Abstract
Background:
Self-care management has recently been suggested as an effective approach for secondary prevention of hypertension. This study was conducted to examine whether self-care behaviors could modulate blood pressure levels and also comparing the different training methods of self-care on patients’ adherence and controlling hypertension.
Materials and Methods:
This study was a prospective randomized controlled clinical trial, conducted on 180 hypertensive patients referring to four centers in Isfahan, Iran, between July and December 2013. Block randomization method were applied to divide eligible subjects into four equal groups, including group A in which the patients and their family were educated by cardiology resident about self-care behaviors through eight sessions, group B and group C were obtained self-care education through four pamphlets or eight short message services (SMS), respectively and group D were obtained only usual care of hypertension without any training about self-care management.
Results:
Increasing vegetable intake and frequency of subject who took antihypertensive medication regularly and the reduction in the frequency of subjects who consumed high salt were significantly more in group A than the others (P = 0.001, P < 0.001 and P < 0.001, respectively). The systolic and diastolic blood pressure had significantly more reduction in the group A than the other groups (−8.18 ± 18.3 and − 3.89 ± 4.1; P < 0.001, respectively).
Conclusions:
The self-care management education integration into the usual care along with using SMS and other educational materials may improve the efficient and effective adherence strategies.
Keywords: Blood pressure, hypertension, pamphlet, randomized controlled clinical trial, self-care, short message service
INTRODUCTION
Hypertension is one of the main public health problems,[1] affecting approximately 25% of the adult population worldwide, and aging increases this figure.[2] Moreover, it is proposed that the prevalence rate of hypertension ranges from 5.2% to 55.3% in different populations.[3] Among Iranian adults the hypertension prevalence is 17.3%[4] and was known as the leading cause of cardiovascular events.[5]
The Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7) recommendation about self-care behaviors are beneficial approach to the management of blood pressure.[6] Meta-analysis of 18 randomized, controlled trials showed that self-care activities manage and treat high blood pressure.[7] Moreover it could decrease emergency and outpatient visits by 40% and 17%, respectively.[8] Therefore, it has recently been suggested as an effective approach for secondary prevention of hypertension.[9] A variety of self-care patterns including disease and symptoms awareness, home monitoring of blood pressure, lifestyle modifications and adherence to treatment were applied in different studies.[10,11,12] Thus, health professionals can play a critical role in training general population about self-care activities.[13,14,15,16] However referring of the patients to the clinics might have some difficulty for them, especially in low or middle income countries.[17] Several studies showed nonface to face education including short message services (SMS) and educational print resources can deliver self-care interventions to hypertensive patients for improving chronic care management.[17,18] Therefore, this system could lead to costs and life savings in healthcare centers’ in developing countries.[17]
To the best of our knowledge, there is no published dataset among Iranian populations on the effect of self-care interventions to manage blood pressure. Therefore, this study is a unique study in Iran which was conducted to examine whether self-care behaviors could modulate blood pressure levels and also comparing the different training methods of self-care on controlling hypertension.
MATERIALS AND METHODS
This study was a prospective randomized controlled clinical trial, conducted among 180 hypertensive patients referring to two major clinics of Isfahan University of Medical Sciences (IUMS) and two health centers in Isfahan, Iran, between July and December 2013. Convenience sampling, nonprobability method was done for subject recruitment during their routine visit in the clinics. Inclusion criteria were being more than 18-year-old; moderate hypertensive or stage I hypertension according to JNC7 (systolic blood pressure [SBP] - 140–158 and/or diastolic blood pressure [DBP] - 90–99);[7] previous hypertension diagnosed and their nationality was Iranian. Exclusion criteria were any acute disease and no willing to participate in the study. Detailed interviews were conducted by trained cardiology resident to obtain information of each participant. The questionnaires covered various health issues including socioeconomic, demographic characteristics, lifestyle behaviors (dietary habits, smoking and physical activity), medical history including medication use and presence or absence of dyslipidemia, diabetes mellitus (DM) and hypertension.
All patients who were willing to participate in this study signed an informed written consent. The study was approved by the Research Council and Ethics Committee of a Medical School of IUMS, Isfahan, Iran.
Block randomization method were applied to divide eligible subjects into four equal groups including group A in which the patients and their family were educated by cardiology resident about self-care behaviors through eight sessions and each session was about 1 h, group B and group C were obtained self-care education through four pamphlets or eight SMS, respectively and group D were obtained only usual care of hypertension without any training about self-care management. All the information used in the education, including face to face, pamphlets and SMS in the Persian language was given to all patients.
Content of hypertension self-management behaviors
Patients in group A, B and C were advised to adhere to take medication daily; increase physical activity aimed for 30–45 min of moderate-intensity aerobic activity (such as a brisk walk); most days of the week; follow the dietary approach to stop hypertension (DASH diet) including eat a diet rich in vegetables and reduce dietary sodium to below 1500 mg/day; stop smoking. Group D did not obtain any education about self-management of hypertension and they had only usual care of hypertension in the clinics.
The self-reported measure of adherence to medication was assessed by calling them weekly and asking about receiving and adhering to the education Failure to adhere defined if the patients in group A not participating in at least one educational session, group B and C not receiving at least one pamphlet and 3 SMS, respectively.
Statistical analysis
Statistical analyses were performed using SPSS for windows version 15 (SPSS Inc., Chicago, IL). Student's paired t-test was carried out to make comparisons between the baseline and the 8-month mean values and Wicoxon Rank test was utilized to compare frequency of qualitative related variables. Analysis of variance (ANOVA) was employed to compare the mean of quantitative and Chi-square test to compare frequency of qualitative baseline characteristics. Furthermore, ANOVA utilized to evaluate the intervention effect between four groups. P < 0.05 was considered as significant.
RESULTS
The study was carried out on 180 hypertensive subjects divided in four equal educational groups including face to face self-care education in the clinics, by pamphlets, SMS and none self-care education. All groups were taken usual care for hypertension. All of them were followed-up until end of study. As shown in Table 1, there was no significant difference in basic characteristics including age, duration of hypertension, gender and education based on educational group.
Table 1.
Basic characteristics of study population
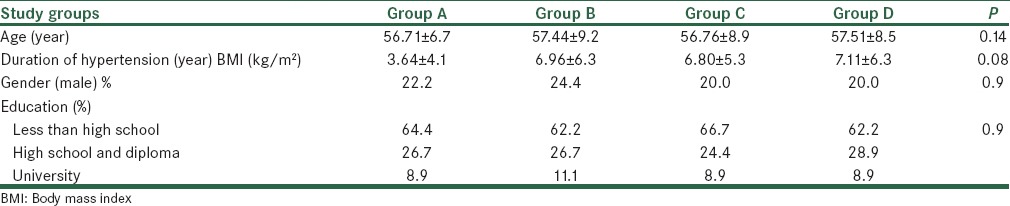
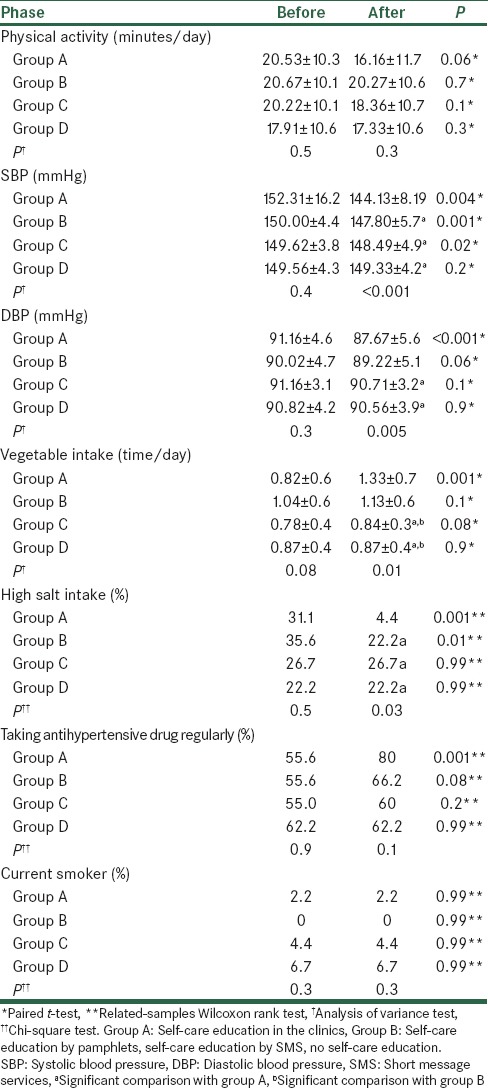
Table 2 demonstrates that mean of physical activity, SBP, DBP and vegetable intake as well as frequency of participants who consumed high salt food, took antihypertensive drug regularly and current smoker were no significant between different groups in the baseline. However, group A and B significantly consumed more vegetables than group C and D after study (P = 0.01). In addition, the frequency of subjects who consumed high salt food were higher in Group A than other groups (P = 0.03). The frequency of participants who took antihypertensive drug regularly and current smoker were no significant across the groups. The mean of SBP and DBP were significantly less than in group A than the others (P < 0.001 and P = 0.005, respectively). Paired analyses showed vegetable intake and frequency of regular taking antihypertensive drug increased after self-care education in group A (P = 0.001). The frequency of subjects who consumed high salt food decreased significantly in group A and B (P = 0.001 and P = 0.01, respectively). Finally, SBP had significant reduction in the group A (P = 0.004), B (P = 0.001) and C (P = 0.02) and DBP only in group A (P = 0.001) [Table 2].
Table 2.
Study population variables after intervention according to group educationa
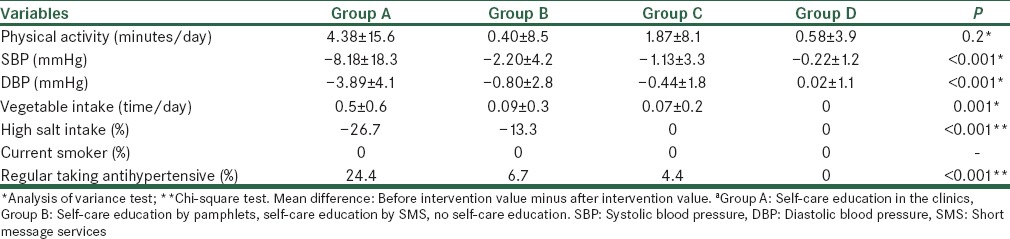
Increasing vegetable intake and frequency of subject who took antihypertensive medication regularly and the reduction in the frequency of subjects who consumed high salt were significantly more in group A than the others (P = 0.001, P < 0.001 and P < 0.001, respectively) [Table 3]. Furthermore, SBP and DBP had significantly more reduction in the group A than the other groups (−8.18 ± 18.3 and − 3.89 ± 4.1; P < 0.001, respectively).
Table 3.
Mean difference in participant's variables before and after intervention based on education groupa
DISCUSSION
This study showed that face to face self-care training offered BP improvement over pamphlet, SMS and usual care. In addition, education-based behavioral interventions could modify salt and vegetable intake as well as taking antihypertensive drug regularly. However, the literatures reported that printed educational materials and SMS.
We found an improvement in dietary components including vegetable and salt intake as well as regular antihypertensive drug taking by face to face self-care training course. In addition printed educational material could impact on salt intake. Although there were no significant differences between vegetable intake and the frequency of patients with high salt food consumption at the baseline, vegetable intake was significantly higher at the end of study through face to face consultations and pamphlets. In addition, the patients reduced high salt food consumption after face to face education of self-care behaviors. So that the mean vegetable intake increase 0.5 time/day in the participants who trained in the clinics which is about 5 times more than the participants who received pamphlets and SMS. Furthermore the regular medication adherence and using low salt diet improved in about ¼ of participants. However, other lifestyle behaviors including smoking and physical activity had no changes during the study. Warren-Findlow et al. reported that low-salt diet intake, medication regimens adherence, doing physical activity and quitting smoking increased during hypertension self-care intervention,[10] which was inconsistent to our finding except for in low–salt diet intake. It seems dietary modifications are the most practical self-care intervention, while and smoking and physical activity need more health personnel's regards and participants’ self-efficacy.[19]
In line with dietary modifications and medication adherence, SBP and DBP decreased via face to face self-care intervention and only we found DBP reduction using pamphlets education. Consistent to our finding several reviews demonstrated the self-care benefits on BPs, especially short-term effect.[8,20] According to these reviews the long-term effects of self-care education in 12 months were uncertain, thus it is necessary that these interventions be done continuously.
Moreover, we found no significant changes in all investigated self-care behaviors as well as BPs using educational SMS. Conflicting to our results several studies reported the beneficial effects of self-care education on medication adherence and other clinical relevant outcomes,[21,22,23,24,25] and hence that Bobrow et al. suggested using mobile phone technology via SMS is a novel, low cost method to convey the intervention and manage contact with patients mainly in a low-resource setting.[25] However, some studies utilized SMS as a reminder after face-to-face education.[17,22] Therefore, it appears in our population using SMS as a reminder may support people with hypertension in self-care management and improving outcomes.
LIMITATIONS
One limitation of this study was that we had no blindness since it was not applicable among our interventional groups. Using short questionnaire was our limitation because completing long questionnaire was complicated in the clinics; therefore we asked only the most important components of self-care.
CONCLUSIONS
Health professional in the clinics played an important role in training self-care behaviors, especially dietary modifications, medication adherence as well as BP regulation. While the printed educational materials and SMS could not affect favorably on lifestyle changes and hypertension control. However, the integration of the self-care management education into the usual care in the clinics and extension of the learning into the home by the means of SMS and other educational materials will increase the potentials of such interventions in the efficient and effective adherence strategies and therefore the healthcare will be available and accessible to all.
ACKNOWLEDGMENT
This study was residency thesis of H. Ahmadzadeh. MD (number 393015) funded by the Research Deputy of School of Medicine, Isfahan University of Medical Sciences. We thankful all health professional in the Clinics and Health Centers that the current study was done. Also we should appreciate all patients who participate in the study.
Footnotes
Source of Support: Cardiovascular Research Institute, Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Jones DW, Hall JE. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure and evidence from new hypertension trials. Hypertension. 2004;43:1–3. doi: 10.1161/01.HYP.0000110061.06674.ca. [DOI] [PubMed] [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 3.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet. 2005;365:217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 4.Shirani S, Kelishadi R, Sarrafzadegan N, Khosravi A, Sadri G, Amani A, et al. Awareness, treatment and control of hypertension, dyslipidaemia and diabetes mellitus in an Iranian population: The IHHP study. East Mediterr Health J. 2009;15:1455–63. [PubMed] [Google Scholar]
- 5.Sarrafzadegan N, Talaei M, Sadeghi M, Kelishadi R, Oveisgharan S, Mohammadifard N, et al. The Isfahan cohort study: Rationale, methods and main findings. J Hum Hypertens. 2011;25:545–53. doi: 10.1038/jhh.2010.99. [DOI] [PubMed] [Google Scholar]
- 6.US Department of Health and Human Services. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Institutes of Health. 2004 Report No.: NIH Publication No. 04-5230. [Google Scholar]
- 7.Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: Meta-analysis of randomised trials. BMJ. 2004;329:145. doi: 10.1136/bmj.38121.684410.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.NHS. Supporting People with Long Term Conditions to Self Care a Guide to Developing Local Strategies and Good Practice. 2006. Available from: http://www.selfmanagementsupport.health.org.uk/media_manager/public/179/SMS_resourcecentre_publications/Self_care-a_guide_to_developing_local_strategies_and_good practice.pdf/
- 9.Sadeghi M, Shiri M, Roohafza H, Rakhshani F, Sepanlou S, Sarrafzadegan N. Developing an appropriate model for self-care of hypertensive patients: First experience from EMRO. ARYA Atheroscler. 2013;9:232–40. [PMC free article] [PubMed] [Google Scholar]
- 10.Warren-Findlow J, Seymour RB, Brunner Huber LR. The association between self-efficacy and hypertension self-care activities among African American adults. J Community Health. 2012;37(1):15–24. doi: 10.1007/s10900-011-9410-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gohar F, Greenfield SM, Beevers DG, Lip GY, Jolly K. Self-care and adherence to medication: A survey in the hypertension outpatient clinic. BMC Complement Altern Med. 2008;8:4. doi: 10.1186/1472-6882-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Padfield PL. The case for home monitoring in hypertension. BMC Med. 2010;8:55. doi: 10.1186/1741-7015-8-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carter BL, Rogers M, Daly J, Zheng S, James PA. The potency of team-based care interventions for hypertension: A meta-analysis. Arch Intern Med. 2009;169:1748–55. doi: 10.1001/archinternmed.2009.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Victor RG, Ravenell JE, Freeman A, Leonard D, Bhat DG, Shafiq M, et al. Effectiveness of a barber-based intervention for improving hypertension control in black men: The BARBER-1 study: A cluster randomized trial. Arch Intern Med. 2011;171:342–50. doi: 10.1001/archinternmed.2010.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carter BL, Ardery G, Dawson JD, James PA, Bergus GR, Doucette WR, et al. Physician and pharmacist collaboration to improve blood pressure control. Arch Intern Med. 2009;169:1996–2002. doi: 10.1001/archinternmed.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woodward A, Wallymahmed M, Wilding J, Gill G. Successful cardiovascular risk reduction in Type 2 diabetes by nurse-led care using an open clinical algorithm. Diabet Med. 2006;23:780–7. doi: 10.1111/j.1464-5491.2006.01889.x. [DOI] [PubMed] [Google Scholar]
- 17.Okuboyejo S, Eyesan O. mHealth: Using mobile technology to support healthcare. Online J Public Health Inform. 2014;5:233. doi: 10.5210/ojphi.v5i3.4865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Redman S, Paul CL. A review of the effectiveness of print material in changing health-related knowledge, attitudes and behaviour. Health Promot J Austr Official J Austr Assoc Health Promot Prof. 1997;7:91–9. [Google Scholar]
- 19.Bosworth HB, Oddone EZ. A model of psychosocial and cultural antecedents of blood pressure control. J Natl Med Assoc. 2002;94:236–48. [PMC free article] [PubMed] [Google Scholar]
- 20.Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-measured blood pressure monitoring in the management of hypertension: A systematic review and meta-analysis. Ann Intern Med. 2013;159:185–94. doi: 10.7326/0003-4819-159-3-201308060-00008. [DOI] [PubMed] [Google Scholar]
- 21.Park LG, Howie-Esquivel J, Dracup K. A quantitative systematic review of the efficacy of mobile phone interventions to improve medication adherence. J Adv Nurs. 2014;70:1932–53. doi: 10.1111/jan.12400. [DOI] [PubMed] [Google Scholar]
- 22.Jones KR, Lekhak N, Kaewluang N. Using mobile phones and short message service to deliver self-management interventions for chronic conditions: A meta-review. Worldviews Evid Based Nurs. 2014;11:81–8. doi: 10.1111/wvn.12030. [DOI] [PubMed] [Google Scholar]
- 23.Khonsari S, Subramanian P, Chinna K, Latif LA, Ling LW, Gholami O. Effect of a reminder system using an automated short message service on medication adherence following acute coronary syndrome. Eur J Cardiovasc Nurs. 2014 doi: 10.1177/1474515114521910. [Epub ahead of print] PubMed PMID: 24491349. [DOI] [PubMed] [Google Scholar]
- 24.Vervloet M, Linn AJ, van Weert JC, de Bakker DH, Bouvy ML, van Dijk L. The effectiveness of interventions using electronic reminders to improve adherence to chronic medication: A systematic review of the literature. J Am Med Inform Assoc. 2012;19:696–704. doi: 10.1136/amiajnl-2011-000748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bobrow K, Brennan T, Springer D, Levitt NS, Rayner B, Namane M, et al. Efficacy of a text messaging (SMS) based intervention for adults with hypertension: Protocol for the StAR (SMS Text-message Adherence suppoRt trial) randomised controlled trial. BMC Public Health. 2014;14:28. doi: 10.1186/1471-2458-14-28. [DOI] [PMC free article] [PubMed] [Google Scholar]


