Abstract
Objective
To identify current practice patterns for unresolved issues in the surgical and adjuvant management of endometrial cancer in Korea.
Methods
We designed and conducted a survey of all 218 active members of the Korean Gynecologic Oncology Group to try to identify how they would manage various case scenarios for endometrial cancer. Data were collected using an Internet survey database.
Results
A total of 108 members (49.5%) responded to the survey. Laparoscopy (81.6%) was the most commonly used mode of surgery in early-stage endometrial cancer. Of all the respondents, 19.8% stated that lymphadenectomy could be omitted and 21.7% recommended selective lymphadenectomy based on sentinel biopsy or frozen results for patients with presumed stage IA/grade 1 disease. On the other hand, 71.9% of respondents recommended para-aortic lymphadenectomy for patients with presumed stage IB/grade 1 disease and 86.4% recommended this treatment for presumed stage IB/grade 3 disease. The majority of respondents performed adjuvant therapy for stage IB/grade 2 (91.7%), IB/grade 3 (99.0%), and stage II (89.6%). Whole pelvic radiotherapy and vaginal brachytherapy were the most frequently used options among these patients. All respondents administered adjuvant therapy when node metastasis was found, and concurrent chemoradiotherapy (53.2%) was the most preferred option for stage IIIC1 disease.
Conclusion
There is broad variation in both the surgical and adjuvant treatment of endometrial cancer among Korean gynecologic oncologists.
Keywords: Adjuvant Therapy, Data Collection, Endometrial Neoplasms, Lymph Node Excision, Practice Pattern
INTRODUCTION
Endometrial cancer is the third most common gynecologic cancer, and its incidence and mortality are increasing in Korea, where more than 1,700 new cases are diagnosed and approximately 250 deaths occur every year from the disease [1,2]. The incidence rate increases every year by 6.9% and the mortality rate, by 6.7%. As such, the burden of this disease can be expected to increase in the near future.
The optimal management of endometrial cancer remains one of the most debated issues, with many differences and discrepancies among gynecologic oncologists. There is significant variability in the treatment algorithms used at different institutions and even among physicians within the same institution. Unresolved questions remain as to the value and extent of lymphadenectomy, the optimal adjuvant therapy for intermediate or high-risk endometrial cancer.
In 2009, the Korean Gynecologic Oncology Group (KGOG) conducted a survey to assess surgical practice patterns for endometrial cancer in Korea [3]. A previous survey by KGOG showed substantial differences in the surgical procedures used for the treatment of endometrial cancer between Korean gynecologic oncologists. Since then, there has been level I evidence from randomized controlled trials for surgical and adjuvant treatment in the field of endometrial cancer [4,5,6,7]. However, certain discrepancies still exist between the clinical guidelines and the actual practice adopted by clinicians. To identify current practice patterns in the surgical and adjuvant management of endometrial cancer in Korea, we conducted a survey of KGOG members.
MATERIALS AND METHODS
This survey was initiated by the Uterine Corpus Committee of the KGOG. In December 2014, we mailed the questionnaire to all 218 KGOG members. The last date for receipt of responses was set for February 13, 2015. The survey was estimated to take 10 minutes to complete and was submitted electronically. All data were stored automatically by the website SurveyMonkey (http://ko.surveymonkey.com), and all responses were anonymous. The respondents were asked about demographic characteristics, including their current practice settings and years since completing fellowship training. The respondents were asked 20 questions regarding surgical and adjuvant procedures for endometrial cancer. Each question referenced a detailed clinical scenario. The survey questions are provided in Supplementary Table 1.
The data were analyzed using frequency distributions and nonparametric tests. In the event of missing data, percentages were determined on the basis of the number of responses received.
RESULTS
1. Respondents' demographics
Table 1 shows the demographics of the survey respondents. Of the 218 KGOG members who received the survey questionnaire, 108 (49.5%) responded. Most were men (87%) and were aged 41 to 50 years (52.8%). Of the respondents, 92.6% had completed a fellowship and 7.4% were currently fellows. Almost half of the respondents (47%) completed their fellowship training more than 10 years ago.
Table 1. Respondents' demographics.
| Variable | No. (%) |
|---|---|
| Age (yr) | |
| 30-40 | 21 (19.4) |
| 41-50 | 57 (52.8) |
| 51-60 | 21 (19.4) |
| 61-70 | 9 (8.3) |
| >70 | 0 |
| Sex | |
| Male | 94 (87.0) |
| Female | 14 (13.0) |
| No. of years since fellowship training | |
| Currently in fellowship training | 8 (7.4) |
| Up to 5 years since completion | 22 (20.4) |
| 6-10 years since completion | 27 (25.0) |
| 11-15 years since completion | 20 (18.5) |
| >15 years since completion | 31 (28.7) |
| No. of endometrial cancer cases managed in your center (per year) | |
| ≤20 | 25 (23.1) |
| 21-40 | 30 (27.8) |
| 41-80 | 25 (23.1) |
| 81-100 | 11 (10.2) |
| 101-150 | 8 (7.4) |
| >150 | 9 (8.3) |
2. Surgical management
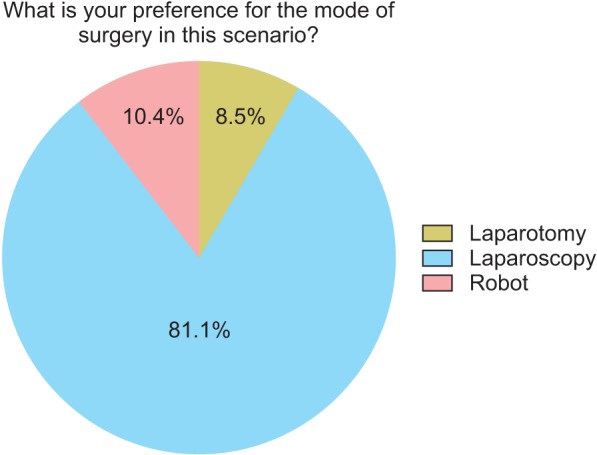
Scenario 1 (mode of surgery for presumed stage I endometrial cancer): the patient was diagnosed with presumed stage I/grade 1 endometrioid adenocarcinoma. Fig. 1 shows the respondents' treatment preferences for the mode of surgery. The majority of respondents (81%) would recommend laparoscopy and only 8.5% stated laparotomy. Approximately 10% of respondents preferred robotic surgery for this clinical scenario.
Fig. 1. Mode of surgery for presumed stage I disease.
Scenario 2 (management for incidentally found stage I endometrial cancer): the patient was incidentally diagnosed with endometrial cancer. A general gynecologist performed a total hysterectomy and bilateral salpingo-oophorectomy without lymphadenectomy.
Scenario 2A (incidentally found stage I/grade 1 endometrial cancer): the final pathology report shows stage IA/grade 1 endometrioid adenocarcinoma. Table 2 lists the respondents' preferences in this scenario. Only 9.5% would recommend additional therapy. All respondents who recommended additional therapy preferred laparoscopic lymph node dissection.
Table 2. Surveyed Korean Gynecologic Oncology Group members' additional therapy recommendations for incidentally found stage I endometrial cancer.
| Scenario | 2A* | 2B† |
|---|---|---|
| Final pathology | IAG1 | IAG3 |
| Recommend adjuvant therapy (%) | 9.5 | 85.6 |
| Type of therapy recommended (%) | ||
| Laparoscopy for lymph node dissection | 100 | 34.1 |
| Laparotomy for lymph node dissection | 0 | 3.4 |
| Vaginal brachytherapy | 0 | 36.4 |
| Whole pelvic radiation therapy | 0 | 18.2 |
| Chemotherapy | 0 | 8 |
*2A, incidentally found stage I/grade 1 endometrial cancer. †2B, incidentally found stage I/grade 3 endometrial cancer.
Scenario 2B (incidentally found stage I/grade 3 endometrial cancer): the final pathology report reveals stage IA/grade 3 disease. Table 2 lists the respondents' preferences. The majority of respondents (85.6%) would recommend additional therapy in this scenario. Among those who recommended additional therapy, vaginal brachytherapy (36.4%) and laparoscopic lymph node dissection (34.1%) were the most commonly preferred options.
Scenario 3 (extent of lymphadenectomy for presumed stage I disease)
Scenario 3A (presumed stage IA/grade 1 endometrial cancer): the patient was diagnosed with presumed stage IA/grade 1 endometrioid adenocarcinoma based on preoperative magnetic resonance imaging (MRI) and biopsy. Preoperative cancer antigen 125 was within the normal range. Table 3 shows the respondents' treatment preferences for the extent of surgery. Of all the respondents, 19.8% stated that lymphadenectomy could be omitted and 21.7% recommended selective lymphadenectomy based on sentinel biopsy or frozen results for patients with presumed stage IA disease. More than half of the respondents (58.5%) preferred lymphadenectomy, of which 31.1% preferred pelvic lymphadenectomy only, 15.1% preferred pelvic and para-aortic lymphadenectomy up to the level of the inferior mesenteric artery (IMA), and 12.3% preferred pelvic and para-aortic lymphadenectomy up to the level of the renal vein.
Table 3. Extent of lymphadenectomy for presumed stage I disease.
| Scenario | 3A* | 3B† | 3C‡ |
|---|---|---|---|
| Preopative biopsy results (grade) | 1 | 1 | 3 |
| Preopative MRI results (myometrial invasion) | Less than half | More than half | More than half |
| Extent of surgery (%) | |||
| SH/BSO | 19.8 | 0 | 0 |
| SH/BSO+sentinel biopsy | 6.6 | 2.9 | 1.9 |
| SH/BSO+selective lymphadenectomy with frozen results | 15.1 | 3.9 | 1.0 |
| SH/BSO+PLND | 31.1 | 21.4 | 10.7 |
| SH/BSO+PLND/PALND (up to IMA level) | 15.1 | 35.0 | 34.0 |
| SH/BSO+PLND/PALND (up to renal vein level) | 12.3 | 36.9 | 52.4 |
BSO, bilateral salpingo-oophorectomy; IMA, inferior mesenteric artery; MRI, magnetic resonance imaging; PALND; para-aortic lymph node dissection; PLND, pelvic lymph node dissection; SH, simple hysterectomy.
*3A, presumed stage IA/grade 1 endometrial cancer. †3B, presumed stage IB/grade 1 endometrial cancer. ‡3C, presumed stage IB/grade 3 endometrial cancer.
Scenario 3B (presumed stage IB/grade 1 endometrial cancer): the patient was diagnosed with presumed stage IB/grade 1 disease based on preoperative MRI and biopsy. Respondents' preferences for the extent of surgery are shown in Table 3. The majority of respondents (93.3%) would recommend lymphadenectomy in this scenario, of which 21.4% preferred pelvic lymphadenectomy, 35.0% preferred pelvic and para-aortic lymphadenectomy up to the IMA level, and 36.9% preferred pelvic and para-aortic lymphadenectomy up to the level of the renal vein.
Scenario 3C (presumed stage IB/grade 3 endometrial cancer): the patient was diagnosed with presumed stage IB/grade 3 disease based on preoperative MRI and biopsy. Respondents' preferences for the extent of surgery are shown in Table 3. The majority of respondents (97.1%) indicated that lymphadenectomy would be recommended, of which 10.7% preferred pelvic lymphadenectomy, 34.0% preferred pelvic and paraaortic lymphadenectomy up to the IMA level, and 52.4% preferred pelvic and para-aortic lymphadenectomy up to the level of the renal vein.
3. Adjuvant treatment
Table 4 shows respondents' preferences for adjuvant therapy in completely staged endometrial cancer. Respondents were asked to complete a table showing the preferred adjuvant therapy based on pathologic findings. In patients with stage IA/grade 1 disease, all respondents indicated that observation was preferable. Our survey reveals that more than 70% of members administered adjuvant therapy except stage IA/grade 1 or stage IA/grade 2: more than 90% administered adjuvant therapy when patients exhibited stage IA/grade 3, stage IB/grade 2 or stage IB/grade 3 disease. In patients with stage IB/grade 3 disease, the majority of respondents (99%) would recommend adjuvant therapy, among which whole pelvic radiation therapy (WPRT) was preferred by 34.4% and WPRT and brachytherapy was preferred by 26%.
Table 4. Surveyed Korean Gynecologic Oncology Group members' adjuvant therapy recommendations for stage I endometrial cancer according to stage and grade.
| Adjuvant options (%) | IAG1 | IAG2 | IAG3 | IBG1 | IBG2 | IBG3 |
|---|---|---|---|---|---|---|
| Observation | 100 | 70.8 | 9.4 | 28.1 | 8.3 | 1 |
| VB | 0 | 19.8 | 46.9 | 35.4 | 37.6 | 17.7 |
| WPRT | 0 | 6.3 | 28.1 | 25 | 26 | 34.4 |
| WPRT+brachytherapy | 0 | 1 | 4.2 | 4.2 | 13.5 | 26 |
| Chemotherapy | 0 | 1 | 7.3 | 4.2 | 7.3 | 8.3 |
| CCRT | 0 | 1 | 4.2 | 3.1 | 7.3 | 12.5 |
CCRT, concurrent chemoradiation therapy; VB, vaginal brachytherapy; WPRT, whole pelvic radiation therapy.
Scenario 4 (adjuvant treatment for stage II): the patient has stage II endometrioid adenocarcinoma with less than half myometrial invasion. Respondents' preferences for adjuvant therapy are listed in Table 5. The majority of respondents (89.6%) would recommend adjuvant therapy for stage II disease, among which WPRT was preferred by 31.8% and vaginal brachytherapy was preferred by 29.4%.
Table 5. Surveyed Korean Gynecologic Oncology Group members' adjuvant therapy recommendations for completely staged endometrial cancer.
| Scenario | Stage II | Stage IA and positive cytology | Stage IIIC1 | Stage IIIA |
|---|---|---|---|---|
| Adjuvant therapy (%) | ||||
| Yes | 89.6 | 55.3 | 100 | 95.7 |
| No | 10.4 | 44.7 | 0 | 4.3 |
| If yes, preferred treatment (%) | ||||
| 1 | WPRT (31.8) | Chemotherapy (57.7) | CCRT (53.2) | Chemotherapy (42.0) |
| 2 | VB (29.4) | CCRT (17.3) | Chemotherapy (28.7) | CCRT (31.8) |
| 3 | WPRT+VB (21.2) | WPRT (13.5) | WPRT+VB (12.8) | WPRT (17.0) |
| 4 | CCRT (14.1) | Hormone therapy (7.7) | WPRT (5.3) | WPRT+VB (9.1) |
CCRT, concurrent chemoradiotherapy; VB, vaginal brachytherapy; WPRT, whole pelvic radiation therapy.
Scenario 5 (adjuvant treatment for stage IA and positive cytology): the patient has stage IA/grade 1 endometrioid adenocarcinoma and malignant cytology. Table 5 shows the respondents' preferences for adjuvant therapy. Over half of respondents (55%) would recommend adjuvant therapy, with 57.7% indicating chemotherapy as their first preference.
Scenario 6 (adjuvant treatment for stage IIIC1): The patient has stage IIIC1 endometrioid adenocarcinoma with more than half of myometrial invasion. Table 5 shows the respondents' preferences for adjuvant therapy. All respondents indicated that adjuvant therapy should be performed in this scenario. More than half of the respondents who recommended adjuvant therapy stated that concurrent chemoradiotherapy (CCRT) would be their first choice of adjuvant therapy.
Scenario 7 (adjuvant treatment for stage IIIA): The patient has stage IIIA/grade 1 endometrioid adenocarcinoma with less than half myometrial invasion. Respondents' preferences of adjuvant therapy are listed in Table 5. The majority of respondents (95.7%) suggested the use of adjuvant therapy in microscopic ovarian metastasis. The most common treatment choices were chemotherapy (42.0%) and CCRT (31.8%).
DISCUSSION
When it came to the mode of surgery, there was a general consensus among KGOG members that minimally invasive surgery was preferable. However, we observed differences between KGOG members in current practice patterns for the treatment of endometrial cancer. This discrepancy was particularly prominent for the extent of surgery and adjuvant therapy options.
The role of minimally invasive surgery in endometrial cancer is expanding. Between 2009 and 2015, there have been significant increases in the proportion of KGOG survey respondents who think that minimally invasive surgery is appropriate for early-stage endometrial cancer (from 49% to 91.5% [n=41/84 to 97/106], p<0.001) [3]. With similar outcomes for laparoscopy and laparotomy in the Gynecologic Oncology Group (GOG) LAP2 study [7], minimally invasive surgery is now considered standard for the treatment of endometrial cancer in Korea. Similarly, a recent survey by the Society of Gynecologic Oncology (SGO) showed that the majority of respondents (85.5%) preferred minimally invasive surgery for the staging of endometrial cancer [8]. However, robotic surgery is not commonly performed in Korea: while laparoscopy is the preferred option in Korea, the SGO survey showed that 97% of respondents now perform robotic gynecologic procedures, compared with 29.0% in the 2007 survey. The SGO survey demonstrated that more than half of the respondents who performed robotic surgery stated that they used it for 50% or more of all their gynecologic cases.
For the extent of surgery for presumed low-risk endometrial cancer, there was a significant difference in opinion among the KGOG respondents, and we found a clear discrepancy between the clinical guidelines and the actual practice adopted by clinicians. As two large randomized controlled trials have demonstrated that comprehensive surgical staging does not improve progression-free or overall survival [5,6], the current National Comprehensive Cancer Network (NCCN) guidelines recommend a more selective and tailored lymphadenectomy approach in early-stage endometrial cancer [9,10]. In this survey, we observed that approximately 60% of respondents recommended lymphadenectomy at least at the pelvic level. The KGOG survey performed in 2009 showed that approximately 67% of respondents preferred routine pelvic lymphadenectomy [3]. As such, there has not been a significant decrease in the proportion of respondents preferring routine pelvic lymphadenectomy for early-stage endometrial cancer in recent years (67% to 58.5% [n=56/84 to 62/106], p=0.249). Considering the results of surveys on lymphadenectomy conducted in other countries, we found significant variation between different geographic regions: While countries in Asia (72.8%) and Central Europe (55.6%) routinely perform lymphadenectomy, countries in the north and south of Europe as well as the United Kingdom, United States, and Canada perform routine lymphadenectomy in less than a third of endometrial cancer cases [11].
The anatomic borders of the lymphadenectomy continue to be controversial in intermediate- and high-risk endometrial cancer. About 37% members defined the upper border of para-aortic lymphadenectomy as the renal vein for intermediate-risk endometrial cancer (presumed stage IB/grade 1), while more than half defined the upper border of para-aortic lymphadenectomy as the renal vein for high-risk endometrial cancer (presumed stage IB/grade 3). Compared to just 11% of members preferring to remove nodes to the level of the renal vein in the 2010 SGO survey [12], the percentage of Korean gynecologic oncologists performing para-aortic lymphadenectomy up to the renal vein is relatively high.
Our survey is the first to assess practice patterns for adjuvant treatment in patients with endometrial cancer in Korea, as we did not ask about adjuvant practice in the 2009 survey. Indications for adjuvant therapy for patients with endometrial cancer are determined by various pathologic prognostic factors such as histologic subtype, grade, lymph node metastasis, myometrial invasion, and lymphovascular space invasion. Patient selection criteria for adjuvant therapy and optimal regimens for endometrial cancer have not yet been established in clinical practice. The current NCCN guidelines allow a broad range of adjuvant therapy options for endometrial cancer.
We observed different adjuvant therapy patterns for the treatment of disease confined to the uterus and for disease with adnexal or nodal involvement. Our survey showed that WPRT and/or vaginal brachytherapy are commonly performed for Stage I endometrial cancer. Four trials evaluated the role of WPRT in endometrial cancer and failed to show improved overall survival [13,14,15,16]. As Postoperative Radiation Therapy for Endometrial Carcinoma-2 (PORTEC-2) showed that vaginal brachytherapy has similar vaginal and pelvic control rates and overall survival to those for WPRT, vaginal brachytherapy is a reasonable choice for patients with stage I endometrial cancer [4]. As evidence that this finding has been adopted Korea, vaginal brachytherapy was the preferred option among KGOG members. Despite adjuvant therapy with WPRT or vaginal brachytherapy, a significant proportion of patients still experience distant metastases. Although the role of adjuvant chemotherapy is currently being studied (GOG 249, PORTEC-3), adjuvant chemotherapy has been adopted among some clinicians even for the treatment of disease confined to the uterus.
Among KGOG members, there is a consensus that patients with stage IIIA and stage IIIC1 disease need adjuvant therapy. However, there is a broad range of opinion on the optimal means of adjuvant therapy. Generally, chemotherapy or CCRT are the preferred options for patients with extrauterine disease. This trend may be a reflection of the current guidelines favoring chemotherapy based on the results of the GOG-122 trial [17]. When we examined survey results from other countries, we found that chemotherapy was the preferred option for adjuvant therapy among Japanese Gynecologic Oncology Group members (79.9%) [18], who performed radiotherapy in just 13% of cases and did not consider CCRT as a treatment option.
While our survey only captures the reported practice patterns of 50% of KGOG members, there is clear variation among practicing gynecologic oncologists. This study is limited by both reporting biases and the response rate. In addition, we did not include non-endometrioid histology and considered only endometrioid adenocarcinoma.
The surgical extent of lymphadenectomy is still one of the most controversial topics in the management of endometrial cancer. Furthermore, there is a broad range of options for adjuvant therapy in the treatment of this disease. In general, radiotherapy is preferred for stage I and stage II disease and chemotherapy is preferred for stage III disease. Currently, the Korean guidelines for treating endometrial cancer are in the process of being revised. For standardizing practice patterns and improving guideline adherence, further studies will be required to identify the differences between actual practice and the revised guidelines once they are published.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
Supplementary Material
References
- 1.Lim MC, Moon EK, Shin A, Jung KW, Won YJ, Seo SS, et al. Incidence of cervical, endometrial, and ovarian cancer in Korea, 1999-2010. J Gynecol Oncol. 2013;24:298–302. doi: 10.3802/jgo.2013.24.4.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee JY, Kim EY, Jung KW, Shin A, Chan KK, Aoki D, et al. Trends in gynecologic cancer mortality in East Asian regions. J Gynecol Oncol. 2014;25:174–182. doi: 10.3802/jgo.2014.25.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee TS, Kim JW, Kim SH, Seong SJ, Song ES, Kim JH, et al. Surgical practice patterns in endometrial cancer: results of the Korean Gynecologic Oncology Group survey. J Gynecol Oncol. 2009;20:107–112. doi: 10.3802/jgo.2009.20.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nout RA, Smit VT, Putter H, Jurgenliemk-Schulz IM, Jobsen JJ, Lutgens LC, et al. Vaginal brachytherapy versus pelvic external beam radiotherapy for patients with endometrial cancer of high-intermediate risk (PORTEC-2): an open-label, non-inferiority, randomised trial. Lancet. 2010;375:816–823. doi: 10.1016/S0140-6736(09)62163-2. [DOI] [PubMed] [Google Scholar]
- 5.ASTEC study group. Kitchener H, Swart AM, Qian Q, Amos C, Parmar MK. Efficacy of systematic pelvic lymphadenectomy in endometrial cancer (MRC ASTEC trial): a randomised study. Lancet. 2009;373:125–136. doi: 10.1016/S0140-6736(08)61766-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benedetti Panici P, Basile S, Maneschi F, Alberto Lissoni A, Signorelli M, Scambia G, et al. Systematic pelvic lymphadenectomy vs. no lymphadenectomy in early-stage endometrial carcinoma: randomized clinical trial. J Natl Cancer Inst. 2008;100:1707–1716. doi: 10.1093/jnci/djn397. [DOI] [PubMed] [Google Scholar]
- 7.Walker JL, Piedmonte MR, Spirtos NM, Eisenkop SM, Schlaerth JB, Mannel RS, et al. Recurrence and survival after random assignment to laparoscopy versus laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group LAP2 Study. J Clin Oncol. 2012;30:695–700. doi: 10.1200/JCO.2011.38.8645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Conrad LB, Ramirez PT, Burke W, Naumann RW, Ring KL, Munsell MF, et al. Role of minimally invasive surgery in gynecologic oncology: an updated survey of members of the Society of Gynecologic Oncology. Int J Gynecol Cancer. 2015;25:1121–1127. doi: 10.1097/IGC.0000000000000450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huh WK, Straughn JM, Jr, Kelly FJ, Kilgore LC. Endometrial carcinoma. Curr Treat Options Oncol. 2001;2:129–135. doi: 10.1007/s11864-001-0055-z. [DOI] [PubMed] [Google Scholar]
- 10.Sonoda Y. Surgical treatment for apparent early stage endometrial cancer. Obstet Gynecol Sci. 2014;57:1–10. doi: 10.5468/ogs.2014.57.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fotopoulou C, Kraetschell R, Dowdy S, Fujiwara K, Yaegashi N, Larusso D, et al. Surgical and systemic management of endometrial cancer: an international survey. Arch Gynecol Obstet. 2015;291:897–905. doi: 10.1007/s00404-014-3510-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soliman PT, Frumovitz M, Spannuth W, Greer MJ, Sharma S, Schmeler KM, et al. Lymphadenectomy during endometrial cancer staging: practice patterns among gynecologic oncologists. Gynecol Oncol. 2010;119:291–294. doi: 10.1016/j.ygyno.2010.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aalders J, Abeler V, Kolstad P, Onsrud M. Postoperative external irradiation and prognostic parameters in stage I endometrial carcinoma: clinical and histopathologic study of 540 patients. Obstet Gynecol. 1980;56:419–427. [PubMed] [Google Scholar]
- 14.Creutzberg CL, van Putten WL, Koper PC, Lybeert ML, Jobsen JJ, Warlam-Rodenhuis CC, et al. Surgery and postoperative radiotherapy versus surgery alone for patients with stage-1 endometrial carcinoma: multicentre randomised trial. PORTEC Study Group. Post Operative Radiation Therapy in Endometrial Carcinoma. Lancet. 2000;355:1404–1411. doi: 10.1016/s0140-6736(00)02139-5. [DOI] [PubMed] [Google Scholar]
- 15.ASTEC/EN.5 Study Group. Blake P, Swart AM, Orton J, Kitchener H, Whelan T, et al. Adjuvant external beam radiotherapy in the treatment of endometrial cancer (MRC ASTEC and NCIC CTG EN.5 randomised trials): pooled trial results, systematic review, and meta-analysis. Lancet. 2009;373:137–146. doi: 10.1016/S0140-6736(08)61767-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keys HM, Roberts JA, Brunetto VL, Zaino RJ, Spirtos NM, Bloss JD, et al. A phase III trial of surgery with or without adjunctive external pelvic radiation therapy in intermediate risk endometrial adenocarcinoma: a Gynecologic Oncology Group study. Gynecol Oncol. 2004;92:744–751. doi: 10.1016/j.ygyno.2003.11.048. [DOI] [PubMed] [Google Scholar]
- 17.Randall ME, Filiaci VL, Muss H, Spirtos NM, Mannel RS, Fowler J, et al. Randomized phase III trial of whole-abdominal irradiation versus doxorubicin and cisplatin chemotherapy in advanced endometrial carcinoma: a Gynecologic Oncology Group Study. J Clin Oncol. 2006;24:36–44. doi: 10.1200/JCO.2004.00.7617. [DOI] [PubMed] [Google Scholar]
- 18.Watanabe Y, Kitagawa R, Aoki D, Takeuchi S, Sagae S, Sakuragi N, et al. Practice pattern for postoperative management of endometrial cancer in Japan: a survey of the Japanese Gynecologic Oncology Group. Gynecol Oncol. 2009;115:456–459. doi: 10.1016/j.ygyno.2009.08.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


