Abstract
Shiga toxigenic Escherichia coli (STEC) O157 and several other serogroups of non-O157 STEC are causative agents of severe disease in humans world-wide. The present study was conducted to characterize STEC O157 and non-O157 serogroups O26, O103, O111, O121, O45, and O145 in ruminants in Malaysia. A total of 136 ruminant feces samples were collected from 6 different farms in Peninsular Malaysia. Immunomagnetic beads were used to isolate E. coli O157 and non-O157 serogroups, while PCR was used for the detection and subtyping of STEC isolates. STEC O157:H7 was isolated from 6 (4%) feces samples and all isolates obtained carried stx 2c, eaeA-γ1, and ehxA. Non-O157 STEC was isolated from 2 (1.5%) feces samples with one isolate carrying stx 1a, stx 2a, stx 2c, and ehxA and the other carrying stx 1a alone. The presence of STEC O157 and non-O157 in a small percentage of ruminants in this study together with their virulence characteristics suggests that they may have limited impact on public health.
1. Introduction
Shiga toxin producing E. coli (STEC), a serologically diverse group of zoonotic pathogens, have emerged as one of the most virulent groups of bacteria associated with cases of food borne disease in humans [1]. STEC can cause a spectrum of diseases ranging from mild diarrhea to severe bloody diarrhea, called hemorrhagic colitis (HC), and even life-threatening sequelae such as hemolytic uremic syndrome (HUS). Patients with HUS were often diagnosed as having thrombotic thrombocytopenic purpura (TTP), although thrombotic microangiopathy is now considered a more accurate description of the condition associated with HUS caused by STEC [2]. Production of Shiga toxin (Stx) is considered as the major virulence factor of STEC [1] which contributes to the development of HUS in humans [2]. Stx production alone is not sufficient for STEC to cause disease. Accessory virulence factors include a 34 kb chromosomal pathogenicity island called the “locus for enterocyte effacement” (LEE) carrying several virulence associated genes, such as the attaching and effacing (eaeA) gene, and a large plasmid (60 MDa) with an ehxA gene encoding an enterohemolysin. EaeA encodes an outer-membrane protein called intimin which enables the intimate adherence of STEC to the intestinal epithelium of the host [3]. The enterohemolysin protein is implicated in extracting iron from the blood released into the intestine [4].
The prototype STEC serotype is E. coli O157:H7 and its ability to cause HC and HUS in many regions and countries is well established. The pathogenic potential and public health significance of several non-O157 STEC serogroups, particularly O26, O103, O111, O121, O145, and O45 referred to as the “big 6” non-O157 STEC serogroups [5], have also been described in recent years due to their association with clinical HC and HUS in humans. In some geographical areas, such as in Europe, the disease caused by non-O157 strains is significantly more common than that caused by O157:H7 [6, 7].
Ruminants are considered an important source of both E. coli O157 and non-O157 with cattle being identified as the primary reservoir. Intestinal carriage of E. coli O157 and non-O157 in ruminants results in their fecal shedding and release into the environment. As a result, infections of E. coli O157 and non-O157 can be transmitted to humans via the consumption of food and water contaminated by animal feces.
Data on E. coli O157 and non-O157 serotypes in ruminants is limited in countries of the tropical regions including Malaysia. In addition, the data reported so far on E. coli O157 and non-O157 in ruminants from tropical countries other than Malaysia demonstrates substantial variation in their prevalence and virulence properties. In West Bengal, India, a total of fourteen STEC O157 isolates were obtained from two (2.04%) slaughtered cattle feces samples and six (7.59%) diarrhoeic calf feces samples [8]. The majority of STEC O157 isolates (85.71%) obtained from this study carried stx 2 alone. STEC O157 was obtained from 0.6% of cattle feces samples in Brazil [9], where the majority of isolates carried ehxA either with both stx 1 and stx 2 or with stx 2 alone. The prevalence of E. coli O157 was found to be 1.25% in cattle farms in central Mexico [10]. Non-O157 STEC was found in 18% of cattle feces samples in Calcutta, India [11], in which stx 1 predominated. In another study in Brazil, non-O157 STEC was isolated from 5.81% of calf feces samples [12] where stx 1 was the dominant stx genotype observed.
Only three studies which isolated STEC O157 from beef samples have to our knowledge been conducted in Malaysia [13–15]. Apart from a single study which reported sporadic cases of STEC O157 infection among 14% of patients presented with bloody diarrhea at a local hospital in Kuala Lumpur, Malaysia [16], there are no other published reports of sporadic cases or outbreaks of STEC O157 and non-O157 in the country. Although studies have demonstrated the presence of STEC O157 in foods of animal origin, the presence and characterization of STEC O157 or non-O157 in ruminant feces from Malaysia has not yet been determined.
The aim of the present study was to examine ruminant feces samples for the presence of STEC O157 and the “big 6” non-O157 STEC serogroups in Malaysia. The isolated strains of E. coli O157 and non-O157 were further characterized to determine their genetic diversity and presence of virulence factors to indicate the risk potential of these strains to public health.
2. Materials and Methods
2.1. Sample Collection and Preparation
Samples were collected from six different ruminant farms in Peninsular Malaysia (Table 1). The geographical distribution of the six farms is depicted in Figure 1. Farms A, C, and F were small dairy cattle farms, while farm E was a small dairy farm consisting of cattle and goats. Farm B was also a dairy farm but with a larger number and diversity of ruminants consisting of cattle, buffaloes, goats, and sheep. Farm D was a large beef cattle farm. A total of 136 fresh ruminant feces samples (~25 g each) from cattle, buffalo, sheep, and goat were collected from the pen floors (over a period of six months) into sterile containers and were stored at 4°C on ice until processed in the lab on the same day. All fecal samples collected were divided into two 10 g samples. One of the 10 g samples was used for enrichment and the other was used for long term storage in tryptone soy broth (TSB; Merck, Darmstadt, Germany) with 25% glycerol at −70°C.
Table 1.
Distribution of ruminant feces samples collected from farms A–F.
| Farm | Location | Ruminant feces samples | Total samples | |||
|---|---|---|---|---|---|---|
| Cattle | Buffalo | Goat | Sheep | |||
| A | Serdang | 25 | — | — | — | 25 |
| B | Kluang | 9 | 20 | 7 | 8 | 44 |
| C | Sentul | 9 | — | — | — | 9 |
| D | Gemas | 24 | — | — | — | 24 |
| E | Puchong | 13 | — | 5 | — | 18 |
| F | Lumut | 16 | — | — | — | 16 |
Figure 1.
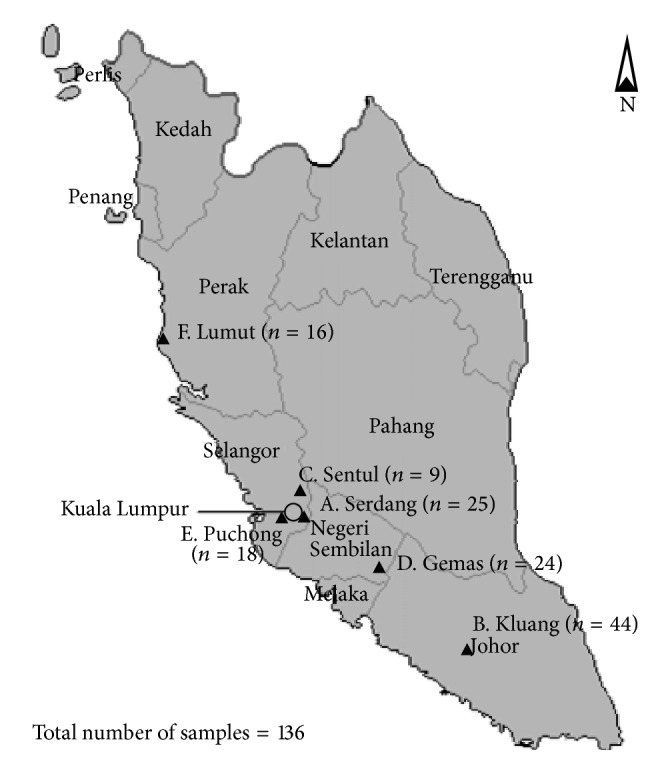
Geographical distribution of farms A–F in Peninsular Malaysia from which the ruminant feces samples were collected.
2.2. Isolation and Characterization of E. coli O157
Each fecal sample (10 g) was diluted 1/10 in buffered peptone water (BPW; Oxoid, Hampshire, UK) and homogenized for 30 s. Samples were incubated for 18 h at 37°C without agitation. Immunomagnetic separation (IMS) was performed using Dynabeads anti-E. coli O157 (Dynal, Oslo, Norway) according to the manufacturer's instructions. Resulting bead-bacteria complexes were spread on to sorbitol-MacConkey agar (SMAC; Oxoid, Hampshire, UK) and sorbitol-MacConkey agar containing the cefixime, tellurite supplement (CT-SMAC; Oxoid, Hampshire, UK) and incubated for 18 h at 37°C. A total of 10 presumptive E. coli O157 colonies per sample were serotyped using an E. coli O157 Latex Test Kit (Oxoid, Hampshire, UK). All isolates agglutinating with the O157 antiserum were further characterized by polymerase chain reaction (PCR) to detect the presence of rfbE, stx 1 , stx 2 , eaeA, ehxA, and fliC genes using primers and reaction conditions as previously described [17].
Characterization of lineage-specific polymorphisms-6 (LSPA-6) of E. coli O157 isolates was performed using target amplification and capillary electrophoresis as described previously [18, 19]. An Applied Biosystems 3130 Genetic Analyzer (Applied Biosystems, California, USA) with a DS-33 matrix and GeneScan 600 LIZsize standard was used for capillary electrophoresis, while a Peak Scanner software (Version 1.0; Applied Biosystems, California, USA) was used to interpret amplicon sizes. LSPA-6 alleles were defined according to [18]. Isolates with LSPA-6 genotype 111111 or 211111 were classified as lineage I (LI) or lineage I/II (LI/II), respectively, while all other allele combinations were grouped as lineage II (LII) [18, 20].
Analysis of Shiga toxin encoding bacteriophage insertion sites (SBI) of E. coli O157 isolates was determined as previously described [21].
2.3. Detection, Isolation, and Characterization of Non-O157 E. coli
Samples (10 g) which were initially stored at −70°C in TSB with 25% glycerol were diluted 1/10 in BPW, homogenized for 30 s, and incubated for 18 h at 37°C without agitation. DNA was extracted from 1 mL of the enriched sample using the Nucleospin Soli DNA extraction kit (Macherey Nagel, Düren, Germany) following the manufacturer's instructions. A multiplex PCR was used to screen enrichments for the presence of STEC virulence genes stx 1 , stx 2 , eaeA, and ehxA using primers and reaction conditions as described by A. W. Paton and J. C. Paton [22] with several modifications. A reaction volume of 25 μL was used with 2 μL of DNA template and final concentration of 0.25 μM of each primer, 5x Green GoTaq Flexi Buffer (Promega, Madison, USA), 200 μM of dNTP, 2 mM of MgCl2, and 1 unit of GoTaq DNA polymerase (Promega, Madison, USA). The PCR products were separated by electrophoresis on a 2% agarose gel, stained with ethidium bromide (0.5 μg/mL) and visualized under UV light. Enriched samples positive for stx and eaeA by PCR were streaked on chromocult-TBX agar (Merck, Darmstadt, Germany) and coliformen agar enhanced selectivity (Merck, Darmstadt, Germany) and incubated overnight at 37°C. Following incubation, up to 50 E. coli colonies per sample were chosen based on colony morphology and screened individually by multiplex PCR for the presence of stx 1 , stx 2 , eaeA, and ehxA as described above. Colonies that were positive for stx and eaeA were then tested for the “big 6” E. coli non-O157 serogroups by PCR using primers and conditions described previously [17, 23].
The enriched samples were also tested for the presence of genes specific to the “big 6” E. coli non-O157 serogroups. Samples that tested positive by PCR for any of the target serogroups were subjected to IMS for O26, O111, O103, and O145 using Dynabeads (Dynal, Oslo, Norway) following the manufacturer's instructions. The bead-bacteria complexes formed during IMS of O26 were plated onto rhamnose MacConkey agar, while those of O111, O103, and O145 were plated onto chromocult-TBX agar and coliformen agar-enhanced selectivity and incubated overnight at 37°C. Following incubation, 10 presumptive colonies (per sample) based on colony morphology were subjected to serogroup specific PCR and those confirmed as a specific serogroup were tested by PCR for the presence of STEC virulence genes. Isolation of serogroups O45 and O121 was performed on enriched fecal samples positive for STEC virulence markers which were directly plated onto chromocult-TBX agar as described above.
2.4. Biochemical Confirmation of E. coli Isolates
All the isolates were biochemically identified as E. coli by citrate utilization and indole production tests [24].
2.5. Bacterial Strains
The bacterial strains used as controls in this study are listed in Table 2.
Table 2.
Bacterial strains used in the study.
| Strain ID | Serogroup | Source | Country | Virulence traits |
|---|---|---|---|---|
| Sakai | O157 | Radish sprouts | Japan | stx 1, stx 2 , eaeA, ehxA |
| ATCC 43895 | O157 | Ground beef | USA | stx 1, stx 2 , eaeA, ehxA |
| EC543a | O157 | Cattle feces | Australia | stx 1, stx 2 , eaeA, ehxA |
| EC6a | O157 | Cattle feces | Australia | stx 2 , eaeA, ehxA |
| 1 UPMa | O157 | Bovine milk | Malaysia | stx 1, stx 2 , eaeA, ehxA |
| 2 UPMa | O157 | Bovine milk | Malaysia | stx 1, stx 2 , eaeA, ehxA |
| 3 UPMa | O157 | Beef | Malaysia | stx 1, stx 2 , eaeA, ehxA |
| 4 UPMa | O157 | Beef | Malaysia | stx 1, stx 2 , eaeA, ehxA |
| MG1655 (E. coli K-12) | OR:H48:K-b | Laboratory strain | USA | None |
| EC3008ac | O26 | Cattle feces | Australia | eaeA |
| EC3009ac | O45 | Cattle feces | Australia | None |
| EC2998ac | O103 | Cattle feces | Australia | None |
| EC3113ac | O111 | Cattle feces | Australia | None |
| EC3111ac | O121 | Cattle feces | Australia | None |
aProvided by Professor Son Radu at Universiti Putra Malaysia.
bOR = O antigen rough strain which does not produce a typeable O antigen.
c E. coli non-O157 strains used as controls in the study, provided by Lesley Duffy at CSIRO, Brisbane, Australia.
2.6. Pulsed-Field Gel Electrophoresis (PFGE)
PFGE using XbaI was performed on all E. coli O157 and non-O157 isolates in a CHEF Mapper (Bio-Rad, California, USA) according to the standardized PulseNet protocol [25]. Banding patterns were analysed using BioNumerics software, version 6.5 (Applied Maths BVBA, Sint-Martens-Latem, Belgium) following the PulseNet protocol.
2.7. Subtyping of stx and Intimin (eaeA) Genes of E. coli O157 and Non-O157
The subtypes of stx and eaeA in isolates carrying these markers were determined following previously published methods [26, 27].
2.8. Detection of Shiga Toxin Expression
Stx expression by the STEC strains was determined according to the method adapted from Shringi et al. [28] using an ELISA kit (Premier EHEC, Meridian Bioscience, Ohio, USA). Mitomycin C (Sigma Aldrich, Missouri, USA) was used at a final concentration of 0.5 μg/mL to induce Stx production. After induction, the cells were lysed using Polymixin B (Sigma Aldrich, Missouri, USA) at a final concentration of 0.5 mg/mL and incubated at 37°C for 1 h with rotary shaking (250 rpm). Polymixin B treated cultures were diluted 1 : 100 in sterile LB broth immediately followed by 1 : 2 dilution in sample diluent of the ELISA kit. Absorbance readings were obtained at wavelengths 450 nm and 630 nm using a Victor X microtiter plate reader (Perkin Elmer, Glen Waverley, Australia) and the results were displayed as the mean value of two independent biological replicates.
3. Results
3.1. Presence of STEC O157 and Virulence Factors
STEC O157 was isolated from 6 (4%) cattle feces samples, all of which were from farm A (Table 3). A total of 32 STEC O157 isolates were obtained from 6 different cattle feces samples. The isolates obtained were clustered into two different PFGE groups (at >92% similarity) with the majority of isolates (28 isolates from 5 different fecal samples) belonging to one PFGE group and the remaining isolates (4 isolates from a single fecal sample) belonging to the other. All 32 STEC O157 isolates were positive for the virulence factors stx 2 , eaeA, and ehxA and also for fliC specific for the H7 antigen indicating they belong to the O157:H7 genotype. All samples from farms B–F were negative for the presence STEC O157.
Table 3.
STEC O157 and non-O157 and their virulence profiles.
| STEC serogroup | Number of STEC+ samples (%) | Source | Number of isolates | Virulence factors | Lineage | SBI profile |
|---|---|---|---|---|---|---|
| O157:H7a | 6 (4%) | Cattle feces | 28b | stx 2c, eaeA-γ1, ehxA | II | SY2c |
| 4b | stx 2c, eaeA-γ1 ehxA | II | SY2c | |||
|
| ||||||
| Non-O157a (unknown) | 2 (1.5%) | Cattle feces | 1 | stx 1a, stx 2a, stx 2c, ehxA | — | — |
| 1 | stx 1 | — | — | |||
aIsolates of STEC O157:H7 and non-O157 were only present in samples obtained from farm A. All samples from farms B–F were negative for STEC O157:H7 and non-O157 isolates.
bOn farm A, 28 of the STEC O157 isolates belonged to one PFGE group (at >92% similarity) and the remaining 4 isolates belonged to another PFGE group.
—: not applicable.
LSPA-6 target amplification indicated that all the STEC O157:H7 isolates collected from cattle feces samples in farm A belong to lineage II (Table 3). According to the SBI genotyping code, genotype SY2c was observed in all STEC O157:H7 isolates collected from cattle feces samples in farm A indicating the association of stx 2c with prophage insertion in the sbcB locus (Table 3).
In addition, all STEC O157:H7 isolates obtained from UPM carried the virulence markers stx 1 , stx 2 , eaeA, and ehxA and belonged to a single PFGE group (at >92% similarity). They were of lineage I and contained the SBI genotype WY12 indicating the association of stx 1 and stx 2a with prophage insertion in the yehV and wrbA loci, respectively.
3.2. Presence of Non-O157 STEC and Virulence Factors
In the initial PCR screen of the enriched samples, various combinations of virulence markers and genes for the target non-O157 serogroups were observed in all the farms except in farm F. Although samples in farm F were positive for different combinations of virulence markers, none of the samples were positive for any of the target non-O157 serogroups tested (Table 4). Overall, the combination of stx (either stx 1 , stx 2 or both) and eaeA was present in 32.3% (44 samples out of 136 samples), while the gene indicating the presence of serogroup O103 seemed to be predominant (44.1% of samples) among all 136 samples.
Table 4.
Occurrence of target virulence factors and “big 6” non-O157 serogroups in the initial PCR screen of the enriched samples from each farm (A–F).
| Farm | Number of samples tested | Percent positive for virulence gene combinationsa | Percent positive for serogroupsa | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| stx 1, stx 2 , eaeA, ehxA | stx 1, stx 2 , ehxA | stx 1 or stx 2 , eaeA, ehxA | stx 1 , ehxA | stx 2 , ehxA | eaeA, ehxA | eaeA | stx 1 or stx 2 alone | O111 | O26 | O121 | O145 | O45 | O103 | ||
| A | 25 | 6.6 | 2.9 | 0 | 0 | 1.5 | 0 | 0 | 0 | 0 | 0 | 5.9 | 0 | 3.7 | 5.1 |
| B | 44 | 13.2 | 2.9 | 0 | 0 | 0 | 0 | 0 | 0 | 0.7 | 9.6 | 13.2 | 0 | 2.2 | 16.2 |
| C | 9 | 2.9 | 0 | 0 | 0 | 0.7 | 2.2 | 0.7 | 0 | 0 | 2.9 | 0.7 | 1.5 | 3.7 | 5.1 |
| D | 24 | 1.5 | 4.4 | 1.5 | 0 | 0 | 0.7 | 0 | 2.9 | 0 | 8.1 | 0 | 0.7 | 0.7 | 10.3 |
| E | 18 | 5.9 | 2.9 | 0.7 | 0 | 0 | 0 | 0 | 0 | 3.7 | 4.4 | 0.7 | 0.7 | 8.1 | 7.4 |
| F | 16 | 0 | 2.2 | 0 | 1.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
|
| |||||||||||||||
| Total | 136 | 30.1 | 15.4 | 2.2 | 1.5 | 2.2 | 2.9 | 0.7 | 2.9 | 4.4 | 25 | 20.6 | 2.9 | 18.4 | 44.1 |
aThe percentage of samples positive were calculated by dividing the number of positive samples for each category in the initial PCR screen by the total number of samples (n = 136) collected.
Although the initial PCR screening of the enriched feces samples indicated a relatively high number of samples with the target genes for the virulence factors and non-O157 serogroups, only 2 samples (1.5%) yielded non-O157 STEC isolates (Table 3). Both of these were cattle feces samples collected from farm A, from which two non-O157 STEC strains (negative for any of the “big 6” non-O157 serogroups) were isolated which belonged to two unique PFGE groups. One of the two non-O157 STEC isolates was positive for stx 1 , stx 2, and ehxA while the other isolate was positive for stx 1 alone.
3.3. Characterization of E. coli Serogroups Lacking stx
E. coli of the target serogroups (O157 and the “big 6” non-O157) lacking stx but carrying other combinations of virulence markers were also isolated from ruminant feces samples (Table 5). These included E. coli of serogroups O157, O103, and O26 which were negative for any of the virulence markers, O157 which carried eaeA alone and O26 with eaeA and ehxA.
Table 5.
Isolation and virulence profiles of E. coli O157 and “big 6” E. coli non-O157 serogroups lacking stx.
| Serogroup | Farm | Source | Number of + samples | Number of isolates tested | Virulence factors | Intimin subtype |
|---|---|---|---|---|---|---|
| O103 | A | Cattle feces | 3 | 3 | None | — |
|
| ||||||
| O157 | B | Cattle feces | 1 | 2 | eaeA | NTa |
| Sheep feces | 2 | 3 |
eaeA (1 isolate) none (2 isolates) |
NT | ||
| Buffalo feces | 3 | 5 | eaeA | NT | ||
|
| ||||||
| O26 | B | Buffalo feces | 2 | 5 | eaeA, ehxA (2 isolates) none (3 isolates) | eaeA-β1 |
|
| ||||||
| O103 | B | Buffalo feces | 1 | 7 | None | — |
|
| ||||||
| O26 | C | Cattle feces | 2 | 11 | None | — |
aNT = non-typable.
—: not applicable.
3.4. stx and eaeA Subtyping
All the STEC O157:H7 isolates collected from cattle feces samples in farm A were positive for stx 2c (Table 3), while all STEC O157:H7 isolates from UPM were positive for stx 1a and stx 2a. One of the non-O157 STEC isolates was positive for stx 1a, stx 2a, and stx 2c, while the other isolate was positive for stx 1a alone (Table 3). Overall, stx 2c was the more prevalent genotype among the stx 2 positive isolates.
Two different eaeA subtypes out of the seven eaeA variants (α1, α2, β1, β2, γ1, γ2/θ, and ε) tested were present among the eaeA positive isolates of E. coli O157 and non-O157. The STEC O157:H7 isolates were positive for eaeA-γ1 (Table 3) while the two O26 isolates lacking stx were positive for eaeA-β1 (Table 5).
3.5. Shiga Toxin Production
Stx production of all the stx 2c positive STEC O157:H7 isolates collected from the cattle feces samples in farm A were below the level of detection. In contrast, all the stx 1a and stx 2a positive STEC O157:H7 isolates obtained from UPM produced a high amount of Stx similar to the positive control STEC O157:H7 isolates, ATCC 43895, EC543a, and EC6a. Of the two non-O157 STEC isolates, Stx production of the stx 1a positive non-O157 isolate was also below the level of detection. However, the stx 1a, stx 2a, and stx 2c positive non-O157 STEC isolate indicated a moderate amount of Stx production although lower than that observed for the UPM STEC O157:H7 isolates.
4. Discussion
In Malaysia, no studies have been conducted so far to characterize STEC O157 or non-O157 in ruminant feces. Thus, the goal of the present study was to gain insight on the virulence determinants of STEC O157 and non-O157 present in ruminant feces in Malaysia.
In this study, STEC O157 was isolated from 6 (4.4%) ruminant feces samples and non-O157 STEC was isolated from 2 (1.5%) of the ruminant feces samples. Several other authors have also reported low isolation rates (less than 10%) of STEC O157 and non-O157 in ruminant feces in tropical countries [8, 12]. However, this study was not adequate to determine the prevalence of STEC O157 and non-O157 in Malaysia and, thus, to obtain more comprehensive data on the prevalence of STEC O157 and non-O157 serogroups in Malaysia, sampling of a wider geographical area within Malaysia should be undertaken.
E. coli O157 populations have been shown to vary in their distribution among bovine and clinical sources due to their genotypic differences [29]. LSPA-6 analysis, a simple multiplex PCR assay, categorizes E. coli O157 strains into three different genotypes referred to as lineage I, lineage I/II, and lineage II. Isolates of lineage I and I/II are mostly associated with human clinical sources while lineage II isolates are mostly associated with bovine sources [18]. In this study, all the STEC O157:H7 isolates belonged to lineage II in contrast to STEC O157 isolates from countries such as Australia and USA where lineage I/II and lineage I predominates [30]. Interestingly, all the STEC O157:H7 isolates from UPM were of lineage I indicating the presence of STEC O157 isolates of both lineage I and II in bovine sources in Malaysia. STEC O157 isolates of lineage II are shown to be less virulent and possibly impaired in their transmissibility to humans compared to lineage I or I/II [31]. The presence of STEC O157 isolates of lineage II in ruminants in Malaysia from this study suggests that these isolates could have less pathogenic potential in humans.
Pathogenic potential of STEC isolates has also been shown to be associated with the presence of particular stx genotypes. E. coli isolates carrying stx 1 or stx 2c are associated with low virulence potential compared to those which carry stx 2 (stx 2a) [32]. In this study, all the STEC O157:H7 isolates obtained carried stx 2c indicating low virulence potential in humans compared to the STEC O157:H7 isolates from UPM with stx 1a and stx 2a. One of the two non-O157 STEC isolates of unknown serogroup with stx 1a, stx 2a, and stx 2c indicated a high pathogenic potential compared to the other isolate with stx 1a alone.
Not all E. coli isolates carrying stx produce Stx [33]. This was true for all stx 2c positive STEC O157:H7 isolates and one of the non-O157 isolates positive for stx 1a obtained in this study. In contrast, the UPM STEC O157 isolates produced Stx. Although the exact reasons for the discrepancy observed in Stx production of stx positive E. coli isolates from this study is not fully understood, previous studies have also identified E. coli isolates positive for stx but negative for Stx production [33, 34]. In fact, the study by Koitabashi et al. [34] suggested that stx 2 positive E. coli O157 strains that produce little or no Stx2 may be widely distributed in the Asian environment.
Particular stx genotypes of STEC O157 have been shown to be associated both with particular SBI genotypes and with their relative frequency of isolation from clinical and bovine sources [21]. Clinical isolates are generally characterized by the carrying of stx 2 and stx 2-associated bacteriophage sequences adjacent to either wrbA or argW (SBI genotypes: WY12, AY2, ASY2, ASY22c), while bovine isolates are characterized by carrying of stx 2c and stx 2c-associated bacteriophage sequences adjacent to sbcB (SBI genotypes: SY2c, SY12c, and ASY12c). In agreement with these observations, the STEC O157 isolates obtained from cattle feces from this study carried stx 2c with an occupied sbcB locus (SY2c). However, the STEC O157 from UPM which were collected from bovine sources carried stx 2 and an occupied wrbA locus indicating characteristics of clinical isolates.
All the STEC O157:H7 isolates in this study and the STEC O157:H7 isolates from UPM carried eaeA-γ1 as reported for eaeA positive E. coli O157 in previous studies [27, 35]. None of the eaeA positive non-STEC O157 could be subtyped using the primers for eaeA subtypes α1, α2, β1, β2, γ1, γ2/θ, and ε. It is possible that these isolates belonged to other intimin subtypes such as δ/κ, ζ, η, ι, λ, μ, and ν which were not tested for in this study. The two eaeA positive E. coli O26 isolates carried eaeA-β1 similar to several other E. coli O26 isolates previously associated with human STEC strains that cause HUS [27].
5. Conclusions
Despite the use of specific and sensitive methods of enrichment and IMS followed in this study to isolate STEC O157 and non-O157, it appears that the presence of both STEC O157 and non-O157 in ruminant feces was low (4% and 1.5%, resp.). The stx 2c carrying STEC O157:H7 isolates of lineage II from this study suggests that these bacteria potentially represent a less pathogenic clone of STEC O157 in Malaysia. This together with the presence of STEC O157 and non-O157 in a small percentage of ruminants in this study could contribute to the reasons for the lack of reported sporadic cases and outbreaks caused by STEC O157 in Malaysia. Similar to STEC O157, the low percentage of non-O157 STEC isolates observed together with their low pathogenic potential indicated by the lack of eaeA and moderate to no Stx production suggests a low probability of causing disease in humans.
Acknowledgments
The authors thank Monash University, Malaysia, and Commonwealth Scientific and Industrial Research Organization (CSIRO) Animal, Food and Health Science, Australia, for funding this study. The authors also thank Lesley Duffy for the provision of E. coli non-O157 isolates, Glen Mellor, Edward Fox, and Sean Moore for expert technical assistance and Professor Son Radu of Universiti Putra Malaysia for the provision of STEC O157 isolates.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Gyles C. L. Shiga toxin-producing Escherichia coli: an overview. Journal of Animal Science. 2007;85(13):E45–E62. doi: 10.2527/jas.2006-508. [DOI] [PubMed] [Google Scholar]
- 2.Tarr P. I., Gordon C. A., Chandler W. L. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. The Lancet. 2005;365(9464):1073–1086. doi: 10.1016/s0140-6736(05)71144-2. [DOI] [PubMed] [Google Scholar]
- 3.Nataro J. P., Kaper J. B. Diarrheagenic Escherichia coli . Clinical Microbiology Reviews. 1998;11(1):142–201. doi: 10.1128/cmr.11.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Law D., Kelly J. Use of heme and hemoglobin by Escherichia coli O157 and other Shiga-like-toxin-producing E. coli serogroups. Infection and Immunity. 1995;63(2):700–702. doi: 10.1128/iai.63.2.700-702.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bosilevac J. M., Koohmaraie M. Predicting the presence of non-O157 shiga toxin-producing Escherichia coli in ground beef by using molecular tests for shiga toxins, intimin, and O serogroups. Applied and Environmental Microbiology. 2012;78(19):7152–7155. doi: 10.1128/aem.01508-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bielaszewska M., Janda J., Blahova K., Sramkova L., Havlik J., Potuznik V. Verocytotoxin-producing Escherichia coli in children with hemolytic uremic syndrome and diarrhea in the Czech Republic. In: Kamali M. A., Goglio A. G., editors. Proceedings of the 2nd International Symposium and Workshop on Verocytotoxin (Shiga-like Toxin)-Producing Escherichia Coli Infections; 1994; Bergamo, Italy. pp. 37–40. [Google Scholar]
- 7.Caprioli A., Tozzi A. E. Epidemiology of Shiga toxin-producing Escherichia coli infections in continental Europe. In: Kaper J. B., O'Brien A. D., editors. Escherichia coli O157:H7 and Other Shiga Toxin-Producing E. coli Strains. Washington, DC, USA: American Society for Microbiology; 1998. pp. 38–48. [Google Scholar]
- 8.Manna S. K., Brahmane M. P., Manna C., Batabyal K., Das R. Occurrence, virulence characteristics and antimicrobial resistance of Escherichia coli O157 in slaughtered cattle and diarrhoeic calves in West Bengal, India. Letters in Applied Microbiology. 2006;43(4):405–409. doi: 10.1111/j.1472-765x.2006.01975.x. [DOI] [PubMed] [Google Scholar]
- 9.Irino K., Kato M. A. M. F., Vaz T. M. I., et al. Serotypes and virulence markers of Shiga toxin-producing Escherichia coli (STEC) isolated from dairy cattle in São Paulo State, Brazil. Veterinary Microbiology. 2005;105(1):29–36. doi: 10.1016/j.vetmic.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 10.Callaway T. R., Anderson R. C., Tellez G., et al. Prevalence of Escherichia coli O157 in cattle and swine in central Mexico. Journal of Food Protection. 2004;67(10):2274–2276. doi: 10.4315/0362-028x-67.10.2274. [DOI] [PubMed] [Google Scholar]
- 11.Khan A., Yamasaki S., Sato T., et al. Prevalence and genetic profiling of virulence determinants of non-O157 Shiga toxin-producing Escherichia coli isolated from cattle, beef, and humans, Calcutta, India. Emerging Infectious Diseases. 2002;8(1):54–62. doi: 10.3201/eid0801.010104. [DOI] [PubMed] [Google Scholar]
- 12.Leomil L., Aidar-Ugrinovich L., Guth B. E. C., et al. Frequency of Shiga toxin-producing Escherichia coli (STEC) isolates among diarrheic and non-diarrheic calves in Brazil. Veterinary Microbiology. 2003;97(1-2):103–109. doi: 10.1016/j.vetmic.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Apun K., Chang P. P., Sim E. H. U., Micky V. Clonal diversity of Escherichia coli isolates from marketed beef in East Malaysia. World Journal of Microbiology & Biotechnology. 2006;22(7):661–667. doi: 10.1007/s11274-005-9086-0. [DOI] [Google Scholar]
- 14.Radu S., Mutalib S. A., Rusul G., et al. Detection of Escherichia coli O157:H7 in the beef marketed in Malaysia. Applied and Environmental Microbiology. 1998;64(3):1153–1156. doi: 10.1128/aem.64.3.1153-1156.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sukhumungoon P., Nakaguchi Y., Ingviya N., et al. Investigation of stx2+, eae+ Escherichia coli O157:H7 in beef imported from Malaysia to Thailand. International Food Research Journal. 2011;18(1):381–386. [Google Scholar]
- 16.Son R., Ansary A., Rusul G., Karim M. I. A. Isolation of verotoxin-producing Escherichia coli associated with diarrhoea in Malaysia containing plasmids showing homology with biotinylated Shiga-like toxin DNA gene probes. World Journal of Microbiology and Biotechnology. 1996;12(3):243–246. doi: 10.1007/bf00360921. [DOI] [PubMed] [Google Scholar]
- 17.Bai J., Shi X., Nagaraja T. G. A multiplex PCR procedure for the detection of six major virulence genes in Escherichia coli O157:H7. Journal of Microbiological Methods. 2010;82(1):85–89. doi: 10.1016/j.mimet.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 18.Yang Z., Kovar J., Kim J., et al. Identification of common subpopulations of non-sorbitol-fermenting, β-glucuronidase-negative Escherichia coli O157:H7 from bovine production environments and human clinical samples. Applied and Environmental Microbiology. 2004;70(11):6846–6854. doi: 10.1128/aem.70.11.6846-6854.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whitworth J., Zhang Y., Bono J., Pleydell E., French N., Besser T. Diverse genetic markers concordantly identify bovine origin Escherichia coli O157 genotypes underrepresented in human disease. Applied and Environmental Microbiology. 2010;76(1):361–365. doi: 10.1128/AEM.01761-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang Y., Laing C., Steele M., et al. Genome evolution in major Escherichia coli O157:H7 lineages. BMC Genomics. 2007;8, article 121 doi: 10.1186/1471-2164-8-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shringi S., Schmidt C., Katherine K., Brayton K. A., Hancock D. D., Besser T. E. Carriage of stx2a differentiates clinical and bovine-biased strains of Escherichia coli O157. PLoS ONE. 2012;7(12) doi: 10.1371/journal.pone.0051572.e51572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paton A. W., Paton J. C. Detection and characterization of shiga toxigenic Escherichia coli by using multiplex PCR assays for stx1, stx2, eaeA, enterohemorrhagic E. coli hlyA, rfb(O111), and rfb(O157) Journal of Clinical Microbiology. 1998;36(2):598–602. doi: 10.1128/jcm.36.2.598-602.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paddock Z., Shi X., Bai J., Nagaraja T. G. Applicability of a multiplex PCR to detect O26, O45, O103, O111, O121, O145, and O157 serogroups of Escherichia coli in cattle feces. Veterinary Microbiology. 2012;156(3-4):381–388. doi: 10.1016/j.vetmic.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 24.Aslanzadeh J. Biochemical profile-based microbial identification systems. In: Tang Y. W., Stratton C. W., editors. Advanced Techniques in Diagnostic Microbiology. New York, NY, USA: Springer; 2006. pp. 84–116. [DOI] [Google Scholar]
- 25.Environmental Science and Research Ltd. Standard operating procedure for PulseNet PFGE of Escherichia coli O157:H7, Escherichia coli non-O157 (STEC), Salmonella serotypes, Shigella sonnei and Shigella flexneri . 2013, http://www.pulsenetinternational.org/assets/PulseNet/uploads/pfge/PNL05_Ec-Sal-ShigPFGEprotocol.pdf.
- 26.Scheutz F., Teel L. D., Beutin L., et al. Multicenter evaluation of a sequence-based protocol for subtyping Shiga toxins and standardizing Stx nomenclature. Journal of Clinical Microbiology. 2012;50(9):2951–2963. doi: 10.1128/jcm.00860-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blanco M., Blanco J. E., Mora A., et al. Serotypes, virulence genes, and intimin types of Shiga toxin (verotoxin)-producing Escherichia coli isolates from cattle in Spain and identification of a new intimin variant gene (eae-xi) Journal of Clinical Microbiology. 2004;42(2):645–651. doi: 10.1128/jcm.42.2.645-651.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shringi S., García A., Lahmers K. K., et al. Differential virulence of clinical and bovine-biased enterohemorrhagic Escherichia coli O157:H7 genotypes in piglet and dutch belted rabbit models. Infection and Immunity. 2012;80(1):369–380. doi: 10.1128/iai.05470-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim J., Nietfeldt J., Ju J., et al. Ancestral divergence, genome diversification, and phylogeographic variation in subpopulations of sorbitol-negative, β-glucuronidase-negative enterohemorrhagic Escherichia coli O157. Journal of Bacteriology. 2001;183(23):6885–6897. doi: 10.1128/jb.183.23.6885-6897.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mellor G. E., Besser T. E., Davis M. A., et al. Multilocus genotype analysis of Escherichia coli O157 Isolates from Australia and the United States provides evidence of geographic divergence. Applied and Environmental Microbiology. 2013;79(16):5050–5058. doi: 10.1128/aem.01525-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leopold S. R., Magrini V., Holt N. J., et al. A precise reconstruction of the emergence and constrained radiations of Escherichia coli O157 portrayed by backbone concatenomic analysis. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(21):8713–8718. doi: 10.1073/pnas.0812949106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kawano K., Okada M., Haga T., Maeda K., Goto Y. Relationship between pathogenicity for humans and stx genotype in Shiga toxin-producing Escherichia coli serotype O157. European Journal of Clinical Microbiology and Infectious Diseases. 2008;27(3):227–232. doi: 10.1007/s10096-007-0420-3. [DOI] [PubMed] [Google Scholar]
- 33.Koitabashi T., Vuddhakul V., Radu S., et al. Genetic characterization of Escherichia coli O157:H7/- strains carrying the stx 2 gene but not producing shiga toxin 2. Microbiology and Immunology. 2006;50(2):135–148. doi: 10.1111/j.1348-0421.2006.tb03779.x. [DOI] [PubMed] [Google Scholar]
- 34.Koitabashi T., Cui S., Kamruzzaman M., Nishibuchi M. Isolation and characterization of the Shiga toxin gene (stx)-bearing Escherichia coli O157 and non-O157 from retail meats in Shandong Province, China, and characterization of the O157-derived stx2 phages. Journal of Food Protection. 2008;71(4):706–713. doi: 10.4315/0362-028x-71.4.706. [DOI] [PubMed] [Google Scholar]
- 35.Ramachandran V., Brett K., Hornitzky M. A., et al. Distribution of intimin subtypes among Escherichia coli isolates from ruminant and human sources. Journal of Clinical Microbiology. 2003;41(11):5022–5032. doi: 10.1128/jcm.41.11.5022-5032.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]


