Description
A 21-year-old Japanese woman developed acute onset of persistent epigastric pain and nausea, and presented to the emergency department 12 h after the onset of symptoms. There was no significant medical history, nor was there allergy, significant family history, recent travel or trauma, and she had not undergone any particular change in eating habits. On examination, she was in acute distress; the blood pressure was 124/75 mm Hg, pulse 90 bpm, respiration 20 breaths/min and temperature 37.4°C. The abdomen was soft and flat, but with positive Mallet-Guy sign (tenderness of left upper quadrant palpation with the patient lying in a right lateral decubitus position). Peripheral white cell count was 1.5×1010/L. Renal and liver functions were normal. A diagnosis of acute pancreatitis was suspected and the patient was started on volume replacement and loxoprofen. However, serum lipase and amylase levels were normal and the CT of the abdomen revealed a high-density lesion behind the pancreas, within the retroperitoneal space (figure 1). On day 4, MR cholangiopancreatography showed an increased signal density of retroperitoneal fat (figure 2). A diagnosis of retroperitoneal panniculitis was considered. The abdominal pain gradually disappeared and white cell count returned to normal (7.8×109/L) on day 4. The patient was discharged on day 7. Although abdominal panniculitis is usually recognised in mesenteric fat tissue, few cases with retroperitoneal panniculitis have been previously reported.1 While causes of abdominal panniculitis may include infectious, neoplastic or autoimmune diseases,2 our case was considered to have an idiopathic cause because of the self-limited course.
Figure 1.
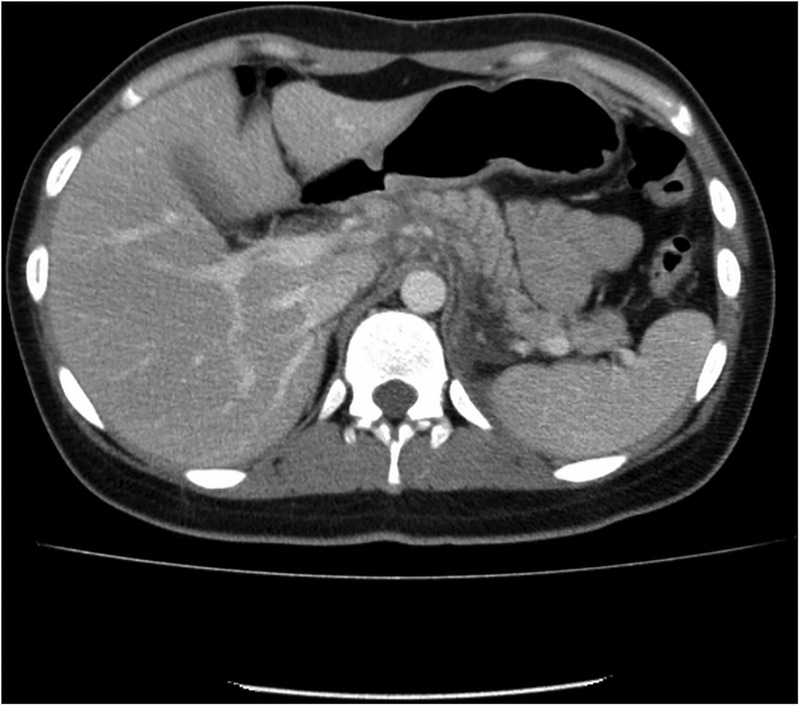
CT of the abdomen revealing a high-density lesion behind the pancreas, within the retroperitoneal space.
Figure 2.
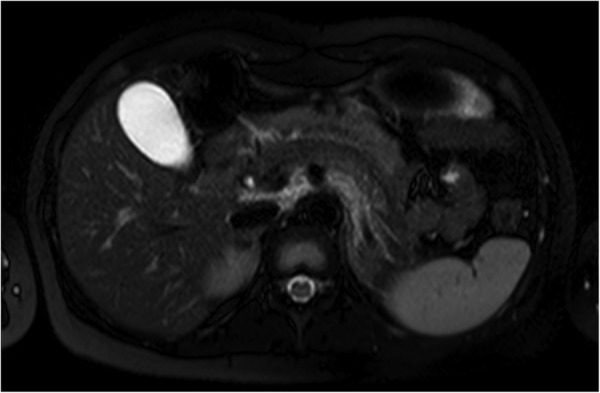
MR cholangiopancreatography showing abnormal signal density within retroperitoneal fat tissue.
Learning points.
Causes of acute abdominal pain with positive Mallet-Guy sign may include retroperitoneal panniculitis in addition to acute pancreatitis.
Abdominal panniculitis may involve not only mesenteric fat, but also retroperitoneal space.
Footnotes
Contributors: NT, TT and TF cared for the patient. NT and YT wrote the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.McCrystal DJ, O'Loughlin BS, Samaratunga H. Mesenteric panniculitis: a mimic of malignancy. Aust N Z J Surg 1998;68:237–9. doi:10.1111/j.1445-2197.1998.tb04754.x [DOI] [PubMed] [Google Scholar]
- 2.Issa I, Baydoun H. Mesenteric panniculitis: various presentations and treatment regimens. World J Gastroenterol 2009;15:3827–30. doi:10.3748/wjg.15.3827 [DOI] [PMC free article] [PubMed] [Google Scholar]


