Abstract
Reactive oxygen species (ROS) have been implicated in a wide variety of disorders ranging between traumatic, infectious, inflammatory, and malignant diseases. ROS are involved in inflammation-induced oxidative damage to cellular components including regulatory proteins and DNA. Furthermore, ROS have a major role in carcinogenesis and disease progression in the myeloproliferative neoplasms (MPNs), where the malignant clone itself produces excess of ROS thereby creating a vicious self-perpetuating circle in which ROS activate proinflammatory pathways (NF-κB) which in turn create more ROS. Targeting ROS may be a therapeutic option, which could possibly prevent genomic instability and ultimately myelofibrotic and leukemic transformation. In regard to the potent efficacy of the ROS-scavenger N-acetyl-cysteine (NAC) in decreasing ROS levels, it is intriguing to consider if NAC treatment might benefit patients with MPN. The encouraging results from studies in cystic fibrosis, systemic lupus erythematosus, and chronic obstructive pulmonary disease warrant such studies. In addition, the antioxidative potential of the widely used agents, interferon-alpha2, statins, and JAK inhibitors, should be investigated as well. A combinatorial approach using old agents with anticancer properties together with novel JAK1/2 inhibitors may open a new era for patients with MPNs, the outlook not only being “minimal residual disease” and potential cure but also a marked improvement in inflammation-mediated comorbidities.
1. Introduction
The Philadelphia negative chronic myeloproliferative neoplasms (MPNs) encompass essential thrombocythemia (ET), polycythemia vera (PV), and myelofibrosis (MF). These neoplasms arise due to an acquired stem cell lesion with subsequent clonal evolution being driven by several mutations, including the highly prevalent JAK2V617F somatic mutation in PV (in >95%, and in about 50% of patients with ET and PMF, resp.) and the CALR and MPL somatic mutations [1–9]. These mutations are virtually mutually exclusive and are all considered “second hits” or “driving mutations” within the MPNs whereas the primary genetic hit or “founding mutation” remains unknown [4].
Common clinical denominators for the MPNs are high rates of thrombohemorrhagic complications, hypermetabolic symptoms, splenomegaly, uncontrolled myeloproliferation, low-grade chronic inflammation, a massive inflammation-mediated comorbidity burden, and immune-deregulation [10–16]. The MPNs have an inherent propensity to progress in a biological continuum from early cancer stages (ET/PV) to more advanced cancer stages (MF or acute myeloid leukemia (AML)) [17, 18]. The concept of such a biological continuum is being increasingly recognized and supported by clinical and molecular studies, the latter displaying increasing JAK2V617F allelic burden throughout the stages. The fact that a JAK2 positive phenotype only persists in 20–50% of the cases when MPNs transform to AML (or even develops biphenotypic AML) also demonstrates the inherent risk of subclone formation which is a characteristic shared by many other cancers [19–23]. Consequently, the malignant clones are heterogeneous and thus difficult to target with chemotherapy, accounting for the inferior survival in MPN associated AML compared to de novo AML [24–26].
The MPNs have recently been described as “A Human Inflammation Model,” in which the fuel that feeds the fire is low-grade chronic inflammation [27]. The hypothesis is that the MPN—with uncontrolled myeloproliferation and uncontrolled cytokine secretion as a consequence of constitutively activated JAK-STAT signalling—by itself creates a proinflammatory milieu in the bone marrow and in the circulation. This proinflammatory milieu founds increasing genomic instability accounting for the propensity of the MPNs to acquire new mutations facilitating clonal evolution and ultimately progression to myelofibrosis and AML. It also links the MPNs with a heavy inflammation-mediated comorbidity burden, including premature atherosclerosis, other inflammatory diseases, and second cancers [22, 27–38]. In this context, it has been known for several years that chronic inflammation per se increases the risk of cancer development, solid as well as hematological, but the major questions in MPNs are, among others, how low-grade inflammation is eliciting genomic instability and clonal evolution and how the founding clone evades the immune system.
In MPNs, the optimal therapeutic goals are to normalize peripheral blood counts, minimize symptoms, prevent vascular complications, restore bone marrow architecture/morphology, and eliminate the risk of progression to MF or evolution to AML. It is crucial to acknowledge that the majority of ET and PV patients have long life-expectancies and therefore treatment related toxicities and long-term side effects influence treatment options [39–42]. The therapeutic agents display striking differences. Treatment with interferon-alpha2 (IFN) has been used successfully for decades, demonstrating its ability to normalize blood counts in the majority of patients, to reduce the JAK2V617F (and CALR) allelic burden, and to restore bone marrow morphology and induce major molecular remission in a subset of patients [43–55]. Because of the immune-enhancing properties, some patients experience autoimmune phenomena, primarily thyroiditis, during IFN treatment. A subset of patients also experiences symptoms similar to those arising in patients with systemic inflammation, including chronic fatigue, flue-like symptoms with low-grade fever, weight loss, and depression all symptoms being associated with chronic inflammation [56–58]. Despite undisputed hematological efficacy and safety being shown in a large number of single-arm IFN studies, similar results obtained from large randomized studies between IFN and the most widely used cytoreductive agent in MPNs, hydroxyurea, are still lacking. Most MPN experts agree that HU increases the risk of skin cancer and concern is increasing in regard to its potential of inducing AML after long-term use (>10 years) [59–64]. With the introduction of JAK inhibitors, the therapeutic landscape has expanded considerably. However, these novel agents potently suppress virtually all immune cells including NK-cells, CD4+ T-cells (Th1 and Th17), regulatory T-cells, macrophages, and dendritic cells (DCs) with ensuing impairment of immune regulation and consequently an increased risk of infections [65–71]. This risk is well documented and involves mainly urinary tract infections and herpes zoster but also more rare infections such as tuberculosis, toxoplasmosis, and progressive multifocal leukoencephalopathy [72–76]. Although patients are exposed to an increased risk of infections during treatment with JAK1/2 inhibitors, this novel treatment modality has definitely demonstrated its efficacy in terms of improvement of quality of life due to a rapid resolution of constitutional symptoms within days in concert with a marked reduction in symptomatic splenomegaly within the next weeks or months in the large majority of patients with myelofibrosis [77–80]. To this end, JAK1/2 inhibition in myelofibrosis is associated with an improved overall survival as well [81, 82]. The impact of JAK1/2 inhibition on symptom burden and splenomegaly in myelofibrosis is considered to be driven mainly by its pronounced anti-inflammatory efficacy as evidenced by a marked reduction in several proinflammatory cytokines during JAK-inhibition therapy [77, 83]. In this regard, the improved survival in ruxolitinib-treated MF patients is likely mainly explained by an improvement in inflammation-mediated comorbidities as well [84]. However, ruxolitinib has failed to demonstrate significant impact on the JAK2 clone [85] which substantiates the need for combinatorial approaches when treating MPNs [28].
Taking into account that chronic inflammation with the production of reactive oxygen species (ROS) may have an important role for the development and progression of MPNs—likely being a very potent driver of clonal evolution and mutagenesis in a vicious self-perpetuating circle—we herein will discuss the role of ROS in MPN pathogenesis and its impact upon comorbidity burden, immune regulation, and disease progression [27, 29, 86–90].
2. Reactive Oxygen Species
Reactive oxygen species (ROS) are a group of oxygen-containing molecules involved in many biological processes including normal cellular signalling and immune defence. Consequently, lacking the ability to produce ROS results in organ dysfunction and disease as evidenced by, for example, chronic granulomatous disease in which the immune system is unable to combat invading bacteria and fungi due to impaired production of ROS by neutrophils [91–95]. However, the same ROS compounds are also involved in several inflammation-driven diseases where an excess of ROS production is thought to account for the tissue damage, dysfunction, and fibrosis associated with the diseases [96, 97]. In addition, elevated levels of ROS, often referred to as oxidative stress, have a major role in cancer development, both in solid tumors and in hematological malignancies [86–90, 97]. There is no clear cut-off that defines exactly which compounds are to be included in the ROS category, and often nonoxygen molecules buffering ROS levels are also included in the analysis of cellular oxidative status. The molecules superoxide (O2 −) and hydrogen-peroxide (H2O2) are obvious ROS, but intracellular levels of glutathione and reduced glutathione are also crucial in the cellular redox interplay. Hydrogen-peroxide is of particular interest since it can freely diffuse across cellular membranes and interact with cells in close proximity to the H2O2 producing cells. This includes the endothelial cells within the intima of artery walls, and oxidative stress has already been linked to cardiovascular diseases, especially the development of premature atherosclerosis in chronic inflammatory diseases [96, 98–100]. H2O2 has been shown to activate NF-κB pathway, thus creating self-perpetuating vicious circles in which inflammation creates ROS which in turn creates more inflammation [101–103]. To avoid such situations, the system has a fail-safe: suppressors of cytokine signalling (SOCS), a family of proteins dedicated to creating negative feedback loops. They are normally activated by inflammatory mediators such as IFN, IL-4, TNF-alpha, and H2O2 [104, 105]. Activated SOCS proteins bind to JAKs disrupting the JAK-STAT pathway, thereby ensuring that the inflammatory process is not being sustained. However, in MPNs, this pathway is constitutively activated and the much warranted SOCS brake is overruled. Furthermore, aberrant methylation of SOCS-coding DNA and consequent dysregulation of SOCS have also been reported in MPNs [106, 107].
3. Hepatitis C as a Model of Inflammation-Mediated Fibrosis and Cancer Development: Similarities to MPNs as “A Human Inflammation Model for Cancer Development”
The initiating event in hepatitis C is a viral infection. This results in chronic inflammation, increased production of ROS and consequently oxidative stress, inability of the immune system to clear the infected cells, an increased risk of progression to terminal cirrhosis, and ultimately an increased risk of developing hepatocellular carcinoma (HCC) or lymphoma [108–113]. In MPNs, the initiating event is unknown, but after acquisition of the JAK2 mutation, MPNs (much like hepatitis patients) exhibit evidence of low-grade chronic inflammation with ensuing fibrosis and bone marrow failure in addition to an increased risk of developing AML. Another similarity is the inability of the host immune system to identify and clear the fundamental problem, for example, the malignant clone in regard to MPNs. Another striking similarity is the existence of a common effective treatment modality: the very potent immune-enhancing, antiviral agent IFN which has been used successfully for decades in hepatitis patients as well as in MPN patients. In this regard, it has recently been hypothesized that a virus infection (e.g., human retrovirus) might be implicated in MPN pathogenesis [27, 114]. It is also of particular interest to note that oxidative stress has been implicated in the therapeutic response. Thus, it was demonstrated, that increasing levels of ROS disrupt IFN signalling, thus counteracting therapy [115].
4. ROS and MPNs
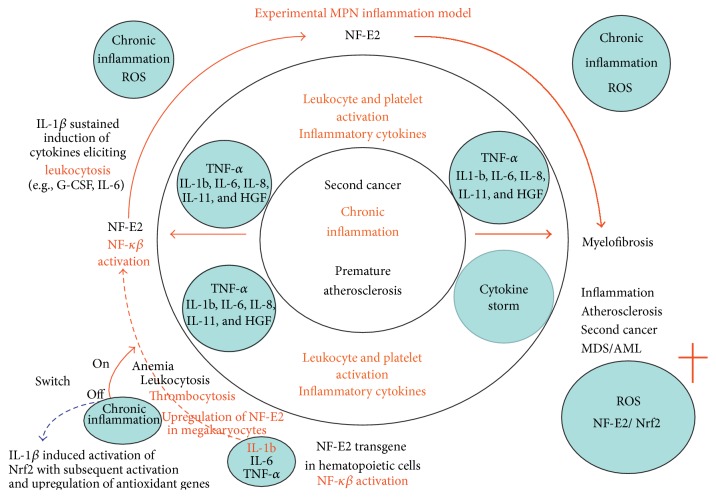
The ROS molecules are produced mainly by neutrophils, macrophages, and monocytes. In the context of MPNs, this is crucial, since the MPN cells are clonal and autonomously dysregulated and have been shown to produce excessive ROS in vitro [87]. Furthermore, MPN patients demonstrate elevated levels of ROS in vivo [86, 116]. An increased ROS production has been observed in other cancers, and in some cases the cancer cells express catalase (the enzyme that metabolizes H2O2) in excess and in addition produce large amounts of H2O2. In this way, the malignant clone itself avoids the toxic effects of H2O2 and suppresses the neighbouring healthy cells (ROS induce apoptosis in healthy cells) thereby facilitating clonal expansion [117–126]. This mechanism has not yet been established in MPNs but certainly warrants further investigation, especially since the excessive ROS production in MPNs gives rise to a proliferative advantage to JAK2 positive clones [28, 87, 127, 128] (Figure 1). In this regard, the model proposed by Marty et al. is in agreement with the MPN inflammation model and excessive ROS accumulation in a vicious self-perpetuating circle. In this context, considering the role of NF-E2 in MPN disease pathogenesis, it is intriguing to speculate if NF-E2 may contribute in driving the vicious inflammation wheel, including ROS accumulation as most recently discussed [29, 129–134]. On the other hand, it has also been demonstrated that the hematopoietic stem cell niche (HSC) in MPNs downregulates catalase activity resulting in an increase in oxidative DNA damage (8-oxo-G) and subsequent double-stranded- (ds-) DNA breaks, a widely accepted measure of ROS induced DNA damage, and perhaps in this way induces instability of the HSC niche [87].
Figure 1.
Sustained NF-E2 expression likely elicits a pronounced oxidative stress milieu with excessive ROS giving rise to myeloid expansion with leukocytosis and excessive thrombocytosis and inflammation-mediated in vivo activation of leukocytes and platelets, thereby further promoting a sustained, self-perpetuating release of inflammatory products. In this vicious circle, an oxidative stress burden with NF-E2 domination over Nrf2 promotes ROS accumulation and megakaryocytic differentiation. Increasing oxidative stress-induced DNA damage of hematopoietic stem cells (HSCs) elicits genomic instability and clonal MPN evolution with accumulation of mutations ultimately terminating in myelofibrotic and leukemic transformation. A relative deficiency of Nrf2 may also result in expansion of the HSC and progenitor cell compartment and ultimately migration of HSCs from their stem cell niches into the circulation (“leaving the burning nest”) to seed in the spleen and liver (myelofibrosis with myeloid metaplasia). The vicious circle may be locked by early intervention with interferon-alpha2 (stopping the fuel to the fire) in combination with a JAK1-2 inhibitor (e.g., ruxolitinib) and a statin, the latter agents “cooling down the system” by their highly potent anti-inflammatory properties which may actually be enhanced (synergism) when being administered simultaneously. With permission from Leukemia Research [29].
In a mouse model, ds-DNA breaks were shown to be a consequence of ROS accumulation, and it was also shown that the CD34+ HSCs themselves produced this excess ROS, probably as a consequence of catalase downregulation [87, 127]. Furthermore, a functional lack of superoxide dismutase (SOD) activity could also be of importance. ROS negatively influence the AKT pathway, which in turn influences Forkhead O/FoxO which regulates the transcription of several antioxidative defence pathways, including GPx, catalase, and SOD [135]. These mice developed aggressive PV phenotype but when they were treated with the potent ROS-scavenger molecule n-acetyl-cysteine (NAC) they developed normal phenotype, demonstrating the direct role in MPN disease development and disease progression [87]. This was substantiated by the finding that NAC treatment of the PV phenotype mice delayed progression to MF phenotype when compared to nontreated mice.
The damaging effects of ROS (besides the proliferative advantage) are also attributed to the consequent oxidation of lipids, proteins, and, most importantly, the ds-DNA breaks due to oxidation. In healthy cells, this insult will be rapidly repaired but a hallmark of most cancers is a defective DNA repair (sometimes even induced by therapy, e.g., hydroxyurea). Furthermore, the response to DNA damage is also affected as demonstrated by the negatively regulated p53 pathway in MPNs [136]. This is also demonstrated in MPNs, where the CHEK2 germline mutations, which are associated with ET and PV, account for an increased risk of developing an MPN. Together with other proteins, the CHEK2 proteins are associated with DNA damage and binding of TP53 (p53) and CHEK2 are involved in many cancers [137–143]. Consequently, harbouring this CHEK2 mutation can result in inadequate DNA repair and consequently increased risk of developing (and sustaining) genetic hits in several cancer types. It is intriguing to consider if germline CHEK2 mutation accounts for the initial genetic instability in some MPN patients. In time and by “chance” this might result in a somatic JAK2 mutation with ensuing increased production of ROS, clonal expansion, and increasing genomic instability due to ineffective DNA repair and an increase in ROS induced DNA damage, all of which further facilitate disease progression with subclone formation and inflammation-mediated bone marrow fibrosis. The role of chronic inflammation and ROS in MPN pathogenesis has most recently been substantiated in a mouse model, in which mice were exposed to the highly potent inflammatory compound, formaldehyde (FA), by inhalation [144]. This agent induced bone marrow toxicity with typical MPN-like alterations in the mice, including an increased number of megakaryocytes and myelofibrosis in concert with the development of anemia, leukopenia, and thrombocythemia. Highly interestingly, these changes were accompanied by evidence of oxidative stress and inflammation in the bone marrow as assessed by significant increases in ROS levels, increased NF-κB activity at both mRNA and protein levels, and significant increases in the inflammatory markers, TNF-alpha and IL-1beta, as well [144]. These observations are in accordance with studies demonstrating that oxidative stress in hematopoietic stem cells can lead to DNA damage, premature senescence, and loss of stem cell function [145]. Accordingly, all together these findings are supportive of the concept that chronic inflammation by induction of oxidative stress and an inflammatory bone marrow microenvironment may give rise to DNA damage and likely an impaired stem cell function with ensuing development of myelofibrosis.
In hepatitis, it has been demonstrated, that the excess of ROS and consequent oxidative stress inhibits IFN signalling, thus counteracting the normal immunosurveillance by NK-cells and CD8+ cytotoxic T-cells (CTLs) [115]. The reduced IFN signalling and ensuing reduction of MHC-I expression by virally infected cells provide an escape route from the innate and adaptive immunosurveillance. A prerequisite of this model is that the MHC-I expression is low enough to avoid CTL activation by antigen recognition, but also high enough to avoid “missing self” activation of NK-cells. This model deserves to be tested in MPNs to elucidate if increased ROS levels might facilitate both clonal expansion and immune evasion, implying ROS-mediated inhibition of IFN signalling and the immune evasion to exhibit dual actions. In this regard, reduced MHC-I expression might keep the tumor below detection limit of CTLs, and even if a tumor cell is indeed detected, probably due to threshold expression of “self” by MHC-I, the consequent IFN signalling from the activated NK-cell will likely have only a limited impact since the pathway is functionally blocked by excess of ROS. By this mechanism, recruitment and activation of other immune cells, in particular macrophages, may be inhibited and the immune response remains unamplified and thus ineffective in combating the clone. This concept is partly supported by the finding of downregulation of HLA expression in ET, PV, and MF and further supported by efficacious treatment with IFN, which increases MHC-I expression of the clonal cells (thus making them “legitimate” targets for CTLs) but also increases the NK-cell compartment, thus inducing the much warranted amplification of the immune system. IFN also mobilizes dormant stem cells rendering them susceptible to targeted therapies [146–149].
Since ROS appear to play a crucial role in disease progression of MPNs, the targeting of ROS seems intuitive, especially since the increased ROS can interfere with both endogenous tumor surveillance and treatment response. Treatment with NAC has been used successfully in an in vivo mouse model after JAK2V617F bone marrow transplant, but never in human MPN subjects. The majority of experiences with human NAC treatment are based on the treatment of patients suffering from paracetamol poisoning. In this setting, the NAC treatment is intensive and of short duration. NAC treatment has also been investigated in spinal cord injuries but again the treatment duration is short [150–153]. However, longer exposure has been investigated in chronic pulmonary diseases: chronic obstructive pulmonary disease (COPD) and cystic fibrosis (CF). Both diseases have a significant inflammatory component, and both diseases showed positive responses to NAC treatment with fewer exacerbations (COPD) and more stable lung function (CF) in the NAC-treated groups [154–156]. Similar results were obtained in patients suffering from systemic lupus erythematosus (SLE) [157].
In order to target MPN related oxidative stress, it is important to acknowledge that the optimal level of ROS is not known. In the experimental MPN models, treatment with NAC almost totally removed any existing ROS, which in an experimental model might give satisfying results but in a human trial might result in a dismal outcome [87, 127]. In vivo, ROS are needed to some extent to ensure normal cellular signalling and to enable the immune system in combating invading bacteria and an obvious problem might be an increase in infectious diseases and (other) neoplastic diseases. However, this has not been identified so far with NAC treatment of COPD and CF, both diseases otherwise heavily burdened by (chronic) infections and the NAC treatment resulted in disease relevant improvements.
5. Discussion and Perspectives
The MPNs are clonal neoplasms intimately associated with a dysregulated immune system [16, 17, 148, 149, 158–160]. As in many other diseases, inflammation and excess generation of ROS are thought to play a major role, both in disease initiation and associated inflammation-mediated comorbidities [27, 28, 84, 135]. The initiation of disease is probably a consequence of defective DNA repair and/or increased acquisition of DNA damage. This could be caused by many factors, for example, germline CHEK2 mutation [142, 143]. Of note, it is also intriguing to consider that the initiation of the disease might be consequent to a “fertile ground” changing the fitness of the stem cell niche for a preexisting abnormal hematopoietic stem cell [4, 161–163]. By chance, the JAK2 mutation is acquired and consequent generation of ROS with clonal expansion and evolution due to genomic instability characterizes the further course of the disease. ROS are also involved in cardiovascular diseases which are major contributors to the comorbidity burden and mortality in MPN patients [11, 15, 96, 98, 99]. Accordingly, the targeting of ROS is an obvious therapeutic option, especially since one of the main goals is to prevent genomic instability, likely facilitated by increased ROS, and thereby ultimately fibrotic and leukemic transformation. In regard to the potent efficacy of NAC in decreasing ROS levels, it is intriguing to consider if NAC treatment might benefit patients with MPNs. The encouraging results from studies in CF, SLE, and COPD warrant such studies.
Furthermore, the antioxidative potential of the widely used agents, IFN, JAK inhibitors, and statins, both as monotherapies and in various combinations, should be investigated. Studies on combinations with IFN, the only agent with the potential to induce “minimal residual disease,” as the backbone and “old antioxidative drugs” (statins, NAC) and the novel JAK1/2-inhibitors are urgently needed. Such studies may further enhance the potency of the novel combination therapy with IFN and ruxolitinib, a concept which already has been shown to be highly efficacious in patients with PV and hyperproliferative MF, implying an improvement in inflammation-mediated comorbidities as well [28, 84, 164]. Such a combinatorial approach using old agents (statins, NAC, and IFN) with anticancer properties (antiproliferative, proapoptotic, antiangiogenic, anti-inflammatory, and antioxidative properties) together with novel JAK1/2 inhibitors may open a new era for patients with MPNs, the outlook not only being “minimal residual disease” and potential cure but also a marked improvement in inflammation-mediated comorbidities. These goals will not only set new standards for treatment of MPNs in the future but may also likely be highly cost-effective when considering the potential of decreasing dosages of very expensive drugs (JAK1/2 inhibitors/ IFN) due to synergism between them and for example, statins, and therefore a reduction in side effects of single agents as well [27, 28, 165–168]. This novel treatment concept, targeting the oxidative stress mechanisms in MPNs, is foreseen to alleviate the heavy disease burden, which encompasses not only an increased risk of severe cardiovascular complications and second cancers but likely also an increased risk of premature atherosclerosis (early ageing?) [28, 29, 135]. By eliminating the oxidative stress overload, improving the defective antioxidative stress defence, and improving “Tumor Immune Surveillance” according to the novel treatment concept as outlined above, we are convinced that the future will look bright for our patients and will enlighten new horizons.
Acknowledgments
Mads Emil Bjørn and Hans Carl Hasselbalch wrote and edited the entire paper.
Conflict of Interests
Mads Emil Bjørn has received partial funding for his Ph.D. study from Novartis Oncology. Hans Carl Hasselbalch has received research grants from Novartis Oncology.
References
- 1.Baxter E. J., Scott L. M., Campbell P. J., et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. The Lancet. 2005;365(9464):1054–1061. doi: 10.1016/S0140-6736(05)71142-9. [DOI] [PubMed] [Google Scholar]
- 2.James C., Ugo V., Le Couédic J.-P., et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature. 2005;434(7037):1144–1148. doi: 10.1038/nature03546. [DOI] [PubMed] [Google Scholar]
- 3.Nangalia J., Massie C. E., Baxter E. J., et al. Somatic CALR mutations in myeloproliferative neoplasms with nonmutated JAK2. The New England Journal of Medicine. 2013;369(25):2391–2405. doi: 10.1056/nejmoa1312542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cazzola M., Kralovics R. From Janus kinase 2 to calreticulin: the clinically relevant genomic landscape of myeloproliferative neoplasms. Blood. 2014;123(24):3714–3719. doi: 10.1182/blood-2014-03-530865. [DOI] [PubMed] [Google Scholar]
- 5.Tefferi A., Thiele J., Vannucchi A. M., Barbui T. An overview on CALR and CSF3R mutations and a proposal for revision of WHO diagnostic criteria for myeloproliferative neoplasms. Leukemia. 2014;28(7):1407–1413. doi: 10.1038/leu.2014.35. [DOI] [PubMed] [Google Scholar]
- 6.Tefferi A. Novel mutations and their functional and clinical relevance in myeloproliferative neoplasms: JAK2, MPL, TET2, ASXL1, CBL, IDH and IKZF1. Leukemia. 2010;24(6):1128–1138. doi: 10.1038/leu.2010.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Langabeer S. E., Andrikovics H., Asp J., et al. Molecular diagnostics of myeloproliferative neoplasms. European Journal of Haematology. 2015 doi: 10.1111/ejh.12578. [DOI] [PubMed] [Google Scholar]
- 8.Campbell P. J., Baxter E. J., Beer P. A., et al. Mutation of JAK2 in the myeloproliferative disorders: timing, clonality studies, cytogenetic associations, and role in leukemic transformation. Blood. 2006;108(10):3548–3555. doi: 10.1182/blood-2005-12-013748. [DOI] [PubMed] [Google Scholar]
- 9.Larsen T. S., Christensen J. H., Hasselbalch H. C., Pallisgaard N. The JAK2 V617F mutation involves B- and T-lymphocyte lineages in a subgroup of patients with Philadelphia-chromosome negative chronic myeloproliferative disorders. British Journal of Haematology. 2007;136(5):745–751. doi: 10.1111/j.1365-2141.2007.06497.x. [DOI] [PubMed] [Google Scholar]
- 10.Finazzi G., Rambaldi A., Guerini V., Carobbo A., Barbui T. Risk of thrombosis in patients with essential thrombocythemia and polycythemia vera according to JAK2 V617F mutation status. Haematologica. 2007;92(1):135–136. doi: 10.3324/haematol.10634. [DOI] [PubMed] [Google Scholar]
- 11.Barbui T., Carobbio A., Finazzi G., et al. Inflammation and thrombosis in essential thrombocythemia and polycythemia vera different role of C-reactive protein and pentraxin 3. Haematologica. 2011;96(2):315–318. doi: 10.3324/haematol.2010.031070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barbui T., Finazzi G., Falanga A. Myeloproliferative neoplasms and thrombosis. Blood. 2013;122(13):2176–2184. doi: 10.1182/blood-2013-03-460154. [DOI] [PubMed] [Google Scholar]
- 13.Andersen C. L., Bjørn M. E., McMullin M. F., et al. Circulating YKL-40 in patients with essential thrombocythemia and polycythemia vera treated with the novel histone deacetylase inhibitor vorinostat. Leukemia Research. 2014;38(7):816–821. doi: 10.1016/j.leukres.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Bjørn M. E., Andersen C. L., Jensen M. K., Hasselbalch H. C. Circulating YKL-40 in myelofibrosis a potential novel biomarker of disease activity and the inflammatory state. European Journal of Haematology. 2014;93(3):224–228. doi: 10.1111/ejh.12332. [DOI] [PubMed] [Google Scholar]
- 15.Marchioli R., Finazzi G., Specchia G., et al. Cardiovascular events and intensity of treatment in polycythemia vera. The New England Journal of Medicine. 2013;368(1):22–33. doi: 10.1056/nejmoa1208500. [DOI] [PubMed] [Google Scholar]
- 16.Barosi G. An immune dysregulation in MPN. Current Hematologic Malignancy Reports. 2014;9(4):331–339. doi: 10.1007/s11899-014-0227-0. [DOI] [PubMed] [Google Scholar]
- 17.Skov V., Thomassen M., Riley C. H., et al. Gene expression profiling with principal component analysis depicts the biological continuum from essential thrombocythemia over polycythemia vera to myelofibrosis. Experimental Hematology. 2012;40(9):771.e19–780.e19. doi: 10.1016/j.exphem.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 18.Vannucchi A. M., Pieri L., Guglielmelli P. JAK2 allele burden in the myeloproliferative neoplasms: effects on phenotype, prognosis and change with treatment. Therapeutic Advances in Hematology. 2011;2(1):21–32. doi: 10.1177/2040620710394474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tefferi A., Guglielmelli P., Larson D. R., et al. Long-term survival and blast transformation in molecularly annotated essential thrombocythemia, polycythemia vera, and myelofibrosis. Blood. 2014;124(16):2507–2513. doi: 10.1182/blood-2014-05-579136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beer P. A., Delhommeau F., LeCouédic J.-P., et al. Two routes to leukemic transformation after a JAK2 mutation-positive myeloproliferative neoplasm. Blood. 2010;115(14):2891–2900. doi: 10.1182/blood-2009-08-236596. [DOI] [PubMed] [Google Scholar]
- 21.Dong X.-F., Yue L.-Z., Fu R., Shao Z.-H. Polycythemia vera transforming to myelofibrosis and then biphenotype acute leukemia. Clinical Laboratory. 2014;60(3):495–499. doi: 10.7754/Clin.Lab.2013.130339. [DOI] [PubMed] [Google Scholar]
- 22.Kristinsson S. Y., Landgren O., Samuelsson J., Björkholm M., Goldin L. R. Autoimmunity and the risk of myeloproliferative neoplasms. Haematologica. 2010;95(7):1216–1220. doi: 10.3324/haematol.2009.020412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Theocharides A., Boissinot M., Girodon F., et al. Leukemic blasts in transformed JAK2-V617F-positive myeloproliferative disorders are frequently negative for the JAK2-V617F mutation. Blood. 2007;110(1):375–379. doi: 10.1182/blood-2006-12-062125. [DOI] [PubMed] [Google Scholar]
- 24.Kundranda M. N., Tibes R., Mesa R. A. Transformation of a chronic myeloproliferative neoplasm to acute myelogenous leukemia: does anything work? Current Hematologic Malignancy Reports. 2012;7(1):78–86. doi: 10.1007/s11899-011-0107-9. [DOI] [PubMed] [Google Scholar]
- 25.Mesa R. A., Li C.-Y., Ketterling R. P., Schroeder G. S., Knudson R. A., Tefferi A. Leukemic transformation in myelofibrosis with myeloid metaplasia: a single-institution experience with 91 cases. Blood. 2005;105(3):973–977. doi: 10.1182/blood-2004-07-2864. [DOI] [PubMed] [Google Scholar]
- 26.Heaney M. L., Soriano G. Acute myeloid leukemia following a myeloproliferative neoplasm: clinical characteristics, genetic features and effects of therapy. Current Hematologic Malignancy Reports. 2013;8(2):116–122. doi: 10.1007/s11899-013-0154-5. [DOI] [PubMed] [Google Scholar]
- 27.Hasselbalch H. C. Chronic inflammation as a promotor of mutagenesis in essential thrombocythemia, polycythemia vera and myelofibrosis. A human inflammation model for cancer development? Leukemia Research. 2013;37(2):214–220. doi: 10.1016/j.leukres.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 28.Hasselbalch H. C. Perspectives on the impact of JAK-inhibitor therapy upon inflammation-mediated comorbidities in myelofibrosis and related neoplasms. Expert Review of Hematology. 2014;7(2):203–216. doi: 10.1586/17474086.2013.876356. [DOI] [PubMed] [Google Scholar]
- 29.Hasselbalch H. C. A role of NF-E2 in chronic inflammation and clonal evolution in essential thrombocythemia, polycythemia vera and myelofibrosis? Leukemia Research. 2014;38(2):263–266. doi: 10.1016/j.leukres.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 30.Bozinovski S., Vlahos R., Anthony D., et al. COPD and squamous cell lung cancer: aberrant inflammation and immunity is the common link. British Journal of Pharmacology. 2015 doi: 10.1111/bph.13198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Karin M. Nuclear factor-kappaB in cancer development and progression. Nature. 2006;441(7092):431–436. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- 32.Roslind A., Johansen J. S. Inflammation and Cancer. Vol. 511. Totowa, NJ, USA: Humana Press; 2009. [Google Scholar]
- 33.Coussens L. M., Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elinav E., Nowarski R., Thaiss C. A., Hu B., Jin C., Flavell R. A. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nature Reviews Cancer. 2013;13(11):759–771. doi: 10.1038/nrc3611. [DOI] [PubMed] [Google Scholar]
- 35.Trinchieri G. Cancer and inflammation: an old intuition with rapidly evolving new concepts. Annual Review of Immunology. 2012;30:677–706. doi: 10.1146/annurev-immunol-020711-075008. [DOI] [PubMed] [Google Scholar]
- 36.Marchioli R., Finazzi G., Landolfi R., et al. Vascular and neoplastic risk in a large cohort of patients with polycythemia vera. Journal of Clinical Oncology. 2005;23(10):2224–2232. doi: 10.1200/jco.2005.07.062. [DOI] [PubMed] [Google Scholar]
- 37.Frederiksen H., Farkas D. K., Christiansen C. F., Hasselbalch H. C., Sørensen H. T. Chronic myeloproliferative neoplasms and subsequent cancer risk: a Danish population-based cohort study. Blood. 2011;118(25):6515–6520. doi: 10.1182/blood-2011-04-348755. [DOI] [PubMed] [Google Scholar]
- 38.Hasselbalch H. C. Idiopathic myelofibrosis: a clinical study of 80 patients. American Journal of Hematology. 1990;34(4):291–300. doi: 10.1002/ajh.2830340411. [DOI] [PubMed] [Google Scholar]
- 39.Quintás-Cardama A. The role of Janus kinase 2 (JAK2) in myeloproliferative neoplasms: therapeutic implications. Leukemia Research. 2013;37(4):465–472. doi: 10.1016/j.leukres.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 40.Wolf D., Rudzki J., Gastl G. Current treatment concepts of Philadelphia-negative MPN. Current Cancer Drug Targets. 2011;11(1):44–55. doi: 10.2174/156800911793743592. [DOI] [PubMed] [Google Scholar]
- 41.Barbui T., Barosi G., Birgegard G., et al. Philadelphia-negative classical myeloproliferative neoplasms: critical concepts and management recommendations from European leukemiaNet. Journal of Clinical Oncology. 2011;29(6):761–770. doi: 10.1200/jco.2010.31.8436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tefferi A., Vainchenker W. Myeloproliferative neoplasms: molecular pathophysiology, essential clinical understanding, and treatment strategies. Journal of Clinical Oncology. 2011;29(5):573–582. doi: 10.1200/jco.2010.29.8711. [DOI] [PubMed] [Google Scholar]
- 43.Larsen T. S., Bjerrum O. W., Pallisgaard N., Andersen M. T., Møller M. B., Hasselbalch H. C. Sustained major molecular response on interferon alpha-2b in two patients with polycythemia vera. Annals of Hematology. 2008;87(10):847–850. doi: 10.1007/s00277-008-0498-4. [DOI] [PubMed] [Google Scholar]
- 44.Larsen T. S., Møller M. B., de Stricker K., et al. Minimal residual disease and normalization of the bone marrow after long-term treatment with alpha-interferon2b in polycythemia vera. A report on molecular response patterns in seven patients in sustained complete hematological remission. Hematology. 2009;14(6):331–334. doi: 10.1179/102453309x12473408860587. [DOI] [PubMed] [Google Scholar]
- 45.Kiladjian J.-J.-J., Cassinat B., Turlure P., et al. High molecular response rate of polycythemia vera patients treated with pegylated interferon α-2a. Blood. 2006;108(6):2037–2040. doi: 10.1182/blood-2006-03-009860. [DOI] [PubMed] [Google Scholar]
- 46.Kiladjian J.-J., Cassinat B., Chevret S., et al. Pegylated interferon-alfa-2a induces complete hematologic and molecular responses with low toxicity in polycythemia vera. Blood. 2008;112(8):3065–3072. doi: 10.1182/blood-2008-03-143537. [DOI] [PubMed] [Google Scholar]
- 47.Quintás-Cardama A., Kantarjian H., Manshouri T., et al. Pegylated interferon alfa-2a yields high rates of hematologic and molecular response in patients with advanced essential thrombocythemia and polycythemia vera. Journal of Clinical Oncology. 2009;27(32):5418–5424. doi: 10.1200/jco.2009.23.6075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hasselbalch H. C., Larsen T. S., Riley C. H., Jensen M. K., Kiladjian J.-J. Interferon-alpha in the treatment of Philadelphia-negative chronic myeloproliferative neoplasms. Status and perspectives. Current Drug Targets. 2011;12(3):392–419. doi: 10.2174/138945011794815275. [DOI] [PubMed] [Google Scholar]
- 49.Kiladjian J.-J., Mesa R. A., Hoffman R. The renaissance of interferon therapy for the treatment of myeloid malignancies. Blood. 2011;117(18):4706–4715. doi: 10.1182/blood-2010-08-258772. [DOI] [PubMed] [Google Scholar]
- 50.Hasselbalch H. C. A new era for IFN-alpha in the treatment of Philadelphia-negative chronic myeloproliferative neoplasms. Expert Review of Hematology. 2011;4(6):637–655. doi: 10.1586/ehm.11.63. [DOI] [PubMed] [Google Scholar]
- 51.Stauffer Larsen T., Iversen K. F., Hansen E., et al. Long term molecular responses in a cohort of Danish patients with essential thrombocythemia, polycythemia vera and myelofibrosis treated with recombinant interferon alpha. Leukemia Research. 2013;37(9):1041–1045. doi: 10.1016/j.leukres.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 52.Silver R. T., Kiladjian J.-J., Hasselbalch H. C. Interferon and the treatment of polycythemia vera, essential thrombocythemia and myelofibrosis. Expert Review of Hematology. 2013;6(1):49–58. doi: 10.1586/ehm.12.69. [DOI] [PubMed] [Google Scholar]
- 53.Quintás-Cardama A., Abdel-Wahab O., Manshouri T., et al. Molecular analysis of patients with polycythemia vera or essential thrombocythemia receiving pegylated interferon α-2a. Blood. 2013;122(6):893–901. doi: 10.1182/blood-2012-07-442012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cassinat B., Verger E., Kiladjian J.-J. Interferon alfa therapy in CALR-mutated essential thrombocythemia. The New England Journal of Medicine. 2014;371(2):188–189. doi: 10.1056/nejmc1401255. [DOI] [PubMed] [Google Scholar]
- 55.Utke Rank C., Weis Bjerrum O., Larsen T. S., et al. Minimal residual disease after long-term interferon-alpha2 treatment: a report on hematological, molecular and histomorphological response patterns in 10 patients with essential thrombocythemia and polycythemia vera. Leukemia & Lymphoma. 2015:1–7. doi: 10.3109/10428194.2015.1049171. [DOI] [PubMed] [Google Scholar]
- 56.Raison C. L., Capuron L., Miller A. H. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends in Immunology. 2006;27(1):24–31. doi: 10.1016/j.it.2005.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dantzer R., O'Connor J. C., Freund G. G., Johnson R. W., Kelley K. W. From inflammation to sickness and depression: when the immune system subjugates the brain. Nature Reviews Neuroscience. 2008;9(1):46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zunszain P. A., Hepgul N., Pariante C. M. Inflammation and depression. Current Topics in Behavioral Neurosciences. 2013;14:135–151. doi: 10.1007/7854_2012_211. [DOI] [PubMed] [Google Scholar]
- 59.Antonioli E., Guglielmelli P., Pieri L., et al. Hydroxyurea-related toxicity in 3,411 patients with Ph'-negative MPN. The American Journal of Hematology. 2012;87(5):552–554. doi: 10.1002/ajh.23160. [DOI] [PubMed] [Google Scholar]
- 60.Björkholm M., Hultcrantz M., Derolf Å. R. Leukemic transformation in myeloproliferative neoplasms: therapy-related or unrelated? Bailliere's Best Practice & Research in Clinical Haematology. 2014;27(2):141–153. doi: 10.1016/j.beha.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 61.Kiladjian J.-J., Chevret S., Dosquet C., Chomienne C., Rain J.-D. Treatment of polycythemia vera with hydroxyurea and pipobroman: final results of a randomized trial initiated in 1980. Journal of Clinical Oncology. 2011;29(29):3907–3913. doi: 10.1200/jco.2011.36.0792. [DOI] [PubMed] [Google Scholar]
- 62.Sirieix M.-E., Debure C., Baudot N., et al. Leg ulcers and hydroxyurea: forty-one cases. Archives of Dermatology. 1999;135(7):818–820. doi: 10.1001/archderm.135.7.818. [DOI] [PubMed] [Google Scholar]
- 63.Quattrone F., Dini V., Barbanera S., Zerbinati N., Romanelli M. Cutaneous ulcers associated with hydroxyurea therapy. Journal of Tissue Viability. 2013;22(4):112–121. doi: 10.1016/j.jtv.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 64.Verner E., Forsyth C., Grigg A. Cyclical thrombocytosis, acquired von Willebrand syndrome and aggressive non-melanoma skin cancers are common in patients with Philadelphia-negative myeloproliferative neoplasms treated with hydroxyurea. Leukemia & Lymphoma. 2014;55(5):1139–1143. doi: 10.3109/10428194.2013.827788. [DOI] [PubMed] [Google Scholar]
- 65.Heine A., Held S. A. E., Daecke S. N., et al. The JAK-inhibitor ruxolitinib impairs dendritic cell function in vitro and in vivo. Blood. 2013;122(7):1192–1202. doi: 10.1182/blood-2013-03-484642. [DOI] [PubMed] [Google Scholar]
- 66.Tefferi A. Ruxolitinib targets DCs: for better or worse? Blood. 2013;122(7):1096–1097. doi: 10.1182/blood-2013-07-509612. [DOI] [PubMed] [Google Scholar]
- 67.Schonberg K., Rudolph J., Vonnahme M., et al. JAK inhibition impairs NK cell function in myeloproliferative neoplasms. Cancer Research. 2015;75(11):2187–2199. doi: 10.1158/0008-5472.can-14-3198. [DOI] [PubMed] [Google Scholar]
- 68.Keohane C., Kordasti S., Seidl T., et al. JAK inhibition induces silencing of T Helper cytokine secretion and a profound reduction in T regulatory cells. British Journal of Haematology. 2015 doi: 10.1111/bjh.13519. [DOI] [PubMed] [Google Scholar]
- 69.Massa M., Rosti V., Campanelli R., Fois G., Barosi G. Rapid and long-lasting decrease of T-regulatory cells in patients with myelofibrosis treated with ruxolitinib. Leukemia. 2014;28(2):449–451. doi: 10.1038/leu.2013.296. [DOI] [PubMed] [Google Scholar]
- 70.Hahn B. H. Systemic lupus erythematosus and accelerated atherosclerosis. The New England Journal of Medicine. 2003;349(25):2379–2380. doi: 10.1056/nejmp038168. [DOI] [PubMed] [Google Scholar]
- 71.Yajnanarayana S. P., Stübig T., Cornez I., et al. JAK1/2 inhibition impairs T cell function in vitro and in patients with myeloproliferative neoplasms. British Journal of Haematology. 2015;169(6):824–833. doi: 10.1111/bjh.13373. [DOI] [PubMed] [Google Scholar]
- 72.Chen Y.-H., Lee C.-H., Pei S.-N. Pulmonary tuberculosis reactivation following ruxolitinib treatment in a patient with primary myelofibrosis. Leukemia & Lymphoma. 2015;56(5):1528–1529. doi: 10.3109/10428194.2014.963082. [DOI] [PubMed] [Google Scholar]
- 73.Hopman R. K., Lawrence S. J., Oh S. T. Disseminated tuberculosis associated with ruxolitinib. Leukemia. 2014;28(8):1750–1751. doi: 10.1038/leu.2014.104. [DOI] [PubMed] [Google Scholar]
- 74.Palandri F., Polverelli N., Catani L., Vianelli N. Ruxolitinib-associated tuberculosis: a case of successful ruxolitinib rechallenge. Annals of Hematology. 2014;94(3):519–520. doi: 10.1007/s00277-014-2183-0. [DOI] [PubMed] [Google Scholar]
- 75.Rowan W., Moule S., Milojkovic D. Progressive multifocal leukoencephalopathy associated with ruxolitinib. The New England Journal of Medicine. 2013;369(2):194–197. doi: 10.1056/nejmc1302135. [DOI] [PubMed] [Google Scholar]
- 76.Goldberg R. A., Reichel E., Oshry L. J. Bilateral toxoplasmosis retinitis associated with ruxolitinib. The New England Journal of Medicine. 2013;369(7):681–683. doi: 10.1056/nejmc1302895. [DOI] [PubMed] [Google Scholar]
- 77.Ostojic A., Vrhovac R., Verstovsek S. Ruxolitinib for the treatment of myelofibrosis: its clinical potential. Therapeutics and Clinical Risk Management. 2012;8:95–103. doi: 10.2147/tcrm.s23277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mesa R. A., Gotlib J., Gupta V., et al. Effect of ruxolitinib therapy on myelofibrosis-related symptoms and other patient-reported outcomes in COMFORT-I: a randomized, double-blind, placebo-controlled trial. Journal of Clinical Oncology. 2013;31(10):1285–1292. doi: 10.1200/jco.2012.44.4489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Verstovsek S., Mesa R. A., Gotlib J., et al. Efficacy, safety, and survival with ruxolitinib in patients with myelofibrosis: results of a median 3-year follow-up of COMFORT-I. Haematologica. 2015;100(4):479–488. doi: 10.3324/haematol.2014.115840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Quintás-Cardama A., Kantarjian H., Cortes J., Verstovsek S. Janus kinase inhibitors for the treatment of myeloproliferative neoplasias and beyond. Nature Reviews Drug Discovery. 2011;10(2):127–140. doi: 10.1038/nrd3264. [DOI] [PubMed] [Google Scholar]
- 81.Verstovsek S., Kantarjian H. M., Estrov Z., et al. Long-term outcomes of 107 patients with myelofibrosis receiving JAK1/JAK2 inhibitor ruxolitinib: survival advantage in comparison to matched historical controls. Blood. 2012;120(6):1202–1209. doi: 10.1182/blood-2012-02-414631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Passamonti F., Vannucchi A. M., Cervantes F., et al. Ruxolitinib and survival improvement in patients with myelofibrosis. Leukemia. 2015;3:739–740. doi: 10.1038/leu.2014.282. [DOI] [PubMed] [Google Scholar]
- 83.Kleppe M., Kwak M., Koppikar P., et al. JAK-STAT pathway activation in malignant and non-malignant cells contributes to MPN pathogenesis and therapeutic response. Cancer Discovery. 2015;5(3):316–331. doi: 10.1158/2159-8290.cd-14-0736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bjørn M. E., Hasselbalch H. C. The impact of ruxolitinib treatment on inflammation-mediated comorbidities in myelofibrosis and related neoplasms. Clinical Case Reports. 2015;3(6):499–503. doi: 10.1002/ccr3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Angona A., Alvarez-Larrán A., Bellosillo B., Longarón R., Fernández-Rodríguez C., Besses C. Dynamics of JAK2 V617F allele burden of CD34+ haematopoietic progenitor cells in patients treated with ruxolitinib. British Journal of Haematology. 2015 doi: 10.1111/bjh.13535. [DOI] [PubMed] [Google Scholar]
- 86.Vener C., Novembrino C., Catena F. B., et al. Oxidative stress is increased in primary and post-polycythemia vera myelofibrosis. Experimental Hematology. 2010;38(11):1058–1065. doi: 10.1016/j.exphem.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 87.Marty C., Lacout C., Droin N., et al. A role for reactive oxygen species in JAK2 V617F myeloproliferative neoplasm progression. Leukemia. 2013;27(11):2187–2195. doi: 10.1038/leu.2013.102. [DOI] [PubMed] [Google Scholar]
- 88.Waris G., Ahsan H. Reactive oxygen species: role in the development of cancer and various chronic conditions. Journal of Carcinogenesis. 2006;5, article 14 doi: 10.1186/1477-3163-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gorrini C., Harris I. S., Mak T. W. Modulation of oxidative stress as an anticancer strategy. Nature Reviews Drug Discovery. 2013;12(12):931–947. doi: 10.1038/nrd4002. [DOI] [PubMed] [Google Scholar]
- 90.Halliwell B. Oxidative stress and cancer: Have we moved forward? The Biochemical Journal. 2007;401(1):1–11. doi: 10.1042/bj20061131. [DOI] [PubMed] [Google Scholar]
- 91.Nishinaka Y., Arai T., Adachi S., Takaori-Kondo A., Yamashita K. Singlet oxygen is essential for neutrophil extracellular trap formation. Biochemical and Biophysical Research Communications. 2011;413(1):75–79. doi: 10.1016/j.bbrc.2011.08.052. [DOI] [PubMed] [Google Scholar]
- 92.Kohchi C., Inagawa H., Nishizawa T., Soma G.-I. ROS and innate immunity. Anticancer Research. 2009;29(3):817–822. [PubMed] [Google Scholar]
- 93.Wink D. A., Hines H. B., Cheng R. Y. S., et al. Nitric oxide and redox mechanisms in the immune response. Journal of Leukocyte Biology. 2011;89(6):873–891. doi: 10.1189/jlb.1010550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Holland S. M. Chronic granulomatous disease. Clinical Reviews in Allergy & Immunology. 2010;38(1):3–10. doi: 10.1007/s12016-009-8136-z. [DOI] [PubMed] [Google Scholar]
- 95.Kuhns D. B., Alvord W. G., Heller T., et al. Residual NADPH oxidase and survival in chronic granulomatous disease douglas. The New England Journal of Medicine. 2010;363(27):2600–2610. doi: 10.1056/nejmoa1007097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.De Marchi E., Baldassari F., Bononi A., Wieckowski M. R., Pinton P. Oxidative stress in cardiovascular diseases and obesity: role of p66Shc and protein kinase C. Oxidative Medicine and Cellular Longevity. 2013;2013:11. doi: 10.1155/2013/564961.564961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zheng S., Zhong Z.-M., Qin S., et al. Advanced oxidation protein products induce inflammatory response in fibroblast-like synoviocytes through NADPH oxidase -dependent activation of NF-κB. Cellular Physiology and Biochemistry. 2013;32(4):972–985. doi: 10.1159/000354500. [DOI] [PubMed] [Google Scholar]
- 98.Singh U., Jialal I. Oxidative stress and atherosclerosis. Pathophysiology. 2006;13(3):129–142. doi: 10.1016/j.pathophys.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 99.Harrison D., Griendling K. K., Landmesser U., Hornig B., Drexler H. Role of oxidative stress in atherosclerosis. The American Journal of Cardiology. 2003;91(3):7A–11A. doi: 10.1016/s0002-9149(02)03144-2. [DOI] [PubMed] [Google Scholar]
- 100.Leopold J. A., Loscalzo J. Oxidative risk for atherothrombotic cardiovascular disease. Free Radical Biology and Medicine. 2009;47(12):1673–1706. doi: 10.1016/j.freeradbiomed.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gloire G., Legrand-Poels S., Piette J. NF-κB activation by reactive oxygen species: fifteen years later. Biochemical Pharmacology. 2006;72(11):1493–1505. doi: 10.1016/j.bcp.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 102.Ben-Neriah Y., Karin M. Inflammation meets cancer, with NF-κB as the matchmaker. Nature Immunology. 2011;12(8):715–723. doi: 10.1038/ni.2060. [DOI] [PubMed] [Google Scholar]
- 103.Karin M., Greten F. R. NF-κB: linking inflammation and immunity to cancer development and progression. Nature Reviews Immunology. 2005;5(10):749–759. doi: 10.1038/nri1703. [DOI] [PubMed] [Google Scholar]
- 104.Alexander W. S. Suppressors of cytokine signalling (SOCS) in the immune system. Nature Reviews Immunology. 2002;2(6):410–416. doi: 10.1038/nri818. [DOI] [PubMed] [Google Scholar]
- 105.Sasi W., Sharma A. K., Mokbel K. The role of suppressors of cytokine signalling in human neoplasms. Molecular Biology International. 2014;2014:24. doi: 10.1155/2014/630797.630797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Capello D., Deambrogi C., Rossi D., et al. Epigenetic inactivation of suppressors of cytokine signalling in Philadelphia-negative chronic myeloproliferative disorders. British Journal of Haematology. 2008;141(4):504–511. doi: 10.1111/j.1365-2141.2008.07072.x. [DOI] [PubMed] [Google Scholar]
- 107.Fourouclas N., Li J., Gilby D. C., et al. Methylation of the suppressor of cytokine signaling 3 gene (SOCS3) in myeloproliferative disorders. Haematologica. 2008;93(11):1635–1644. doi: 10.3324/haematol.13043. [DOI] [PubMed] [Google Scholar]
- 108.Ivanov A. V., Bartosch B., Smirnova O. A., Isaguliants M. G., Kochetkov S. N. HCV and oxidative stress in the liver. Viruses. 2013;5(2):439–469. doi: 10.3390/v5020439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Khadem Ansari M. H., Omrani M.-D., Kheradmand F. Oxidative stress response in patients infected by diverse hepatitis C virus genotypes. Hepatitis Monthly. 2015;15(2):1–5. doi: 10.5812/hepatmon.22069.e22069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lin W., Tsai W.-L., Shao R.-X., et al. Hepatitis C virus regulates transforming growth factor β1 production through the generation of reactive oxygen species in a nuclear factor κB-dependent manner. Gastroenterology. 2010;138(7):2509–2518. doi: 10.1053/j.gastro.2010.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Fujinaga H., Tsutsumi T., Yotsuyanagi H., Moriya K., Koike K. Hepatocarcinogenesis in hepatitis C: HCV shrewdly exacerbates oxidative stress by modulating both production and scavenging of reactive oxygen species. Oncology. 2011;81(supplement 1):11–17. doi: 10.1159/000333253. [DOI] [PubMed] [Google Scholar]
- 112.Takaki A. Control of oxidative stress in hepatocellular carcinoma: helpful or harmful? World Journal of Hepatology. 2015;7(7):p. 968. doi: 10.4254/wjh.v7.i7.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Martin M., Herceg Z. From hepatitis to hepatocellular carcinoma: a proposed model for cross-talk between inflammation and epigenetic mechanisms. Genome Medicine. 2012;4(1, article 8) doi: 10.1186/gm307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Thorsteinsdottir S., Bjerrum O. W., Hasselbalch H. C. Myeloproliferative neoplasms in five multiple sclerosis patients. Leukemia Research Reports. 2013;2(2):61–63. doi: 10.1016/j.lrr.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Di Bona D., Cippitelli M., Fionda C., et al. Oxidative stress inhibits IFN-α-induced antiviral gene expression by blocking the JAK-STAT pathway. Journal of Hepatology. 2006;45(2):271–279. doi: 10.1016/j.jhep.2006.01.037. [DOI] [PubMed] [Google Scholar]
- 116.Hurtado-Nedelec M., Csillag M.-J., Boussetta T., et al. Increased reactive oxygen species production and p47phox phosphorylation in neutrophils from myeloproliferative disorders patients with JAK2 (V617F) mutation. Haematologica. 2013;98(10):1517–1524. doi: 10.3324/haematol.2012.082560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Glorieux C., Zamocky M., Sandoval J. M., Verrax J., Calderon P. B. Regulation of catalase expression in healthy and Cancer cells. Free Radical Biology and Medicine. 2015 doi: 10.1016/j.freeradbiomed.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 118.Smith P. S., Zhao W., Spitz D. R., Robbins M. E. Inhibiting catalase activity sensitizes 36B10 rat glioma cells to oxidative stress. Free Radical Biology and Medicine. 2007;42(6):787–797. doi: 10.1016/j.freeradbiomed.2006.11.032. [DOI] [PubMed] [Google Scholar]
- 119.Hwang T. S., Choi H. K., Han H. S. Differential expression of manganese superoxide dismutase, copper/zinc superoxide dismutase, and catalase in gastric adenocarcinoma and normal gastric mucosa. European Journal of Surgical Oncology. 2007;33(4):474–479. doi: 10.1016/j.ejso.2006.10.024. [DOI] [PubMed] [Google Scholar]
- 120.Rainis T., Maor I., Lanir A., Shnizer S., Lavy A. Enhanced oxidative stress and leucocyte activation in neoplastic tissues of the colon. Digestive Diseases and Sciences. 2007;52(2):526–530. doi: 10.1007/s10620-006-9177-2. [DOI] [PubMed] [Google Scholar]
- 121.Sander C. S., Hamm F., Elsner P., Thiele J. J. Oxidative stress in malignant melanoma and non-melanoma skin cancer. The British Journal of Dermatology. 2003;148(5):913–922. doi: 10.1046/j.1365-2133.2003.05303.x. [DOI] [PubMed] [Google Scholar]
- 122.Zelen I., Djurdjevic P., Popovic S., et al. Antioxidant enzymes activities and plasma levels of oxidative stress markers in B-chronic lymphocytic leukemia patients. Journal of B.U.ON. 2010;15(2):330–336. [PubMed] [Google Scholar]
- 123.Szatrowski T. P., Nathan C. F. Production of large amounts of hydrogen peroxide by human tumor cells. Cancer Research. 1991;51(3):794–798. [PubMed] [Google Scholar]
- 124.Vaquero E. C., Edderkaoui M., Pandol S. J., Gukovsky I., Gukovskaya A. S. Reactive oxygen species produced by NAD(P)H oxidase inhibit apoptosis in pancreatic cancer cells. The Journal of Biological Chemistry. 2004;279(33):34643–34654. doi: 10.1074/jbc.m400078200. [DOI] [PubMed] [Google Scholar]
- 125.Mochizuki T., Furuta S., Mitsushita J., et al. Inhibition of NADPH oxidase 4 activates apoptosis via the AKT/apoptosis signal-regulating kinase 1 pathway in pancreatic cancer PANC-1 cells. Oncogene. 2006;25(26):3699–3707. doi: 10.1038/sj.onc.1209406. [DOI] [PubMed] [Google Scholar]
- 126.Li N., Ragheb K., Lawler G., et al. Mitochondrial complex I inhibitor rotenone induces apoptosis through enhancing mitochondrial reactive oxygen species production. Journal of Biological Chemistry. 2003;278(10):8516–8525. doi: 10.1074/jbc.m210432200. [DOI] [PubMed] [Google Scholar]
- 127.Yalcin S., Marinkovic D., Mungamuri S. K., et al. ROS-mediated amplification of AKT/mTOR signalling pathway leads to myeloproliferative syndrome in Foxo3−/− mice. The EMBO Journal. 2010;29(24):4118–4131. doi: 10.1038/emboj.2010.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Xu D., Zheng H., Yu W.-M., Qu C.-K. Activating mutations in protein tyrosine phosphatase Ptpn11 (Shp2) enhance reactive oxygen species production that contributes to myeloproliferative disorder. PLoS ONE. 2013;8(5) doi: 10.1371/journal.pone.0063152.e63152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Goerttler P. S., Kreutz C., Donauer J., et al. Gene expression profiling in polycythaemia vera: overexpression of transcription factor NF-E2. British Journal of Haematology. 2005;129(1):138–150. doi: 10.1111/j.1365-2141.2005.05416.x. [DOI] [PubMed] [Google Scholar]
- 130.Mutschler M., Magin A. S., Buerge M., et al. NF-E2 overexpression delays erythroid maturation and increases erythrocyte production. British Journal of Haematology. 2009;146(2):203–217. doi: 10.1111/j.1365-2141.2009.07742.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Kaufmann K. B., Gründer A., Hadlich T., et al. A novel murine model of myeloproliferative disorders generated by overexpression of the transcription factor NF-E2. Journal of Experimental Medicine. 2012;209(1):35–50. doi: 10.1084/jem.20110540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Aumann K., Frey A.-V., May A. M., et al. Subcellular mislocalization of the transcription factor NF-E2 in erythroid cells discriminates prefibrotic primary myelofibrosis from essential thrombocythemia. Blood. 2013;122(1):93–99. doi: 10.1182/blood-2012-11-463257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wehrle J., Seeger T. S., Schwemmers S., Pfeifer D., Bulashevska A., Pahl H. L. Transcription factor nuclear factor erythroid-2 mediates expression of the cytokine interleukin 8, a known predictor of inferior outcome in patients with myeloproliferative Neoplasms. Haematologica. 2013;98(7):1073–1080. doi: 10.3324/haematol.2012.071183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bogeska R., Pahl H. L. Elevated nuclear factor erythroid-2 levels promote epo-independent erythroid maturation and recapitulate the hematopoietic stem cell and common myeloid progenitor expansion observed in polycythemia vera patients. Stem Cells Translational Medicine. 2013;2(2):112–117. doi: 10.5966/sctm.2012-0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Hasselbalch H. C., Thomassen M., Riley C. H., et al. Whole blood transcriptional profiling reveals deregulation of oxidative and antioxidative defence genes in myelofibrosis and related neoplasms. Potential implications of downregulation of Nrf2 for genomic instability and disease progression. PLoS ONE. 2014;9(11) doi: 10.1371/journal.pone.0112786.e112786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Nakatake M., Monte-Mor B., Debili N., et al. JAK2V617F negatively regulates p53 stabilization by enhancing MDM2 via La expression in myeloproliferative neoplasms. Oncogene. 2012;31(10):1323–1333. doi: 10.1038/onc.2011.313. [DOI] [PubMed] [Google Scholar]
- 137.Cybulski C., Górski B., Huzarski T., et al. CHEK2 is a multiorgan cancer susceptibility gene. The American Journal of Human Genetics. 2004;75(6):1131–1135. doi: 10.1086/426403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Simon M., Ludwig M., Fimmers R., et al. Variant of the CHEK2 gene as a prognostic marker in glioblastoma multiforme. Neurosurgery. 2006;59(5):1078–1085. doi: 10.1227/01.neu.0000245586.23710.ef. [DOI] [PubMed] [Google Scholar]
- 139.Wu X., Dong X., Liu W., Chen J. Characterization of CHEK2 mutations in prostate cancer. Human Mutation. 2006;27(8):742–747. doi: 10.1002/humu.20321. [DOI] [PubMed] [Google Scholar]
- 140.Suchy J., Cybulski C., Wokołorczyk D., et al. CHEK2 mutations and HNPCC-related colorectal cancer. International Journal of Cancer. 2010;126(12):3005–3009. doi: 10.1002/ijc.25003. [DOI] [PubMed] [Google Scholar]
- 141.Złowocka E., Cybulski C., Górski B., et al. Germline mutations in the CHEK2 kinase gene are associated with an increased risk of bladder cancer. International Journal of Cancer. 2008;122(3):583–586. doi: 10.1002/ijc.23099. [DOI] [PubMed] [Google Scholar]
- 142.Janiszewska H., Bak A., Pilarska M., et al. A risk of essential thrombocythemia in carriers of constitutional CHEK2 gene mutations. Haematologica. 2012;97(3):366–370. doi: 10.3324/haematol.2011.049494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Janiszewska H., Bąk A., Hartwig M., et al. The germline mutations of the CHEK2 gene are associated with an increased risk of polycythaemia vera. British Journal of Haematology. 2015 doi: 10.1111/bjh.13559. [DOI] [PubMed] [Google Scholar]
- 144.Zhang Y., Liu X., McHale C., et al. Bone marrow injury induced via oxidative stress in mice by inhalation exposure to formaldehyde. PLoS ONE. 2013;8(9) doi: 10.1371/journal.pone.0074974.e74974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Yahata T., Takanashi T., Muguruma Y., et al. Accumulation of oxidative DNA damage restricts the self-renewal capacity of human hematopoietic stem cells. Blood. 2011;118(11):2941–2950. doi: 10.1182/blood-2011-01-330050. [DOI] [PubMed] [Google Scholar]
- 146.Mullally A., Bruedigam C., Poveromo L., et al. Depletion of Jak2V617F myeloproliferative neoplasm-propagating stem cells by interferon-α in a murine model of polycythemia vera. Blood. 2013;121(18):3692–3702. doi: 10.1182/blood-2012-05-432989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Hasan S., Lacout C., Marty C., et al. JAK2V617F expression in mice amplifies early hematopoietic cells and gives them a competitive advantage that is hampered by IFNα . Blood. 2013;122(8):1464–1477. doi: 10.1182/blood-2013-04-498956. [DOI] [PubMed] [Google Scholar]
- 148.Riley C. H., Hansen M., Brimnes M. K., et al. Expansion of circulating CD56bright natural killer cells in patients with JAK2-positive chronic myeloproliferative neoplasms during treatment with interferon-α . European Journal of Haematology. 2015;94(3):227–234. doi: 10.1111/ejh.12420. [DOI] [PubMed] [Google Scholar]
- 149.Skov V., Riley C. H., Thomassen M., et al. Whole blood transcriptional profiling reveals significant down-regulation of human leukocyte antigen class I and II genes in essential thrombocythemia, polycythemia vera and myelofibrosis. Leukemia & Lymphoma. 2013;54(10):2269–2273. doi: 10.3109/10428194.2013.764417. [DOI] [PubMed] [Google Scholar]
- 150.Karalija A., Novikova L. N., Kingham P. J., Wiberg M., Novikov L. N. Neuroprotective effects of N-acetyl-cysteine and acetyl-L-carnitine after spinal cord injury in adult rats. PLoS ONE. 2012;7(7) doi: 10.1371/journal.pone.0041086.e41086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Karalija A., Novikova L. N., Kingham P. J., Wiberg M., Novikov L. N. The effects of N-acetyl-cysteine and acetyl-l-carnitine on neural survival, neuroinflammation and regeneration following spinal cord injury. Neuroscience. 2014;269:143–151. doi: 10.1016/j.neuroscience.2014.03.042. [DOI] [PubMed] [Google Scholar]
- 152.Shen F., Coulter C. V., Isbister G. K., Duffull S. B. A dosing regimen for immediate N-acetylcysteine treatment for acute paracetamol overdose. Clinical Toxicology. 2011;49(7):643–647. doi: 10.3109/15563650.2011.604034. [DOI] [PubMed] [Google Scholar]
- 153.Schmidt L. E. Identification of patients at risk of anaphylactoid reactions to N-acetylcysteine in the treatment of paracetamol overdose. Clinical Toxicology. 2013;51(6):467–472. doi: 10.3109/15563650.2013.799677. [DOI] [PubMed] [Google Scholar]
- 154.Shen Y., Cai W., Lei S., Zhang Z. Effect of high/low dose N-acetylcysteine on chronic obstructive pulmonary disease: a systematic review and meta-analysis. Journal of Chronic Obstructive Pulmonary Disease. 2014;11(3):351–358. doi: 10.3109/15412555.2013.858315. [DOI] [PubMed] [Google Scholar]
- 155.Santus P., Corsico A., Solidoro P., Braido F., Di Marco F., Scichilone N. Oxidative stress and respiratory system: pharmacological and clinical reappraisal of N-acetylcysteine. Journal of Chronic Obstructive Pulmonary Disease. 2014;11(6):705–717. doi: 10.3109/15412555.2014.898040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Conrad C., Lymp J., Thompson V., et al. Long-term treatment with oral N-acetylcysteine: affects lung function but not sputum inflammation in cystic fibrosis subjects. A phase II randomized placebo-controlled trial. Journal of Cystic Fibrosis. 2015;14(2):219–227. doi: 10.1016/j.jcf.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 157.Lai Z.-W., Hanczko R., Bonilla E., et al. N-acetylcysteine reduces disease activity by blocking mammalian target of rapamycin in T cells from systemic lupus erythematosus patients: a randomized, double-blind, placebo-controlled trial. Arthritis and Rheumatism. 2012;64(9):2937–2946. doi: 10.1002/art.34502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Skov V., Larsen T. S., Thomassen M., et al. Whole-blood transcriptional profiling of interferon-inducible genes identifies highly upregulated IFI27 in primary myelofibrosis. European Journal of Haematology. 2011;87(1):54–60. doi: 10.1111/j.1600-0609.2011.01618.x. [DOI] [PubMed] [Google Scholar]
- 159.Skov V., Larsen T. S., Thomassen M., et al. Molecular profiling of peripheral blood cells from patients with polycythemia vera and related neoplasms: identification of deregulated genes of significance for inflammation and immune surveillance. Leukemia Research. 2012;36(11):1387–1392. doi: 10.1016/j.leukres.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 160.Riley C. H., Jensen M. K., Brimnes M. K., et al. Increase in circulating CD4+CD25+Foxp3+ T cells in patients with Philadelphia-negative chronic myeloproliferative neoplasms during treatment with IFN-α . Blood. 2011;118(8):2170–2173. doi: 10.1182/blood-2011-03-340992. [DOI] [PubMed] [Google Scholar]
- 161.Le Bousse-Kerdilès M.-C. Primary myelofibrosis and the ‘bad seeds in bad soil’ concept. Fibrogenesis & Tissue Repair. 2012;5(supplement 1, article S20) doi: 10.1186/1755-1536-5-s1-s20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Lataillade J.-J., Pierre-Louis O., Hasselbalch H. C., et al. Does primary myelofibrosis involve a defective stem cell niche? From concept to evidence. Blood. 2008;112(8):3026–3035. doi: 10.1182/blood-2008-06-158386. [DOI] [PubMed] [Google Scholar]
- 163.Lundberg P., Karow A., Nienhold R., et al. Clonal evolution and clinical correlates of somatic mutations in myeloproliferative neoplasms. Blood. 2014;123(14):2220–2228. doi: 10.1182/blood-2013-11-537167. [DOI] [PubMed] [Google Scholar]
- 164.Bjørn M., de Stricker K., Kjær L., Ellemann K., Hasselbalch H. C. Combination therapy with interferon and JAK1-2 inhibitor is feasible: proof of concept with rapid reduction in JAK2V617F-allele burden in polycythemia vera. Leukemia Research Reports. 2014;3(2):73–75. doi: 10.1016/j.lrr.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Hasselbalch H. C. The role of cytokines in the initiation and progression of myelofibrosis. Cytokine & Growth Factor Reviews. 2013;24(2):133–145. doi: 10.1016/j.cytogfr.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 166.Hasselbalch H. C., Riley C. H. Statins in the treatment of polycythaemia vera and allied disorders: an antithrombotic and cytoreductive potential? Leukemia Research. 2006;30(10):1217–1225. doi: 10.1016/j.leukres.2005.12.018. [DOI] [PubMed] [Google Scholar]
- 167.Hasselbalch H. C. Perspectives on chronic inflammation in essential thrombocythemia, polycythemia vera, and myelofibrosis: Is chronic inflammation a trigger and driver of clonal evolution and development of accelerated atherosclerosis and second cancer? Blood. 2012;119(14):3219–3225. doi: 10.1182/blood-2011-11-394775. [DOI] [PubMed] [Google Scholar]
- 168.Griner L. N., Mcgraw K. L., Johnson J. O., List A. F., Reuther G. W. JAK2-V617F-mediated signalling is dependent on lipid rafts and statins inhibit JAK2-V617F-dependent cell growth. British Journal of Haematology. 2013;160(2):177–187. doi: 10.1111/bjh.12103. [DOI] [PMC free article] [PubMed] [Google Scholar]