Abstract
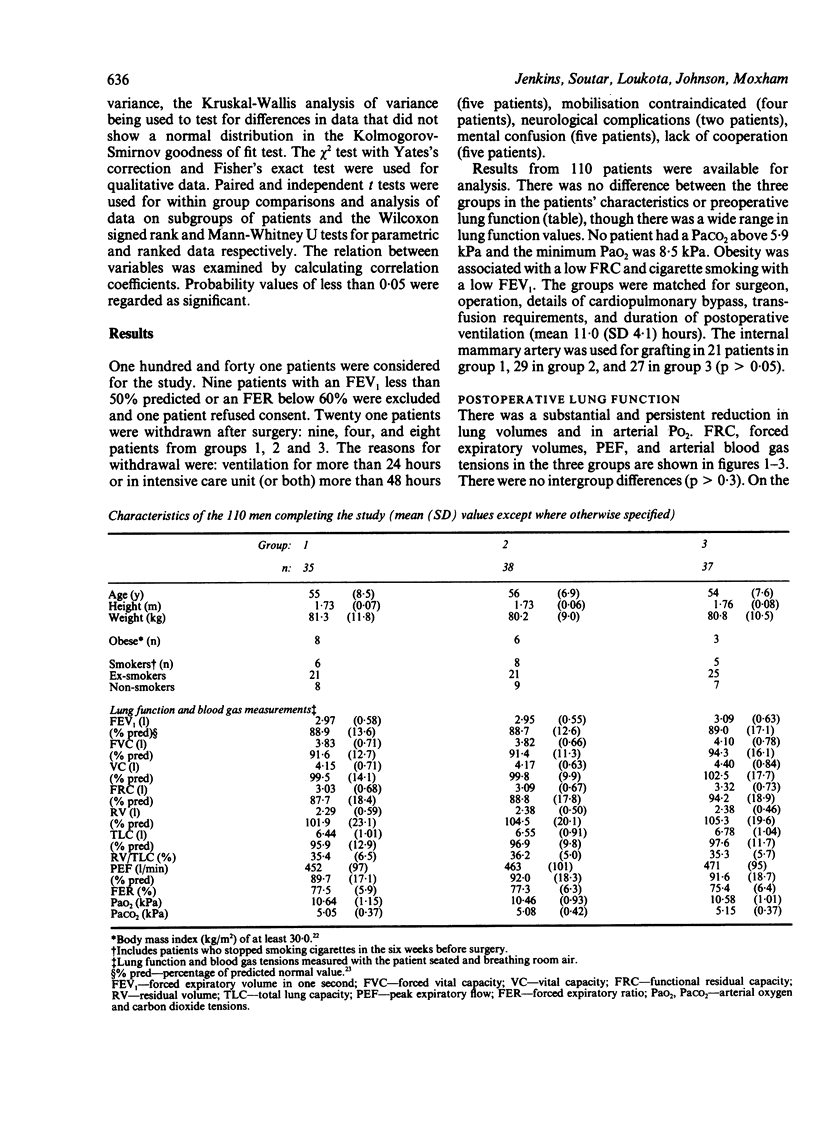
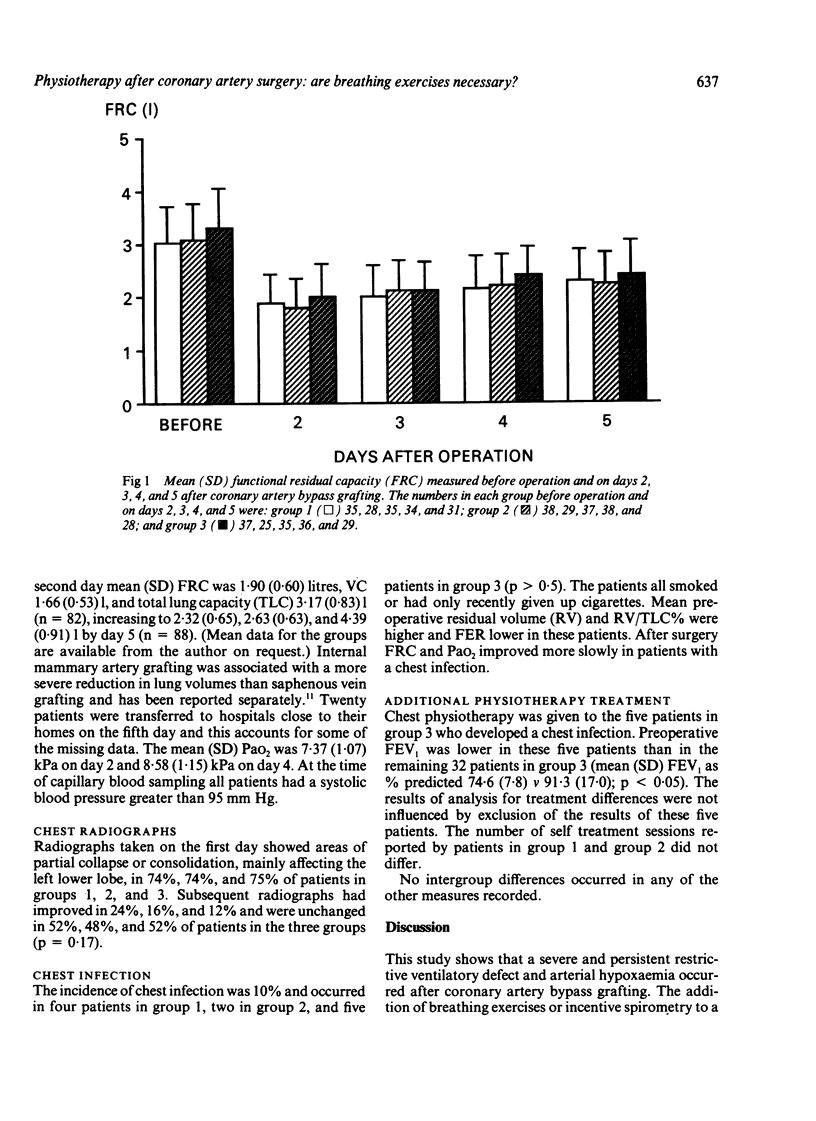
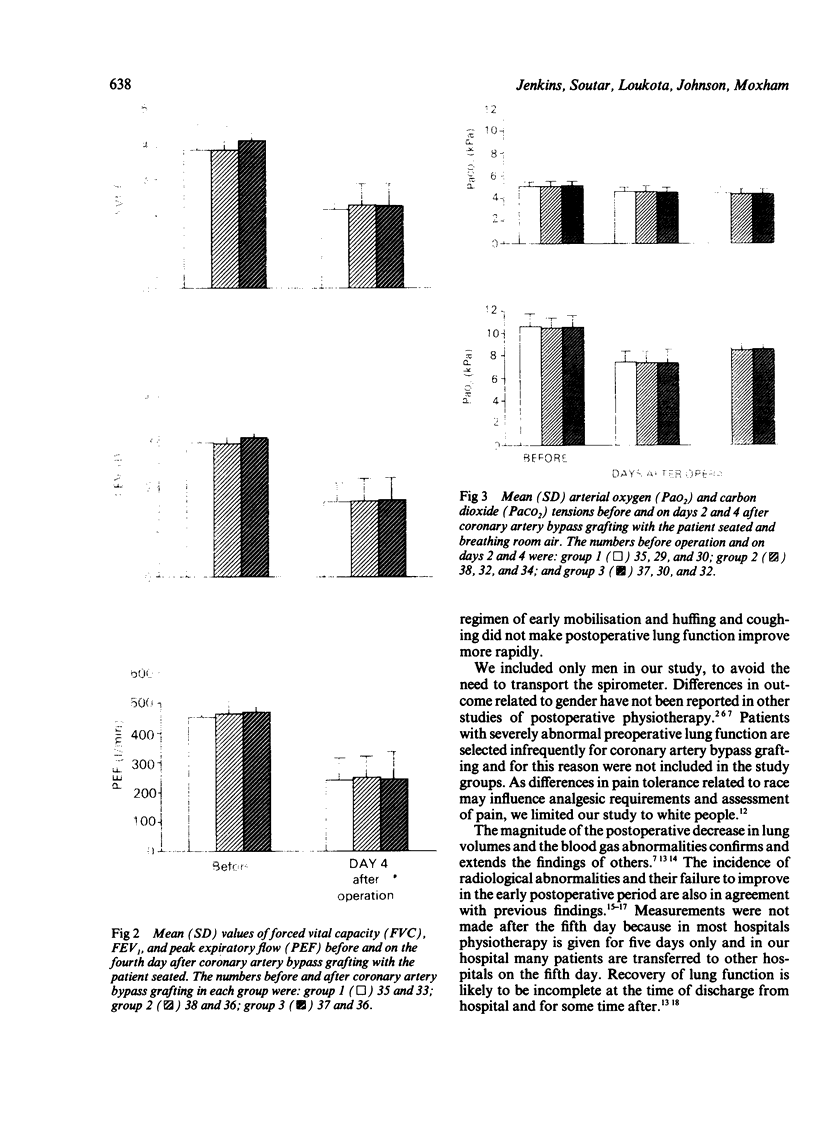
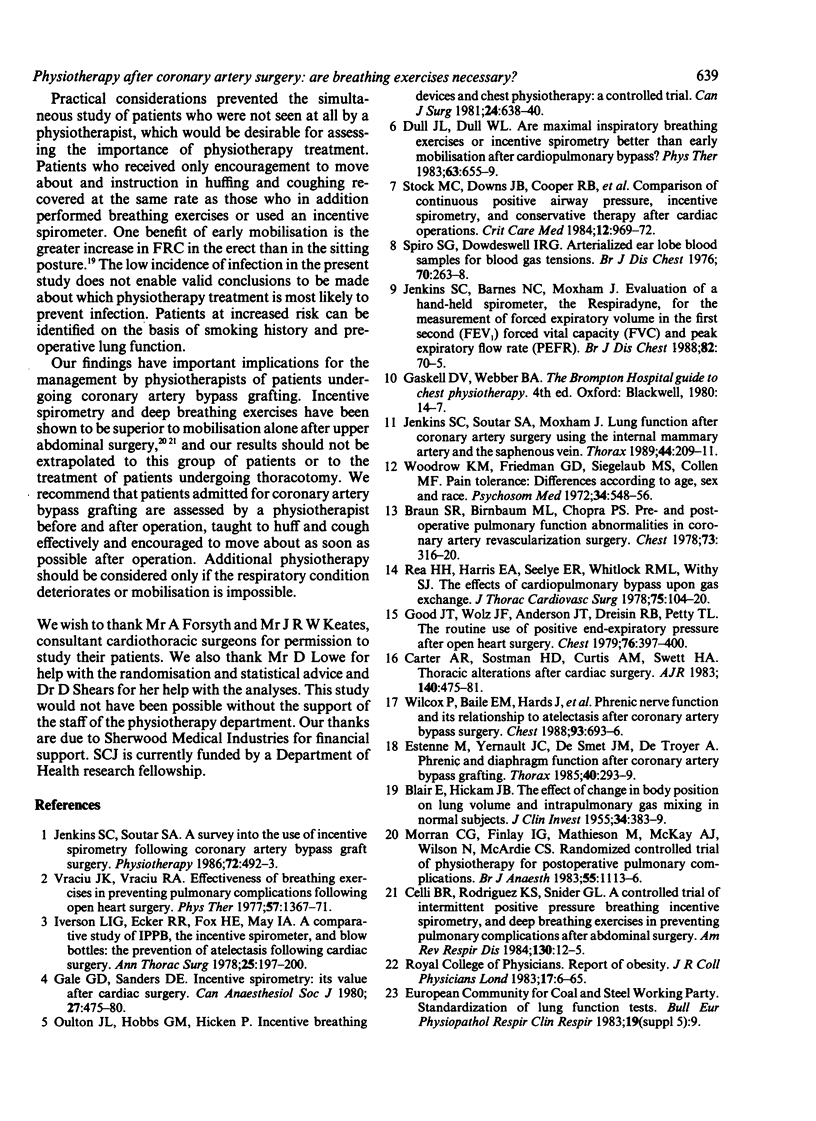
One hundred and ten men undergoing coronary artery bypass grafting took part in a prospective randomised study comparing three physiotherapy protocols. All patients were taught self supported huffing and coughing by a physiotherapist and encouraged to move about. This comprised the sole treatment for the 37 control patients (group 3). Additional physiotherapy included breathing exercises for the 35 patients in group 1 and use of an incentive spirometer for the 38 patients in group 2. Functional residual capacity (FRC) was measured daily at the bedside until the fifth postoperative day and arterial blood gas tensions were measured on the second and fourth postoperative days. After surgery patients developed a severe restrictive ventilatory defect and profound arterial hypoxaemia. There were no differences between the three groups. Mean FRC on day 2 was 1.90 litres (61% of the preoperative value), increasing to 2.32 1 by day 5 (76% of the preoperative value). The mean arterial oxygen tension was 7.37 kPa on day 2 and 8.58 kPa on day 4. Four patients in group 1, two in group 2, and five in group 3 developed a chest infection. It is concluded that the addition of breathing exercises or incentive spirometry to a regimen of early mobilisation and huffing and coughing confers no extra benefit after uncomplicated coronary artery bypass grafting.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BLAIR E., HICKAM J. B. The effect of change in body position on lung volume and intrapulmonary gas mixing in normal subjects. J Clin Invest. 1955 Mar;34(3):383–389. doi: 10.1172/JCI103086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun S. R., Birnbaum M. L., Chopra P. S. Pre- and postoperative pulmonary function abnormalities in coronary artery revascularization surgery. Chest. 1978 Mar;73(3):316–320. doi: 10.1378/chest.73.3.316. [DOI] [PubMed] [Google Scholar]
- Carter A. R., Sostman H. D., Curtis A. M., Swett H. A. Thoracic alterations after cardiac surgery. AJR Am J Roentgenol. 1983 Mar;140(3):475–481. doi: 10.2214/ajr.140.3.475. [DOI] [PubMed] [Google Scholar]
- Celli B. R., Rodriguez K. S., Snider G. L. A controlled trial of intermittent positive pressure breathing, incentive spirometry, and deep breathing exercises in preventing pulmonary complications after abdominal surgery. Am Rev Respir Dis. 1984 Jul;130(1):12–15. doi: 10.1164/arrd.1984.130.1.12. [DOI] [PubMed] [Google Scholar]
- Dull J. L., Dull W. L. Are maximal inspiratory breathing exercises or incentive spirometry better than early mobilization after cardiopulmonary bypass? Phys Ther. 1983 May;63(5):655–659. doi: 10.1093/ptj/63.5.655. [DOI] [PubMed] [Google Scholar]
- Dundee J. W. Abuse of benzodiazepines. Br J Anaesth. 1983 Jan;55(1):1–2. doi: 10.1093/bja/55.1.1. [DOI] [PubMed] [Google Scholar]
- Estenne M., Yernault J. C., De Smet J. M., De Troyer A. Phrenic and diaphragm function after coronary artery bypass grafting. Thorax. 1985 Apr;40(4):293–299. doi: 10.1136/thx.40.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale G. D., Sanders D. E. Incentive spirometry: its value after cardiac surgery. Can Anaesth Soc J. 1980 Sep;27(5):475–480. doi: 10.1007/BF03007047. [DOI] [PubMed] [Google Scholar]
- Good J. T., Jr, Wolz J. F., Anderson J. T., Dreisin R. B., Petty T. L. The routine use of positive end-expiratory pressure after open heart surgery. Chest. 1979 Oct;76(4):397–400. doi: 10.1378/chest.76.4.397. [DOI] [PubMed] [Google Scholar]
- Iverson L. I., Ecker R. R., Fox H. E., May I. A. A comparative study of IPPB, the incentive spirometer, and blow bottles: the prevention of atelectasis following cardiac surgery. Ann Thorac Surg. 1978 Mar;25(3):197–200. doi: 10.1016/s0003-4975(10)63521-7. [DOI] [PubMed] [Google Scholar]
- Jenkins S. C., Barnes N. C., Moxham J. Evaluation of a hand-held spirometer, the Respiradyne, for the measurement of forced expiratory volume in the first second (FEV1), forced vital capacity (FVC) and peak expiratory flow rate (PEFR). Br J Dis Chest. 1988 Jan;82(1):70–75. doi: 10.1016/0007-0971(88)90010-1. [DOI] [PubMed] [Google Scholar]
- Jenkins S. C., Soutar S. A., Forsyth A., Keates J. R., Moxham J. Lung function after coronary artery surgery using the internal mammary artery and the saphenous vein. Thorax. 1989 Mar;44(3):209–211. doi: 10.1136/thx.44.3.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oulton J. L., Hobbs G. M., Hicken P. Incentive breathing devices and chest physiopathy: a controlled therapy. Can J Surg. 1981 Nov;24(6):638–640. [PubMed] [Google Scholar]
- Rea H. H., Harris E. A., Seelye E. R., Whitlock R. M., Withy S. J. The effects of cardiopulmonary bypass upon pulmonary gas exchange. J Thorac Cardiovasc Surg. 1978 Jan;75(1):104–120. [PubMed] [Google Scholar]
- Spiro S. G., Dowdeswell I. R. Arterialized ear lobe blood samples for blood gas tensions. Br J Dis Chest. 1976 Oct;70(4):263–268. doi: 10.1016/0007-0971(76)90042-5. [DOI] [PubMed] [Google Scholar]
- Stock M. C., Downs J. B., Cooper R. B., Lebenson I. M., Cleveland J., Weaver D. E., Alster J. M., Imrey P. B. Comparison of continuous positive airway pressure, incentive spirometry, and conservative therapy after cardiac operations. Crit Care Med. 1984 Nov;12(11):969–972. doi: 10.1097/00003246-198411000-00010. [DOI] [PubMed] [Google Scholar]
- Vraciu J. K., Vraciu R. A. Effectiveness of breathing exercises in preventing pulmonary complications following open heart surgery. Phys Ther. 1977 Dec;57(12):1367–1371. doi: 10.1093/ptj/57.12.1367. [DOI] [PubMed] [Google Scholar]
- Wilcox P., Baile E. M., Hards J., Müller N. L., Dunn L., Pardy R. L., Paré P. D. Phrenic nerve function and its relationship to atelectasis after coronary artery bypass surgery. Chest. 1988 Apr;93(4):693–698. doi: 10.1378/chest.93.4.693. [DOI] [PubMed] [Google Scholar]
- Woodrow K. M., Friedman G. D., Siegelaub A. B., Collen M. F. Pain tolerance: differences according to age, sex and race. Psychosom Med. 1972 Nov-Dec;34(6):548–556. doi: 10.1097/00006842-197211000-00007. [DOI] [PubMed] [Google Scholar]