Abstract
Background:
Stress urinary incontinence (SUI) is considered as one of the major hygienic problems among women. The main aim of the study is to assess the potential risk factors associated with SUI among Iranian women.
Materials and Methods:
This study was conducted on 90 married women with history of SUI diagnosed by an urologist and were selected randomly. Their pelvic muscles contraction (PMC) and the history of the subjects were assessed for some of risk factors such as age, height, weight, body mass index (BMI), pregnancy history, miscarriage, type of delivery (normal vaginal delivery or cesarean section), number of offspring born healthy in addition to other risk factors such as chronic cough, constipation and hypothyroidism by use of POP Questionnaire. Data were analyzed using Pearson correlation coefficient and SPSS version 18 Software.
Results:
There was a significant relation between SUI and height (P < 0.05, r = 0.45), vaginal delivery (NVD) (P < 0.05, r = 0.2), number of genitourinary surgery (P < 0.05, r = 0.42), hypothyroidism and constipation (P < 0.05). An inverse relatively strong significant relation was found between SUI and cesarean section (P < 0.05, r = –0.50) No significant relation was found between SUI and weight, BMI, age, chronic cough and miscarriage, and other study parameters. An inverse significant relation between PMC and weight (P < 0.05, r = –0.52), BMI (P < 0.05, r = –0.42) and number of genitourinary surgery (P < 0.05, r = –0.18).
Conclusion:
Cesarean section had a preventive effect on SUI versus normal vaginal delivery. The rate of SUI was higher in taller women or those suffering from hypothyroidism or constipation or who had genitourinary surgery. The women with high BMI had lower pelvic floor muscles strength.
Keywords: Biofeedback, risk factors, stress urinary incontinence
INTRODUCTION
Urinary incontinence is the unintentional passing of urine. It may not be so weighty in some situations and in slight volume, but it may result in disappointment and anxiety particularly among women. Since the disorder is more common among females compared to males due to the distinctions of their body structure and specifically pregnancy issue, there has been specific attention given to this disease among females. As some various changes occur after labor, the women are more susceptible to disease due to the decrease in their pelvic floor muscles contractions.[1,2,3] It has been confirmed that 10% to 30% of women of age group 15-46 years and 50% of patients in care centers suffer from urinary incontinence[4], with the number increasing with advancing age. As a result, we observe that 30% to 50% of women over 65 years complain of this disorder.[5] Various factors are involved in SUI occurrence, such as decrease pelvic floor muscles contractions, heavy exercises and physical activities, aging, menopause, number of deliveries, type of labor, increase weight, constipation, chronic coughs and many more factors.[6,7] The risk of developing SUI among obese women with a body mass index of 30 or more (MBI ≥30) regardless of age and number of deliveries is twice compared to underweight women.[8] Thirty four percent of people diagnosed with SUI suffer from mental and social disorders such as depression, insomnia and other related problems. These factors negatively affect their social and sexual life.[9] Therefore, due to the substantial importance of these problems, it is vital to identify potential risk factors on developing the disorder with the intention of preventing them or at least lower their effects. Hence, the aim of the research is to assess and evaluate relation of potential risk factors and SUI among Iranian women.
MATERIALS AND METHODS
This is a cross-sectional study, which was carried out from November 2012 to May 2013 among the married women who had more than 18 years of age that were referred to Urology Clinics of affiliated hospitals of Isfahan Medical Sciences, Iran, and were diagnosed with SUI by use of clinical examination (Marshall Test and Positive Cough Test), Pad Test (the weight gain of more than 8 g/24 h has been considered to be significant) and if the previous test results were not reliable, urodynamic tests was done for the cases. Among them, 90 women were selected by simple random sampling and by biofeedback device using a computer and electronic instruments to let an individual know when the pelvic muscles are contracting. The pelvic floor muscles strength were measured through the vaginal probes, which were specified for each patients. POP Questionnaire was completed for each patient consisting of information such as age, height, weight, body mass index (BMI), history of pregnancy and delivery (number of conceptions, number of offspring delivered healthy, number of miscarriage, genitourinary surgery, and other potential risk factors such as smoking cigarette, hypothyroidism, chronic cough and constipation. Collected data were recorded and analyzed using SPSS 18 Software and relevant statistical tests, such as Pearson correlation coefficient, were applied to assess the relationship between these factors and SUI. A P < 0.05 was considered as significant level in these statistical methods.
RESULTS
The total number of patients in this study was 90 individuals, aging 43 to 53 years (mean: 48 years). The range of the sample height was 156-167 cm (mean: 162 cm). The range of our subjects’ weight was 60.4-79 kg (mean: 69.9 Kg). Average BMI was 26.7 ± 3.5. Given the results in Table 1, we evaluate the relation between risk factors and SUI and PMC.
Table 1.
Pearson correlation coefficient for pelvic floor contractions and SUI with some risk factors
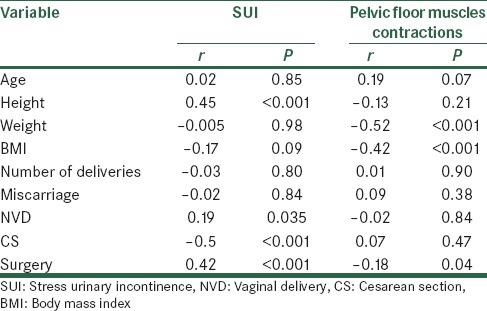
Pearson correlation coefficient revealed a direct significant relation between SUI and height (P < 0.05, r = 0.45), vaginal delivery (NVD) (P < 0.05, r = 0.2), number of genitourinary surgery (P < 0.05, r = 0.42), hypothyroidism and constipation (P < 0.05). On the other hand, an inverse relatively strong significant relation was found between SUI and cesarean section (P < 0.05, r = –0.50). That is, as the number of cesarean section increases, likelihood of developing SUI decreases. In addition, No significant relation was found between SUI and weight, BMI, age, chronic cough and miscarriage, and other study parameters. Also, this correlation demonstrated an inverse significant relation between PMC and weight (P < 0.05, r = –0.52), BMI (P < 0.05, r = –0.42) and number of genitourinary surgery (P < 0.05, r = –0.18).
DISCUSSION
The study provides evidences that there is a direct and significant relation between height and rate of urine leakage. However, it has not been proven that there is a relationship between height and having bigger pelvic bone but it seems, taller women have pelvic bone with higher diameter. Increase of pelvic bone diameter results on higher consistency between anatomic position of pelvic internal organs and pelvic floor muscles and levator ani muscle. So with aging and increasing number of delivery, taller women with wider pelvic bone are more prone to develop prolapse and weakening of pelvic floor muscles and consequently the possibility for urinary incontinence and increase severity of the complications.[10,11,12,13] There was an direct relation between NVD and SUI and also inverse relation between urine leakage and number of cesarean section among sample patients, and because actually, NVD considers an actual factor in causing prolapse of pelvic floor muscles and increasing SUI development, cesarean section which considers a replacement to NVD and there has been a tendency toward cesarean section selectively for first pregnancy or consecutive pregnancies in hope to prevent or decrease urinary incontinence and involuntary stool elimination, vaginal prolapse or hemorrhoids.[14,15,16,17] Other obtained result from this study was the inverse relation between pelvic floor muscle contractions and BMI among patients. Other study has also shown a significant relation between urinary incontinence and BMI increase that affect the quality of life of patients negatively, and obese women and those women that do not exercise regularly are more susceptible to urinary incontinence.[18,19,20] In fact, it is expected a decrease on pelvic floor muscles contractions with BMI increase, which was agreed by our study too, and consequently more potential risk for urine leakage. However, the result was not fruitful in this second part of study as no significant relation was found between BMI and urine leakage and a need for in depth study was felt.[11,21] In this research population, we had found 16% for incidence of hypothyroidism; in comparison with general women population (about 10%)[22] direct significant relationship between hypothyroidism and the SUI had been demonstrated. So according to the previous studies there is a definite relation between thyroid and voiding dysfunction.[23]
Complications in pelvic floor muscles function affect women with various ages and have a wide range of signs and symptoms that is rarely separable and some predisposing factors include pregnancy, birth trauma, increase age, hysterectomy and lifestyle.[18,24] Therefore, it is fundamental to provide some guidance in educational programs for women health benefit.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lemone P, Burke K. Medical-Surgical Nursing. 3rd ed. New Jersey: Pearson Education; 2004. pp. 733–5. [Google Scholar]
- 2.Holroyd-Ledue JM, Straus SE. Management of urinary incontinence in women. Scientific review. JAMA. 2004;297:986–95. doi: 10.1001/jama.291.8.986. [DOI] [PubMed] [Google Scholar]
- 3.Abreu NS, Baracho ES, Tirado MG, Dias RC. Quality of life from the prespective of elderly women with urinary incontinence. Rev Bras Fisioter, São Carlos. 2007;11:429–36. [Google Scholar]
- 4.Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4–20. doi: 10.1002/nau.20798. [DOI] [PubMed] [Google Scholar]
- 5.Jonathan BF. 13th ed. Alphen aan den Rijn, South Holland, Netherlands: Wolters Cluver; 2002. Novak's Gynecology; pp. 637–86. [Google Scholar]
- 6.Littleton L, Engebretson J. Maternal, Neonatal and Women's Health Nursing. Albany, NY: Delmar Thomson Learning Inc; 2002. p. 245. [Google Scholar]
- 7.Kegel AH. Progressive resistance exercise in the functional restoration of the perineal muscle. Am J Obstet Gynecol. 1948;56:238–48. doi: 10.1016/0002-9378(48)90266-x. [DOI] [PubMed] [Google Scholar]
- 8.Henalla SM, Kirwan P, Castleden CM, Hutchins CJ, Breeson AJ. The effect of pelvic floor exercises in the treatment of genuine urinary stress incontinence in women at two hospitals. Br J Obstet Gynaecol. 1998;95:602–6. doi: 10.1111/j.1471-0528.1988.tb09491.x. [DOI] [PubMed] [Google Scholar]
- 9.Wilson PD, Al Samarrai T, Deakin M, Kolbe E, Brown AD. An objective assessment of physiotherapy for female genuine stress incontinece. Br J Obstet Gynaecol. 1987;94:575–82. doi: 10.1111/j.1471-0528.1987.tb03153.x. [DOI] [PubMed] [Google Scholar]
- 10.Mouritsen L. Pelvic floor exercise for female stress urinary incontinece. Int Urogynecol J. 1994;5:44–51. [Google Scholar]
- 11.Cammu H, van Nylen M. Pelvic floor muscle exercises: 5 years later. Urology. 1995;45:113–8. doi: 10.1016/s0090-4295(95)97180-7. [DOI] [PubMed] [Google Scholar]
- 12.Berghmans LC, Frederiks CM, de Bie RA, Weil EH, Smeets LW, van Waalwijk van Doom ES, et al. Efficacy of biofeedback, when included with pelvic floor muscle exercise treatment, for genuinc stress incontinence. Neurourol Urodyn. 1996;15:37–52. doi: 10.1002/(SICI)1520-6777(1996)15:1<37::AID-NAU4>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 13.Glavind K, Nøhr SB, Walter S. Biofeedback and physiotherapy versus physiotherapy alone in treatment of genuine stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7:339–43. doi: 10.1007/BF01901111. [DOI] [PubMed] [Google Scholar]
- 14.Bastana KN. Electrotherapy Simplifield. 1st ed. India: Jaypee Brothers Medical Publishers; 2008. pp. 148–206. [Google Scholar]
- 15.Fantl JA, Newman DK, Colling J, DeLancey JO, Keeys C, Loughery R, et al. Rockville, MD: US Department of Health and Human Services Public Health Service, Agency for Health Care Policy and Research: AHCPR Publication; 1996. Urinary incontinence in adults: Acute and chronic management. Clinical Practice Guideline No. 2; p. 16. [Google Scholar]
- 16.Stein M, Discippio W, Davia M, Taub H. Biofeedback for the treatment of stress and urge incontinence. J Urol. 1995;153:641–3. doi: 10.1097/00005392-199503000-00023. [DOI] [PubMed] [Google Scholar]
- 17.Bump RC, Hurt WG, Fantl JA, Wyman JF. Assessment of kegel muscle exercise performance after brief verbal instruction. Am J Obstet Gynecol. 1991;165:322–9. doi: 10.1016/0002-9378(91)90085-6. [DOI] [PubMed] [Google Scholar]
- 18.Wyman JF, Fantl JA, McClish DK, Harkins SW, Uebersax JS, Ory MG. Quality of life following bladder training in older women with urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1997;8:223–9. doi: 10.1007/BF02765818. [DOI] [PubMed] [Google Scholar]
- 19.Burns PA, Pranikoff K, Nochajski TH, Hadley EC, Levy KJ, Ory MG. A comparison of effectiveness of biofeedback and pelvic muscle exercise treatment of stress incontinence in older community-dwelling women. J Gerontol. 1993;48:M167–74. doi: 10.1093/geronj/48.4.m167. [DOI] [PubMed] [Google Scholar]
- 20.Glavind K, Nøhr SB, Walter S. Pelvic floor training using biofeedback for muscle awareness in the treament of stress urinary incontinence: Preliminary results. Int Urogynecol J. 1992;3:288–91. [Google Scholar]
- 21.Sung MS, Hong JY, Choi YH, Baik SH, Yoon H. FES-Biofeedback versus intensive pelvic floor muscle exercise for the prevention and prevention and treatment of genuine stress incontinence. J Korean Med Sci. 2000;15:303–8. doi: 10.3346/jkms.2000.15.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vanderpump MP. The epidemiology of thyroid disease. Br Med Bull. 2011;99:39–51. doi: 10.1093/bmb/ldr030. [DOI] [PubMed] [Google Scholar]
- 23.Alizadeh F, Zargham M, Nouri-Mahdavi K, Khorrami MH, Izadpanahi MH, Sichani MM. Bladder involvement in thyroid dysfunction. J Res Med Sci. 2013;18:167. [PMC free article] [PubMed] [Google Scholar]
- 24.Burns PA, Pranikoff K, Nochajski TH, Desotelle P, Harwood MK. Treament of stress incontinence with pelvic floor exercises and biofeedback. J Am Geriatr Soc. 1990;38:341–4. doi: 10.1111/j.1532-5415.1990.tb03517.x. [DOI] [PubMed] [Google Scholar]


