal JV, Petersen ET, Golay X, Merchant N, Larkman DJ. A method for rapid in vivo measurement of blood T1. NMR Biomed. 2011;24:80–8. doi: 10.1002/nbm.1559. [DOI] [PubMed] [Google Scholar]
- 18.Tadamura E, Hatabu H, Li W, Prasad PV, Edelman RR. Effect of oxygen inhalation on relaxation times in various tissues. J Magn Reson Imaging. 1997;7:220–225. doi: 10.1002/jmri.1880070134. [DOI] [PubMed] [Google Scholar]
- 19.Shimada K, Nagasaka T. In vivo Measurement of Longitudinal Relaxation Time of Human Blood by Inversion-recovery Fast Gradient-echo MR Imaging at 3T. Magn Reson Med. 2012;11:265–271. doi: 10.2463/mrms.11.265. [DOI] [PubMed] [Google Scholar]
- 20.Heijtel DFR, Mutsaerts HJMM, Bakker E, Schober P, Stevens MF, Petersen ET, van Berckel BNM, Majoie CBLM, Booij J, van Osch MJP, Vanbavel E, Boellaard R, Lammertsma AA, Nederveen AJ. Accuracy and precision of pseudo-continuous arterial spin labeling perfusion during baseline and hypercapnia: a head-to-head comparison with 15O H2O positron emission tomography. Neuroimage. 2014;92:182–92. doi: 10.1016/j.neuroimage.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 21.Noseworthy MD, Kim JK, Stainsby Ja, Stanisz GJ, Wright Ga. Tracking oxygen effects on MR signal in blood and skeletal muscle during hyperoxia exposure. J Magn Reson Imaging. 1999;9:814–20. doi: 10.1002/(sici)1522-2586(199906)9:6<814::aid-jmri8>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 22.Floyd TF, Clark JM, Gelfand R, Detre JA, Ratcliffe S, Guvakov D, Lambertsen CJ, Eckenhoff RG. Independent cerebral vasoconstrictive effects of hyperoxia and accompanying arterial hypocapnia at 1 ATA. J Appl Physiol. 2003;95:2453–61. doi: 10.1152/japplphysiol.00303.2003. [DOI] [PubMed] [Google Scholar]
- 23.Sicard KM, Duong TQ. Effects of hypoxia, hyperoxia, and hypercapnia on baseline and stimulus-evoked BOLD, CBF, and CMRO2 in spontaneously breathing animals. Neuroimage. 2005;25:850–858. doi: 10.1016/j.neuroimage.2004.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pilkinton DT, Hiraki T, Detre JA, Greenberg JH, Reddy R. Absolute cerebral blood flow quantification with pulsed arterial spin labeling during hyperoxia corrected with the simultaneous measurement of the longitudinal relaxation time of arterial blood. Magn Reson Med. 2012;67:1556–65. doi: 10.1002/mrm.23137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hare HV, Germuska M, Kelly ME, Bulte DP. Comparison of CO2 in air versus carbogen for the measurement of cerebrovascular reactivity with magnetic resonance imaging. J Cereb Blood Flow Metab. 2013;33:1799–805. doi: 10.1038/jcbfm.2013.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Donahue MJ, Faraco CC, Strother MK, Chappell Ma, Rane S, Dethrage LM, Hendrikse J, Siero JCW. Bolus arrival time and cerebral blood flow responses to hypercarbia. J Cereb Blood Flow Metab. 2014;34:1243–52. doi: 10.1038/jcbfm.2014.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Langdon W, Donahue MJ, van der Kolk AG, Rane S, Strother MK. Correlating hemodynamic magnetic resonance imaging with high-field intracranial vessel wall imaging in stroke. J Radiol Case Rep. 2014;8:1–10. doi: 10.3941/jrcr.v8i6.1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Faraco CC, Strother MK, Dethrage LM, Jordan L, Singer R, Clemmons PF, Donahue MJ. Dual echo vessel-encoded ASL for simultaneous BOLD and CBF reactivity assessment in patients with ischemic cerebrovascular disease. Magn Reson Med. 2015;73:1579–92. doi: 10.1002/mrm.25268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chiarelli PA, Bulte DP, Wise R, Gallichan D, Jezzard P. A calibration method for quantitative BOLD fMRI based on hyperoxia. Neuroimage. 2007;37:808–20. doi: 10.1016/j.neuroimage.2007.05.033. [DOI] [PubMed] [Google Scholar]
- 30.Blockley NP, Griffeth VEM, Simon AB, Dubowitz DJ, Buxton RB. Calibrating the BOLD response without administering gases: Comparison of hypercapnia calibration with calibration using an asymmetric spin echo. Neuroimage. 2014 doi: 10.1016/j.neuroimage.2014.09.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Germuska M, Bulte DP. MRI measurement of oxygen extraction fraction, mean vessel size and cerebral blood volume using serial hyperoxia and hypercapnia. Neuroimage. 2014;92:132–42. doi: 10.1016/j.neuroimage.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 32.Frederick B, Tong Y, Strother MK, Nickerson L, Lindsey K, Donahue MJ. Derivation of flow information from a hypocarbia challenge study using time delay correlation processinge. Proc. ISMRM, 21st Annual Meeting; Salt Lake City. 2013; p. 206. [Google Scholar]
- 33.Ashkanian M, Gjedde A, Mouridsen K, Vafaee M, Hansen KV, Ostergaard L, Andersen G. Carbogen inhalation increases oxygen transport to hypoperfused brain tissue in patients with occlusive carotid artery disease: increased oxygen transport to hypoperfused brain. Brain Res. 2009;1304:90–5. doi: 10.1016/j.brainres.2009.09.076. [DOI] [PubMed] [Google Scholar]
- 34.Lu H, Golay X, Pekar JJ, Van Zijl PCM. Functional magnetic resonance imaging based on changes in vascular space occupancy. Magn Reson Med. 2003;50:263–274. doi: 10.1002/mrm.10519. [DOI] [PubMed] [Google Scholar]
- 35.Donahue MJ, van Laar PJ, van Zijl PCM, Stevens RD, Hendrikse J. Vascular space occupancy (VASO) cerebral blood volume-weighted MRI identifies hemodynamic impairment in patients with carotid artery disease. J Magn Reson Imaging. 2009;29:718–724. doi: 10.1002/jmri.21667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu F, Liu P, Pascual JM, Xiao G, Lu H. Effect of hypoxia and hyperoxia on cerebral blood flow, blood oxygenation, and oxidative metabolism. J Cereb Blood Flow Metab. 2012;32:1909–18. doi: 10.1038/jcbfm.2012.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zaharchuk G, Martin AJ, Dillon WP. Noninvasive imaging of quantitative cerebral blood flow changes during 100% oxygen inhalation using arterial spin-labeling MR imaging. AJNR Am J Neuroradiol. 2008;29:663–7. doi: 10.3174/ajnr.A0896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Donahue MJ, Strother MK, Hendrikse J. Novel MRI approaches for assessing cerebral hemodynamics in ischemic cerebrovascular disease. Stroke. 2012;43:903–915. doi: 10.1161/STROKEAHA.111.635995. [DOI] [PubMed] [Google Scholar]
- 39.MacIntosh BJ, Lindsay AC, Kylintireas I, Kuker W, Günther M, Robson MD, Kennedy J, Choudhury RP, Jezzard P. Multiple inflow pulsed arterial spin-labeling reveals delays in the arterial arrival time in minor stroke and transient ischemic attack. Am J Neuroradiol. 2010;31:1892–1894. doi: 10.3174/ajnr.A2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jenkinson M, Smith S. A global optimisation method for robust affine registration of brain images. Med Image Anal. 2001;5:143–156. doi: 10.1016/s1361-8415(01)00036-6. [DOI] [PubMed] [Google Scholar]
- 41.Alsop DC, Detre JA, Golay X, Günther M, Hendrikse J, Hernandez-Garcia L, Lu H, Macintosh BJ, Parkes LM, Smits M, van Osch MJP, Wang DJJ, Wong EC, Zaharchuk G. Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the european consortium for ASL in dementia. Magn Reson Med. 2015;73:102–116. doi: 10.1002/mrm.25197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Van Osch MJP, Teeuwisse WM, van Walderveen MAA, Hendrikse J, Kies DA, van Buchem MA. Can arterial spin labeling detect white matter perfusion signal? Magn Reson Med. 2009;62:165–73. doi: 10.1002/mrm.22002. [DOI] [PubMed] [Google Scholar]
- 43.Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. AJNR Am J Neuroradiol. 2000;21:643–646. [PMC free article] [PubMed] [Google Scholar]
- 44.Taylor DW, Whisnant JP Collaborators NAS ic CET. Beneficial Effect of Carotid Endarterectomy in Symptomatic Patients with High-Grade Stenosis. N Engl J Med. 1991;115:34. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- 45.Haddock B, Larsson HBW, Hansen AE, Rostrup E. Measurement of brain oxygenation changes using dynamic T(1)-weighted imaging. Neuroimage. 2013;78:7–15. doi: 10.1016/j.neuroimage.2013.03.068. [DOI] [PubMed] [Google Scholar]
- 46.Rostrup E, Larsson HBW, Toft PB, Garde K, Henriksen O. Signal changes in gradient echo images of human brain induced by hypo- and hyperoxia. NMR Biomed. 1995;8:41–47. doi: 10.1002/nbm.1940080109. [DOI] [PubMed] [Google Scholar]
- 47.Watson NA, Beards SC, Altaf N, Kassner A, Jackson A. The effect of hyperoxia on cerebral blood flow: a study in healthy volunteers using magnetic resonance phase-contrast angiography. Eur J Anaesthesiol. 2000;17:152–9. doi: 10.1046/j.1365-2346.2000.00640.x. [DOI] [PubMed] [Google Scholar]
- 48.Aslan S, Xu F, Wang PL, Uh J, Yezhuvath US, van Osch M, Lu H. Estimation of labeling efficiency in pseudocontinuous arterial spin labeling. Magn Reson Med. 2010;63:765–71. doi: 10.1002/mrm.22245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Faraco CC, Strother MK, Siero JC, Arteaga DF, Scott AO, Jordan LC, Donahue MJ. The cumulative influence of hyperoxia and hypercapnia on blood oxygenation and R2(.) J Cereb Blood Flow Metab. 2015 doi: 10.1038/jcbfm.2015.168. [DOI] [PMC free article] [PubMed] [Google Scholar]