Abstract
Different clones of methicillin-susceptible (MSSA) and methicillin-resistant (MRSA) Staphylococcus aureus have been found in humans as well as in animals and retail meat. However, more information about the genetic characteristics and similarities between strains is needed. The aim of this study was to identify and characterize Staphylococcus aureus from humans, and to compare their characteristics with isolates of animal origin. A total of 550 nasal swabs were taken from healthy humans, and S. aureus was isolated and identified. Positive S. aureus isolates were subjected to molecular typing and susceptibility testing. In addition, 108 MRSA isolates recovered from clinical patients in the state of North Dakota and 133 S. aureus isolates from animals and meat previously analyzed were included. The nasal carriage of S. aureus in healthy people was 7.6% and, in general, clones were genetically diverse. None of the S. aureus strains obtained from healthy people were mecA- or PVL-positive. A total of 105 (97.2%) MRSA isolates from clinical cases harbored the mecA gene and 11 (10.2%) isolated from blood stream infections harbored the PVL gene. The most common resistance profile among S. aureus from healthy people was penicillin, and from clinical cases were erythromycin-penicillin-ciprofloxacin. The rate of multidrug resistance (MDR) was 70% in humans. Most of the S. aureus harboring mecA and PVL genes were identified as ST5 and ST8, and exhibited MDR. However, S. aureus isolates of animal origin used for comparison exhibited a lower rate of MDR. The most common resistance profiles in isolates of animal origin were penicillin-tetracycline and penicillin-tetracycline-erythromycin, in animals and raw meat, respectively. The ST5 was also found in animals and meat, with ST9 and ST398 being the major clones. The genetic similarity between clones from humans and meat suggests the risk of spread of S. aureus in the food chain.
Introduction
In the last few decades, many bacterial species have developed resistance to antimicrobial agents that have been commonly used to treat them [1]. Staphylococcus aureus is one of the pathogens known to rapidly develop resistance to antimicrobial agents as new antibiotics are introduced [2]. Within a couple years after the introduction of penicillin to clinical medicine, the first penicillin-resistant S. aureus was discovered. The first methicillin-resistant S. aureus (MRSA) strains were identified from clinical specimens in 1961; two years after methicillin was introduced as an antibiotic [3, 4].
Methicillin-resistant S. aureus has been implicated in community-associated (CA-MRSA), healthcare-associated (HA-MRSA), and livestock-associated (LA-MRSA) infections worldwide. In the United States, the nasal carriage of S. aureus in humans was 29% (78.9 million people) and that of MRSA approximately 1.5% (4.1 million people) in 2003–2004 [5]. In 2005, there were an estimated 478,000 hospitalizations that corresponded to S. aureus infections, approximately 278,000 of those were attributed to MRSA [6]. In addition, an invasive MRSA infection was developed by about 94,000 people, leading to 19,000 deaths. The distribution of these infections were approximately 86% HA-MRSA and 14% CA-MRSA [7]. However, HA-MRSA clones have been progressively replaced by CA-MRSA strains due to the expanding community reservoir and the increasing influx into the hospital of individuals who harbor CA-MRSA [8, 9].
Meat-producing animals have also been identified as carriers of MRSA [10–12]. Moreover, it has been found that retail meat can also be contaminated with MRSA [13–15]. These findings have increased the concern that food may serve as a vehicle for transmission of MRSA to the human population [16].
Resistance to methicillin in S. aureus is primarily mediated by the mecA gene, which encodes the low-affinity penicillin-binding protein 2a (PBP2a) [17, 18]. Recently, a novel mecA homolog gene (mecA LGA251 re-named mecC) has been detected in S. aureus strains from humans and livestock that were phenotypically resistant to methicillin but tested negative for the mecA gene. The mecC gene exhibits about 70% sequence homology to the mecA gene and is located on the staphylococcal cassette chromosome mec type XI (type-XI SCCmec) [19–22]. Among virulence factors, the Panton–Valentine leukocidin (PVL) exotoxin encoding gene has been associated with most CA-MRSA strains [23, 24] that cause severe skin infections and necrotizing pneumonia [25].
Different clones of methicillin-susceptible S. aureus (MSSA) and MRSA have been found in humans as well as in animals and retail meat. Typically, clones that cause CA-MRSA infections (USA300 and USA400) are different than those causing HA-MRSA infections (USA100 and USA200) [26]. Some sequence types (ST) associated to HA-MRSA have been identified including: ST5, ST8, ST22, ST36, ST45, among others [27]. The sequence types ST30 and ST80 have been associated with CA-MRSA [28] and ST398 has been linked with animals [10, 29]. The sequence types ST398 and ST9 have been detected in both animals (pigs) and meat (pork meat), with a genetic similarity between S. aureus strains from these different sources [15]. However, the clonal type ST398 has also been detected in human patients [10, 29].
The objective of this study was to identify and characterize Staphylococcus aureus isolated from humans, and to compare the molecular characteristics and antimicrobial susceptibility with S. aureus isolates from animals and meat.
Materials and Methods
Samples
A total of 550 nasal swab samples were obtained from undergraduate students enrolled in the Department of Veterinary and Microbiological Sciences, North Dakota State University, who were considered as healthy humans. Samples were obtained from plates used in class that were discarded at the end of the study, thus none of the isolates obtained were identifiable by traceback. Samples were collected in the fall semester of 2010 (n = 231) and in the spring semester of 2011 (n = 319). In addition, a total of 108 MRSA isolates recovered from clinical cases of MRSA affected by wound and blood stream infections (sepsis, bone, cerobrospinal fluid [CSF], synovial fluid, subdural fluid, tissue, leg ulcer and pleural fluid) were obtained from the North Dakota Department of Health (Bismarck, ND) in the summer of 2010.
A total of 133 S. aureus strains isolated from animals (pig, n = 30; sheep, n = 26; cattle, n = 2), raw meat (pork, n = 35; chicken, n = 25; beef, n = 9), and deli meat (ham, n = 4; chicken, n = 2) were used to compare the molecular characteristics and antimicrobial susceptibility with S. aureus isolates from humans. The S. aureus strains of animal origin were isolated and analyzed as previously described by Buyukcangaz et al. (2013) [15] (Tables 1 and 2).
Table 1. Source and characteristics of S. aureus isolates of animal origin used in the study.
| Source | S. aureus isolates | 16S rRNA | mecA | PVL |
|---|---|---|---|---|
| Animals | ----------No.---------- | ------------------------No.------------------------ | ||
| Sheep | 26 | 26 | 0 | 0 |
| Pig | 30 | 30 | 0 | 0 |
| Cattle | 2 | 2 | 0 | 0 |
| Total | 58 | 58 | 0 | 0 |
| Raw meat | ||||
| Pork | 35 | 35 | 5 | 0 |
| Chicken | 25 | 25 | 0 | 0 |
| Beef | 9 | 9 | 0 | 0 |
| Total | 69 | 69 | 5 | 0 |
| Deli meat | ||||
| Ham | 4 | 4 | 0 | 0 |
| Turkey | 0 | 0 | 0 | 0 |
| Chicken | 2 | 2 | 0 | 0 |
| Total | 6 | 6 | 0 | 0 |
Adapted from Buyukcangaz et al. (2013) [15].
Table 2. Antimicrobial resistance profiles of S. aureus isolates of animal origin used in this study.
| Antimicrobial resistance profile | Antimicrobial subclasses | Isolates | Source | Isolates |
|---|---|---|---|---|
| ----------No.---------- | --No.-- | -----------------No.----------------- | ||
| ERY-PEN-TET-GEN-CHL-CIP-QUI | 7 | 1 | Pork meat | 1 |
| ERY-PEN-TET-CHL-CIP-QUI | 6 | 1 | Pork meat | 1 |
| ERY-PEN-TET-CHL | 4 | 2 | Pig | 2 |
| ERY-PEN-TET-KAN | 4 | 1 | Pork meat | 1 |
| ERY-PEN-TET | 3 | 14 | Pork meat | 11 |
| 3 a | ||||
| PEN-TET-GEN | 3 | 1 | Sheep | 1 |
| PEN-TET-KAN | 3 | 1 | Pork meat | 1 a |
| PEN-TET-CHL | 3 | 1 | Pig | 1 |
| ERY-PEN | 2 | 4 | Pork meat | 3 |
| 1 a | ||||
| ERY-TET | 2 | 5 | Pork meat | 5 |
| PEN-TET | 2 | 39 | Pig | 19 |
| Sheep | 17 | |||
| Pork meat | 2 | |||
| Chicken meat | 1 | |||
| ERY | 1 | 4 | Chicken meat | 3 |
| Chicken deli meat | 1 | |||
| PEN | 1 | 21 | Pig | 7 |
| Sheep | 1 | |||
| Pork meat | 4 | |||
| Beef | 4 | |||
| Chicken meat | 3 | |||
| Ham | 2 | |||
| TET | 1 | 10 | Sheep | 6 |
| Pork meat | 3 | |||
| Chicken meat | 1 | |||
Ciprofloxacin (CIP); chloramphenicol (CHL); erythromycin (ERY); gentamicin (GEN); kanamycin (KAN); quinupristin/dalfopristin (QUI); penicillin (PEN); and tetracycline (TET).
a mecA positive.
Institutional Review Board (IRB) approval was sought for the human isolates and the study was considered exempt by NDSU IRB. Institutional Animal Care and Use Committee (IACUC) approval was used for the animal work as described previously [15].
Culture method
Nasal swabs were taken from healthy humans by using a sterile moistened swab inserted into the nostril, to a depth of approximately 1 cm, and rotated five times. For each subject, both nostrils were sampled using the same swab. Nasal swabs were inoculated onto mannitol salt agar (MSA) plates (Becton, Dickinson and Company [BD], Sparks, MD) and incubated at 37°C for 48 h. All colonies surrounded by yellow zones on MSA after incubation were selected. Colonies with pink or red zones on MSA were excluded.
All presumptive S. aureus colonies were confirmed by biochemical testing using Sensititre Gram Positive ID (GPID) plates (Sensititre®, TREK Diagnostic Systems Ltd., Cleveland, OH), according to the manufacturer's recommendations.
Staphylococcus aureus isolates from healthy humans, and MRSA isolates from clinical cases, were stored at -80°C in brain–heart infusion broth (BD) containing 20% glycerol until use.
Multiplex polymerase chain reaction (mPCR)
Staphylococcus aureus strains from healthy humans and from clinical cases stored at -80°C were recovered to trypticase soy agar (TSA) plates and incubated at 37°C for 18 to 24 h. The extraction of DNA was carried out by suspending one colony in 50 μL of DNase/RNase-free distilled water (Gibco Invitrogen, Grand Island, NY, USA), heating (99°C, 10 min) and centrifugation (30,000 × g, 1 min) to remove cellular debris. The remaining DNA was transferred to a new tube and stored at -20°C until use.
A multiplex PCR assay was used to detect: 16S rRNA (identification of S. aureus), mecA (associated with methicillin resistance) and PVL-encoding genes (virulence factor) (Table 3). Two microliters of the DNA template (described above) was added to a 50 μL final reaction mixture: 1X Go Taq® Reaction Buffer (pH 8.5), 1.25 U of Go Taq® DNA polymerase, 200 μM dNTP (Promega, Madison, WI, USA), and 1 μM of primers (16S rRNA, mecA, LukS/F-PV) (Integrated DNA Technologies, Inc., Coralville, IA, USA). The conditions of the PCR reactions were adjusted according to the protocol described by Makgotlho et al. (2009) [30] using a thermocycler (Eppendorf, Hamburg, Germany).
Table 3. Nucleotide sequence of the primers used for detection of 16S rRNA, mecA, Panton-Valentine leukocidin, mecA LGA251, arcC, aroE, glpF, gmk, pta, tpi, and yqiL genes.
| Primer | Oligonucleotide sequence | Amplicon Size (bp) |
|---|---|---|
| Staph 756 F | 5’-AACTCTGTTATTAGGGAAGAACA-3’ | 756 |
| Staph 750 R | 5’-CCACCTTCCTCCGGTTTGTCACC-3’ | |
| mecA 1 F | 5’-GTAGAAATGACTGAACGTCCGATAA-3’ | 310 |
| mecA-2 R | 5’-CCAATTCCACATTGTTTCGGTCTAA-3’ | |
| luk-PV-1 F | 5’-ATCATTAGGTAAAATGTCTGGACATGATCCA-3’ | 433 |
| luk-PV-2 R | 5’-GCATCAAGTGTATTGGATAGCAAAAGC-3’ | |
| mecA LGA251 FP | 5'-TCACCAGGTTCAAC[Y]CAAAA-3' | 356 |
| mecA LGA251 RP | 5'-CCTGAATC[W]GCTAATAATATTTC-3' | |
| mecA LGA251 MultiFP | 5'-GAAAAAAAGGCTTAGAACGCCTC-3' | 718 |
| mecA LGA251 RP | 5'-CCTGAATC[W]GCTAATAATATTTC-3' | |
| mecA LGA251 MultiFP | 5'-GAAAAAAAGGCTTAGAACGAATC-3' | 138 |
| mecA LGA251 MultiRP | 5'-GATCTTTTCCGTTTTCAGC-3' | |
| arcC F | 5'-TTGATTCACCAGCGCGTATTGTC-3' | 456 |
| arcC R | 5'-AGGTATCTGCTTCAATCAGCG-3' | |
| aroE F | 5'-ATCGGAAATCCTATTTCACATTC-3' | 456 |
| aroE R | 5'-GGTGTTGTATTAATAACGATATC-3' | |
| glpF F | 5'-CTAGGAACTGCAATCTTAATCC-3' | 465 |
| glpF R | 5'-TGGTAAAATCGCATGTCCAATTC-3' | |
| gmK F | 5'-ATCGTTTTATCGGGACCATC-3' | 429 |
| gmK R | 5'-TCATTAACTACAACGTAATCGTA-3' | |
| pta F | 5'-GTTAAAATCGTATTACCTGAAGG-3' | 474 |
| pta R | 5'-GACCCTTTTGTTGAAAAGCTTAA-3' | |
| tpi F | 5'-TCGTTCATTCTGAACGTCGTGAA3' | 402 |
| tpi R | 5'-TTTGCACCTTCTAACAATTGTAC-3' | |
| yqiL F | 5'-CAGCATACAGGACACCTATTGGC-3' | 516 |
| yqiL R | 5'-CGTTGAGGAATCGATACTGGAAC-3' |
The mPCR products (10 μL) were loaded into a 1.5% (wt/vol) agarose gel (Agarose ITM) using EzVision One loading dye (Amresco, Solon, OH, USA) and electrophoresis was carried out in 1X TAE buffer at 100 v for 1 h. A molecular weight marker 100-bp ladder (Promega, Madison, WI, USA) and a negative (DNase/RNase-free distilled water) and a positive control (S. aureus ATCC 33591; MRSA) were included on each gel. Bands corresponding to each gene were visualized using an Alpha Innotech UV imager (FluorChemTM).
All MRSA clinical isolates that were negative for the mecA gene by mPCR assay were subjected to the detection of the mecC gene (Table 3) by PCR according to the protocol described by Stegger et al. (2011) [31].
Pulsed-field gel electrophoresis (PFGE)
The PulseNet protocol with minor modifications was used [26]. Briefly, S. aureus strains were recovered from frozen stock to TSA plates and incubated at 37°C for 18 to 24 h. A single colony was inoculated onto a second TSA plate and incubated at 37°C for 18 to 24 h. Colonies were transferred to 5-mL polystyrene round-bottom tubes containing 2 mL of cell suspension buffer (100 mM Tris HCl [pH 8.0], Invitrogen; 100 mM EDTA [pH 8.0], Gibco), adjusting the cell concentrations to an absorbance of 0.9 to 1.1 using a spectrophotometer (Smart SpecTM plus, Bio-Rad Laboratories, USA) at 610 nm. The following steps (plug preparation, lysis, washing, and the SmaI enzyme restriction digestion) were performed according to the PulseNet protocol. Salmonella Branderup H9812 was used as a DNA marker [32].
The electrophoresis was carried out in a Chef Mapper (Bio-Rad Laboratories) PFGE rig, with an initial switch time of 5 s, a final switch time of 40 s, and a total running time of 17 h 45 min. The gels were stained with ethidium bromide (1.5 μg/mL), and then the macrorestriction patterns were visualized using a UVP imager (UVP, Upland, CA).
Macrorestriction patterns of Staphylococcus aureus isolates from humans, animals and meat were analyzed using the BioNumerics Fingerprinting software (Ver 6.6 Applied Math, Austin, TX). The similarity index was calculated using the Dice coefficient, a band position tolerance of 1%, and an optimization of 0.5%. The unweighted-pair group method with arithmetic mean algorithm (UPGMA) was used to construct a dendrogram, and clusters were selected using a cutoff at 80% level of genetic similarity [26].
Multilocus sequence typing (MLST)
After the construction of the dendrogram (PFGE) containing S. aureus, at least one human isolate from each cluster was selected as a representative of the group for MLST analysis. Strains of S. aureus from animals and meat were included for comparison and STs were obtained from previous work [15]. Sequencing of MLST PCR products of the selected human isolates was carried out at Iowa State University’s DNA Sequencing Facility (Ames, IA). Briefly, S. aureus isolates were struck to TSA plates and incubated at 37°C for 18 to 24 h. DNA extraction from cells was carried out using the boiling method as described above.
Internal fragments of the following seven housekeeping genes: arcC, aroE, glpF, gmk, pta, tpi, and yqiL were amplified (Table 3; S1 Data) [33]. All PCR reactions were carried out in 50-μL volumes: 1 μL of DNA template, Taq DNA polymerase (Promega) (1.25 U), 1X PCR buffer (Promega), primers (0.1 μM) (Integrated DNA Technologies, Inc.), and dNTPs (200 μM) (Promega). The PCR conditions were adjusted according to the protocol described by Enright et al. (2000) [33] using a thermocycler (Eppendorf). Ten microliters of the PCR products were loaded into 1% agarose gels in 1X TAE with EzVision One loading dye, and electrophoresis was run at 100 V in 1X TAE for 1 h. Images were captured using an Alpha Innotech imager.
The amplicon purification was carried out using the QIAquick® PCR Purification Kit (Qiagen, Valencia, CA) according to the manufacturer’s instructions. Purified PCR products were sequenced at Iowa State University’s DNA Facility (Ames, IA) using an Applied Biosystems 3730xl DNA Analyzer (Applied Biosystems, Foster City, CA). Sequence data were imported into DNAStar (Lasergene, Madison, WI), trimmed, and aligned to the control sequences (from the MLST site) and interrogated against the MLST database (http://saureus.mlst.net/). Sequence types of selected S. aureus isolates were added to the strain information for analysis in BioNumerics software.
Susceptibility testing
Staphylococcus aureus isolates were subjected to antimicrobial susceptibility testing using the broth microdilution method and the National Antimicrobial Resistance Monitoring System (NARMS) panels (CMV3AGPF, Sensititre®, Trek Diagnostics), according to the manufacturer’s and the Clinical Laboratory Standards Institute (2012) [34] guidelines. Antimicrobials in the panel and their resistance breakpoints were as follows: erythromycin (≥8 μg/mL), tetracycline (≥16 μg/mL), ciprofloxacin (≥4 μg/mL), chloramphenicol (≥32 μg/mL), penicillin (≥0.25 μg/mL), vancomycin (≥16 μg/mL), nitrofurantoin (≥128 μg/mL), gentamicin (≥16 μg/mL), quinupristin/dalfopristin (≥4 μg/mL), linezolid (≥8 μg/mL), kanamycin (≥64 μg/mL), and daptomycin (susceptible ≤1 μg/mL). Multidrug resistance (MDR) was considered as resistance to at least three classes of the antimicrobials tested [35] (S4 Data).
Results
The results for identification of S. aureus (16S rRNA), mecA and PVL genes in samples obtained from humans are shown in Table 4 and S2 Data & S3 Data. The prevalence of nasal carriage of S. aureus in healthy people was 7.6%. None of these isolates harbored the mecA or PVL genes. Clinical isolates were identified as MRSA strains in the hospital using standard microbiological procedures. As expected, all of these isolates were confirmed as S. aureus strains by the detection of 16S rRNA gene using the PCR assay. Among the 108 MRSA clinical isolates, a total of 105 (97.2%) harbored the mecA gene and 11 (10.2%) carried the PVL gene. Of interest, the PCR assay did not detect the PVL gene in MRSA strains isolated from clinical cases affected by wound infections.
Table 4. Identification of 16S rRNA, mecA and Panton-Valentine Leukocidin (PVL) genes in S. aureus from healthy people, and MRSA isolates from clinical cases.
| Source | Samples | Positive for S. aureus | Positive for MRSA | 16S rRNA | mecA | PVL |
|---|---|---|---|---|---|---|
| Healthy people | ---No.--- | -----No.----- | --No. (%)-- | ----------------No. (%)---------------- | ||
| Fall 2010 | 231 | 17 (7.4) | 17 (7.4) | 0 (0.0) | 0 (0.0) | |
| Spring 2011 | 319 | 25 (7.8) | 25 (7.8) | 0 (0.0) | 0 (0.0) | |
| Total | 550 | 42 (7.6) | 42 (7.6) | 0 (0.0) | 0 (0.0) | |
| Clinical cases | ||||||
| Blood | 99 | 99 (100) | 99 (100) | 99 (100) | 96 (97.0) | 11 (11.1) |
| Wound | 9 | 9 (100) | 9 (100) | 9 (100) | 9 (100) | 0 (0.0) |
| Total | 108 | 108 (100) | 108 (100) | 108 (100) | 105 (97.2) | 11 (10.2) |
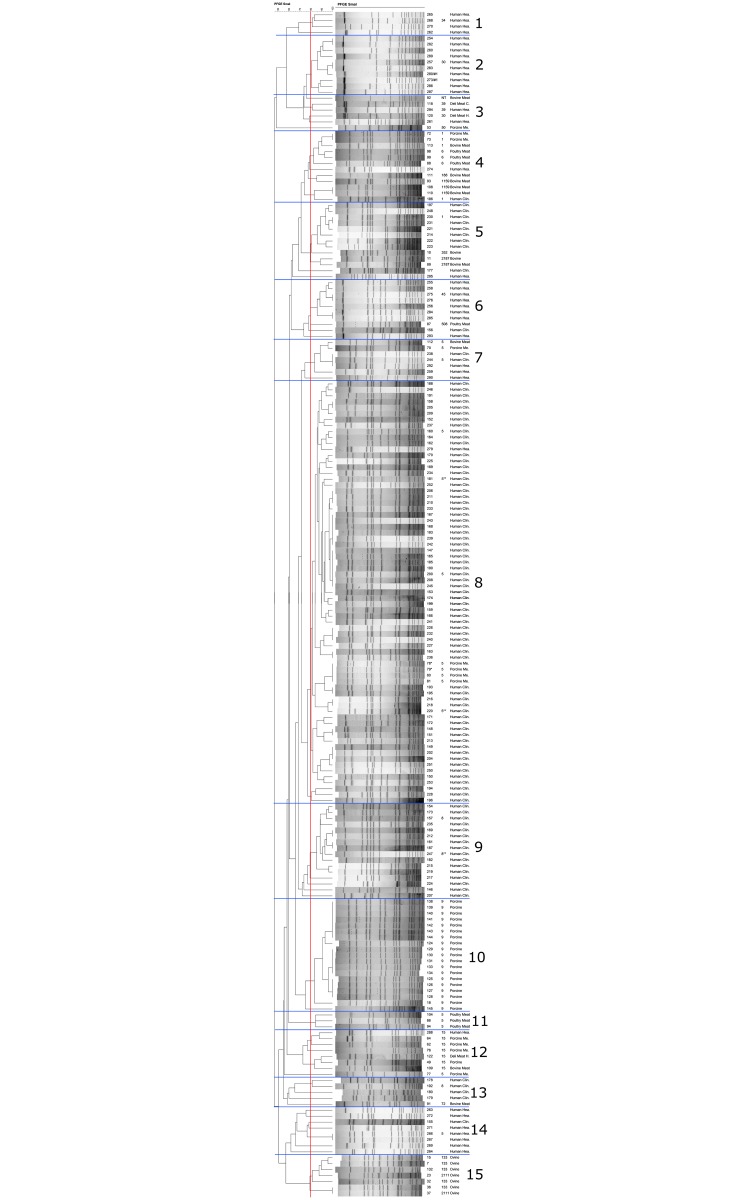
The genetic similarity between S. aureus strains isolated from humans and S. aureus strains of animal origin were analyzed using BioNumerics software. Fig 1 shows a dendrogram containing the macrorestriction patterns of S. aureus strains and the sequence type (ST) of some isolates from each cluster (S1 Data). Thirty-four S. aureus ST398 strains of animal origin were not included in the dendrogram as they failed to restrict. A total of fifteen clusters was observed, of which six were homogenous, containing one type of isolate exclusively from healthy humans (cluster 1 and 2), MRSA isolates from clinical cases (cluster 9), or isolates of animal origin (clusters 10, 11 and 15). In general, genetic diversity was observed among isolates from healthy humans, classified in different clusters with the sequence types: ST5, ST15, ST30, ST34, ST39 and ST45. Genetic similarity was observed between S. aureus strains from humans and meat: cluster 3 (ST39), cluster 4 (ST1), cluster 7 (ST5), and cluster 12 (ST15). In cluster 9, the genetic similarity between mecA-positive strains and one strain that did not harbor mecA nor mecC genes isolated from clinical cases, and were identified as ST8. In addition, two clinical isolates identified as MRSA ST5 that were mecA- and mecC-negative exhibited a genetic similarity with mecA-positive S. aureus ST5 strains isolated from humans and from pork meat (cluster 8).
Fig 1. Dendrogram showing the genetic similarity between S. aureus isolates from humans, and of animal origin.
The scale indicates levels of similarity with a vertical line indicating the cutoff (80% level of similarity), numbers represent the sample codes, followed on the right by the sequence type (ST) and the type of the sample. *mecA-positive S. aureus in pork meat. **mecA- and mecC-negative MRSA from clinical cases.
Among the antimicrobials tested using CLSI interpretation criteria [34], most MRSA isolates from clinical cases were resistant to erythromycin, penicillin and ciprofloxacin, and S. aureus isolates from healthy people exhibited resistance primarily to penicillin (Table 5, S4 Data). A rate of 70% of MDR strains was detected in humans, primarily among clinical isolates that were all identified as MRSA. In humans, one clinical isolate identified as MRSA was susceptible to all antimicrobial agents. The minimum inhibitory concentrations (MICs) of resistant S. aureus strains from humans are shown in Table 6. High MICs were observed in most of the penicillin-resistant S. aureus isolates from humans (8 - >16 μg/mL). The majority of ciprofloxacin-resistant S. aureus isolates from humans exhibited a MIC > 4 μg/mL.
Table 5. Antimicrobial resistance profiles of Staphylococcus aureus from healthy people, and methicillin-resistance Staphylococcus aureus (MRSA) isolates from clinical cases.
| Antimicrobial resistance profile | Antimicrobial subclasses | Samples | Type | Samples |
|---|---|---|---|---|
| -----------No.---------- | --No.-- | ---------------No.--------------- | ||
| ERY-PEN-TET-CIP-KAN | 5 | 5 | Clinical MRSA a | 2 |
| Healthy human | 3 | |||
| ERY-PEN-CIP-KAN-QUI | 5 | 1 | Clinical MRSA a | 1 |
| ERY-PEN-CIP-KAN-DAP | 5 | 5 | Clinical MRSA a | 5 |
| ERY-PEN-CIP-KAN | 4 | 29 | Clinical MRSA a | 25 |
| Clinical MRSA b | 2 | |||
| Healthy human | 2 | |||
| ERY-PEN-CIP-DAP | 4 | 1 | Clinical MRSA a | 1 |
| ERY-PEN-TET | 3 | 2 | Healthy human | 2 |
| ERY-PEN-KAN | 3 | 3 | Clinical MRSA a | 2 |
| Healthy human | 1 | |||
| ERY-CIP-KAN | 3 | 1 | Clinical MRSA a | 1 |
| PEN-TET-CIP | 3 | 1 | Clinical MRSA a | 1 |
| PEN-CIP-KAN | 3 | 2 | Clinical MRSA a | 1 |
| Healthy human | 1 | |||
| ERY-PEN-CIP | 3 | 55 | Clinical MRSA a | 51 |
| Healthy human | 4 | |||
| ERY-PEN | 2 | 9 | Clinical MRSA a | 36 |
| Healthy human | 6 | |||
| PEN-CIP | 2 | 8 | Clinical MRSA a | 3 |
| Healthy human | 5 | |||
| ERY-CIP | 2 | 1 | Clinical MRSA a | 1 |
| ERY | 1 | 2 | Healthy human | 2 |
| PEN | 1 | 22 | Clinical MRSA a | 6 |
| Healthy human | 16 | |||
| CIP | 1 | 2 | Clinical MRSA a | 2 |
Ciprofloxacin (CIP); Daptomycin (DAP); erythromycin (ERY); kanamycin (KAN); quinupristin/dalfopristin (QUI); penicillin (PEN); and tetracycline (TET).
a mecA positive.
b mecA and mecC negative.
Resistance according to CLSI (2012) criteria [34].
Table 6. Minimum inhibitory concentrations (MICs) of resistant Staphylococcus aureus isolates from healthy humans and clinical cases.
| Antimicrobial Agent (breakpoints) a | Resistant S. aureus isolates | MIC (μg/mL) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0.5–1 | 2 | 4 | >4 | 8 | >8 | 16 | >16 | 32 | >32 | 256 | 512 | 1024 | >1024 | ||
| ----No.---- | No. | ||||||||||||||
| (%) | |||||||||||||||
| ERY | 7 | 107 | |||||||||||||
| (≥8 μg/mL) | (6.1) | (93.9) | |||||||||||||
| PEN | 143 | 11 | 9 | 26 | 36 | 36 | 25 | ||||||||
| (≥0.25 μg/mL) | (7.7) | (6.3) | (18.2) | (25.2) | (25.2) | (17.5) | |||||||||
| TET | 8 | 2 | 2 | 4 | |||||||||||
| (≥16 μg/mL) | (25.0) | (25.0) | (50.0) | ||||||||||||
| KAN | 46 | 13 | 10 | 13 | 10 | ||||||||||
| (≥64 μg/mL) | (28.3) | (21.7) | (28.3) | (21.7) | |||||||||||
| CIP | 111 | 1 | 110 | ||||||||||||
| (≥4 μg/mL) | (0.9) | (99.1) | |||||||||||||
| QUI | 1 | 1 (100) | |||||||||||||
| (≥4 μg/mL) | |||||||||||||||
| DAP b | 6 | 3 | 3 | ||||||||||||
| (50) | (50) | ||||||||||||||
Ciprofloxacin (CIP); Daptomycin (DAP); erythromycin (ERY); kanamycin (KAN); quinupristin/dalfopristin (QUI); penicillin (PEN); and tetracycline (TET).
aLevels of MIC against tested antibiotics [34].
bCriteria for Dap: susceptible ≤1 μg/mL.
Discussion
Presumptive S. aureus isolates on MSA plates from healthy people were confirmed by biochemical testing (Sensititre identification plates) with an agreement of 100% with PCR (detection of the 16S rRNA gene) (Table 4). In this study, a nasal carriage rate of 7.6% was observed for S. aureus, which is considerably lower than the prevalence reported in other studies (29–32%) [5, 36]. However, those studies considered a significantly larger sample size, different demographic characteristics, and different sampling years as part of a nationally representative assessment of carriage of S. aureus. In this study, S. aureus strains isolated were from healthy college age individuals and did not harbor the mecA or PVL genes. Other studies have reported a nasal carriage rate of MRSA of approximately 0.8 to 1.5% in the community [5, 36], 0.5 to 44% in patients [37], 20% in healthcare workers [38] and 30% in people living and working on farms with MRSA-positive pigs or dust [39]. In contrast, Buyukcangaz et al. (2013) [15] failed to detect the mecA and PVL genes in S. aureus isolates from meat-producing animals (Table 1) that were used for the comparison with human isolates in this study. However, a low prevalence of S. aureus harboring the mecA gene was found in pork meat.
The proportion of MRSA in relation to all S. aureus strains causing infections is still unknown, making it difficult to accurately estimate the magnitude of MRSA infections and to design appropriate health action policies [7, 40]. In this study, three clinical isolates identified as MRSA were negative for the mecA gene using the protocol described by Makgotlho et al. (2009) [30]. For that reason, the presence of the novel mecA homolog (mecA LGA251 or mecC), was assessed using the protocol described by Stegger et al. (2011) [31]. However, these strains were negative for the mecC gene (138 and 718 bp fragments), but tested positive for the 356 bp fragment using degenerate primers. Therefore, further investigation should be carried out to determine the genetic variation of this mecA variant. In addition, it is known that borderline oxacillin-resistant S. aureus (BORSA) exhibit an intermediate resistance level to oxacillin, which is non-mecA mediated [41, 42]. All mecA- and mecC-negative S. aureus strains identified as MRSA were subjected to oxacillin susceptibility testing. One of those isolates exhibited an intermediate resistance level to oxacillin (2–4 μg/mL) [34], which could be considered as BORSA. Different modifications in the PBP genes causing amino acid substitutions in the transpeptidase domain has been also associated with the borderline resistance [41].
The virulence factor PVL, was detected in this study in 11.1% of MRSA isolates from clinical cases identified as blood stream infections. The MRSA isolates from cases identified as wound infections did not harbor the PVL gene. The PVL toxin is a pore-forming protein that appears to be associated with increased disease severity of mecA-positive S. aureus strains, primarily associated with blood stream infections [24]. Although the PVL gene is considered as a stable marker for CA-MRSA, some CA-MRSA strains have been found to be PVL-negative [9].
In this study, some S. aureus strains isolated from humans of each cluster in the dendrogram (Fig 1) were subjected to MLST to determine the sequence type. In general, different clones were observed in healthy humans, which indicate the presence of genotypically diverse S. aureus clones circulating in the community. Although, MRSA was not detected in healthy people, they have the potential to become carriers with the risk of spreading infections to the community [38]. Methicillin-resistant S. aureus strains isolated from clinical cases in this study presented a lower genetic diversity, and were primarily of ST5 and ST8. Previously, both ST5 and ST8 have been associated with HA-MRSA infections [27, 42]. A description of the genetic characteristics of MRSA clones associated with invasive human infections could help to focus efforts towards the study of the most common clones circulating in the hospital environment.
The molecular characteristics of S. aureus strains isolated from humans were also compared with isolates of animal origin. Genetic similarity was observed between mecA- and mecC-negative MRSA isolates from clinical cases and mecA-positive S. aureus strains isolated from clinical cases and pork meat, which suggests modifications occurring in the PBP genes in mecA- and mecC-negative MRSA strains [41] potentially resulting in slight changes in the macrorestriction patterns observed.
Contamination of meat with S. aureus strains from animals and humans could occur during slaughtering or processing. In this study, the genetic similarity between strains from humans and meat suggests contamination of raw meat during handling. In addition, the genetic similarity between S. aureus strains isolated from meat-producing animals and retail meat has been found previously, also supporting contamination of meat during slaughtering [15]. In this study, other S. aureus strains that have been previously related to LA-MRSA and pig farmers, such as ST398 and ST9 [10, 15, 29] were not detected in S. aureus isolates from humans. However, Sung et al. (2008) [43] found that animal lineages were closely related to human lineages, which could be due to the adaptive behavior of S. aureus [44].
In this study, resistance to penicillin predominated in the S. aureus strains isolated from healthy people, and the resistance profiles Ery-Pen-Cip and Ery-Pen-Cip-Kan were most common in MRSA isolates from clinical cases (Table 5). Comparing the antimicrobial resistance patterns of human isolates with S. aureus isolates of animal origin, some differences were observed (Table 2). According to the CLSI (2012) [34] interpretation criteria, most S. aureus isolates from animals exhibited resistance to penicillin and tetracycline, and from retail meat to the former antibiotics and erythromycin. Tetracycline-resistant S. aureus strains were isolated from animals and retail meat, however, ciprofloxacin-resistant S. aureus strains were found in clinical isolates. A higher rate of MDR S. aureus strains were obtained from humans than animals and meat, which could be due to the high number of MRSA strains from clinical cases affected by acute infections that were included in this study. Most MRSA strains isolated from clinical cases have been found to be MDR [45]. In addition, clinical isolates (identified as MRSA) showed higher MICs to penicillin (Table 6) than S. aureus strains obtained from animals and meat [15] suggesting the potential influence of treatment or exposure on the selection of resistant strains. In this study, all S. aureus strains were susceptible to linezolid, which has been considered as a good alternative for the treatment of MDR S. aureus [46]. The CLSI (2012) [34] criteria establishes the susceptibility to daptomycin at MICs ≤1 μg/mL, therefore in clinical isolates MICs of 2 and 4 μg/mL were considered non-susceptible isolates. The interpretation of results for gentamicin, kanamycin, and penicillin could be ambiguous due to their accepted breakpoints and limited dilutions available on the NARMS panel. For example, all S. aureus strains isolated from humans exhibited MICs ≤128 μg/mL for gentamicin, which has a breakpoint ≥16 μg/mL; for kanamycin and penicillin some S. aureus strains showed MICs ≤128 μg/mL and ≤0.25 μg/mL, respectively, however the CLSI criteria recommends a breakpoint ≥64 μg/mL and ≥0.25 μg/mL as resistance. Therefore, interpretation of some resistances may require further evaluation using a wider dilution range of antimicrobials in order to improve the interpretation of susceptibility testing results for those antibiotics.
Conclusion
The nasal carriage of S. aureus in healthy humans appears to be low, with clones genotypically diverse, and were mecA- and PVL-negative. Staphylococcus aureus strains harboring the mecA and PVL genes were present in clinical isolates from patients affected by invasive infections, and most of these isolates were of ST5 and ST8, and exhibited MDR profiles. Genetic similarity was observed between S. aureus strains isolated from humans and raw meat suggesting that contamination of meat during handling or processing could pose a risk for transmission to humans.
Supporting Information
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
This work was supported by the Dean’s Office, College of Agriculture, Food Systems and Natural Resources College, North Dakota State University (Valeria Velasco), the Dean’s Office, College of Veterinary Medicine, Iowa State University, Ames, Iowa; and the Commission of Scientific Research Projects, Uludag University (Project YDP (V)-2009/4) (Esra Buyukcangaz).
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the Dean’s Office, College of Agriculture, Food Systems and Natural Resources College, North Dakota State University (Valeria Velasco), the Dean’s Office, College of Veterinary Medicine, Iowa State University, Ames, Iowa; and the Commission of Scientific Research Projects, Uludag University (Project YDP (V)-2009/4) (Esra Buyukcangaz). The sponsors had no role in the study design, data collection, and analysis, decision to publish or preparation of the manuscript.
References
- 1. Swartz MN. Use of antimicrobial agents and drug resistance. N Engl J Med. 1997;337: 491–492. [DOI] [PubMed] [Google Scholar]
- 2. Lowy FD. Antimicrobial resistance: the example of Staphylococcus aureus . J Clin Invest. 2003;111: 1265–1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jevons MP. Celbenin-resistant Staphylococci. Br Med J. 1961;1: 124–125. [Google Scholar]
- 4. de Lencastre H, Oliveira D, Tomasz A. Antibiotic resistant Staphylococcus aureus: a paradigm of adaptive power. Curr Opin Microbiol. 2007;10: 428–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gorwitz RJ, Kruszon-Moran D, McAllister SK, McQuillan G, McDougal LK, Foshheim GE, et al. Changes in the prevalence of nasal colonization with Staphylococcus aureus in the United States, 2001–2004. J Infect Dis. 2008;197: 1226–1234. 10.1086/533494 [DOI] [PubMed] [Google Scholar]
- 6. Klein E, Smith DL, Laxminarayan R. Hospitalizations and deaths caused by methicillin-resistant Staphylococcus aureus, United States, 1999–2005. Emerg Infect Dis. 2007;13: 1840–1846. 10.3201/eid1312.070629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Klevens RM, Morrison MA, Nadle J, Petit S, Gershman K, Ray S, et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. J Am Med Assoc. 2007;298: 1763–1771. [DOI] [PubMed] [Google Scholar]
- 8. D’Agata EMC, Webb GF, Horn MA, Moellering RC Jr., Ruan S. Modeling the invasion of community-acquired methicillin-resistant Staphylococcus aureus into hospitals. Clin Infect Dis. 2009;48: 274–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nimmo GR, Bergh H, Nakos J, Whiley D, Marquess J, Huygens F, et al. Replacement of healthcare-associated MRSA by community-associated MRSA in Queensland: Confirmation by genotyping. J Infect. 2013;67: 439–447. 10.1016/j.jinf.2013.07.020 [DOI] [PubMed] [Google Scholar]
- 10. van Belkum A, Melles DC, Peeters JK, van Leeuwen WB, van Duijkeren E, Huijsdens XW, et al. Methicillin-resistant and -susceptible Staphylococcus aureus sequence type 398 in pigs and humans. Emerg Infect Dis. 2008;14: 479–483. 10.3201/eid1403.070760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Guardabassi L, O'Donoghue M, Moodley A, Ho J, Boost M. Novel lineage of methicillin-resistant Staphylococcus aureus, Hong Kong. Emerg Infect Dis. 2009;15: 1998–2000. 10.3201/eid1512.090378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Persoons D, Van Hoorebeke S, Hermans K, Butaye P, de Kruif A, Haesebrouck F, et al. Methicillin-resistant Staphylococcus aureus in poultry. Emerg Infect Dis. 2009;15: 452–453. 10.3201/eid1503.080696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. de Boer E, Zwartkruis-Nahuis JT, Wit B, Huijsdens XW, de Neeling AJ, Bosch T, et al. Prevalence of methicillin-resistant Staphylococcus aureus in meat. Int J Food Microbiol. 2009;134: 52–56. 10.1016/j.ijfoodmicro.2008.12.007 [DOI] [PubMed] [Google Scholar]
- 14. Pu S, Han F, Ge B. Isolation and characterization of methicillin-resistant Staphylococcus aureus strains from Louisiana retail meats. Appl Environ Microbiol. 2009;75: 265–267. 10.1128/AEM.01110-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Buyukcangaz E, Velasco V, Sherwood JS, Stepan RM, Koslofsky RJ, Logue CM. Molecular typing of Staphylococcus aureus and methicillin-resistant Staphylococcus aureus (MRSA) isolated from retail meat and animals in North Dakota, USA. Foodborne Pathog Dis. 2013;10: 608–617. 10.1089/fpd.2012.1427 [DOI] [PubMed] [Google Scholar]
- 16. O'Brien AM, Hanson BM, Farina SA, Wu JY, Simmering JE, Wardyn SE, et al. MRSA in conventional and alternative retail pork products. PLoS One. 2012;7(1): e30092 10.1371/journal.pone.0030092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hartman B, Tomasz A. Altered penicillin-binding proteins in methicillin-resistant strains of Staphylococcus aureus . Antimicrob. Agents Chemother. 1981;19: 726–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Van De Griend P, Herwaldt LA, Alvis B, DeMartino M, Heilmann K, Doern G, et al. Community-associated methicillin-resistant Staphylococcus aureus, Iowa, USA. Emerg Infect Dis. 2009;15: 1582–1589. 10.3201/eid1510.080877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. García-Álvarez L, Holden MTG, Lindsay H, Webb CR, Brown DFJ, Curran MD, et al. Meticillin-resistant Staphylococcus aureus with a novel mecA homologue in human and bovine populations in the UK and Denmark: a descriptive study. The Lancet. 2011;11: 595–603. 10.1016/S1473-3099(11)70126-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ito T, Hiramatsu K, Tomasz A, de Lencastre H, Perreten V, Holden MTG, et al. Guidelines for reporting novel mecA gene homologues. Antimicrob. Agents Chemother. 2012;56: 4997–4999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Laurent F, Chardon H, Haenni M, Bes M, Reverdy M-E, Madec J-Y, et al. MRSA harboring mecA variant gene mecC, France. Emerg Infect Dis. 2012;18: 1465–1467. 10.3201/eid1809.111920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Petersen A, Stegger M, Heltberg O, Christensen J, Zeuthen A, Knudsen LK, et al. Epidemiology of methicillin-resistant Staphylococcus aureus carrying the novel mecC gene in Denmark corroborates a zoonotic reservoir with transmission to humans. Clin Microbiol Infect. 2012;19: E16–E22. 10.1111/1469-0691.12036 [DOI] [PubMed] [Google Scholar]
- 23. Baba T, Takeuchi F, Kuroda M, Yuzawa H, Aoki K, Oguchi A, et al. Genome and virulence determinants of high virulence community-acquired MRSA. The Lancet. 2002;359: 1819–1827. [DOI] [PubMed] [Google Scholar]
- 24. Dufour P, Gillet Y, Bes M, Lina G, Vandenesch F, Floret D, et al. Community-acquired methicillin-resistant Staphylococcus aureus infections in France: emergence of a single clone that produces Panton-Valentine leukocidin. Clin Infect Dis. 2002;35: 819–824. [DOI] [PubMed] [Google Scholar]
- 25. Ebert MD, Sheth S, Fishman EK. Necrotizing pneumonia caused by community-acquired methicillin-resistant Staphylococcus aureus: an increasing cause of "mayhem in the lung". Emerg Radiol. 2009;16: 159–162. 10.1007/s10140-008-0706-5 [DOI] [PubMed] [Google Scholar]
- 26. McDougal LK, Steward CD, Killgore GE, Chaitram JM, McAllister SK, Tenover FC, et al. Pulsed-field gel electrophoresis typing of oxacillin-resistant Staphylococcus aureus isolates from the United States: establishing a national database. J Clin Microbiol. 2003;41: 5113–5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Deurenberg RH, Vink C, Kalenic S, Friedrich AW, Bruggeman CA, Stobberingh EE. The molecular evolution of methicillin-resistant Staphylococcus aureus . Clin Microbiol Infect. 2007;13: 222–235. [DOI] [PubMed] [Google Scholar]
- 28. Stenhem M, Ortqvist A, Ringberg H, Larsson L, Olsson-Liljequist B, Hæggman S. et al. Imported methicillin-resistant Staphylococcus aureus, Sweden. Emerg Infect Dis. 2010;16: 189–196. 10.3201/eid1602.081655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Krziwanek K, Metz-Gercek S, Mittermayer H. Methicillin-Resistant Staphylococcus aureus ST398 from human patients, upper Austria. Emerg Infect Dis. 2009;15: 766–769. 10.3201/eid1505.080326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Makgotlho PE, Kock MM, Hoosen A, Lekalakala R, Omar S, Dove M, et al. Molecular identification and genotyping of MRSA isolates. FEMS Immunol Med Microbiol. 2009;57: 104–115. 10.1111/j.1574-695X.2009.00585.x [DOI] [PubMed] [Google Scholar]
- 31. Stegger M, Andersen PS, Kearns A, Pichon B, Holmes MA, Edwards G, et al. Rapid detection, differentiation and typing of methicillin-resistant Staphylococcus aureus harbouring either mecA or the new mecA homologue mecA LGA251. Clin Microbiol Infect. 2011;18: 385–400. [DOI] [PubMed] [Google Scholar]
- 32. Ribot EM, Fair MA, Gautom R, Cameron DN, Hunter SB, Swaminathan B, et al. Standardization of pulsed-field gel electrophoresis protocols for the subtyping of Escherichia coli O157:H7, Salmonella, and Shigella for PulseNet. Foodborne Pathog Dis. 2006;3: 59–67. [DOI] [PubMed] [Google Scholar]
- 33. Enright MC, Day NP, Davies CE, Peacock SJ, Spratt BG. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus . J Clin Microbiol. 2000;38: 1008–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.[CLSI] Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. 22nd Informational Supplement. Document 2012; M100-S22. CLSI, Wayne, PA.
- 35. Aydin A, Muratoglu K, Sudagidan M, Bostan K, Okuklu B, Harsa S. Prevalence and antibiotic resistance of foodborne Staphylococcus aureus isolates in Turkey. Foodborne Pathog Dis. 2011;8: 63–69. 10.1089/fpd.2010.0613 [DOI] [PubMed] [Google Scholar]
- 36. Mainous AG III, Hueston WJ, Everett CJ, Diaz VA. Nasal carriage of Staphylococcus aureus and methicillin-resistant S. aureus in the United States, 2001–2002. Ann Fam Med. 2006;4: 132–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tiemersma EW, Bronzwaer SLAM, Lyytikäinen O, Degener JE, Schrijnemakers P, Bruinsma N, et al. Methicillin-resistant Staphylococcus aureus in Europe, 1999–2002. Emerg Infect Dis. 2004;10: 1627–1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kumar P, Shukla I, Varshney S. Nasal screening of healthcare workers for nasal carriage of coagulase positive MRSA and prevalence of nasal colonization with Staphylococcus aureus. Biol Med. 2011;3: 182–186. [Google Scholar]
- 39. Van Den Broek IVF, Van Cleef BAGL, Haenen A, Broens EM, Van Der Wolf PJ, Van Den Broek JM, et al. Methicillin-resistant Staphylococcus aureus in people living and working in pig farms. Epidemiol Infect. 2009;137: 700–708. 10.1017/S0950268808001507 [DOI] [PubMed] [Google Scholar]
- 40. Moxnes JF, de Blasio BF, Leegaard TM, Fossum Moen AE. Methicillin-resistant Staphylococcus aureus (MRSA) is increasing in Norway: a time series analysis of reported MRSA and Methicillin-sensitive S. aureus cases, 1997–2010. PLoS One. 2013;8(8): e70499 10.1371/journal.pone.0070499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Nadarajah J, Lee MJS, Louie L, Jacob L, Simor AE, Louie M, et al. Identification of different clonal complexes and diverse amino acid substitutions in penicillin-binding protein 2 (PBP2) associated with boderline oxacillin resistance in Canadian Staphylococcus aureus isolates. J Med Microbiol. 2006;55: 1675–1683. [DOI] [PubMed] [Google Scholar]
- 42. Stefani S, Chung DR, Lindsay JA, Friedrich AW, Kearns AM, Westh H, et al. Methicillin-resistant Staphylococcus aureus (MRSA): global epidemiology and harmonisation of typing methods. Int J Antimicrob Agents. 2012;39: 273–282. 10.1016/j.ijantimicag.2011.09.030 [DOI] [PubMed] [Google Scholar]
- 43. Sung JML, Lloyd DH, Lindsay JA. Staphylococcus aureus host specificity: comparative genomics of human versus animal isolates by multi-strain microarray. Microbiol. 2008;154: 1949–1959. [DOI] [PubMed] [Google Scholar]
- 44. McCarthy AJ, Lindsay JA, Loeffler A. Are all meticillin-resistant Staphylococcus aureus (MRSA) equal in all hosts? Epidemiological and genetic comparison between animal and human MRSA. Vet Dermatol. 2012;23: 267–e54. 10.1111/j.1365-3164.2012.01072.x [DOI] [PubMed] [Google Scholar]
- 45. Arora S, Devi P, Arora U, Devi B. Prevalence of methicillin-resistant Staphylococcus aureus (MRSA) in a tertiary care hospital in Northern India. J Lab Physicians. 2014;2: 79–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kishore S, Verma D, Siddique M. Comparison of in-vitro activities of linezolid and vancomycin against Staphylococcus aureus isolated from a tertiary care hospital. J Clin Diagn Res. 2014;8: DC12–DC15. 10.7860/JCDR/2014/7751.4338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. McClure JA, Conly JM, Lau V, Elsayed S, Louie T, Hutchins W, et al. Novel multiplex PCR assay for detection of the staphylococcal virulence marker Panton-Valentine leukocidin genes and simultaneous discrimination of methicillin-susceptible from -resistant staphylococci. J Clin Microbiol. 2006;44: 1141–1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.