Abstract
Background:
Incidence rates of Meniere's disease vary considerably from 157/100,000 in the United Kingdom to 15/100,000 in the United States. Furthermore, in Iran prevalence of Meniere's disease is high, whereas we have not a reliable statistical study on it. A wide range of treatments are used for the treatment of the condition with no consensus on the most effective intervention. The aim of the present study, which involved 37 patients treated because of severe vertigo due to persistent Meniere's disease from 1996 to 2011, was to compare the effectiveness of two surgical methods cochleosacculotomy and endolymphatic sac decompression on vertigo and tinnitus.
Materials and Methods:
In a cross-sectional study, we compared two surgical approaches in patients with Meniere's disease who did not respond to usual medical treatment. Twenty-three patients underwent cochleosacculotomy surgery and 14 patients endolymphatic sac decompression surgery. We compared all the patients for resolving of vertigo, tinnitus.
Results:
After surgery, in patients of both group vertigo was improved significantly (P < 0.0001), tinnitus was improved, but it was not significant (P > 0.05) and hearing level was worse than before (especially in patients who had undergone cochleosacculotomy) (P < 0.0001).
Conclusion:
Based on the data of the current study, cochleosacculotomy and endolymphatic sac decompression improved vertigo in patients with persistent Meniere's disease.
Keywords: Cochleosacculotomy, endolymphatic sac decompression, Meniere's disease
INTRODUCTION
Meniere's disease (idiopathic endolymphatic hydrops) is a disorder of inner ear that present with spontaneous and episodic attacks of vertigo; tinnitus; a sensorineural hearing loss which usually fluctuates; and sensation of aural fullness.[1] It is one of the most common causes of otologic dizziness.[2] Although the peak age of presentation of Meniere's disease is between 40 and 60 years old, it can present at any age including the very young and the elderly. Causes of Meniere's disease are unknown although some cases are secondary to infections, trauma, metabolic disorders, autoimmune disorders, medications, or endocrine disorders. Medical therapy is affected on both the acute attacks, as well as preventing future attacks and typically involves salt restriction, steroids, and diuretics. For acute symptoms, short-term use of intramuscular or intravenous benzodiazepines, as well as anti-nausea medications may also be helpful. In some cases of Meniere's disease where medical management and lifestyle adjustments have not been adequate, surgical therapy is usually reserved. The most common procedures for Meniere's disease include labyrinthectomy, endolymphatic sac decompression, cochleosacculotomy, vestibular nerve section and intratympanic injection of medications such as steroids or antibiotics.[3] Attacks of vertigo were relieved by endolymphatic sac shunt or decompression procedure, in one-half to two-thirds of cases. There was no improvement of hearing in endolymphatic sac surgery procedure and has a small risk of worsening. Recovery time after this procedure is short compared to the other procedures.[4] Cochleosacculotomy is a method of vestibular surgery, performed through the round window to create a shunt between the cochlear duct and the saccule causes both damage of hearing and vestibular parts. In Endolymphatic sac shunt surgery, result showed a higher percentage of patients attained complete vertigo control/hearing preservation.[5]
Studies suggest that there is no coherent study about surgery methods on patients afflicted by Meniere's disease in Iran. Therefore, we decided to perform a study and investigate the result of vestibular system surgery in persistent Meniere's disease.
MATERIALS AND METHODS
This cross-sectional study was conducted in ear, nose, and throat (ENT) wards of hospitals in Isfahan, Iran. All the patients involved in the study were given medical treatment because of severe vertigo due to persistent Meniere's disease, and failure to the medical treatment they were a candidate for surgery. Diagnostic criteria's for Meniere's disease were hearing loss, true vertigo and tinnitus for more than 24 h. All patients had undergone surgery by one of the cochleosacculotomy, and endolymphatic sac decompression were compared in aspects of vertigo, tinnitus from 1996 to 2011. Patients with neurological disorders were excluded, and 37 patients were finally evaluated. Before the surgery, the preoperative information including surgery method, vertigo, tinnitus, smoking, and hearing were extracted from the patient's medical file then the survey were conducted. After the surgery, the postoperative information was gathered from patients by an ENT specialist and his assistant by examination. Afterward, an audiologist examined the patient's hearing, and they were categorized in four groups, mild, moderate, severe and profound. For determining the degree of hearing, we applied standard tests such as speech discrimination score, pure tone audiometry, and speech recognition test. The patient's degree of hearing examined between frequencies from 125 to 8000 Hz. Suggested frequencies by American Association of Head and Neck Surgery includes 500, 1000, 2000, 3000 Hz. Finally, all the collected data's were analyzed statistical by SPSS software version 22, IBM, USA, and standard test of significance (Chi-square, t-test, Mann–Whitney U-test, Wilcoxon, P < 0.05) were used.
RESULTS
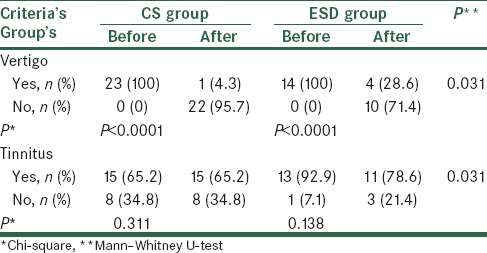
A total of 37 patients were examined in this study. Twenty-three patients (62.2%) underwent cochleosacculotomy surgery, and the other 14 patients (37.8%) underwent the endolymohatic sac decompression surgery. No significant difference was detected in regards of age, sex, and smoking (P > 0.05) between both groups [Table 1]. All 37 patients suffered from the vertigo before the surgery. After the operation, we discovered that vertigo improved in 22 patients of cochleosacculotomy group (95.7%) and 10 patients of endolymphatic sac decompression group (71.4%). These results obviously depicts that improvement of vertigo is significant in both groups (P < 0.0001) and the vertigo improvement was significantly greater in cochleosacculotomy compare to endolymphatic sac decompression (P = 0.031) [Table 2]. According to Table 2, 15 patients who had undergone cochleosacculotomy (14.3%) and 13 patients who had undergone endolymphatic sac decompression (92.9%) were afflicted by tinnitus before the surgery, however, in the decompression group, 2 patients (14.3%) improved, whereas 3 patients (21.4%) suffered from tinnitus after the surgery. Therefore, tinnitus decrease was not significant in both groups (P > 0.05). In addition tinnitus improvement was noticeable in decompression group in compression with cochleosacculotomy, but not statistically significant (P = 0.214).
Table 1.
Comparison of age, sex, and smoking between two groups
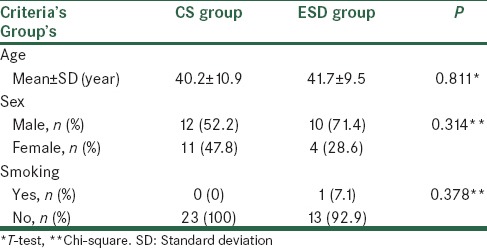
Table 2.
Comparison of vertigo and tinnitus before and postsurgery
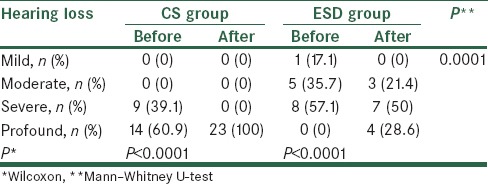
Prior to surgery in patients who had undergone cochleosacculotomy the hearing was severe in 9 patients (39.1%), profound in 14 ones (60.9%), and none of them were mild or moderate. After the surgery, the patients hearing had been decreased in such way which all of them were in the profound group. This decreasing in hearing was significant (P < 0.0001).
In decompression group before the surgery, the patients hearing was mild in one person (7.1%), moderate in 5 patients (35.7%), severe in 8 persons (57.1%) and none of them were profound. After the surgery, the patients hearing was moderate in 3 persons (21.4%), severe in 7 persons (50%) and in 4 persons (28.6%) was profound. These results evidently recommend a significant decrease in hearing in this group (P < 0.0001) [Table 3].
Table 3.
Comparison of hearing before and after surgery
DISCUSSION
Investigating through the previous surveys indicates that there are not enough studies over the comparison between cochleosacculotomy and endolymphatic sac decompression methods. Our results implicated that vertigo improved in both groups significantly.
Giddings et al. stated long-term control of vertigo was poor, and more than 80% of the patients suffered a significant hearing loss after cochleosacculotomy.[6] According to 10 years studies over endolymphatic sac surgery, Convert et al. reported that vertigo recovered in 64.5% and the hearing power got better in 14.8%.[7] Hu A and his colleague, Teufert KB and his colleague and Heidenreich KD et al. stated that cochleosacculotomy gives results comparable with other nondestructive surgical procedures performed to suppress vertigo in Meniere's syndrome.[8,9,10] Goto et al. Kim et al. studies show that vertigo improved after the endolymphatic sac decompression.[11,12]
In addition, our study reminds that vertigo improvement were more noticeable in cochleosacculotomy group in comparison with decompression group.
The tinnitus decreased, but not significantly in both groups; probably it is due to a number of study different results gained in other studies with more participants. For example, Berlinger studied 111 patients who had undergone endolymphatic sac decompression, and Albera et al. 173 patients who had undergone labyrinthectomy (gold standard destructive method in Meniere's disease) and they concluded that tinnitus decreased.[13,14]
Before the surgery, the hearing of patients who had undergone cochleosacculotomy was just in two severe (39.1%) and profound (60.9%) levels, however, more than half of the all patients who had undergone decompression were in severe level (57.1%). After the surgery, we found that, the hearing of all cochleosacculotomy group was profound, but 78.6% of patients of decompression group were in severe and profound levels, it means that hearing significantly decreased. In Dionne and Kinney studies, the hearing got worse after cochleosacculotomy, but montandon believes that hearing did not have worsened after this method.[14,15]
Our results showed that hearing loss in cochleosacculotomy was significantly more noticeable than decompression group which could be due to surgical technique.
CONCLUSION
According to results of the current study, both cochleosacculotomy and endolymphatic sac decompression methods were effective on vertigo improvement with noticeable effects on tinnitus. However, more studies are required in order to determine precious expressions about the treatment of persistent Meniere's disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Crane BT, Schessel DA, Nedzelski J, Minor LB. Peripheral vestibular disorders. In: Flint PW, Haughey BH, Lund VJ, Niparko JK, Richardson MA, Robbins KT, et al., editors. Cummings Otolaryngology Head and Neck Surgery. 5th ed. Philadelphia: Mosby; 2010. pp. 2328–45. [Google Scholar]
- 2.Wetmore SJ. Endolymphatic sac surgery for Ménière's disease: Long-term results after primary and revision surgery. Arch Otolaryngol Head Neck Surg. 2008;134:1144–8. doi: 10.1001/archotol.134.11.1144. [DOI] [PubMed] [Google Scholar]
- 3.Morris BS. Meniere's disease: A common disorder in outpatient clinic. Proceedings of UCLA Healthcare. 2014;18:1–3. [Google Scholar]
- 4.Kitahara T, Horii A, Imai T, Ohta Y, Morihana T, Inohara H, et al. Effects of endolymphatic sac decompression surgery on vertigo and hearing in patients with bilateral Ménière's disease. Otol Neurotol. 2014;35:1852–7. doi: 10.1097/MAO.0000000000000469. [DOI] [PubMed] [Google Scholar]
- 5.Derebery MJ, Fisher LM, Berliner K, Chung J, Green K. Outcomes of endolymphatic shunt surgery for Ménière's disease: Comparison with intratympanic gentamicin on vertigo control and hearing loss. Otol Neurotol. 2010;31:649–55. doi: 10.1097/MAO.0b013e3181dd13ac. [DOI] [PubMed] [Google Scholar]
- 6.Giddings NA, Shelton C, O’Leary MJ, Brackmann DE. Cochleosacculotomy revisited. Long-term results poorer than expected. Arch Otolaryngol Head Neck Surg. 1991;117:1150–2. doi: 10.1001/archotol.1991.01870220098017. [DOI] [PubMed] [Google Scholar]
- 7.Convert C, Franco-Vidal V, Bebear JP, Darrouzet V. Outcome-based assessment of endolymphatic sac decompression for Ménière's disease using the Ménière's disease outcome questionnaire: A review of 90 patients. Otol Neurotol. 2006;27:687–96. doi: 10.1097/01.mao.0000227661.52760.f1. [DOI] [PubMed] [Google Scholar]
- 8.Hu A, Parnes LS. 10-year review of endolymphatic sac surgery for intractable meniere disease. J Otolaryngol Head Neck Surg. 2010;39:415–21. [PubMed] [Google Scholar]
- 9.Teufert KB, Doherty J. Endolymphatic sac shunt, labyrinthectomy, and vestibular nerve section in Meniere's disease. Otolaryngol Clin North Am. 2010;43:1091–111. doi: 10.1016/j.otc.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 10.Heidenreich KD, Basura GJ, Zwolan TA, El-Kashlan HK, Telian SA. Transcanal labyrinthectomy for intractable vertigo after unilateral cochlear implantation. Otol Neurotol. 2011;32:1270–2. doi: 10.1097/MAO.0b013e31822e0e73. [DOI] [PubMed] [Google Scholar]
- 11.Goto F, Tsutsumi T, Ogawa K. Lateral semicircular canal plugging with endolymphatic sac decompression as new surgical treatment for intractable Meniere's disease. Acta Otolaryngol. 2012;132:893–5. doi: 10.3109/00016489.2012.663932. [DOI] [PubMed] [Google Scholar]
- 12.Kim SH, Ko SH, Ahn SH, Hong JM, Lee WS. Significance of the development of the inner ear third window effect after endolymphatic sac surgery in Ménière disease patients. Laryngoscope. 2012;122:1838–43. doi: 10.1002/lary.23332. [DOI] [PubMed] [Google Scholar]
- 13.Berlinger NT. Meniere's disease: New concepts, new treatments. Minn Med. 2011;94:33–6. [PubMed] [Google Scholar]
- 14.Albera R, Canale A, Parandero F, Ducati A, Lanotte M. Surgical indication in Menière's disease therapy: Clinical and epidemiological aspects. Eur Arch Otorhinolaryngol. 2011;268:967–72. doi: 10.1007/s00405-011-1490-5. [DOI] [PubMed] [Google Scholar]
- 15.Syed I, Aldren C. Meniere's disease: An evidence based approach to assessment and management. Int J Clin Pract. 2012;66:166–70. doi: 10.1111/j.1742-1241.2011.02842.x. [DOI] [PubMed] [Google Scholar]


