Abstract
Background
Public health is increasingly concerned with recognising factors that lead to sex differences in stroke. We conducted a study to determine the effect of sex on knowledge of stroke risk factors and warning signs, and how both are perceived, in a representative sample of adults.
Methods
A representative sample of the population of Extremadura, Spain was selected using a double randomisation technique. Previously trained medical students carried out face-to-face interviews using a structured questionnaire.
Results
2409 subjects were interviewed [59.9 % women; mean age (SD) 49.0 (18.7) years]. Seventy-three percent of all subjects reported at least one correct warning sign of stroke (OR: 1.01; 95 % CI: 0.84–1.21). The most frequently mentioned warning signs were sudden weakness, dizziness, and headache. There were no sex differences regarding the types of warning symptoms that respondents listed. Women displayed better knowledge of risk factors than men (OR: 1.23; 95 % CI: 1.05–1.46). Women were more likely to name hypertension as a risk factor for stroke whereas men more frequently listed smoking, alcohol consumption and a sedentary lifestyle as risk factors. In response to stroke, women were significantly less likely than men to choose to call an ambulance or to go immediately to hospital (OR: 0.69; 95 % CI: 0.60–0.85).
Conclusions
Stroke knowledge is suboptimal in both men and women. We detected better knowledge of stroke risk factors in women, as well as differences in the type of risk factors listed by men and women. There were significant sex differences regarding response to stroke or to its warning signs.
Electronic supplementary material
The online version of this article (doi:10.1186/s13104-015-1582-1) contains supplementary material, which is available to authorized users.
Keywords: Gender, Stroke, Knowledge, Warning signs, Risk factors, Education, Population survey, Women
Background
Prompt recognition of stroke symptoms is critical to timely treatment and women have increased delay to treatment [1]. It is known that stroke is more harmful to women in terms of mortality, functional prognosis, and impact on quality of life. Some studies have shown that women delay going to hospital significantly compared to men, and that they are attended later than men after reaching the hospital [2, 3]. Plausible explanations for these delays are unclear, although they may be due in part to sex-related differences in clinical presentation [4] and also to differences in patients’ knowledge of stroke and response to symptoms.
Numerous studies carried out in the past few years have evaluated knowledge of stroke in the general population, but far fewer of them have analysed sex differences, especially in Europe [5–11]. According to available data, the population’s general knowledge of stroke, its risk factors and warning signs, and response in the event of stroke or stroke symptoms show room for improvement [12]. Limited knowledge can contribute to delays in seeking medical attention after stroke onset, which may have repercussions on the final outcome [13].
The aim of the present study is to identify any sex differences in knowledge of stroke, its vascular risk factors and warning symptoms, illness perception, and attitude towards strokes in a representative sample of adults in the general population.
Methods
The sample included 2409 subjects older than 18, randomly selected and surveyed with face-to-face interviews. The census districts in Extremadura provided the information used in participant selection. District information is available in the database kept by Spain’s national statistics institute (INE) and our study used data corresponding to January 1, 2008.
The survey instrument was a structured questionnaire divided into four sections with open-and closed-ended questions. The first section of the questionnaire collected information on sociodemographic variables. The second section contained a list of open-ended questions about knowledge of stroke, its symptoms and risk factors, and unhealthy habits. The third section consisted of open-ended questions about the respondent’s hypothetical response to presenting or witnessing signs of a cerebrovascular event, and upon suspecting stroke or transient ischaemic attack (TIA) in a family member or himself/herself. The fourth section contained questions about the respondent’s experiences with the disease and presence of any risk factors or unhealthy habits. The study was approved by the hospital ethics committee. A copy of the final questionnaire may be requested from the corresponding author. A summary of the questionnaire as Additional file 1 is included.
The procedure for collecting information was face-to-face interview. Interviews were conducted by medical students at the University of Extremadura who had previously been trained in the interview method by the research group. Equal numbers of interviews were assigned to each population unit. For each population unit, researchers extracted a second random sample; this one was neighbourhood-specific and every neighbourhood had the same likelihood of being selected. This process yielded a selected street and an alternate street. Each interviewer started at the first house on the list and interviewed the individual who opened the door if that person met eligibility criteria.
Eligible candidates were individuals older than 18 residing in Extremadura who had no cognitive impairment and were willing to participate in the study. All participants gave their express permission to participate. The subject received a copy of the signed and dated consent form.
Analysis
Data analyses were performed using SPSS software version 15.0 (SPSS Inc.). Some of the variables were recoded as discrete variables to facilitate logistic regression analysis. Knowledge of warning symptoms and classic risk factors was encoded as naming one or more appropriate responses, or none. The dependent variable “hypothetical response to warning symptoms or stroke” was categorised as appropriate (going immediately to hospital or calling the emergency number) or inappropriate (all other options). For purpose of this analysis, subjects were classified by age as younger than 65 or 65 and older. The total sample was also divided into deciles in order to evaluate knowledge by age groups.
We completed a sex-based logistic regression analysis to examine demographic and socioeconomic variables, previous experience with the disease, and presence of vascular risk factors.
Results
Sample profile
The final sample comprised 967 men (40.1 %) and 1442 women (59.9 %). There were no significant differences with regard to age or area of residence (Table 1).
Table 1.
Sociodemographic features and self-reported life-style and medical conditions related to stroke in the study sample by gender
| Men n = 967 | Women n = 1442 | p | |||
|---|---|---|---|---|---|
| Age in years, median, IQR | 48 | 31.8 | 49 | 28.5 | 0.082 |
| Rural residence, n % | 246 | 25.4 | 381 | 26.4 | 0.587 |
| Education level, n % | 0.001 | ||||
| Tertiary | 265 | 27.9 | 330 | 23.3 | |
| Secondary | 259 | 27.3 | 335 | 23.6 | |
| Primary | 304 | 32.0 | 507 | 35.8 | |
| No studies | 121 | 21.8 | 245 | 17.3 | |
| Prefer not to answer | 18 | 1.9 | 25 | 1.7 | |
| Income €/year, n % | <0.001 | ||||
| ≤30,000 | 606 | 62.6 | 886 | 61.5 | |
| >30,000 | 91 | 9.4 | 45 | 3.1 | |
| Prefer not to answer | 270 | 27.9 | 511 | 35.4 | |
| Occupational status, n % | <0.001 | ||||
| Employed full-time | 503 | 52.0 | 632 | 43.9 | |
| Unemployed | 102 | 10.5 | 307 | 21.3 | |
| Others | 355 | 36.7 | 402 | 28.0 | |
| Prefer not to answer | 7 | 0.7 | 99 | 6.9 | |
| Vascular risk factor, n % | |||||
| Hypertension | 231 | 23.9 | 339 | 23.5 | 0.795 |
| Dyslipidaemia | 261 | 27.0 | 304 | 21.1 | 0.001 |
| Diabetes | 90 | 9.3 | 138 | 9.6 | 0.892 |
| Smoking | 400 | 41.4 | 372 | 25.8 | 0.010 |
| Alcohol | 252 | 26.1 | 65 | 4.5 | 0.001 |
| Moderate/morbid obesity | 168 | 17.5 | 119 | 13.7 | <0.001 |
Thirty-three men and 49 women (3.4 % of each group) reported having suffered a stroke and were able to certify it with medical records. Mean age was 65.1 in females and 68.2 in males. A similar number of respondents stated that a first degree-relative had suffered cerebrovascular disease by sex: 33.4 % of the men and 33.7 % of the women.
Knowledge of stroke
More women (85.6 vs 82.6 %; p = 0.038) knew what cerebrovascular diseases are. And, more women than men (44.3 vs 39.0 %; p = 0.035) were familiar with the term “ictus”, the term approved in Spain to denote cerebrovascular event. Most respondents identified the brain as the organ affected by stroke: 70.8 % of men and 72.2 % of women (p = 0.284). However, 15.1 % of men and 13.6 % of women erroneously named the heart (p = 0.324).
Knowledge of stroke warning signs (SWS)
Knowledge of SWS was tested with open-ended questions and data were later recoded for analysis in logical categories. Respondents able to correctly name at least one warning sign of the disease accounted for 73.4 % of the men and 73.6 % of the women. The mean number of listed symptoms was similar between the sexes: 1.42 (SD: 1.2) for men and 1.43 (SD: 1.2) for women (P = 0.871). Likewise, there were no significant sex differences for the type of warning signs that were listed. The most commonly reported stroke symptoms were paralysis/loss of strength, dizziness/instability, and headache. Other warning signs, such as language impairment and vision or sensory disturbances, were reported by less than 1 out of every 8 respondents regardless of sex (Table 2). Facial paralysis was not named as a SWS by any of the respondents. Non-neurological symptoms, such as chest pain or difficulty breathing, were reported by 13.8 % of the men and 13.2 % of the women.
Table 2.
Stroke warning signs and risk factors reported by survey respondents answering open-ended questions
| Men | Women | p | |||||
|---|---|---|---|---|---|---|---|
| n | % | 95 % CIa | n | % | 95 % CIa | ||
| Signs and symptoms | |||||||
| Paralysis/weakness | 302 | 31.8 | 28.9–34.8 | 443 | 30.7 | 28.4–33–1 | 0.790 |
| Dizziness/lack of balance | 301 | 31.2 | 28.3–34.1 | 439 | 30.4 | 28.1–32.8 | 0.721 |
| Headache | 288 | 29.8 | 26.9–32.7 | 444 | 30.7 | 28.4–33.2 | 0.528 |
| Altered consciousness | 151 | 15.6 | 13.4–18.0 | 219 | 15.2 | 13.4–17.1 | 0.775 |
| Sudden difficulty speaking | 105 | 10.8 | 9.1–13.0 | 185 | 12.8 | 11.2–14.7 | 0.145 |
| Blurred vision, loss of vision | 96 | 9.9 | 8.2–12.0 | 146 | 10.1 | 8.7–11.8 | 0.874 |
| Numbness, dead sensation | 72 | 7.4 | 5.9–9.2 | 110 | 7.6 | 6.4–9.1 | 0.867 |
| Confusion/disorientation | 54 | 5.6 | 4.3–7–2 | 79 | 5.5 | 4.4–6–7 | 0.911 |
| None of the above | 195 | 20.2 | 17.8–22.8 | 295 | 20.5 | 18.5–22.6 | 0.861 |
| No neurological symptoms | 133 | 13.8 | 11.8–16–1 | 191 | 13.2 | 11.6–15–1 | 0.720 |
| Risk factors | |||||||
| Smoking | 519 | 53.7 | 50.5–56.8 | 696 | 48.3 | 45.7–50.8 | 0.009 |
| Unhealthy diet | 393 | 40.6 | 37.6–43.8 | 623 | 43.2 | 40.7–45.8 | 0.211 |
| High blood pressure | 320 | 33.1 | 30.2–36.1 | 584 | 40.5 | 37.9–43.1 | 0.002 |
| Alcohol | 460 | 47.6 | 44.3–50.7 | 583 | 40.3 | 37.9–42.9 | 0.005 |
| Lack of exercise/unhealthy lifestyle | 313 | 32.4 | 29.5–35.4 | 386 | 26.7 | 24.5–29.1 | 0.002 |
| High cholesterol | 244 | 25.2 | 22.6–28.9 | 361 | 25.0 | 22.8–27.3 | 0.912 |
| Heart disease | 174 | 17.9 | 15.7–20.5 | 280 | 19.4 | 17.5–21.5 | 0.381 |
| Stress | 155 | 16.0 | 13.8–18.5 | 256 | 17.8 | 15.8–19.8 | 0.270 |
| Diabetes | 129 | 13.3 | 11.3–15.6 | 213 | 14.8 | 13.0–16.7 | 0.323 |
| Obesity | 145 | 14.9 | 12.8–17.4 | 190 | 13.2 | 11.5–15.0 | 0.206 |
| Dementia | 30 | 3.1 | 2.2–4.4 | 53 | 3.7 | 2.8–4.7 | 0.449 |
| Atherosclerosis | 21 | 2.1 | 1.4–3.3 | 26 | 1.8 | 1.2–2.6 | 0.521 |
| Atrial fibrillation | 16 | 1.6 | 1.0–2.7 | 18 | 1.2 | 0.8–1.9 | 0.407 |
Breakdown by sex
95 % CI 95 % confidence interval for proportions
aExact method
Among respondents older than 65, both men (OR: 0.5; 95 % CI: 0.4–0.6) and women (OR: 0.4; 95 % CI: 0.3–0.5) were less likely to name at least one warning sign of stroke. Figure 1 shows that knowledge of at least one SWS, broken down by age, follows an inverted U distribution, with fewer individuals among both the youngest and oldest respondents demonstrating knowledge of stroke.
Fig. 1.
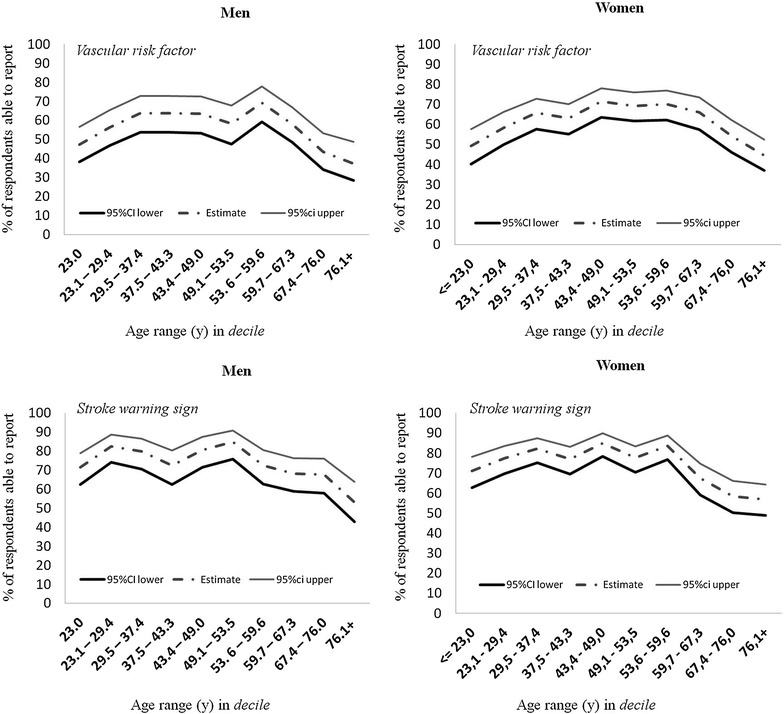
Percentage of respondents able to report at least one stroke warning sign or vascular risk factor broken down by sex and age
Area of residence did not significantly influence ability to cite more than one warning symptom, whereas knowledge of symptoms showed a clear and proportional increase with higher educational or income levels. Women with high blood pressure had a significantly better knowledge of SWS (OR: 1.7; 95 % CI: 1.3–2.3). This was also applicable to people with diabetes, regardless of sex. Other participants with vascular risk factors did not display better knowledge; in fact, rates were significantly worse in at-risk groups such as obese men (OR: 0.5; 95 % CI :0.4–0.8), overweight women (OR: 0.6; 95 % CI: 0.5–0.8), obese women (OR: 0.6; 95 % CI: 0.4–0.8) and women with dyslipidaemia (OR: 0.7; 95 % CI: 0.5–0.9). Personal or family experience with the disease was only associated with better knowledge of SWS in women (OR: 1.5; 95 % CI: 1.1–1.9) (Table 3, part 1).
Table 3.
Sex differences in stroke knowledge broken down by self-reported risk factors and experience with stroke
| Men | Women | |||||
|---|---|---|---|---|---|---|
| OR | 95 % CI | P | OR | 95 % CI | P | |
| Part 1. Knowledge of at least one warning sign | ||||||
| Vascular risk factor | ||||||
| Age > 65 years | 0.5 | 0.4–0.6 | <0.0001 | 0.4 | 0.3–0.5 | <0.0001 |
| Hypertension | 1.2 | 0.8–1.6 | 0.357 | 1.7 | 1.3–2.3 | <0.0001 |
| Diabetes | 1.6 | 1.0–2.6 | 0.029 | 1.5 | 1.0–2.2 | 0.032 |
| Dyslipidaemia | 1.3 | 0.9–1.8 | 0.128 | 0.7 | 0.5–0.9 | 0.006 |
| Smoking | 0.9 | 0.7–1.3 | 0.859 | 0.8 | 0.6–1.1 | 0.052 |
| Overweight | 1.2 | 0.8–1.7 | 0.277 | 0.6 | 0.5–0.8 | 0.001 |
| Obesity | 0.5 | 0.4–0.8 | 0.001 | 0.6 | 0.4–0.8 | 0.002 |
| Stroke experience | ||||||
| Personal | 2.1 | 0.8–5.4 | 0.139 | 1.2 | 0.6–2.5 | 0.524 |
| Relatives | 1.3 | 0.9–1.8 | 0.740 | 1.5 | 1.1–1.9 | 0.003 |
| Part 2. Knowledge of at least one risk factor | ||||||
| Vascular risk factor | ||||||
| Age > 65 years | 0.5 | 0.4–0.6 | <0.0001 | 0.5 | 0.4–0.7 | <0.0001 |
| Hypertension | 0.6 | 0.5–0.9 | 0.003 | 1.1 | 0.8–1.4 | 0.539 |
| Diabetes | 0.9 | 0.6–1.5 | 0.825 | 1.1 | 0.7–1.5 | 0.788 |
| Dyslipidaemia | 1.4 | 1.1–2.0 | 0.010 | 0.7 | 0.5–0.9 | 0.007 |
| Smoking | 1.2 | 0.9–1.5 | 0.172 | 0.8 | 0.7–1.1 | 0.207 |
| Overweight | 0.9 | 0.7–1.3 | 0.947 | 0.9 | 0.7–1.1 | 0.865 |
| Obesity | 0.7 | 0.5–1.0 | 0.684 | 0.7 | 0.5–0.9 | 0.680 |
| Stroke experience | ||||||
| Personal | 0.9 | 0.5–1.8 | 0.855 | 0.8 | 0.5–1.5 | 0.548 |
| Relatives | 1.5 | 1.1–1.9 | 0.008 | 1.8 | 1.4–2.4 | <0.0001 |
Univariate analysis
95 % CI 95 % confidence interval, OR Odds Ratio
Knowledge of stroke risk factors
Open-ended questions were also used to test knowledge of stroke risk factors. Respondents able to name at least one vascular risk factor accounted for 61.2 % of women and 56.1 % of men. Women were more likely than men to name one or more risk factors (OR: 1.23; 95 % CI: 1.05–1.46). The risk factors most frequently named by both sexes were tobacco, alcohol, poor diet, high blood pressure, and sedentary lifestyle. High cholesterol level was named by 1 in 4 respondents, diabetes by approximately 1 in 8, and atrial fibrillation by 1/100 respondents (Table 2). Men were more likely to name tobacco (OR: 1.24; 95 % CI: 1.05–1.46), alcohol (OR: 1.33; 95 % CI: 1.13–1.60) and sedentary lifestyle (OR: 1.31; 95 % CI: 1.10–1.56), whereas women were significantly more likely to name high blood pressure, the main risk factor for stroke (OR: 0.72; 95 % CI: 0.61–0.86).
As with knowledge of warning signs, respondents older than 65 were less able to name at least one classic risk factor, this was true of both men and women. Figure 1 shows that knowledge of at least one risk factor broken down by age group follows an inverted U-shaped distribution.
Residents of rural areas were significantly less likely than urban residents to name more than one risk factor. Educational and income levels also exerted a clear and proportional effect. Interestingly, respondents with vascular risk factors did not display a better knowledge, except for men with dyslipidaemia (OR: 1.40; 95 % CI: 1.11–2.00). A prior history of stroke was not associated with better knowledge of risk factors. However, having witnessed the disease in one’s family was linked to better knowledge of stroke (Table 3, part 2).
Response to stroke
Respondents were asked open-ended questions with no clues about their hypothetical response to experiencing different symptoms suggesting stroke. Next, they were asked how they would respond if they believed they were experiencing a stroke or a TIA. Symptoms causing the most concern in the general population were alterations of consciousness, sudden onset of weakness, and difficulty speaking; visual disturbances and intense headache caused the least concern. Significantly more men than women selected an appropriate response for all listed symptoms: alterations of consciousness (OR: 1.44; 95 % CI: 1.18–1.76), sudden weakness (OR: 1.33; 95 % CI: 1.11–1.60), language impairment (OR: 1.35; 95 % CI: 1.14–1.60), visual disturbances (OR: 1.40; 95 % CI: 1.10–1.65) and headache (OR: 1.27; 95 % CI: 1.08–1.50). Regardless of sex, we observed that appropriate response to all symptoms was clearly less frequent among older respondents.
An appropriate response to a suspected stroke was indicated by 83.4 % of men and 77.5 % of women. The difference between men’s and women’s response to stroke was statistically significant (OR: 1.45; 95 % CI: 1.18–1.79), and it remained after adjusting for age, area of residence, educational level and income level (OR: 1.32; 95 % CI: 1.01–1.73). Responses given by participants with vascular risk factors were poor overall, and only female smokers indicated more appropriate responses to suspected stroke (OR: 1.86; 95 % CI: 1.36–2.55). Rates of appropriate responses in women with hypertension, and in men with hypertension, diabetes, and dyslipidaemia, were significantly lower than in subjects without these risk factors. Respondents with a history of stroke were not more likely to respond appropriately in the event of an additional stroke. In fact, this group’s rate of correct responses was significantly lower than that of the rest of the population in both sexes: men (OR: 0.38; 95 % CI: 0.18–0.79) and women (OR: 0.31; 95 % CI: 0.17–0.55). Experience with the disease in the family was not associated with higher rates of appropriate responses to suspected stroke in either men (p = 0.190) or women (p = 0.317).
Upon suspecting a TIA, men would be more likely than women to go immediately to the hospital or call the emergency number (45.1 vs 38.8 %). These differences were found to be significant in the univariate analysis (OR: 1.29; 95 % CI: 1.10–1.52), but they were no longer significant after adjusting for age, area of residence, educational level and income level (p = 0.449) (Fig. 2).
Fig. 2.

Percentage of appropriate responses planned in the event of acute stroke, TIA, or listed stroke symptoms. Breakdown by sex
Discussion
Stroke knowledge has been addressed by many population-based cross-sectional studies, although few of them have investigated sex effects [14].
Previous studies have defined knowledge of cerebrovascular disease symptoms as the ability to name one or more warning signs in response to open-ended questions [15]. Our study found no significant sex differences in the number of correctly identified SWS or the type of signs mentioned. Most of the studies conducted in Western countries have shown either that women are more able to name warning signs of stroke [9, 16–21] or that no significant sex differences are present [6, 22, 23]. A study conducted more than 10 years ago in Spain showed that only 32.6 % of the population was able to identify at least one SWS and that men were considerably more knowledgeable about stroke than women [5]. However, as confirmed by our study, the situation in Spain has clearly changed over time. More than 70 % of this population is able to name at least one symptom of stroke. As reported by other studies [6, 8, 9, 18], the most frequently named warning symptoms were paralysis, dizziness, and headache. Approximately 1 out of every 8 individuals wrongly identified chest pain and shortness of breath as SWS; this reflects the confusion between ischaemic heart disease and stroke in part of the general population [15, 17]. The factors associated with a better knowledge of stroke symptoms are being younger than 65, higher educational level, and higher income level. Similar findings have been published in earlier studies [5, 12]. Other studies have also reported that individuals with a history of stroke or vascular risk factors do not display more ample knowledge of the disease [18, 22, 24]. These findings have important implications for health education, since this population is at the most risk for stroke. In our study, only women with high blood pressure and individuals with diabetes seemed to be better informed.
Women in our population display considerably more knowledge of risk factors than men, which coincides with findings from other studies [15–17]. Few studies have shown a greater knowledge of stroke risk factors among men [5]. There are differences between the types of vascular risk factors listed by men and women. While men more frequently named risk factors associated with lifestyle, women were more likely to cite medical conditions such as high blood pressure. A possible explanation for this tendency is that women seem to be better informed about disease prevention than men, and they may also be more interested in health-related issues [14].
Few studies have examined sex differences in response to stroke [5, 9, 23, 25, 27]. Concerning immediate response to stroke or its warning signs, men are significantly more likely than women to call an ambulance or go immediately to hospital. These differences remain after adjusting for age, residence or socioeconomic level, factors shown by previous research to be associated with a more appropriate response to stroke [20, 25–27]. These findings are especially relevant since some studies reveal that women tend to delay going to hospital more than men [2, 3, 28]. Prehospital delay is known to be one of the major factors limiting use of reperfusion therapy for stroke because stroke has a narrow therapeutic window [29]. A meta-analysis showed that thrombolytic treatment was more effective in women than in men. However, proportionally fewer women than men do not receive tPA after acute stroke [30]. Fewer women than men reach hospital within the first hours after symptom onset, and this observation may partially explain why women are less likely to be treated with thrombolysis [4]. There is no reasonable explanation for this tendency, although we suggest that men and women may not perceive the severity of the disease in the same way, and women may underestimate the urgency of warning signs. Some studies have shown that while women are aware that cardiovascular disease is one of the main causes of death, only a small percentage of them regard ischaemic heart disease and stroke as the greatest threat to their health [29]. This misperception may be one of the obstacles to women who require medical attention.
Our study has some methodological limitations. First, the survey may have a selection bias since the numbers of male and female participants did not match exactly. Second, there may also be a non-response bias, given that individuals who refused to participate or could not be contacted might have a different level of stroke knowledge. Third, results depend on the type of questionnaire; in face-to-face interviews, the interviewer may unintentionally influence the results and lead to inconsistent measurements. Lastly, cross-sectional studies cannot prove causality.
A number of tests have been developed to assess specific stroke knowledge, including the stroke symptom questionnaire, stroke action test, and stroke awareness questionnaire, in which residents learn how to dial 911, etc., for general directions when a stroke has occurred [31]. However, there are presently few references to methods assessing community resident knowledge regarding ways to cope with pre-hospital stroke symptoms in the scientific literature. Therefore, other limitation of this job is that no psychometric properties that show the validity and reliability of this type of survey.
Conclusions
Severity of stroke symptoms, mortality rates, and residual disability rates are higher in women, which results in lower quality of life after stroke [1, 2]. Stroke’s differential effect on women will continue to gain importance in the decades to come. Therefore, public awareness campaigns must be implemented to increase knowledge of stroke in the general population and make women aware of the importance of going immediately to hospital if they experience warning signs of stroke. Both the general population and the scientific and medical communities stand to benefit from better education on stroke.
Authors’ contributions
Author contributions to the study and manuscript preparation include the following. JMRM had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: JMRM. Acquisition of data: JMRM, RAG and MVMN. Analysis and interpretation of data: JMRM, RAG, MVMN, DPP, and JJAS. Drafting of the manuscript: JMRM. Critical revision of the manuscript for important intellectual content: MRM, RAG, MVMN, DPP, and JJAS. All authors read and approved the final manuscript.
Acknowledgements
This study was supported by a grant from Neuroscience research projects, FUNDESALUD and Neurology Society of Extremadura (FUNNE0901). The authors appreciate assistance from the Research Area of the Spanish Society of Neurology.
Competing interests
Financial competing interests: I disclose that we haven’t received any reimbursements, fees, funding, or salary from an organization in the past 5 year that may in any way gain or lose financially from the publication of this manuscript, either now or in the future. We don’t hold any stocks or shares in an organization that may in any way gain or lose financially from the publication of this manuscript, either now or in the future. We don’t hold or aren’t applying for any patents relating to the content of the manuscript. We haven’t received any reimbursements, fees, funding, or salary from an organization that holds or has applied for patents relating to the content of the manuscript. We don’t have any other financial competing interests.Non-financial competing interests: There aren’t any non-financial competing interests (political, personal, religious, ideological, academic, intellectual, commercial or any other) to declare in relation to this manuscript.
Abbreviations
- SD
standard deviation
- OR
odds ratio
- CI
confidence interval
- TIA
transient ischaemic attack
- SWS
stroke warning signs
- tPA
tissue plasminogen activator
Additional file
10.1186/s13104-015-1582-1 Description of the survey instrument.
Contributor Information
José M. Ramírez-Moreno, Phone: 0034218100, Email: j.ramrez@gmail.com
Rafael Alonso-González, Email: r.alonso@rbht.nhs.uk.
Diego Peral-Pacheco, Email: diego@unex.es.
María Victoria Millán-Núñez, Email: victoria.minu@hotmail.com.
José J. Aguirre-Sánchez, Email: josejavieraguirre@jjneuro.e.telefonica.net
References
- 1.The Lancet Neurology Sex differences and stroke prevention. Lancet Neurol. 2014;13(4):339. doi: 10.1016/S1474-4422(14)70057-2. [DOI] [PubMed] [Google Scholar]
- 2.Foerch C, Misselwitz B, Humpich M, Steinmetz H, Neumann-Haefelin T, Sitzer M, for the Arbeitsgruppe Schlaganfall Hessen Sex disparity in the access of elderly patients to acute stroke care. Stroke. 2007;38:2123–2126. doi: 10.1161/STROKEAHA.106.478495. [DOI] [PubMed] [Google Scholar]
- 3.Mandelzweig L, Goldbourt U, Boyko V, Tanne D. Perceptual, social, and behavioral factors associated with delays in seeking medical care in patients with symptoms of acute stroke. Stroke. 2006;37:1248–1253. doi: 10.1161/01.STR.0000217200.61167.39. [DOI] [PubMed] [Google Scholar]
- 4.Di Carlo A, Lamassa M, Baldereschi M, et al. Sex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe: data from a multicenter multinational hospital-based registry. Stroke. 2003;34:1114–1119. doi: 10.1161/01.STR.0000068410.07397.D7. [DOI] [PubMed] [Google Scholar]
- 5.Segura T, Vega G, Lopez S, Rubio F, Castillo J. Public perception of stroke in Spain. Cerebrovasc Dis. 2003;16:21–26. doi: 10.1159/000070110. [DOI] [PubMed] [Google Scholar]
- 6.Parahoo K, Thompson K, Cooper M, Stringer M, Ennis E, McCollan P. Stroke: awareness of the signs, symptoms and risk factors—a population-based survey. Cerebrovasc Dis. 2003;16:134–140. doi: 10.1159/000070593. [DOI] [PubMed] [Google Scholar]
- 7.Müller-Nordhorn J, Nolte CH, Rossnagel K, et al. Knowledge about risk factors for stroke. A population-based survey with 28090 participants. Stroke. 2006;37:946–950. doi: 10.1161/01.STR.0000209332.96513.82. [DOI] [PubMed] [Google Scholar]
- 8.Neau JP, Ingrand P, Godeneche G. Awareness within the French population concerning stroke signs, symptoms, and risk factors. Clin Neurol Neurosurg. 2009;111:659–664. doi: 10.1016/j.clineuro.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 9.Hickey A, Holly D, McGee H, Conroy R, Shelley E. Knowledge of stroke risk factors and warning signs in Ireland: development and application of the Stroke Awareness Questionnaire (SAQ) Int J Stroke. 2012;7:298–306. doi: 10.1111/j.1747-4949.2011.00698.x. [DOI] [PubMed] [Google Scholar]
- 10.Baldereschi M, Di Carlo A, Vaccaro C, Polizzi B, Inzitari D. Promotion implementation of stroke care in Italy project working group. Stroke knowledge in Italy. Neurol Sci. 2015;36:415–421. doi: 10.1007/s10072-014-1964-5. [DOI] [PubMed] [Google Scholar]
- 11.Madsen TE, Baird KA, Silver B, Gjelsvik A. Analysis of gender differences in knowledge of stroke warning signs. J Stroke Cerebrovasc Dis. 2015;24:1540–1547. doi: 10.1016/j.jstrokecerebrovasdis.2015.03.017. [DOI] [PubMed] [Google Scholar]
- 12.Jones SP, Jenkinson AJ, Leathley MJ, Watkins CL. Stroke knowledge and awareness: an integrative review of the evidence. Age Ageing. 2010;39:11–22. doi: 10.1093/ageing/afp196. [DOI] [PubMed] [Google Scholar]
- 13.Kwan J, Hand P, Sandercock P. A systematic review of barriers to delivery of thrombolysis for acute stroke. Age Ageing. 2004;33:116–121. doi: 10.1093/ageing/afh064. [DOI] [PubMed] [Google Scholar]
- 14.Stroebele N, Müller-Riemenschneider F, Nolte CH, Müller-Nordhorn J, Bockelbrink A, Willich SN. Knowledge of risk factors, and warning signs of stroke: a systematic review from a gender perspective. Int J Stroke. 2011;6:60–66. doi: 10.1111/j.1747-4949.2010.00540.x. [DOI] [PubMed] [Google Scholar]
- 15.Yoon SS, Heller RF, Levi C, Wiggers J, Fitzgerald PE. Knowledge of stroke risk factors, warning symptoms and treatment among an Australian urban population. Stroke. 2001;32:1926–1930. doi: 10.1161/01.STR.32.8.1926. [DOI] [PubMed] [Google Scholar]
- 16.Pancioli AM, Broderick J, Kothari R, et al. Public perception of stroke warning signs and knowledge of potential risk factors. JAMA. 1998;279:1288–1292. doi: 10.1001/jama.279.16.1288. [DOI] [PubMed] [Google Scholar]
- 17.Reeves MJ, Hogan JG, Rafferty AP. Knowledge of stroke risk factors and warning signs among Michigan adults. Neurology. 2002;59:1547–1552. doi: 10.1212/01.WNL.0000031796.52748.A5. [DOI] [PubMed] [Google Scholar]
- 18.Schneider AT, Pancioli AM, Khoury JC, et al. Trends in community knowledge of the warning signs and risk factors for stroke. JAMA. 2003;289:343–346. doi: 10.1001/jama.289.3.343. [DOI] [PubMed] [Google Scholar]
- 19.Silver FL, Rubini F, Black D, Hodgson CS. Advertising strategies to increase public knowledge of the warning signs of stroke. Stroke. 2003;34:1965–1969. doi: 10.1161/01.STR.0000083175.01126.62. [DOI] [PubMed] [Google Scholar]
- 20.Nedeltchev K, Fischer U, Arnold M, Kappeler L, Mattle HP. Low awareness of transient ischemic attacks and risk factors of stroke in a Swiss urban community. J Neurol. 2007;254:179–184. doi: 10.1007/s00415-006-0313-x. [DOI] [PubMed] [Google Scholar]
- 21.Reeves MJ, Rafferty AP, Aranha AA, Theisen V. Changes in knowledge of stroke risk factors and warning signs among Michigan adults. Cerebrovasc Dis. 2008;25:385–391. doi: 10.1159/000121338. [DOI] [PubMed] [Google Scholar]
- 22.Sug Yoon S, Heller RF, Levi C, Wiggers J, Fitzgerald PE. Knowledge of stroke risk factors, warning symptoms, and treatment among an Australian urban population. Stroke. 2001;32:1926–1930. doi: 10.1161/01.STR.32.8.1926. [DOI] [PubMed] [Google Scholar]
- 23.Weltermann BM, Homann J, Rogalewski A, Brach S, Voss S, Ringelstein EB. Stroke knowledge among stroke support group members. Stroke. 2003;31:1230–1233. doi: 10.1161/01.STR.31.6.1230. [DOI] [PubMed] [Google Scholar]
- 24.Greenlund KJ, Neff LJ, Zheng Z-J, et al. Low public recognition of major stroke symptoms. Am J Prev Med. 2003;25:315–319. doi: 10.1016/S0749-3797(03)00206-X. [DOI] [PubMed] [Google Scholar]
- 25.Pandian JD, Jaison A, Deepak SS, et al. Public awareness of warning symptoms, risk factors, and treatment of stroke in Northwest India. Stroke. 2005;36:644–648. doi: 10.1161/01.STR.0000154876.08468.a0. [DOI] [PubMed] [Google Scholar]
- 26.Johnston SC, Fayad PB, Gorelick PB, et al. Prevalence and knowledge of transient ischaemic attack among US adults. Neurology. 2003;60:1429–1434. doi: 10.1212/01.WNL.0000063309.41867.0F. [DOI] [PubMed] [Google Scholar]
- 27.Mikulık R, Bunt L, Hrdlicka D, Dusek L, Vaclavık D, Kryza J. Calling 911 in response to stroke: a nationwide study assessing definitive individual behavior. Stroke. 2008;39:1844–1849. doi: 10.1161/STROKEAHA.107.499806. [DOI] [PubMed] [Google Scholar]
- 28.Menon SC, Pandey DK, Morgenstern LB. Critical factors determining access to acute stroke care. Neurology. 1998;51:427–432. doi: 10.1212/WNL.51.2.427. [DOI] [PubMed] [Google Scholar]
- 29.Moser DK, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation. 2006;114:168–182. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- 30.Kent DM, Price LL, Ringleb P, Hill MD, Selker HP. Sex-based differences in response to recombinant tissue plasminogen activator in acute ischemic stroke: a pooled analysis of randomized clinical trials. Stroke. 2005;36:62–65. doi: 10.1161/01.STR.0000150515.15576.29. [DOI] [PubMed] [Google Scholar]
- 31.Zhao Q, Yang L, Zhang X, Zhu X, Zuo Q, Wu Y, et al. Development and validation of the pre-hospital stroke symptoms coping test. PLoS One. 2014;9(10):e110022. doi: 10.1371/journal.pone.0110022. [DOI] [PMC free article] [PubMed] [Google Scholar]


