Abstract
Positron emission tomography (PET) is widely used nowadays for tumor staging and therapy response in the clinic. However, average PET radiation exposure has increased due to higher PET utilization. This study aims to review state-of-the-art PET tracer dosage optimization methods after accounting for the effects of human body attenuation and scan protocol parameters on the counting rate. In particular, the relationship between the noise equivalent count rate (NECR) and the dosage (NECR-dosage curve) for a range of clinical PET systems and body attenuation sizes will be systematically studied to prospectively estimate the minimum dosage required for sufficiently high NECR. The optimization criterion can be determined either as a function of the peak of the NECR-dosage curve or as a fixed NECR score when NECR uniformity across a patient population is important. In addition, the systematic NECR assessments within a controllable environment of realistic simulations and phantom experiments can lead to a NECR-dosage response model, capable of predicting the optimal dosage for every individual PET scan. Unlike conventional guidelines suggesting considerably large dosage levels for obese patients, NECR-based optimization recommends: i) moderate dosage to achieve 90% of peak NECR for obese patients, ii) considerable dosage reduction for slimmer patients such that uniform NECR is attained across the patient population, and iii) prolongation of scans for PET/MR protocols, where longer PET acquisitions are affordable due to lengthy MR sequences, with motion compensation becoming important then. Finally, the need for continuous adaptation of dosage optimization to emerging technologies will be discussed.
Keywords: PET, PET/CT, PET/MR, dosage, NECR, optimization, Monte-Carlo
Introduction
Imaging is nowadays considered an essential part of modern nuclear medicine procedures as it provides the means to obtain an abundance of multi-dimensional information for the diagnosis, prognosis and therapy response monitoring of a variety of diseases in the clinic [1]. In particular, positron emission tomography (PET) is an established imaging modality for the in-vivo inspection of a wide spectrum of diseases in oncology [2-4], cardiology [5] and neurology [6]. PET has gained considerable attention in the medical imaging community in the last few decades, over other nuclear imaging techniques, as most of the chemically relevant to human body radioisotopes are positron emitters (11C, 13N, 15O, 18F) and thus can more efficiently label pharmaceutical substances of physiological interest. Meanwhile, the significant evolution of PET scanner technology over the last decades enabled, for the first time, 3D multi-functional imaging of numerous molecular and cellular biochemical processes [4].
Despite the advantages of PET as a metabolic in-vivo imaging modality, acquisition of accurate and high-resolution anatomical information is currently not possible by PET alone due to underlying physical limitations, even when prolonging scan time through transmission acquisitions or when state-of-the-art time-of-flight (TOF) technology is employed. This has led to the introduction of hybrid scanners, such as PET/Computed Tomography (PET/CT) and PET-Magnetic Resonance (PET/MR) systems where the CT or MR modalities can be utilized to obtain the missing anatomical information. Additionally, the development of fully integrated multi-modality PET systems nowadays enables acquisition of anatomical maps that are perfectly co-registered with PET images, thus allowing for the precise localization and attenuation correction of the PET signal, which is very important for quantitative imaging tasks and image-guided therapy [2].
However, radiation exposure can be a serious concern for adult and particularly children patients, especially in the case of PET/CT hybrid systems, due to the ionizing nature of both PET and CT radiation, with the latter contributing to relatively higher absorbed doses than the former modality. Previously, studies assessed the risk of radiation dose absorbed by the human tissue during whole-body PET and CT scans and proposed efficient PET dosage regimens to reduce the total exposure as much as possible, although exposure from CT remains significant [7,8]. Fortunately with the advent of hybrid PET/MR imaging, the total radiation absorbed dose in clinic can be now significantly reduced thanks to the zero contribution of ionizing radiation by MR modality. Therefore, as PET/MR imaging becomes widely applicable, the main effort in further reducing absorbed dose to patients and personnel can be concentrated on the injected dosage minimization without degrading image quality (IQ). The decay rate, or activity, of a positron-emitting radiopharmaceutical is a random process following the well-characterized Poisson distribution [9]. Thus, the acquisition of the PET data is a statistical imaging process characterized by a level of inherent uncertainty, which can be quantified with the statistical index of standard deviation [10]. According to the principles of Poisson distribution, the relative percentage uncertainty in the detected coincidence rate is reduced with higher number of counts and thus, from a statistical point of view, it is highly desirable to be able to achieve the maximum possible counts for a given amount of scan time or equivalently the highest count rate.
However, the type of counts recorded during a PET acquisition can be classified as either true, scattered or random coincidence events, as it will be explained later, of which only the trues accurately reflect the actual underlying radionuclide activity distribution, while scattered and random events contaminate the total signal with misleading information. Thus, a high number of overall detected coincidence events, also known as prompts, do not necessarily translate to higher statistical quality and signal to noise ratio (SNR) for the acquired PET raw data and respective reconstructed images. Instead, the index of noise-equivalent counts could be employed to quantify the net positive contribution or SNR of the prompts. Therefore, retaining a sufficiently high noise-equivalent count rate (NECR), as opposed to prompt counts rate, could be a more reliable strategy to ensure a high SNR for the measured PET data and the respective images for a given scan period.
PET systems detect coincidence events at a particular rate for a given underlying activity distribution in the FOV [9,11]. The measured total coincidences count rate per unit of total activity distribution in the FOV characterizes the sensitivity of a PET scanner [10]. Higher scanner sensitivity can indeed be one of the factors ensuring high NECR and SNR performance, but it is usually fixed for each PET system, thus leaving no margins of data quality optimization. However, another parameter that can drastically affect NECR for a given scanner and could be used for its optimization is the amount of administered radiopharmaceutical dosage [12-14]. Therefore, NECR and consequently SNR, can be significantly regulated for a given scanner or sensitivity, either to a maximum or a sufficiently high value by administering a proper amount of radiopharmaceutical dosage.
Furthermore, the relationship between the administered dosage and the “statistically useful” count rate, i.e. the NECR, of a PET scanner may depend on a range of parameters which can be either scanner-related such as the geometric efficiency, detection efficiency, energy window and dead-time effect [11,13] or patient-related, such as the degree of radiation attenuation caused by the body and the relative position between the targeted source distribution and the current bed field-of-view (FOV) of the scanner [13]. By systematically and quantitatively analyzing the effects of these factors on NECR for a range of dosage levels, an accurate NECR-dosage response model can be designed allowing for the prediction of the minimum possible amount of dosage required to sufficiently maintain NECR, or statistically useful counts, at a quantitatively acceptable level. In the past, many studies [10,14] systematically examined the effect of these factors on different types of PET coincidence count rates (true, random, scatter) and the NECR.
As a result, a possible strategy for the optimization of the administered dosage prior to every individual PET scan could consist of two essential steps: i) Initially, a systematic assessment of the NECR response as a function of the administered dosage needs to be conducted for a family of clinical PET scanners and a variety of patient- and scanner-related study parameters, as described above. This will enable the design of a parameterized model that can adequately describe the NECR-dosage relationship for a wide set of acquisition scenarios often present in clinical routine. Then, ii) such model could be utilized to predict, for a given set of patient attenuation properties and scanner settings, an optimal range of dosagelevels for which a nearly maximal NECR is expected by the model. The terms “range of dosage” and “nearly maximal NECR” imply that the predicted outcome will initially be a range of dosages as opposed to a single value while the final dosage recommendation may correspond to a NECR value close to the peak, expressed as a user-defined percentage (%) of the latter, e.g. at least 90% of the peak NECR for the given set of parameters.
However, the previous dosage regimen scheme may result in highly variable NECR scores among patient scans, as the criterion is a percentage of the peak which may vary significantly across the scan populations, e.g. between slim and obese patients. Alternatively, a dose optimization strategy that would ensure NECR equivalency over a population of patient scans could utilize the same NECR-dosage response model to predict the amount of dosage that would induce a fixed NECR score for all scans, regardless of the patient and scanner factors involved. In that case, the optimal dosage would obviously not correspond to a maximal NECR for all cases, as the previous scheme, but would ensure a sufficient and uniform NECR performance across the population. The losses in NEC counts could then be compensated by accordingly elongating the PET scan duration. This could be applicable i) to some extent, to longer PET/CT protocols, but ii) more efficiently to simultaneous PET-MR protocols, where the lengthy MR acquisitions permit equally long PET acquisitions.
Therefore, the aim of this review is to present a collection of studies demonstrating the feasibility of NECR-based dosage optimization in individual PET studies, after systematically evaluating the dosage effect on NECR for a representative set of patient- and scanner- parameters. Thus, individualized prediction of optimal dosage may become possible prior to every PET scan, paving the way for personalized multimodality PET clinical imaging protocols across a wide range of patients and scanner configurations.
Critical analysis
Coincidence types and their contribution to the actual PET information
PET utilizes trace amounts of positron emitting radiopharmaceuticals (radio-tracers), such as 18F-fluorodeoxyglucose (FDG) [2,4,15]. Each emitted positron travels a short distance (range) before it annihilates with an electron causing the emission of two gamma photons, each of 511 keV energy, at nearly opposite directions [16,17]. Radiotracers emitting positrons of relatively low kinetic energy are preferred to ensure minimum energy (dose) deposition at the point of emission and small travelled distance of the positron (positron range) before its annihilation. Subsequently, the two emitted gamma photons are detected in coincidence by two opposing PET detectors. The line connecting that pair of detectors is known as the line of response (LOR) for that coincident event and defines the geometrical space where the annihilation occurred [16,17]. This type of coincidence event, called ‘true coincidence’, is the desired type of count in PET imaging, as it defines an LOR that includes the actual point of annihilation and thus positively contributes to the true or net PET signal [18]. However, there are also two other possible types of detection events, which are contaminating the overall PET signal with erroneous information: the scattered and random coincidences.
Scattered coincidence events, simply denoted also as “scatter”, occur when at least one of the two emitted gamma photons undergoes Compton scattering when interacting with the patient’s body or a detector crystal before its actual detection, causing it to change direction and thus divert from the true LOR while losing part of its kinetic energy deposited at detection point [16]. Scatter events may still be detectable as coincidences, provided the energy of each scattered photon deposited in PET detectors still lies within the energy window accounted by the PET system. However, the trajectories of two photons, of which at least one has undergone Compton scattering, are no longer aligned with respect to each other, thus violating the basic assumption of 180-degree angle between them and resulting in mispositioned LORs [16,19]. The fraction of scatter to the total number of detected events, known as scatter fraction, depends on the attenuation properties of the imaging subject and detectors as well as the energy window of the system, the latter determined by the finite energy resolution of the detection system.
Similarly, random coincidence events, also known simply as “randoms”, may also trigger LORs mispositioning but through a different mechanism: the nearly simultaneous but accidental (random) detection of two gamma photons produced by different annihilations. As a result, randoms are more likely observed at high-count rates where interference between different but ly simultaneous annihilations is more probable [20,21]. Therefore, random coincidence detection rates depend on the rate of individual gamma photon detections, known as singles rate, which in turn, depends on the rate of gamma photon emissions (activity) within the field-of-view (FOV) [16]. In fact randoms rate is proportional to the square of singles rate, and thus it can become considerable at high activity concentration levels. Furthermore, randoms are expected to increase with the coincidence time window (CTW) width of the scanner, which determines the maximum allowed difference in the estimated detection time between two singles event to be considered as a coincidence event [16]. The slower the detection system is responding to a given rate of incident gamma photons, the larger the uncertainty in estimating the exact time of detection and, thus the larger the CTW width has to be to minimize rejection of true coincidences. Consequently, for a given activity level, wider CTWs are expected to yield higher fraction of random events [16,17,19]. As a result, both scatter and random events reduce image quality (IQ) by degrading spatial resolution and contrast due to inaccuracies caused by LOR mispositioning [18].
Standardized uptake value (SUV) metric and its limitation for image-based PET data quality assessments
One important feature of PET imaging is its ability to acquire quantitative estimates of in-vivo concentration of physiologically relevant radiopharmaceuticals which can later be used for a wide range of quantitative imaging tasks, e.g. for tumor characterization, differentiation and response to therapy in oncology [22]. The activity concentration measurements at every image pixel can be normalized with respect to the total administered PET tracer dosage and the lean body mass or weight of the patient to obtain the surrogate metric of standardized uptake value (SUV), a well-established index in clinical nuclear medicine [22]. However, SUV only reflects the normalized radioactivity concentration present in the tissue of interest at a certain time. As a result, it should be pointed out that SUV may not be considered fully quantitative, as it is inherently time-dependent and can be also influenced by various patient- and scanner-related parameter [23,24].
Recently, Silva-Rodriguez et al. presented a PET simulation framework (Figure 1) consisting of multiple FDG-PET realistic digital phantoms to enable systematic comparative SUV evaluations at various regions of interest (ROIs) between true input and reconstructed simulated PET images for three different SUV calculation methods [22]. Although the study showed the usefulness of SUV metric in evaluating clinically relevant tumor characteristics from PET images, it also demonstrated its high sensitivity to the partial volume effect and statistical noise which can considerably affect detectability and quantification of tumor regions in the reconstructed PET images [22].
Figure 1.

Realistic digital framework of multiple simulated FDG-PET studies. The presented framework enables comparisons of realistic SUV values from reconstructed simulated PET images against the ground truth. Published with permission of the author and the Publisher. Originally published in Silva-Rodriguez J, Aguiar P, Dominguez-Prado I, Fierro P, Ruibal A. Simulated FDG-PET studies for the assessment of SUV quantification methods. Rev Esp Med Nucl Imagen Mol 2015; 34(1): 13-8. Copyright © 2014 Elsevier España, S.L.U. and SEMNIM. All rights reserved [22].
The ALARA principle
The general human population is daily exposed to low levels of ionizing radiation, relative to the safety limits, originated from the universe and long-lived radioisotopes in certain earth locations. However, radiation exposure of the general population due to medical procedures has recently increased on average due to the more extensive usage of radiation in medicine, including nuclear medicine exams, mainly for the purpose of i) diagnosing diseases at earlier stages and assessing their progress, ii) evaluating treatment response and iii) designing optimal image-guided therapeutic schemes. In particular, absorbed radiation dose itself is an important parameter to study, because it may lead to deterministic or stochastic damaging radiobiological effects in living tissues if the safety limits are exceeded [25]. In particular, PET is associated with a relatively low radiation exposure to patients due to internal administration of beta (positron) emitting radiopharmaceuticals. The injected dosage is then distributed over time across the human tissue while emitting gamma ionizing radiation due to the positron annihilation effect [26]. The amount of energy or dose deposited as a result of the interaction of beta and gamma particles with human tissue is proportionally related to the amount of administered dosage. The radiobiological effects of beta and gamma radiation may potentially be harmful at any age, if a very large dosage is administered, although typical PET dosage levels are within safety limits.However, dosage regularization may be particularly important for children and the fetus, which are considered highly radiosensitive [8,27,28-31], primarily because their cells are dividing faster and, secondly, because they have longer life-time ahead to potentially develop long-term stochastic effects, such as carcinogenesis [8]. For instance, young children (5 years old) exposed to radiation from an atomic bomb have 1.7-2.1 greater risk of developing cancer compared to young adults (20 years old) [32]. In addition, unlike dosage-radiobiological risk relationship described above, NECR-dosage curve is not linear, but instead exhibits a peak at moderate dosage levels, as it will be demonstrated later. Thus, very high dosages not only increase exposure, if applied repeatedly, e.g. in longitudinal studies, but also are undesirable as they may in fact diminish statistical quality of the acquired PET data. On the other hand, extremely low dosage levels may as well impact quality, except if proportionally longer PET acquisitions can be afforded, e.g. in the case of PET/MR acquisitions, to compensate for the low NECR [33]. Therefore, radiation exposure should be restricted to levels as low as reasonably achievable (ALARA principle) or avoided if not absolutely necessary for special radiosensitive population members such as children and pregnant women [15,31,34,35].
Thus, the ALARA concept encourages administration of reasonably low or moderate amounts of administered PET dosage after accounting for the available scan time and any other factor that could help further reduce exposure without affecting data quality. It essentially demonstrates both the need for dosage minimization as well as the importance of retaining sufficient or reasonable statistical quality. Therefore, any dosage regularization strategy, as those described in this review article, should follow the ALARA principles. Table 1 presents a collection of human population average exposure levels due to characteristic nuclear medicine exams (left column) and cosmic radiation (right column), as compiled from published reports [2,32,36-38]. Although the occupational dose limit for an adult is only 50 mSv, the ALARA principles should always be followed in medical procedures for the maximum reasonable limitation of patient and personnel exposure.
Table 1.
Radiation exposure for characteristic medical exams and cosmic radiation levels
| Radiation exposure (mSv) | |||
|---|---|---|---|
|
| |||
| Medical Imaging sources | Daily activities and occupations (Cosmic radiation) | ||
| FDG (185 MBq) PET scan | 3-4 | Flight: Montreal to London | 0.0478 |
| CT-chest | 7.0 | Dentistry | 0.06 (annual) |
| PET/CT (non-modified protocol) | 25 | Living at sea level | 0.24 |
| Chest X-ray | 0.1 | Average dose/person (UK) | 2.5 (annual) |
| PET scan (15 yrs old)-modified protocol | 7.6 | Aircrew | 4.5 (annual) |
| CT scan (15 yrs old)-modified protocol | 5.9 | Metal mines | 2.7 (annual) |
| PET/CT scan (15 yrs old)-modified protocol | 13.5 | ||
The importance of thenoise-equivalent counting rate (NECR) metric
An important parameter when evaluating the performance of a PET system is the count rate as a function of the total activity present in the FOV because it can considerably affect the statistical quality and SNR of projection data and IQ of reconstructed images for a given imaging protocol [3]. The inherent uncertainty in coincidence rate measurements is expressed with the presence of noise in the projection and image space. The Poisson properties of the counts distribution in PET measurements suggest lower percentage noise and enhanced SNR when higher numbers of true coincidence counts are acquired. Thus, studies have suggested increasing the amount of injected dosage as an attempt to limit the presence of noise in the acquired PET data [3]. However, this strategy may have negative implications for both the data quality in the projection and image data as well as the patient. In particular, the administration of very large amounts of dosage is expected to i) considerably rise the number of randoms and the associated artifacts, ii) trigger counting losses due to dead-time effect and iii) increase radiation exposure [13]. In other words, not only the total number of counts (prompts) but also their synthesis in trues, scatter and randoms is also important from a statistical point of view, as scatter and randoms are contaminating the measurements.
Thus, an alternative acquisition scheme resulting in similar total number of counts but acquired from a smaller amount of dosage and for longer time period may be more appropriate from a statistical and dosimetric point of view as it will be associated with a larger trues fraction and less radiation exposure for the patient and the personnel. On the other hand, prolonged scan periods may not be clinically feasible, given the high patient throughput requirements in the PET clinic.
A suitable metric to quantify the overall statistical usefulness of the total count rates by taking into account their synthesis is NECR [3,10] and is defined as follows [9]:
NECR = R 2 true/(Rtrue + aRscatter + bRrandom)
where Rtrue, Rscatter and Rrandom denote the true, scatter and random coincidences count rates, respectively. Also ‘Δ’ represents the occupied area in the FOV by the patient while ‘b’ depends on the method used to estimate random events [33]. As its name implies, NECR can be considered as the equivalent trues count rate that would yield to the same level of statistical noise as the one currently present in the measured prompt counts [39].
Random coincidences can be estimated by employing a delayed coincidence window (δ + ΔT) which is time-shifted relative to the standard coincidence window (ΔT) [9]. The use of delayed window allows for the exclusive estimation of random events spatial distribution, thus providing an automated and practical method for online randoms subtraction from the prompts distribution, the latter estimated from the original window [9]. However, random online subtraction can significantly increase the statistical noise in the data. On the other hand, estimation of scatter coincidences is possible by applying a scatter simulation algorithm on registered anatomical images, when the activity distribution is entirely within the scanner FOV [9]. The estimated scatter count profile is then subtracted from the prompts projection profiles. Overall, the true coincidences rate can be estimated by Rtrue = Rprompt - Rscatter - Rrandom [10].
NECR has been evaluated by many studies [10,14,40] as a surrogate metric of statistical quality of acquired projection data. The objective quantitative assessment of the statistical quality of acquired PET raw data offered by the NECR metric could help towards a more efficient optimization of the administered dosage which, in turn, determines the trade-off between competing scanner and patient factors. By modeling the relation between the individual components of NECR response (trues, scatter and randoms) and various patient- and scanner-related factors of PET studies, it is possible to predict the minimum administered dosage required to acquire sufficient noise equivalent counts within a clinically acceptable scan period [13].
The detected coincidence counts at every line of response (LOR) bin in the raw data follow the Poisson distribution. Thus, the standard deviation (δ) of each estimated count rate is expected to be equal to the square root of the measured mean count rates N, i.e. σ= √N, supposing the same activity distribution was measured multiple times. Then, the ratio of the standard deviation of counts to their mean, known as % statistical noise, can be derived by (1√N)×100, where N represents the mean counts in each LOR [41]. Moreover, NECR per pixel denotes the metric of NECR density (NECRD) [42] and is obtained by dividing NECR by the number of image pixels defining the attenuating volume of the scanned patient. On the other hand, the SNR of the projection data is defined as the ratio of the mean pixel value to the standard deviation, i.e. N/√N = √N and it is equivalent to the square root of NEC counts for a fixed acquisition time Δt (SNR2 data equiv. to NEC = NECR × Δt) [10,11,43]. A recent study investigated the relationship between NEC and SNR2 in an experimental phantom set-up as well as in clinical PET scans and found satisfactory correlation between the two metrics in all phantom cases while, in the clinical cases, high correlation was observed for low and moderate body mass index (BMI) indices (< 28 kg/m2). The authors note that further studies are required to determine this relationship for patients of higher BMI indices [44].
There are strong indications that NECR can be a suitable criterion for determining the optimal amount of administered dosage in a PET clinical study. Nevertheless, as explained above, NECR refers directly to the statistical quality (SNR2) of the projection data (sinogram) measurements only. Although the average quality of the reconstructed images is expected to increase with NECR for the same reconstruction algorithm, image regions of different level of counts may be affected differently. Moreover, each iteration of various reconstruction algorithms may exercise a different impact in the final quality of the images for the same set of projection data. Thus, despite the usefulness of the NECR in quantifying the statistical quality of PET projection data, its value as a metric of quality of the images is limited and depends on a large set of reconstruction parameters. Thus, NECR may not be a 100% reliable indicato when the target is quality of a specific image ROI, as the choice of a reconstruction algorithm may considerably affect IQ to an extent that cannot be predicted by NECR alone [14].
Noise-equivalent counting rate and injected dosage
The administration of amounts of activity below or above the recommended optimal dosage levels can be problematic for various reasons. Figure 2 presents the effect of within FOV activity distributions on true, scatter and random coincidence events. Very large amounts of administered dosage may degrade SNR in projection data and quality of images due to the relatively higher increase rate of random (Figure 2A) compared to true (Figure 2B) and scatter (Figure 2C) coincidences [45,46].
Figure 2.

Random (sub-figure A), true (sub-figure B) and scatter (sub-figure C) coincidences counts as a function of injected dosage activity for six patients (A, B,…, F) of different weights (legend of sub-figure A). Obtained with permission from Monte Carlo simulation of PET images for injection dose optimization/Jiri Boldys, Jiri Dvorak, Magdalena Skopalova and Otakar Belohlavek/ International Journal for Numerical Methods in Biomedical Engineering 2013; 29: 988-999. Copyright © 2012 John Wiley & Sons, Ltd [45].
This is attributed to the exponential relationship between randoms rate and activity, unlike true and scatter coincidence rates that are exhibiting an approximately linear dependence with activity. As a result, NECR will increase with dosage at low injected levels but then is expected to level-off or even drop as the dosage becomes moderate or very high, thus diminishing statistical quality [45]. On the downside, very small administered dosage levels may result in poor count statistics and inaccurate LOR positioning in the projection data thus degrading spatial resolution and contrast [18,46]. The count losses as a result of a very low NECR could be compensated by elongating the scan duration. However this is not always feasible in the clinic due to high patient throughput requirements and the increased likelihood for subject motion. As a result, reconstructed PET images produced from either high or low injected dosage levels are usually characterized by low statistical quality affecting their diagnostic, prognostic and quantitative value.
Therefore, the optimization of PET administered dosage by determining at least a proper range of dosage levels, for which NECR is sufficiently high, is vital in order to exploit the maximum counting rate capabilities of a scanner after accounting for the effects of all relevant factors in a clinical PET study. Subsequently, the minimum dosage level within that range can be selected to minimize radiation exposure to the patient and personnel according to ALARA principles.
Impact of patient body attenuating volume
The patient body size or, more precisely, the human tissue volume exhibiting non-negligible attenuation properties can considerably affect the detected number of counts [42]. In general and for the same attenuation values, the larger the volume of attenuating tissues of a patient, the larger the fraction of scatter and random coincidences and the lower the detection rate of true coincidences [13]. Between patients of similar age groups, adipose or fat tissues are the most variant [14,40,45]. The impact of patient attenuating volume on the various coincidence count rate types and to NECR may, in turn, propagate to IQ metrics through the image reconstruction process. For instance, the scatter and random coincidences increase the background noise of the image thus diminish ing reliability in diagnosis of small and low-contrast lesions [47]. Therefore, the relationship between NECR and administered dosage and the optimal dosage is expected to vary for different patients or scanners [3,42].
Ideally, the effect of body attenuation on NECR-dosage relationship should be studied with respect to the actual three-dimensional (3D) body attenuating tissue distribution. However, for the purposes of NECR model-based dosage optimization, that approach would introduce unnecessary complexity, as the main attribute affecting NECR is the total volume and not the distribution of the 3D attenuating human tissues. Therefore, most relevant NECR studies approximately described the body attenuation properties with a single, yet sufficient for their purpose, indices such as the weight, body mass index (BMI) or height [14,44,48].
In the past, a number of phantoms as well as clinical studies had investigated the effect of different attenuating volume sizes on the number and type of coincidences detected [3,45]. A common and rather obvious observation of these studies is that true coincidence rates are often higher in small phantom sizes compared to larger ones due to the relative smaller attenuation volume of the former [3]. Patient studies have also confirmed that the size of patients may influence the composition of detected coincidences in trues, scatter and randoms and hence NECR. An example is shown by Accorsi et al. where the increasing patient weight diminishes measured NECR [42]. This example also demonstrates the usefulness of body attenuating volume size as a criterion to optimize injected dosage. Indeed, the different attenuation properties between patients have triggered considerable variability on observed NECRD- dosage curves [42]. Overall, it has been found that NECR and NECRD are reduced almost linearly with patient weight [10]. The graphs also demonstrate that the injection of higher dosage does not significantly affect NECR with respect to its highest peak, while it may lead to detection of less NEC events, due to the increase of randoms fraction and the frequent occurrence of dead-time effects [42], thus, degrading resolution in the final images [14,40]. In fact, Watson et al. suggested a feasible dosage reduction scheme, which also retained NECR at acceptable levels, providing that scan duration is increased. Furthermore, for a fixed scan time, it was shown that the NECR can be reduced by a factor of 0.44 and the mean SNR by a factor of 0.66 for a 120 kg patient compared to a 60 kg patient [10]. Therefore, in order to retain for 120 kg patients a similarly high NECR and IQ level as for 60 kg patients, it has been recommended to extend acquisition times by at least 2.3 times more for 120 kg patients. On the contrary, the alternative remedy of increasing the administered dosage for large or obese patients is not promoted, because it may lead to significant deterioration of NECR and IQ while unnecessarily increasing radiation dose exposure to patient and staff [43,44].
Moreover, as shown by Figure 4A, NECRD is no longer proportional to injected dosage after it reaches its highest peak, due to a) the significant increase of random events and b) the non-negligible losses of trues as a result of dead-time effects at higher dosage levels [42]. Therefore, it has been suggested to select the minimum from all dosages corresponding to at least 90-95% of peak NECRD. Since the expected NECR gain beyond 90-95% of peak NECR is negligible (5-10%) compared to the nearly 100% increase of dosage required to achieve that gain, it is not recommended to introduce any additional amount of dosage. However, such a strategy would induce a large variability in NECR performance among different patient scans, as NECR is significantly affected by a number of patients and scanner factors including human body attenuation and electronics dead-time response. Therefore, an alternative strategy could target the regulation of dosage such that a relatively constant NECR score is achieved for all patient scans. For instance, the maximum expected NECR for the most obese patients could be selected as the optimization criterion. As this NECR level will likely be relatively low, a prolongation of the PET scan is highly recommended to compensate for the NEC losses.
Figure 4.
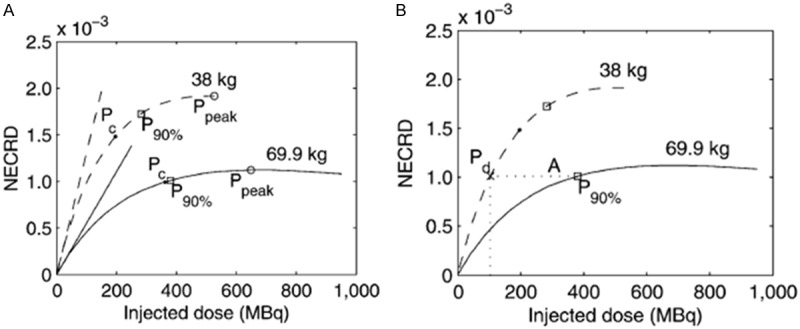
A. NECRD curves of two patients 69.9 kg and 38 kg each. B. Smaller or slimmer patients can achieve similar NECRD scores with larger or obese patients but at significantly smaller injected dosage. In addition, the increase of scan duration, whenever clinical protocols permit, allows for detection of more NECs for a given NECRD, thus providing, at lower administered dosage, similar IQ to the case of a higher administered dose but shorter scan duration. Ppeak = maximum NECRD, P90% = 90% peak NECRD, Pc = protocol based injected dose, Pd = dose that should be injected to a lighter patient to result in same NECRD as that of P90% for a heavier patient. This research was originally published in JNM. Accorsi R., Karp JS, and Surti S. Improved dose regimen in pediatric PET. J Nucl Med. 2010; 51(2): 293-300. Figure 1. © by the Society of Nuclear Medicine and Molecular Imaging, Inc. [42].
Furthermore, pediatric PET studies have suggested decreasing dosage levels and, at the same time, prolonging the scan duration for children (~38 kg) patients relative to adult (~69.9 kg) patients, such that the total NEC count levels between pediatric and adult patient populations are matched in the end, but with significant less dosage for the former [42]. In fact, the two PET acquisition strategies above could also be combined for the case of pediatric patients to deliver similar quality of acquired pediatric PET data, with that of adult patients at even lower dosage levels than each of the two methods above. This could be realized by simultaneously considering a) adult-equivalent acquisition times for pediatric scans together with b) 90-95% peak NECR dosage for each individual pediatric PET exam.
Following a NECR maximization scheme, Carlier et al. showed that the moderate levels of injected dosage are systematically exceeded [44]. In fact, they suggested setting the target NEC value to 75% of peak NECR in order to administer lower dosage to patients [44]. However, in the case of obese patients, such strategy resulted in very low NECR, therefore, they proposed increasing the acquisition time per bed position to enhance the total NECs recorded [44]. Their finding was in accordance with results and recommendations from other studies, such as Masuda et al. [49] and Karakatsanis et al. [13], thus confirming that injection of a higher dosage to obese patients may be unnecessary for the improvement of SNR in projection data. Alternatively, scan prolongation may help IQ in reconstructed images.
In addition, the results of three different phantom sizes (Figure 3) evaluating the impact of different possible degrees of human tissue attenuation on the projection data NECR and the optimized dosage are presented in Figure 6B [13]. It is illustrated that different bed positions and phantom sizes may considerably affect NECR-dosage response curve due to the variability of activity accumulation and degree of attenuation across the non-uniform human body parts. For instance, Karakatsanis et al. study employed Monte Carlo simulations to model two bed positions: the first positioned the heart in the center of the FOV, while the second placed the bladder in the center of the FOV with the two organs being associated with significantly different uptake and accumulation of the administered radiopharmaceutical as in real clinical scans [13]. Thus, the authors demonstrated the importance of incorporating a good approximation of the spatial distribution of the attenuating volume prior to each scan, for example based on the scan topogram or ideally the CT image, if available, in order to more accurately plan the optimal administered dosage. An example of a family of digital voxelized human torso phantoms of different sizes employed to evaluate the effect of attenuation distribution in a dosage optimization strategy is shown in Figure 6B [13].
Figure 3.
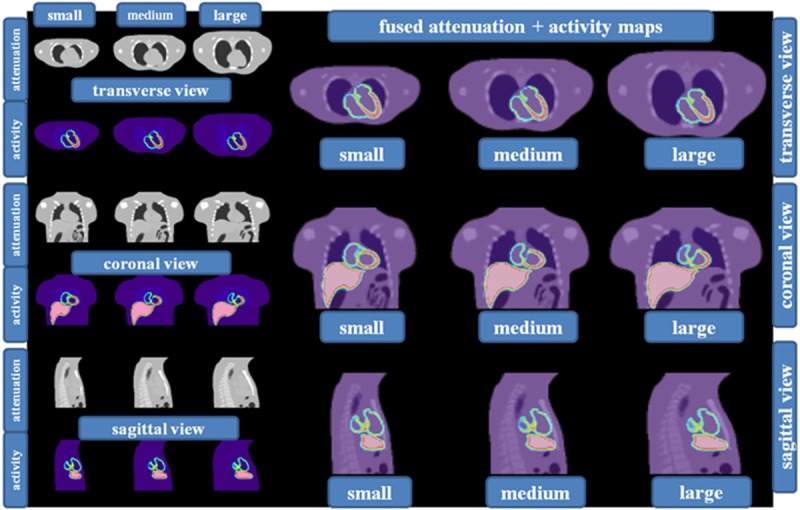
Three different phantom sizes versus the effect of body attenuation on the NECR and optimized dosage administration. Small, medium and large phantoms with three different views show the variability in attenuation and activity distribution across two different bed positions. Bed position one: heart at the center of the FOV and Bed position two: bladder at the center of the FOV. Obtained with permission from Karakatsanis et al. Monte-Carlo based characterization of the counting rate (NECR) response for personalized optimization of the administered activity in clinical PET imaging. Frontiers in Biomedical Technologies 2014; (1) 1 14-34. Copyright © Journal of Frontiers in Biomedical Technologies [13].
Figure 6.
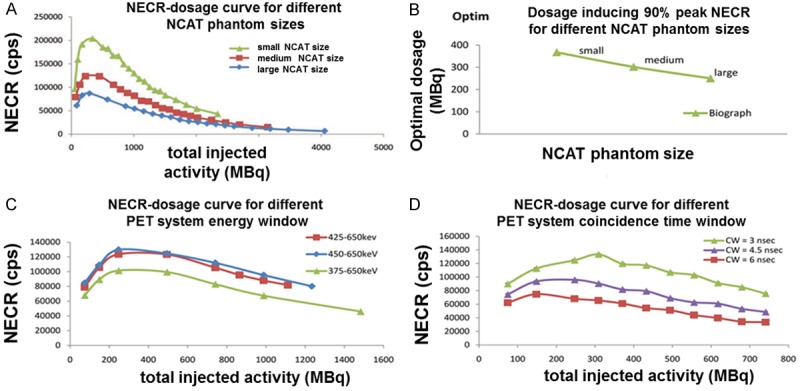
NECR-dosage curves vs. different patient- or system- specific factors (phantom size, energy window, coincidence time window). (A) NECR-dosage curve as a function of NCAT phantom size class, (B) injected activity, such that max. NECR is triggered in (A), as a function of the size of the NCAT phantom, (C) NECR-dosage curve as a function of PET system energy window, (D) NECR-dosage curve as a function of PET system coincidence time window (CW). Obtained with permission from Karakatsanis et al. Monte-Carlo based characterization of the counting rate (NECR) response for personalized optimization of the administered activity in clinical PET imaging. Frontiers in Biomedical Technologies 2014; (1) 1 14-34. Copyright © Journal of Frontiers in Biomedical Technologies [13].
Notably, although the optimal injected dosage would have been expected to increase with weight, as other studies have recommended [42,48], the results of this study, in fact, suggest a slight decrease for the optimal injected dosage. This is attributed to the applied criterion of NECR maximization for determining dosage, as NECR-dosage curves begin dropping at smaller dosage levels with larger attenuating volumes due to the relative smaller reduction of scatter and randoms counts, compared to the trues (Figure 2). However, in this case, the optimal dosage would result in significantly smaller NECR levels for obese compared to slim patients.
Therefore, for tasks where the NECR equivalency along a patient population is important, we would instead recommend optimizing dosage such that the same NECR is achieved among all patients regardless of their attenuation properties. In such a scheme, the recommended dosage is expected to be smaller for slim patients and larger for obese patients. In fact, this is confirmed by the results in Figure 4B after drawing a horizontal line at a particular NECR level and observing the dosage corresponding to the intersection points of the line with each of the NECR-dosage curves for different patient weights. However, for such optimization scheme the recommended NECR level remains an open question. Based on the effect of attenuation on NECR-dosage relationship, we recommend using the maximum NECR score achieved for the most obese member of a representative patient population. Our suggestion derives from the fact that scans of the most obese patients cannot achieve high NECRs, regardless of the injected dosage, and thus cannot be included in such dosage regimen schemes if higher NECR levels are selected as the optimization criterion.
For larger or obese patients the higher photon attenuation caused by the additional volume of adipose or fat tissue can negatively impact the fraction of true coincidence rates. Thus for this class of patients, further prolongation of scan time at moderate dosage levels could result in higher number of NECs and potentially higher IQ scores than scans of moderate duration but higher dosage amounts. Effectively, the increase of scan time, whenever the minimum patient throughput clinical requirements permit, can act as a scaling factor in the NEC-dosage relationship without influencing NECR curve shape. As a result, it may enable a more efficient management of dosage reduction while, retaining NECRD at acceptable levels [14,42]. Therefore, for simultaneous PET/MR protocols, where MR lengthy acquisitions allow for similarly elongated PET scans, the aforementioned optimization criterion may involve further lower NECR scores, compared to standard PET/CT protocols. The lower NECR performance can be effectively compensated by the longer acquisitions such that the total number of acquired NECs is sufficient.
Regarding the effect of attenuating tissue volume on scatter events, according to Figure 2C, scatter events are higher in absolute numbers for slim patient models in all examined activity levels, compared to obese patients [45]. Despite scattering volume being smaller in size in slimmer patients, the absolute number of scatter events can be higher [45], mainly because they are considerably less attenuated than in the case of obese patients. Nevertheless, the scatter fraction is expected to be less for slimmer patients as the number of true events reduces to a much greater extent, compared to scatter events, with increasing patient weight (Figure 2B and 2C).
Nowadays, dosage is administered linearly with patient weight based on the European Association of Nuclear Medicine (EANM) guidelines [45]. However, these recommended dosage levels do not necessarily correspond to equivalently optimal NECR or IQ scores, as discussed above. As a result, patients may receive higher than optimal or necessary amounts of dosage. Therefore, it is important to optimize dosage administration of each individual patient scan, i.e. after accounting for particular patient- and scanner-related factors, such that a nearly maximum NECR (90-95% of peak NECR) or sufficient but uniform NECR score across the population is achieved for the lowest possible dosage, according to ALARA principles [45].
NECR-dosage curves have been observed to first reach a global maximum (peak) at a moderate dosage level followed by a plateau over a relatively wide range of moderate to high administered dosage levels [42]. Chang et al. investigated the effect of three different BMI groups on measured PET NECR performance [14]. As illustrated in Figure 5, the authors demonstrated that NECR is indeed affected by the levels of administered dosage but not to a significant degree [14]. More specifically, they showed that increasing administered dosage by 100% can be associated with reduced image noise by only 12%. Therefore, they conjectured that administered dosage can be reduced from more than 555 MBq to the range of 296-444 MBq to drastically limit radiation exposure without significant degradation of the projection data SNR. For instance, dosage reduction to 370 MBq from 529 MBq limited the effective dose to approximately 5 mSv.
Figure 5.
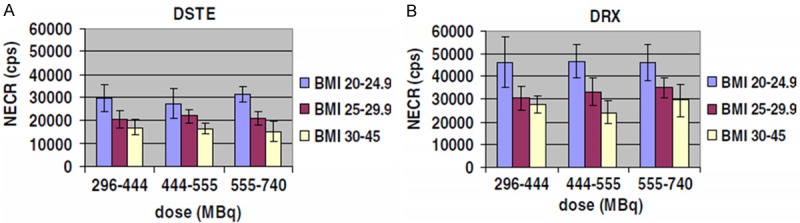
NECR measurements in different patient BMI groups and three different administered dosage levels for two types of GE PET scanners: (A) DSTE (BGO) and (B) DRX (LYSO). NECR does not change significantly with increasing dose. The improved scintillation crystal (LYSO) properties resulted in NECR and IQ enhancements. Chang T., Chang G., Kohlmyer S., Clark Jr. JW, Rohren E., and Mawlawi OR. Effects of injected dose, BMI and scanner type on NECR and image noise in PET imaging. Phys Med Biol 2011; 56: 5275-5285, Published 26 July 2011 © Institute of Physics and Engineering in Medicine. Reproduced by permission of IOP Publishing. All rights reserved. doi:10.1088/0031-9155/56/16/013 [14].
Furthermore Carlier et al. performed a systematic dosage optimization study based on both phantom as well as clinical NECR evaluations over a large patient population [44]. They utilized two dose regimens, a) 3 MBq/kg and b) 90% of NECR, to determine optimal dosage. In the second case they used two NECR-based optimization criteria and they finally extracted NECR-dosage curves for multiple bed positions demonstrating the usefulness and clinical feasibility of their method for retrospective optimization of dosage on completed clinical PET scans and for patients with BMI less than 28 kg/m2. Consequently, the study did not focus on prospective optimization of dosage in individual PET scans and it would be useful to expand its application for a larger group of patients, including obese cases with BMI larger than 28 kg/m2.
Noise-equivalent counting rate and energy window
The energy window of a PET scan is an important parameter as it can be utilized, if the system energy resolution permits, to efficiently discard a large fraction of scatter coincidences and thus maintain high NECR performance and sufficient SNR and IQ scores [3]. More specifically and for a given energy resolution which is constant for every PET scanner system the lower energy threshold (LET) of the window can be either: i) reduced to increase overall system sensitivity and limit statistical noise or ii) increased to limit scatter coincidence counts from contaminating the projection data and the final reconstructed PET images [3]. Overall widening the energy window enhances the sensitivity of a PET scanner, in terms of true coincidences count rate. However, very wide energy windows may be also associated with low NECs and NECR due to the higher acceptance ratio of scatter and randoms events enhancing their fraction [3]. Therefore a more balanced trade-off between sensitivity and resolution can be achieved by carefully adjusting the width of energy window with respect to its measured energy resolution. For instance, detailed Monte Carlo simulation studies have demonstrated that when LET increases from 375 keV to 450 keV the NECR was also increased due to the lower detection rate of primarily scattered events (Figure 6C) [3,13]. In addition, by lowering the upper energy threshold, detection of random events caused by event pile-up at high-count rates and thus LOR mispositioning could also be avoided. However, unlike NECR itself, the optimal dosage corresponding to 90% peak NECR appeared to be insensitive to such energy window width modifications [7]. Despite this, a careful adjustment of the energy window width would still be very appreciated as it could contribute to NECR enhancement and improved resolution thanks to more effective rejection of scatter and pile-up effects, the latter becoming more evident at high count rates [17,50]. Alternatively, potentially better energy resolutions of future PET systems supporting narrower energy windows could also be utilized to further reduce dosage for the same NECR levels as those of current PET systems with moderate energy resolution, thus demonstrating the potential of energy window in future dosage optimization strategies.
Moreover, coincidence time window (CTW) and the associated temporal resolution of a PET scanner detector system could be another important parameter affecting NECR and optimal dosage. CTW is defined as the minimum time required to reliably detect two single events in coincidence, given the temporal resolution of a PET scanner. For example, Karakatsanis et al. showed that the shorter CTW a PET system can support, according to the intrinsic limitations of detector system’s finite temporal resolution, the less random events are detected and therefore, the higher NECR can be achieved (Figure 6D) [13]. A short CTW or equivalently a superior temporal resolution could therefore constitute an important benefit in terms of dosage optimization and NECR performance as it could allow the effective limitation of random contamination in future PET systems of superior temporal resolution.
Parameters that improve signal-to-noise ratio
Noise-equivalent counting rate, positron emission tomography electronics and scintillation crystal types
PET scanner electronics high counting performance is vital for the efficient detection of coincidences events. Two important performance characteristics of a scanner electronics coincidences acquisition system are temporal and energy resolution [9,10,51]. The energy resolution enables the application of narrower energy windows with many benefits as described above. In addition, a high temporal resolution allows the use of a relatively short time coincidence window to further reduce the detection rate of random coincidences compared to older generation and thus, slower electronics [9,10]. This effect is attributed to the observation that random coincidence events tend to be associated with larger time differences between the arrival times of the two gamma photons that triggered them [18,51]. For example, Watson et al. showed for a 130 kg patient, that the SNR increases by 37% in new generation faster Pico-3D electronics compared to older generation non-Pico counting systems [10]. The improvement of electronics and particularly of their temporal response can result in significantly higher NECRs and therefore better IQ thus, leading to lower optimal administered dosage levels.
The scintillation crystal properties can play also an important role in determining NECR and optimal dosage as they may considerably impact the detection rates of random and scatter coincidences. In particular, the higher light output yield is responsible for the conversion efficiencyof the deposited energy of incident gamma photons to light photons in the crystal [39]. For instance, the cerium-doped rare-earth Lutetium-Yttrium Oxyorthosilicate (LYSO) crystal is characterized by more efficient and faster conversion to light output than Bismuth Germanate Oxyorthosilicate (BGO) crystal [39]. This attribute results in the production of better-resolved and clearer signal pulses and therefore in more accurate and precise energy measurements thus enhancing energy resolution and allowing for narrower energy windows [11]. A comparison of BGO and LYSO crystal performances confirmed that various scintillation properties may influence the detection of counts differently [14]. Thus, it has been found that the higher light output yield and faster light decay time of LYSO also allow for higher count rates and therefore, higher peak of NECR by 57% in comparison to BGO [14]. Overall, the utilization of scintillation crystals with efficient and fast light production properties allows for the detection of more counts in a given amount of scan time. This can lead to further reduction of optimal dosage, by widening the optimization gain margins due to the improvement of the limiting trade-off between competing system acquisition factors, such as CTW width and trues sensitivity.
Reconstructions enhanced with time-of-flightand resolution modeling features
The introduction of time-of-flight (TOF), a technology that utilizes very high temporal resolution of modern clinical PET scanners at the single events level to more precisely localize coincidence events along each LOR, can efficiently limit noise propagation and other resolution degradation effects in the resulted image [52,53] thus, enhancing SNR and image resolution, and consecutively further reducing the optimal administered dosage to patients [54]. The improved detection technology requires scintillation crystals with higher energy and temporal resolution to more accurately reject contaminating coincidence events, such as randoms or motion-translated events, as well as to reduce the uncertainty in locating the spatial position of a coincidence event across its LOR [53]. In fact, the recent advent of clinical PET scanners with faster temporal resolution (in the range of 400 ps), further improves the localization of events [55]. Furthermore, TOF is especially useful in cases of obese patients because the amount of adipose tissue is correlated with relatively high fractions of random and scatter events or low total number of counts, conditions in which TOF scanners have demonstrated significant benefits [54].
The use of different image reconstruction algorithms with TOF can determine the levels of contrast and noise in PET images. In Jakoby et al., it was shown that the use of 3D OP-OSEM (ordinary Poisson ordered-subset-expectationmaximization) algorithm, with point spread function (PSF) resolution response modeling and TOF capabilities enabled contrast improvement, noise reduction and consequently considerable enhancement of the SNR and resolution in the final images. These improvements are more apparent in regions of low activityin both 83 kg and 61 kg patients. For instance, the 83 kg patient image was characterized by an enhancement in SNR by a factor of 1.7, an increase of contrast by 19% and a reduction in noise by 22% [53]. The improvement was more obvious in obese than slim patients. These observations can be supported by the following equation [55]:
SNRTOF = √(D/Δx) × SNRnon-TOF
where D is the effective diameter of the patient and Δx is the corresponding spatial uncertainty. This equation shows that SNRTOF improves with obese patients and better temporal resolutions. The benefits of TOF and PSF OP-OSEM reconstruction algorithms in the IQ scores when applied on low-count projection data has been also recently demonstrated in whole-body dynamic and parametric PET clinical studies [56] where the acquisition protocol demands for faster scans per bed with limited count statistics and robust graphical analysis methods applied after [57-59] or within the tomographic reconstruction process [60,61].The significant enhancement in the SNR of the reconstructed images, due to the exploitation of TOF acquisition and PSF reconstruction may, therefore, allow for further reduction of the optimal dosage.
Disscusions
Fundamental limitations
As discussed above, the inherently stochastic process of positron emission inevitably results in the presence of statistical noise in the acquired projection data and finally the reconstructed PET images [10]. According to the properties of the Poisson distribution present in the projection data, the SNR of PET raw measurements is expected to be equal to the square root of the number of detected NECs thus, demonstrating the direct relationship between NEC, NECR and SNR. The uncertaintyin detecting the NEC coincidence counts depends on several factors such as patient attenuation properties, energy window, and PET electronics performance. As Cherry et al. has stated: “Large numbers of counts have smaller percentage uncertainties and are statistically more reliable than small number of counts” [9]. In fact, increasing the total number of detected NECs or increasing the detection rate of NECs, when scan time is limited, as it is always the case in the clinic, remain until today a very important performance target for clinical PET systems and their associated scan protocols. A high NECR will ensure sufficient statistical quality in PET measurements for a limited acquisition period, allowing at the same time administration of safe amounts of radioactivity. Therefore, the noise levels in the acquired measurements constitute a non-negligible limitation for dose optimization methods. In addition, when the imaging protocol involves short time frames, as in the case of dynamic single- or particularly multi-bed acquisitions, the count levels are expected to be substantially low amplifying the noise and reducing the SNR in the projection data [62]. In this case, the NECR may not be a reliable indicator for the IQ of the respective PET images, as different image reconstruction algorithms may exhibit substantially variable performance at low count conditions. Two recent studies proposed appropriate regularization schemes to more effectively limit the observed bias and noise compared to simple post-smoothing methods [63,64].
The human body can be characterized, from a gamma radiation point of view, as an absorber and scatterer, significantly affecting the number of NECs and hence, the overall quality of PET measurements. In this review, a series of patient or phantom experimental and simulation studies have been presented that systematically studied the effect of human body attenuation on NECs. The degree of attenuation from different possible sizes of the human body is a very important parameter to study as it can dramatically affect the performance of the scanner, perhaps more than any other system-related factor while it also impacts radiation dose absorption. For instance, Karakatsanis et al. showed that a large cylindrical phantom, approximating the human torso of an obese patient significantly reduced the NEC peak, compared to a smaller phantom representing the torso size of a slim patient for the same total activity in the FOV [3,50]. This is due to the photoelectric absorption, within the human body, or scattering, away of the scanner FOV, of the emitted gamma photons before reaching the PET system detectors and is generally termed as “radiation attenuation” [9]. As the patient size increases there is a higher probability of γ-rays to be absorbed or scattered within the larger attenuating medium, diminishing NECR performance, and thus attenuation can be a serious limiting factor when optimizing dosage. A number of studies presented in previous sections have suggested as the best remedy the prolongation of scan time for large or obese patients, if clinical protocol permits, to allow for detection of more NECs and enhance contrast-to-noise ratio (CNR) alleviating the need for increased administered dosage [13,65,66]. Also, it has been recommended to inject the minimum possible dosage corresponding to 90-95% as opposed to 100% of NECR peak, as NECR-dosage curves have been observed to exhibit a plateau for a relatively wide range of moderate dosage levels [13,42]. Overall, reduced dosage when combined with sufficiently longer but clinically acceptable scan durations could eliminate dead-time effects, retain high percentage of trues fractionand thus, ensure sufficient NECs in the measurements and potentially high IQ scores in the reconstructed images.
Moreover, one limitation that may affect the translation of the findings of a NECR-based injected dosage optimization PET study from simulations and phantoms to real human studies is the validity of extrapolating models and associated conclusions to human cases, as errors may be introduced due to the differences in habitus [14]. The phantom [42] and patient [14] examples given above are similar but not the same. This is due to the inter-patient differences in anatomy and physiology that could affect patient radiotracer distribution and which cannot be easily accounted for in simulations or experiments [27]. In addition, the pharmacokinetics (uptake, delivery, metabolism, clearance, and excretion rates) of each radiopharmaceutical can be quite different even among subsequent PET scans of the same patient performed only a few days apart [9]. The inevitable statistical fluctuations in PET measurements and consequently in NECR performance assessments can be expressed as random errors and they are expected to affect reproducibility in radiation imaging [9].
Non-fundamental limitations
Several PET imaging study parameters such as patient size, scanner type and scan protocol should be accounted for when regulating the administered dosage to achieve maximal NECR while avoiding unnecessary exposure to ionizing radiation. The administration of a very small or large dosage may result in the detection of either insufficiently true coincidence counts or excessive contamination by randoms and inefficient utilization of available PET radiotracer and scanner resources.
The choice of radiopharmaceutical is critical when determining the associated radiation exposure to adults and children. First, radiation dose increases with activity concentration and the effective physical and biological half-life of the administered radiotracer [67]. Second, the deposited dose from the emitted radiotracer depends on the energy of the emitted particle [67]. Third, dose deposition can be affected by tissue absorption characteristics, the shape, size and distance between organs and metabolism [68]. Xie et al., has shown that in small organs the energy deposition is lower compared to larger organs as the travel distance of positrons and photons through the smaller tissues is shorter [68].
Technical limitations
The choice of energy window is important as it allows the acceptance or rejection of coincidences according to their measured energy. The efficiency of this energy-based count rejection lies primarily to the ability of the system to resolve between two distinct energy levels, as quantified by the performance metric of the scanner energy resolution. Furthermore, the random-to-true events ratio can be reduced by choosing a suitable coincidence time windowwhich is, in turn, determined by the temporal resolution of the PET scanner [9]. In this context, the selection of the PET radiopharmaceutical can be critical as its energy distribution [9]may be associated with different probabilities of physical interaction undergoing between photon and attenuating medium before detection [69].
Another technical limitation in conventional PET data acquisition and subsequent image reconstruction is the non-precise localization of coincidence events within each LOR. Although a true coincidence event implies that the defined LOR includes the actual annihilation point, it is inherently not possible to precisely localize the exact position of the annihilation point along the LOR without additional knowledge of the arrival times of the two gamma photons involved. However, the development of TOF acquisition helps to significantly overcome this limitation. TOF technology utilizes the superior temporal resolution capabilities of modern PET detector systems to approximately estimate the difference in the time of flight of the two coincident gamma photons and thus considerably limit the uncertainty in the position of the annihilation point along each LOR [70]. As a result, PET images reconstructed from projection data with TOF information have higher SNR and superior resolution [53,71]. The SNR is considerably improved because the location uncertainty is now limited to a smaller section of the LOR which is determined by the inherenttemporal resolution of the detector pair [55]. The support and exploitation of TOF technology directly translates to the gain of significant optimization margins for further dosage reduction, as it decisively helps more precisely locate true annihilations positions and thus substantially reduces tomographic propagation of inaccuracies caused by random and scatter coincidences or any other PET resolution degrading factors such as subject motion, erroneous MR-based attenuation correction and partial volume effects [55].
Future developments
The development of novel hybrid PET scanners can improve diagnosis in many clinical applications by efficiently utilizing the additional information from complementary imaging modalities while optimizing dosage for each individual case. For instance, the emerging hybrid PET/MR imaging technology can improve, over currently established PET/CT scanners, the reliability in disease staging and prognosis as MR provides superior soft tissue contrast with respect to CT and also, does not involve any type of radiation, thus significantly reducing total effective radiation exposure by at least 50% compared to CT [72,73]. In addition, as MR usually requires considerable scan time to acquire the necessary multi-parametric information, simultaneous PET/MR protocols can now utilize the available extra time to accommodate relatively longer PET acquisitions of high statistical quality but with reduced injected dosage levels. In addition dosage optimization could benefit from the advent of various state-of-the-art technological advancements. For example, a PET scan with depth-of-interaction detectors and laser segmented LYSO could correct for patient movements precisely [74]. This innovation could provide in future better IQ, efficient reduction of dosage and support for longer but less sensitive to motion acquisitions.
In order to perform full body PET, multiple consecutive 3D images at different bed positions are acquired. A new project proposes the development of a body PET scanner that will cover the entire human body at once [75]. This scanner will have remarkably high sensitivity [76], e.g. 40-fold higher than current scanners, which may result in very low radiation dose from the PET scan (e.g. 150 μSv). This could have huge implications for the justification of imaging humans even at healthy conditions or at prenatal phase [77]. In addition to the scanner development, appropriate image reconstruction techniques are extended to process the large amount of data and produce the highest quality images possible [78]. This promising methodology is expected to enable imaging at ultra-low radioactivity dosage.
Conclusions
The optimization of the amount of administered radiotracer dosage in PET for each individual PET scan can be very important for the satisfaction of the ALARA safety recommendations as well as for the cost- and time-efficient utilization of the available resources in clinical PET centers. For that purpose, a validated NECR-dosage response model can be initially designed after the systematic assessment of the effect on measured NECR-dosage curves of a range of patient- and scanner-related factors commonly present in the clinical routine, including patient attenuation volume and physiological status, scanner energy and coincidences time windows and the applied image reconstruction algorithm. This optimization strategy can be repeated for a number of state-of-the-art clinical PET systems available today or projected for the future, according to the current technology trends. Then the NECR-dosage model can be utilized to predict prior to every individual PET scan a range of dosage amounts corresponding to at least 90% peak NECR scores for the particular patient and scanner characteristics involved in the clinical exam. Finally, recognizing the importance of the ALARA principles, the minimum dosage from the predicted range can actually be administered to the patient. However, although this approach may result in high NECR scores for the slimmer patients, it generally causes a large variation in the NECR performance over a population of patient scans, which may not facilitate its clinical translation.
Alternatively, we propose utilizing the same NECR-dosage response model but using a constant NECR score as an optimization criterion, which could be determined from the maximum expected NECR for the most obese patients of a representative population. Therefore, the dosage can now be regulated such that this NECR score is achieved in every scan. In that case, the NEC losses expected from the possibly low NECR performance can be compensated by accordingly elongating the PET scan duration as much as the clinical scan protocol permits. This could be applicable to some extent for PET/CT scans, but more practically for simultaneous PET/MR scans, where lengthy PET acquisitions can be affordable due to the long total acquisition time of multiple MR applied sequences (30-50 min). Thus, a considerable reduction of the injected dosage can be achieved, especially for slimmer or pediatric patients, while still acquiring measurements of sufficient statistical quality and SNR, as quantified by NECR.
Although currently established dosage regimen schemes in the clinic lead to recommend dosages significantly lower than the average annually absorbed radiation dose, many studies currently acknowledge that additional care should be exercised when optimizing the administered dosage for pediatric or pregnant patients, due to the increased radio-sensitivity of children tissues and the fetus respectively. Furthermore, cardiovascular, brain and pediatric PET/MR imaging can be promising for the assessment of early strategies of disease and thus a very low PET dosage could enable its routine and wide application over a group of population associated with a higher risk profile. In all these cases, a smaller percentage of peak NECR or smaller fixed NECR could be targeted with a proper prolongation of scan time to compensate for the NEC losses. Naturally, in that case motion compensation becomes very important [79]. Finally, as the scanner count rate performance and reconstruction algorithms are continuously improving, the dosage optimization schemes should constantly adapt to efficiently exploit as much technological advancements as possible.
Acknowledgements
Dr Tsoumpas was recipient of the Research Mobility Award from the University of Leeds, which allowed him to complete this review article.
Disclosure of conflict of interest
None.
References
- 1.Nievelstein RA, Quarles van Ufford HM, Kwee TC, Bierings MB, Ludwig I, Beek FJ, de Klerk JM, Mali WP, de Bruin PW, Geleijns J. Radiation exposure and mortality risk from CT and PET imaging of patients with malignant lymphoma. Eur Radiol. 2012;22:1946–1954. doi: 10.1007/s00330-012-2447-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boellaard R, O’Doherty MJ, Weber WA, Mottaghy FM, Lonsdale MN, Stroobants SG, Oyen WJ, Kotzerke J, Hoekstra OS, Pruim J, Marsden PK, Tatsch K, Hoekstra CJ, Visser EP, Arends B, Verzijlbergen FJ, Zijlstra JM, Comans EF, Lammertsma AA, Paans AM, Willemsen AT, Beyer T, Bockisch A, Schaefer-Prokop C, Delbeke D, Baum RP, Chiti A, Krause BJ. FDG PET and PET/CT: EANM procedure guidelines for tumour PET imaging: version 1.0. Eur J Nucl Med Mol Imaging. 2010;37:181–200. doi: 10.1007/s00259-009-1297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karakatsanis NA, Parasyris A, Nikita KS, Loudos G. A simulation study for optimizing the injected dose of clinical PET systems. IEEE Inter Workshop Imaging Syst Tech. 2008 [Google Scholar]
- 4.Kapoor V, McCook BM, Torok FS. An introduction to PET-CT imaging. Radiographics. 2004;24:523–543. doi: 10.1148/rg.242025724. [DOI] [PubMed] [Google Scholar]
- 5.Schwaiger M, Ziegler S, Nekolla SG. PET/CT: challenge for nuclear cardiology. J Nucl Med. 2005;46:1664–1678. [PubMed] [Google Scholar]
- 6.Tai YF, Piccini P. Applications of positron emission tomography (PET) in neurology. J Neurol Neurosurg Psychiatry. 2004;75:669–676. doi: 10.1136/jnnp.2003.028175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Willowson KP, Bailey EA, Bailey DL. A retrospective evaluation of radiation dose associated with low dose FDG protocols in wholebody PET/CT. Australas Phys Eng Sci Med. 2012;35:49–53. doi: 10.1007/s13246-011-0119-8. [DOI] [PubMed] [Google Scholar]
- 8.Fahey FH. Dosimetry of Pediatric PET/CT. J Nucl Med. 2009;50:1483–1491. doi: 10.2967/jnumed.108.054130. [DOI] [PubMed] [Google Scholar]
- 9.Cherry SR, Sorenson JA, Phelps ME. Physics in nuclear medicine. Philadelphia: Elsevier/Saunders; 2012. [Google Scholar]
- 10.Watson CC, Casey ME, Bendriem B, Carney JP, Townsend DW, Eberl S, Meikle S, Difilippo FP. Optimizing injected dose in clinical PET by accurately modeling the counting-rate response functions specific to individual patient scans. J Nucl Med. 2005;46:1825–1834. [PubMed] [Google Scholar]
- 11.Saha GB. Basics of PET imaging: physics, chemistry, and regulations. New York: Springer; 2010. [Google Scholar]
- 12.Walker MD, Matthews JC, Asselin MC, Saleem A, Dickinson C, Charnley N, Julyan PJ, Price PM, Jones T. Optimization of the injected activity in dynamic 3D PET: a generalized approach using patient-specific NECs as demonstrated by a series of 15O-H2O scans. J Nucl Med. 2009;50:1409–1417. doi: 10.2967/jnumed.109.062679. [DOI] [PubMed] [Google Scholar]
- 13.Karakatsanis NA, Loudos G, Ragmim A, Nikita KS. Monte-carlo based characterization of the counting rate (NECR) response for personalized optimization of the administered activity in clinical PET imaging. Front Biomed Technol. 2014;1:14–34. [Google Scholar]
- 14.Chang T, Chang G, Kohlmyer S, Clark JW, Rohren E, Mawlawi OR. Effects of injected dose, BMI and scanner type on NECR and image noise in PET imaging. Phys Med Biol. 2011;56:5275–5285. doi: 10.1088/0031-9155/56/16/013. [DOI] [PubMed] [Google Scholar]
- 15.Devine CE, Mawlawi O. Radiation safety with positron emission tomography and computed tomography. Semin Ultrasound CT MR. 2010;31:39–45. doi: 10.1053/j.sult.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Zanzonico P. Positron emission tomography: a review of basic principles, scanner design and performance, and current systems. Semin Nucl Med. 2004;34:87–111. doi: 10.1053/j.semnuclmed.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Turkington TG. Introduction to PET instrumentation. J Nucl Med Technol. 2001;29:4–11. [PubMed] [Google Scholar]
- 18.Liang Y. Performance optimization of a PET insert for simultaneous breast PET/MR imaging. University of Waterloo. 2013 [Google Scholar]
- 19.Schmitz RE, Alessio AM, Kinahan PE, Mason NS, Lin EC. The physics of PET/Ct scanners. PET and PET/CT: a clinical guide. 2005:3. [Google Scholar]
- 20.IAEA. Quality assurance for PET and PET/CT systems. 2009. [Google Scholar]
- 21.Bailey DL. Positron emission tomography: basic sciences. London: Springer; 2005. [Google Scholar]
- 22.Silva-Rodriguez J, Aguiar P, Dominguez-Prado I, Fierro P, Ruibal A. Simulated FDG-PET studies for the assessment of SUV quantification methods. Rev Esp Med Nucl Imagen Mol. 2015;34:13–18. doi: 10.1016/j.remn.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 23.Thie JA. Understanding the standardized uptake value, its methods, and implications for usage. J Nucl Med. 2004;45:1431–1434. [PubMed] [Google Scholar]
- 24.Kinahan PE, Fletcher JW. Positron emission tomography-computed tomography standardized uptake values in clinical practice and assessing response to therapy. Semin Ultrasound CT MR. 2010;31:496–505. doi: 10.1053/j.sult.2010.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson DR, Kyriou J, Morton EJ, Clifton A, Fitzgerald M, Macsweeney E. Radiation protection in interventional radiology. Clin Radiol. 2001;56:99–106. doi: 10.1053/crad.2000.0640. [DOI] [PubMed] [Google Scholar]
- 26.Phelps ME. PET: the merging of biology and imaging into molecular imaging. J Nucl Med. 2000;41:661–681. [PubMed] [Google Scholar]
- 27.Fahey FH, Treves ST, Adelstein SJ. Minimizing and communicating radiation risk in pediatric nuclear medicine. J Nucl Med. 2011;52:1240–1251. doi: 10.2967/jnumed.109.069609. [DOI] [PubMed] [Google Scholar]
- 28.Anja K. Radiation dose and radiation risk to foetuses and newborns during X-ray examinations. University of Oulu. 2004 [Google Scholar]
- 29.Xie T, Zaidi H. Fetal and maternal absorbed dose estimates for positron-emitting molecular imaging probes. J Nucl Med. 2014;55:1459–1466. doi: 10.2967/jnumed.114.141309. [DOI] [PubMed] [Google Scholar]
- 30.Zanotti-Fregonara P, Champion C, Trebossen R, Maroy R, Devaux JY, Hindie E. Estimation of the beta+ dose to the embryo resulting from 18F-FDG administration during early pregnancy. J Nucl Med. 2008;49:679–682. doi: 10.2967/jnumed.107.048900. [DOI] [PubMed] [Google Scholar]
- 31.Goodman TR, Amurao M. Medical imaging radiation safety for the female patient: rationale and implementation. Radiographics. 2012;32:1829–1837. doi: 10.1148/rg.326125508. [DOI] [PubMed] [Google Scholar]
- 32.Alessio AM, Kinahan PE, Manchanda V, Ghioni V, Aldape L, Parisi MT. Weight-based, lowdose pediatric whole-body PET/CT protocols. J Nucl Med. 2009;50:1570–1577. doi: 10.2967/jnumed.109.065912. [DOI] [PubMed] [Google Scholar]
- 33.Eldib M, Bini J, Lairez O, Faul DD, Oesingmann N, Fayad ZA, Mani V. Feasibility of (18) F-Fluorodeoxyglucose radiotracer dose reduction in simultaneous carotid PET/MR imaging. Am J Nucl Med Mol Imaging. 2015;5:401–407. [PMC free article] [PubMed] [Google Scholar]
- 34.Voss SD, Reaman GH, Kaste SC, Slovis TL. The ALARA concept in pediatric oncology. Pediatr Radiol. 2009;39:1142–1146. doi: 10.1007/s00247-009-1404-5. [DOI] [PubMed] [Google Scholar]
- 35.Kaste SC. PET-CT in children: where is it appropriate? Pediatr Radiol. 2011;41(Suppl 2):509–513. doi: 10.1007/s00247-011-2096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Radiology info. Radiation dose in X-Ray and CT exams. 2013. [Google Scholar]
- 37.IAEA. 2013. Radiation in everyday life. [Google Scholar]
- 38.IAEA. Radiation, people and the environment. Austria: 2004. [Google Scholar]
- 39.Jadvar H, Parker JA. Clinical PET and PET/CT. London: Springer; 2005. [Google Scholar]
- 40.Chang T, Chang G, Kohlmyer S, Clark JW, Rohren E, Mawlawi OR. Effects of injected dose, BMI and scanner type on NECR and image noise in PET imaging. Phys Med Biol. 2011;56:5275–5285. doi: 10.1088/0031-9155/56/16/013. [DOI] [PubMed] [Google Scholar]
- 41.Saha GB. Physics and radiobiology of nuclear medicine. New York: Springer; 2006. [Google Scholar]
- 42.Accorsi R, Karp JS, Surti S. Improved dose regimen in pediatric PET. J Nucl Med. 2010;51:293–300. doi: 10.2967/jnumed.109.066332. [DOI] [PubMed] [Google Scholar]
- 43.Masuda Y, Kondo C, Matsuo Y, Uetani M, Kusakabe K. Comparison of imaging protocols for 18F-FDG PET/CT in overweight patients: optimizing scan duration versus administered dose. J Nucl Med. 2009;50:844–848. doi: 10.2967/jnumed.108.060590. [DOI] [PubMed] [Google Scholar]
- 44.Carlier T, Ferrer L, Necib H, Bodet-Milin C, Rousseau C, Kraeber-Bodere F. Clinical NECR in 18F-FDG PET scans: optimization of injected activity and variable acquisition time. Relationship with SNR. Phys Med Biol. 2014;59:6417–6430. doi: 10.1088/0031-9155/59/21/6417. [DOI] [PubMed] [Google Scholar]
- 45.Boldyš J, Dvořák J, Skopalová M, Bělohlávek O. Monte Carlo simulation of PET images for injection dose optimization. Int J Numer Method Biomed Eng. 2013;29:988–999. doi: 10.1002/cnm.2527. [DOI] [PubMed] [Google Scholar]
- 46.Inoue K, Kurosawa H, Tanaka T, Fukushi M, Moriyama N, Fujii H. Optimization of injection dose based on noise-equivalent count rate with use of an anthropomorphic pelvis phantom in three-dimensional 18F-FDG PET/CT. Radiol Phys Technol. 2012;5:115–122. doi: 10.1007/s12194-011-0144-z. [DOI] [PubMed] [Google Scholar]
- 47.Barrington SF, Wahl RL, Maisey M. Atlas of clinical positron emission tomography. London: Hodder Arnold; 2006. [Google Scholar]
- 48.Watson CC, Casey ME, Bendriem B, Carney JP, Townsend DW, Eberl S, Meikle S, Difilippo FP. Optimizing injected dose in clinical PET by accurately modeling the counting-rate response functions specific to individual patient scans. J Nucl Med. 2005;46:1825–1834. [PubMed] [Google Scholar]
- 49.Masuda Y, Kondo C, Matsuo Y, Uetani M, Kusakabe K. Comparison of imaging protocols for 18F-FDG PET/CT in overweight patients: Optimizing scan duration versus administered dose. J Nucl Med. 2009;50:844–848. doi: 10.2967/jnumed.108.060590. [DOI] [PubMed] [Google Scholar]
- 50.Karakatsanis NA, Parasyris A, Loudos G, Nikita KS. A simulation study of the countingrate performance of clinical PET systems applying a methodology for optimizing the injected dose. IEEE Nucl Sc Symp Med Imaging Conf. 2008:5014–5019. [Google Scholar]
- 51.Karakatsanis N, Nikita K. A simulation model of the counting-rate response of clinical PET systems and it's application to optimize the injected dose. 6th IEEE Inter Symp Biomed Imag: from Nano to Macro. 2009:398–401. [Google Scholar]
- 52.Small GR, Wells RG, Schindler T, Chow BJ, Ruddy TD. Advances in cardiac SPECT and PET imaging: overcoming the challenges to reduce radiation exposure and improve accuracy. Can J Cardiol. 2013;29:275–284. doi: 10.1016/j.cjca.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 53.Jakoby BW, Bercier Y, Conti M, Casey ME, Bendriem B, Townsend DW. Physical and clinical performance of the mCT time-of-flight PET/CT scanner. Phys Med Biol. 2011;56:2375–2389. doi: 10.1088/0031-9155/56/8/004. [DOI] [PubMed] [Google Scholar]
- 54.Murray I, Kalemis A, Glennon J, Hasan S, Quraishi S, Beyer T, Avril N. Time-of-flight PET/CT using low-activity protocols: potential implications for cancer therapy monitoring. Eur J Nucl Med Mol Imaging. 2010;37:1643–1653. doi: 10.1007/s00259-010-1466-5. [DOI] [PubMed] [Google Scholar]
- 55.Conti M. Focus on time-of-flight PET: the benefits of improved time resolution. Eur J Nucl Med Mol Imaging. 2011;38:1147–1157. doi: 10.1007/s00259-010-1711-y. [DOI] [PubMed] [Google Scholar]
- 56.Karakatsanis NA, Lodge MA, Rahmim A, Zaidi H. Introducing time-of-flight and resolution recovery image reconstruction to clinical whole-body PET parametric imaging. IEEE Nucl Sci Symp Med Imag Conf. 2014 [Google Scholar]
- 57.Karakatsanis NA, Lodge MA, Tahari AK, Zhou Y, Wahl RL, Rahmim A. Dynamic whole-body PET parametric imaging: I. Concept, acquisition protocol optimization and clinical application. Phys Med Biol. 2013;58:7391–7418. doi: 10.1088/0031-9155/58/20/7391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Karakatsanis NA, Lodge MA, Zhou Y, Wahl RL, Rahmim A. Dynamic whole-body PET parametric imaging: II. Task-oriented statistical estimation. Phys Med Biol. 2013;58:7419–7445. doi: 10.1088/0031-9155/58/20/7419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Karakatsanis N, Zhou Y, Lodge M, Casey ME, Wahl RL, Rahmim A. Quantitative wholebody parametric PET imaging incorporating a generalized Patlak model. IEEE IEEE Nucl Sc Symp Med Imaging Conf. 2013:1–9. [Google Scholar]
- 60.Karakatsanis N, Lodge M, Wahl R, Rahmim A. Direct 4D whole-body PET/CT parametric image reconstruction: concept and comparison vs. indirect parametric imaging. J Nucl Med. 2013;54:2133–2133. [Google Scholar]
- 61.Karakatsanis NA, Rahmim A. Whole-body PET parametric imaging employing direct 4D nested reconstruction and a generalized nonlinear Patlak model. SPIE Medical Imaging. 2014 Phys Med Imaging: 90330Y. [Google Scholar]
- 62.Karakatsanis NA, Lodge MA, Yun Z, Mhlanga J, Chaudhry MA, Tahari AK, Segars WP, Wahl RL, Rahmim A. Dynamic multi-bed FDG PET imaging: Feasibility and optimization. IEEE Nucl Sc Symp Med Imaging Conf. 2011:3863–3870. [Google Scholar]
- 63.Karaoglanis K, Polycarpou I, Efthimiou N, Tsoumpas C. Post filtering regularized OSEM can improve low count statistics of PET iterative reconstruction simulated data. Hell J Nucl Med. 2015;18:140–145. doi: 10.1967/s002449910209. [DOI] [PubMed] [Google Scholar]
- 64.Ahn S, Ross SG, Asma E, Miao J, Jin X, Cheng L, Wollenweber SD, Manjeshwar RM. Quantitative comparison of OSEM and penalized likelihood image reconstruction using relative difference penalties for clinical PET. Phys Med Biol. 2015;60:5733–5751. doi: 10.1088/0031-9155/60/15/5733. [DOI] [PubMed] [Google Scholar]
- 65.Hausmann D, Dinter DJ, Sadick M, Brade J, Schoenberg SO, Busing K. The impact of acquisition time on image quality in wholebody 18F-FDG PET/CT for cancer staging. J Nucl Med Technol. 2012;40:255–258. doi: 10.2967/jnmt.112.103291. [DOI] [PubMed] [Google Scholar]
- 66.Farquhar TH, Llacer J, Sayre J, Tai YC, Hoffman EJ. ROC and LROC analyses of the effects of lesion contrast, size, and signal-tonoise ratio on detectability in PET images. J Nucl Med. 2000;41:745–754. [PubMed] [Google Scholar]
- 67.Mejia AA, Nakamura T, Masatoshi I, Hatazawa J, Masaki M, Watanuki S. Estimation of absorbed doses in humans due to intravenous administration of fluorine-18-fluorodeoxyglucose in PET studies. J Nucl Med. 1991;32:699–706. [PubMed] [Google Scholar]
- 68.Xie T, Zaidi H. Monte Carlo-based evaluation of S-values in mouse models for positronemitting radionuclides. Phys Med Biol. 2013;58:169–182. doi: 10.1088/0031-9155/58/1/169. [DOI] [PubMed] [Google Scholar]
- 69.Badawi RD, Marsden PK, Cronin BF, Sutcliffe JL, Maisey MN. Optimization of noiseequivalent count rates in 3D PET. Phys Med Biol. 1996;41:1755–1776. doi: 10.1088/0031-9155/41/9/014. [DOI] [PubMed] [Google Scholar]
- 70.Conti M. State of the art and challenges of time-of-flight PET. Phys Med. 2009;25:1–11. doi: 10.1016/j.ejmp.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 71.Moses WW. Recent advances and future advances in time-of-flight PET. Nucl Instrum Methods Phys Res A. 2007;580:919–924. doi: 10.1016/j.nima.2007.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Catana C, Guimaraes AR, Rosen BR. PET and MR imaging: the odd couple or a match made in heaven? J Nucl Med. 2013;54:815–824. doi: 10.2967/jnumed.112.112771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Partovi S, Robbin MR, Steinbach OC, Kohan A, Rubbert C, Vercher-Conejero JL, Kolthammer JA, Faulhaber P, Paspulati RM, Ros PR. Initial experience of MR/PET in a clinical cancer center. J Magn Reson Imaging. 2014;39:768–80. doi: 10.1002/jmri.24334. [DOI] [PubMed] [Google Scholar]
- 74.Moriya T, Fukumitsu K, Sakai T, Ohsuka S, Okamoto T, Takahashi H, Watanabe M, Yamashita T. Development of PET detectors using monolithic scintillation crystals processed with sub-surface laser engraving technique. IEEE Trans Nucl Sc. 2010;57:2455–2459. [Google Scholar]
- 75.Cherry SR. The 2006 Henry N. Wagner Lecture: Of mice and men (and positrons)--advances in PET imaging technology. J Nucl Med. 2006;47:1735–1745. [PubMed] [Google Scholar]
- 76.Poon JK, Dahlbom ML, Moses WW, Balakrishnan K, Wang W, Cherry SR, Badawi RD. Optimal whole-body PET scanner configurations for different volumes of LSO scintillator: a simulation study. Phys Med Biol. 2012;57:4077–4094. doi: 10.1088/0031-9155/57/13/4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jones T, Budinger TF. The potential for lowdose functional studies in maternal-fetal medicine using PET/MR imaging. J Nucl Med. 2013;54:2016–2017. doi: 10.2967/jnumed.113.123919. [DOI] [PubMed] [Google Scholar]
- 78.Tsoumpas C, Brain C, Dyke T, Gold D. Incorporation of a two metre long PET scanner in STIR. J Phys: Conf Ser. 2015;637:012030. [Google Scholar]
- 79.Karakatsanis N, Tsoumpas C, Zaidi H. Generalized 3D and 4D motion compensated whole-body PET image reconstruction employing nested EM deconvolution. IEEE International Conf Imaging Syst Tech (IST) 2014:263–268. [Google Scholar]


