Abstract
Vitamin D may have an important role in pain perception. Inadequate vitamin D levels are associated with suboptimal recovery after surgery. However, the effects of hypovitaminosis D on postoperative pain-related outcomes and its impact on health-related quality of life after surgery are not well understood. The objective of this study was to determine the effects of hypovitaminosis D on postoperative pain-related outcomes and health-related quality of life at 3 months after knee arthroplasty.
This was a longitudinal cohort study of 191 consecutive Hong Kong Chinese patients who were given patient-controlled morphine analgesia for up to 72 hours after 214 knee arthroplasties. Serum total 25-hydroxyvitamin D (25-OHD) concentration was assessed by liquid chromatography-tandem mass spectrometry. The primary outcomes were postoperative pain intensity at rest scores (0–72 h), Western Ontario and McMaster Universities (WOMAC) osteoarthritis index (pain, stiffness and function), and moderate-to-severe persistent pain (transformed WOMAC pain score of 0–75 at 3 months after knee arthroplasty; 0, extreme pain; 100, no pain). Group differences were analyzed using generalized estimating equation models and a logistic regression model.
The prevalence of preoperative hypovitaminosis D (25-OHD <50 nmol/L) was 44% (95% confidence interval [CI]: 37%–51%). There were transient higher pain intensity scores in the moderate-to-severe hypovitaminosis D (25-OHD <30 nmol/L) group compared with the sufficient vitamin D group. Vitamin D status had no effect on total WOMAC index (P = 0.22). The incidence of moderate-to-severe persistent pain was 9% (95% CI: 6%–14%). Hypovitaminosis D increased the risk of moderate-to-severe persistent pain (adjusted odds ratio 2.64, 95% CI: 1.03–6.77).
Preoperative hypovitaminosis D had subtle effects on pain intensity scores in the early postoperative period and is a risk factor for moderate-to-severe persistent pain after knee arthroplasty. Hypovitaminosis D was not associated with worse health-related quality of life at 3 months after knee arthroplasty.
INTRODUCTION
Adequate cutaneous and dietary vitamin D levels are necessary for optimal health.1 Inadequate exposure to sunlight from sedentary lifestyle, rapid urbanization and high air pollution, and a low vitamin D Chinese diet have contributed to a high prevalence (63%) of vitamin D insufficiency in elderly subjects living in Hong Kong (latitude 22.3 N).2
Vitamin D may have an important role in pain perception and propagation due to its anti-inflammatory and immune-modulatory effects.3 Although the causal role of low vitamin D on pain due to osteomalacia is well recognized,4 the combination of surgery and hypovitaminosis D may be deleterious.3,5 Several studies have shown an association between hypovitaminosis D and suboptimal functional recovery after joint arthroplasty,6–8 perhaps due to acute reductions in 25-hydroxyvitamin D (25-OHD) concentration after surgery (40% in the first 12 hours and 20% at 3 months compared with preoperative baseline).9 Furthermore, as serum interleukin-6 (pro-inflammatory and pro-nociceptive cytokine) was elevated during the first week after knee arthroplasty,10 patients may have enhanced pain sensitivity.11
The effects of hypovitaminosis D on postoperative pain-related outcomes and its impact on health-related quality of life after knee arthroplasty are not well understood. We hypothesized that hypovitaminosis D was associated with worse pain-related outcomes and health-related quality of life. This prospective cohort study examined the effects of hypovitaminosis D on early postoperative pain-related outcomes, health-related quality of life, and risk of moderate-to-severe persistent pain at 3 months after knee arthroplasty.
METHODS
Study Design, Setting and Participants
Ethical approval for this cohort study (CRE-2010.505) was provided by The Joint Chinese University of Hong Kong-New Territories East Cluster Clinical Research Ethics Committee, Hong Kong, on 7 December 2010. All patients gave written informed consent before surgery for participation in the study and were followed-up by telephone interview at 3 months after surgery.
We recruited consecutive patients from November 2011 to January 2014 undergoing general anesthesia or regional anesthesia for major elective primary or revision of knee arthroplasty who were expected to be given patient controlled morphine analgesia after surgery (we had initially included 25 patients undergoing 31 hip arthroplasty in the funded study but anonymous peer reviewers recommended that the analyses to be restricted to knee arthroplasty population for clearer interpretation of the results). Exclusion criteria included subjects under 18 years, contraindications to intravenous morphine patient-controlled analgesia, pre-existing comorbidities (serum creatinine >150 nmol/L or other renal diseases, liver function impairment, hepatitis or liver cirrhosis, chronic pancreatitis, history of gastric or small-bowel resection, inflammatory bowel disease, neurological disorder) and medications’ use (anticonvulsants, glucocorticoids, and antiretrovirals). Using a standardized questionnaire, we collected demographic, pre-existing comorbidities, smoking status, pain medications used at home, regular use of vitamin D supplements, and the amount of sun exposure time in the last week.
Preoperative Anesthesia Management
Patients undergoing general anesthesia were induced with propofol 2 mg/kg, fentanyl 1 μg/kg, a nondepolarizing neuromuscular blocker, endotracheal intubation, and maintained with isoflurane 1% to 2% in 40% oxygen/air mixture. Intravenous morphine 0.1 mg/kg was given to the patient after induction of anesthesia approximately 5 minutes before skin incision. Supplementary analgesia was achieved with fentanyl 10 μg bolus at the discretion of the duty anesthesiologist. For spinal anesthesia, the lumbar puncture was performed using a 25G pencil-point spinal needle to the L2/3 or L3/4 level. Heavy bupivacaine 0.5% 2.6 mL together with fentanyl 25 μg was injected into the subarchnoid space. In the post-anesthesia care unit (PACU), all patients received an intravenous patient controlled analgesia (IVPCA) with morphine (Graseby 2200 pump) 1 mg bolus, lockout time of 5 minutes and a 4-hour dose limit of 0.3 mg/kg for up to 72 h. The nurse-based, anesthesiologist-led Acute Pain Service team monitored the postoperative pain management of patients daily.
Vitamin D Analyses
Preoperative fasting serum 25-OHD concentration was measured using a liquid chromatography-tandem mass spectrometry, with limits of detection of 10.0 nmol/L and an inter-assay coefficient of variation of ≤6.5%.12 Hypovitaminosis D was defined as severe (<12.5 nmol/L), moderate (12.5–29 nmol/L), mild (30–49 nmol/L) and sufficient as 50 to 220 nmol/L.13 As the results were available to clinical and research staff 7 days after sample collection, the outcome assessments collected at 72 hours were unlikely to be biased.
Outcome Assessments
The pain intensity at rest was measured at hourly intervals for first 12 hours, 4 to 6 hourly thereafter for up to 72 hours after surgery by ward nurses as routine practice using a numeric analogue scale from 0 (no pain) to 10 (worst imaginable pain). We also measured the cumulative morphine consumption up to 72 hours recorded by the patient-controlled analgesia device.
Self-reported level of pain relief was measured daily using a 5-point Likert scale that ranged from 0 (none) to 4 (complete) during the first 3 days after surgery. For each patient, the area under the pain relief curve (TOTPAR) was calculated and then a percentage of the maximum TOTPAR estimated.14 A dichotomous descriptor of at least >50% maximum TOTPAR represented a clinically meaningful outcome of adequate pain relief.14
During the first 3 days after knee arthroplasty, we measured the patient's health status after surgery and anesthesia daily using a reliable and validated Chinese version15 of a 9-item Quality of Recovery (QoR) questionnaire.16 The score ranges from 0 to 18, with higher scores representing better recovery.
General health-related quality of life was measured before surgery, on the third day and third month after surgery using the Chinese (Hong Kong) version of the European Quality of Life-5 Dimensions (EQ-5D).17 Patients were also asked to rate how good or bad their health state was on a visual analogue scale from 0 (worst imaginable) to 100 (best imaginable).17 The EQ-5D index, a preference/utility-based measure, was estimated using the descriptive responses and applying the US set of reference weights.18
The Chinese version of the Western Ontario and McMaster Universities (WOMAC) osteoarthritis index, a valid and reliable instrument, was used to measure health status in patients with osteoarthritis of the knee before and at three months after surgery.19 The 24-item WOMAC questionnaire has three subscales: pain (5 items with subtotal score ranging from 0 to 20), stiffness (2 items with subtotal score ranging from 0 to 8), and function (17 items with subtotal score ranging from 0 to 68). The subtotal and overall WOMAC index scores were calculated and transformed to range from 0 to 100, with higher scores indicating better health status. Moderate-to-severe persistent pain was defined as a WOMAC pain score of 0 to 75 at 3 months after knee arthroplasty.20
Statistical Analysis
Independent sample Kruskal-Wallis test was used to compare the age, duration of anesthesia, duration of PACU stay, duration of IVPCA, cumulative morphine dose, and length of hospital stay between vitamin D status groups. Otherwise, χ2 tests were used to compare perioperative characteristics between 25-OHD groups. Listwise deletion was used to deal with missing completely at random follow-up data.
The primary outcomes were pain intensity, WOMAC index, and moderate-to-severe persistent pain. Changes in outcome measures over time were analyzed with the use of generalized estimating equation population averaged models,21 with treatment and time as fixed effects adjusting for covariates selected on the basis of a causal directed acyclic graph approach.22 In the generalized estimating equation models, we used an exchangeable correlation structure and adjusted for seasonal variations in 25-OHD concentration, and for patients who may have had staged bilateral knee arthroplasty. The effect of vitamin D status on outcome was captured by the time-exposure interaction and Wald tests were used to test for the significance of this. A logistic regression was used to determine the risk of moderate-to-severe persistent pain associated with hypovitaminosis D, taking into account staged bilateral knee arthroplasty that 23 patients had. The odds ratio (OR) and 95% confidence interval (95% CI) were reported. The area under the receiver-operating characteristic curve (AUROC) and the Hosmer-Lemeshow (HL) goodness-of-fit test were estimated to assess the model discrimination and calibration performance, respectively. All analyses were performed using STATA 13.1 (StataCorp, College Station, TX).
Using PASS 11 software (NCSS, Kaysville, UT), a logistic regression of moderate-to-severe persistent pain on hypovitaminosis D (assumed local prevalence of hypovitaminosis D at 23%)2 with a sample size of 214 will achieve 80% power at a 5% significance level to detect a change corresponding to an odds ratio of 2.50 (risk from 32%20 to 54%).
RESULTS
Of 248 patients screened, 206 patients were recruited but 15 did not get IVPCA with morphine for postoperative pain management, leaving 191 patients undergoing 214 knee arthroplasty for analysis (Fig. 1). As 1 patient had postoperative cardiac complications, no QoR and EQ-5D assessments were available on the third day after surgery. Two patients were lost to follow-up at 3 months after surgery (Fig. 1).
FIGURE 1.

Flow of participants in the cohort study.
The preoperative prevalence of mild and moderate-to-severe hypovitaminosis D were 36.4% (95% CI 30.0%–43.3%) and 7.5% (95% CI 4.3%–11.9%), respectively. The preoperative characteristics, duration of anesthesia, PACU stay, and duration of IVPCA were similar between vitamin D status groups (Table 1). None of the patients reported chronic opioid use before surgery.
TABLE 1.
Characteristics of 191 Patients Undergoing 214 Knee Arthroplasty By Serum 25-OHD Concentration∗

Although there was no significant vitamin D status group-time interaction effect (P = 0.47) after adjusting for age, sex, obesity (BMI ≥30), current smoking, type of anesthesia and season, there was a significant difference between vitamin D status group (P < 0.01) in Figure 2. On arrival to the ward and during the first hour, the moderate-to-severe hypovitaminosis D group had higher pain scores (mean difference [MD] 1.4, 95% CI: 0.4–2.4 and 1.0, 95% CI: 0.1–2.0, respectively) than the sufficient vitamin D group (P < 0.01 and P = 0.03, respectively). Between the 7th and 10th hour, the moderate-to-severe hypovitaminosis D group had higher pain scores than the sufficient vitamin D group (Fig. 2), but otherwise, there was no difference at other times. The pain intensity scores were relatively similar at all times, except between 2nd and 4th hour, between mild hypovitaminosis D and sufficient vitamin D groups (Fig. 2). After adjusting for age, sex, maximum TOTPAR, type of anesthesia, and season, there was no significant difference between vitamin D status groups for mean cumulative morphine consumption (P = 0.12). Patients with sufficient vitamin D levels required 35 mg (95% CI 31–39) of morphine for pain relief, whereas those with mild and moderate-to-severe hypovitaminosis D groups required 39 mg (95% CI 33–44) and 46 mg (95% CI 35–58), respectively.
FIGURE 2.
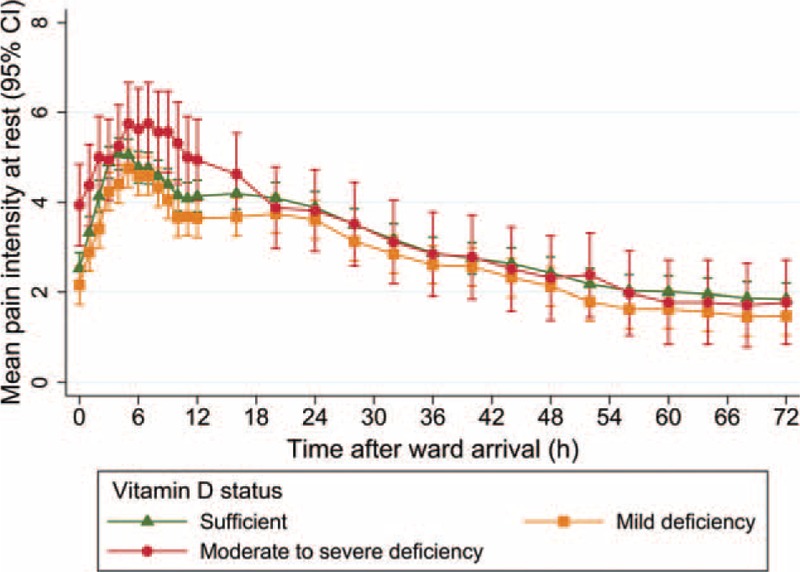
Comparison of mean (95% confidence interval) pain intensity at rest scores over time by vitamin D status groups. Green triangle represents sufficient 25-OHD levels (50–220 nmol/L), orange square represents mild deficiency (30–49 nmol/L), and red circle represents moderate-to-severe deficiency (<30 nmol/L).
The baseline estimates and the mean change over 3 days for QoR scores, and mean change over 3 months for EQ-5D and WOMAC outcomes are shown in Table 2. There was a vitamin D status-time interaction on EQ-5D VAS (P = 0.02, Fig. 3) but not for EQ-5D index (Table 2). There was no effect of vitamin D status on total WOMAC index, WOMAC pain, and stiffness subscales (Table 2). The effect of vitamin D status groups on WOMAC function was marginally significant (P = 0.07); preoperative WOMAC function was lowest in the moderate-to-severe hypovitaminosis D group compared with the sufficient vitamin D group (MD −13.1, 95% CI −24.1 to −2.0) but was associated with the largest improvements over time (Table 2).
TABLE 2.
Mean (95% Confidence Interval) Baseline Values and Changes Over Time By Patient-Centered Outcomes
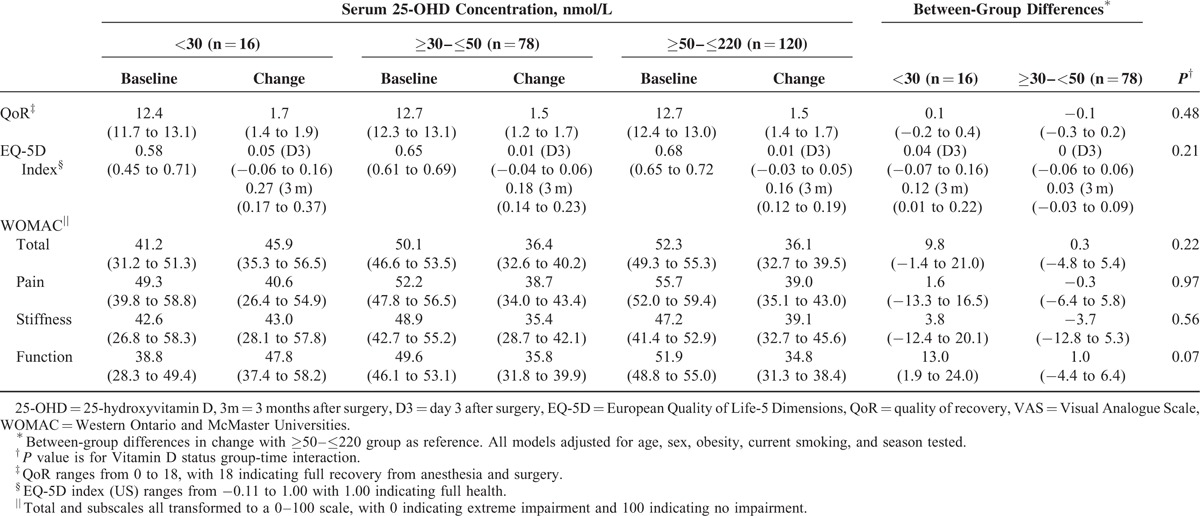
FIGURE 3.
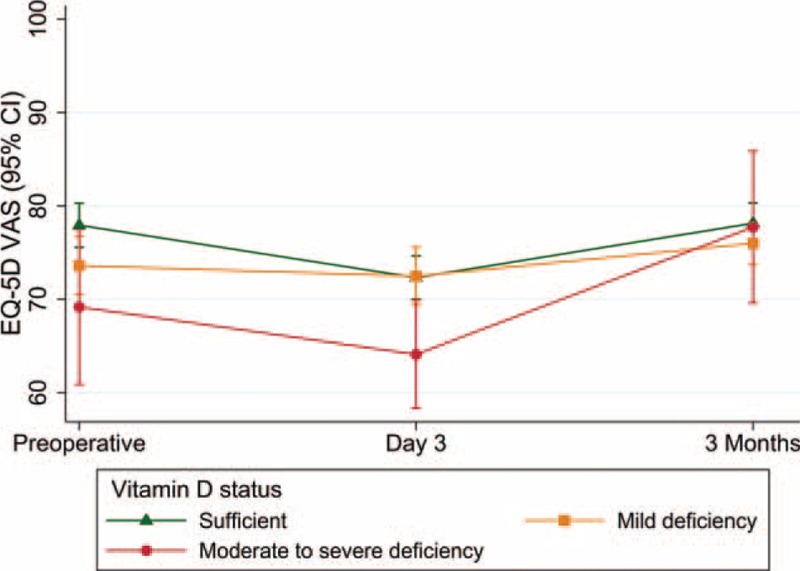
Comparison of mean (95% confidence interval) EQ-5D visual analogue score over time by vitamin D status groups. Green triangle represents sufficient 25-OHD levels (50–220 nmol/L), orange square represents mild deficiency (30–49 nmol/L), and red circle represents moderate-to-severe deficiency (<30 nmol/L).
The prevalence of preoperative moderate-to-severe pain was 79.9% (95% CI 73.9–85.1). There was no association between preoperative hypovitaminosis D (25-OHD <50 nmol/L) and the risk of preoperative moderate-to-severe pain (OR 1.60, 95% CI 0.80–3.21, P = 0.18). At 3-month follow-up, 72 (34%), 14 (6.6%) and 6 (2.8%) patients reported mild, moderate, and severe persistent pain. The incidence of moderate-to-severe persistent pain was 9.3% (95% CI 5.9–14.2), with a median WOMAC Pain score of 65 (interquartile range [IQR] 46–74) in this group. Compared with patients without pain or mild persistent pain, those with moderate-to-severe persistent pain had lower median (IQR) WOMAC stiffness (100 [75–100] vs 75 [50–100]) (P = 0.001) and WOMAC function (91 [82–97] vs 62 [50–69]) (P < 0.001).
Patients with preoperative hypovitaminosis D seemed more likely to develop moderate-to-severe persistent pain after surgery (13.8%) than patients with normal preoperative 25-OHD concentration (5.9%) (P = 0.05). After adjusting for age, sex, obesity, type of anesthesia, preoperative moderate-to-severe pain, and season, there was evidence supporting the association between hypovitaminosis D and risk of moderate-to-severe persistent pain (OR 2.64, 95% CI 1.03–6.77, P = 0.04). The model calibration was adequate (HL test P = 0.82) and discrimination was acceptable (AUROC 0.74, 95% CI 0.64–0.84).
DISCUSSION
In this prospective cohort of Hong Kong Chinese patients undergoing knee arthroplasty, nearly half had preoperative hypovitaminosis D, higher than other studies using the same cutoff at 50 nmol/L.6,23,24 The effects of hypovitaminosis D on pain outcomes and short-term health-related quality of life outcomes were mixed. Moderate-to-severe hypovitaminosis D was associated with transient higher pain intensity at rest scores without affecting the total morphine consumption or the quality of recovery after surgery. Although moderate-to-severe hypovitaminosis D patients had a lower preoperative health-related quality of life, we found clinically important improvements in EQ-5D VAS and index, total WOMAC index, and subdomains over time, with values at 3 months comparable with those in the sufficient vitamin D group. Our regression analysis suggested a 2- to 3-fold increased risk of moderate-to-severe persistent pain with hypovitaminosis D.
We found a clinically important transient difference in pain intensity at rest scores associated with moderate-to-severe hypovitaminosis D in the early postoperative period on the ward. Otherwise, there was no evidence that patients with hypovitaminosis D had higher morphine requirements or inadequate pain relief than patients with sufficient vitamin D levels during the first 3 days after surgery. In a retrospective review of medical records from 185 patients undergoing laparoscopic bariatric surgery, there was no association between vitamin D deficiency and increased opioid requirements.3
The improvements in WOMAC domains after arthroplasty within each vitamin D status group exceeded the minimal clinically important difference of 14 to 22 (on 0–100 point scale) for knee arthroplasty.25 Among the improvements between 25-OHD groups, the moderate-to-severe hypovitaminosis D group showed a significant improvement in function after having the lowest preoperative function score, with accompanying clinically important improvements in the EQ-5D VAS and index scores. This is consistent with previous findings26 wherein patients reported relatively larger improvements in knee-related functioning or general health status (according to EQ-5D index) having corresponding improvements in EQ-5D VAS. A possible explanation for patients with poorer baseline health status showing stronger improvements in EQ-5D index and functioning after knee arthroplasty may include a higher likelihood of expectations being fulfilled after experiencing major pain and disability before surgery.26 In contrast, another study showed that moderate-to-severe hypovitaminosis D was associated with less postoperative improvement in WOMAC stiffness at 6 months after knee arthroplasty.6
Moderate-to-severe persistent pain after an elective procedure that is performed to relieve pain can be considered a treatment failure.20 Our incidence of moderate-to-severe persistent pain was substantially lower than a previous study,20 but the overall incidence of persistent pain (mild, moderate, and severe) was similar. The strongest independent predictors of persistent pain after total knee arthroplasty identified in a recent systematic review were catastrophizing, mental health, preoperative knee pain, and pain at other sites.27 Our study suggests that consideration be given to hypovitaminosis D as a risk factor for persistent pain after knee arthroplasty.
Currently, there is no consensus on the definition of vitamin D deficiency or the optimal level of total serum 25-OHD concentration.28 Large seasonal variations in circulating 25-OHD concentration relative to the annual mean concentration has implications for research methodology.29 Estimating the annual mean concentration of 25-OHD from a single value by using a cosinor model reclassified 7% of participants with regards to vitamin D deficiency.29 Therefore, vitamin D status misclassification is a probable threat to our study validity; our adjusted estimate (OR 2.64, 95% CI 1.03–6.77) is likely to be biased toward the null. The generalizability of the results to other settings is limited due to the role of ethnicity, latitude, environmental and lifestyle factors affecting 25-OHD concentrations, as well as the wide variety of anesthetic techniques (eg, local infiltration analgesia, femoral nerve block, epidural analgesia) available for patients undergoing knee arthroplasty.
A recent review highlighted the role of Vitamin D on the etiology and maintenance of chronic pain state.30 Caution is required in attributing the improvements in WOMAC function in the moderate-to-severe hypovitaminosis D group to the use of postoperative vitamin D supplements as we did not measure this and few patients in our study were taking vitamin D supplements of sufficient dose before surgery. Currently, there is no clear benefit associated with the use of vitamin D supplements for chronic pain.31 However, in a preliminary study of chronic pain patients, higher plasma concentration of interleukin-10 (anti-inflammatory and anti-nociceptive cytokine) was associated with decreased pain intensity.32 Hence, attenuating the decrease in serum 25-OHD after knee arthroplasty9 with supplemental vitamin D to modulate the role of cytokines in chronic pain processing seems plausible and warrants further study.
In conclusion, this prospective cohort study in Hong Kong Chinese patients undergoing knee arthroplasty found a high prevalence of preoperative hypovitaminosis D. Moderate-to-severe hypovitaminosis D had subtle effects on pain intensity scores in the early postoperative period but the health-related quality of life outcomes at 3 months were comparable with other patients with a sufficient level of vitamin D concentration. Hypovitaminosis D is likely to be a new risk factor for the development of moderate-to-severe persistent pain after knee arthroplasty.
Acknowledgments
This research work was fully funded by a grant from the Research Grants Council of the Hong Kong Special Administrative Region, China (Project reference: CUHK469411). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Hong Kong Research Grants Council or the Hospital Authority of Hong Kong. The authors have no conflicts of interest to disclose.
Footnotes
Abbreviations: 25-OHD = 25-hydroxyvitamin D, 95% CI = 95% confidence interval, ASA = American Society of Anesthesiologists, AUROC = area under the receiver operating characteristic curve, BMI = body mass index, EQ-5D = European Quality of Life-5 Dimensions, HL = Hosmer-Lemeshow, IQR = interquartile range, IVPCA = intravenous patient-controlled analgesia, MD = mean difference, OR = odds ratio, PACU = postanesthesia care unit, QoR = Quality of Recovery, TOTPAR = area under pain relief curve, WOMAC = Western Ontario and McMaster Universities.
Contributions: AL helped design the study, conduct the study, analyze and interpret the data, and write the manuscript; SKCC and TG helped design the study, analyze and interpret the data, and revised the manuscript for important intellectual content; WS and CHC helped in the acquisition of data and in revising the manuscript for important intellectual content.
Meetings: Part of this work was previously presented at the combined Royal Australasian College of Surgeons Annual Scientific Congress and the Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine Annual Scientific Meeting, in Singapore, 5th-9th May 2014.
The authors report no conflicts of interest.
REFERENCES
- 1.Stechschulte SA, Kirsner RS, Federman DG. Vitamin D: bone and beyond, rationale and recommendations for supplementation. Am J Med 2009; 122:793–802. [DOI] [PubMed] [Google Scholar]
- 2.Wat WZ, Leung JY, Tam S, et al. Prevalence and impact of vitamin D insufficiency in southern Chinese adults. Ann Nutr Metab 2007; 51:59–64. [DOI] [PubMed] [Google Scholar]
- 3.Bose S, Khanna A, You J, et al. Low serum vitamin D levels are not associated with increased postoperative pain and opioid requirements: a historical cohort study. Can J Anaesth 2015; 62:770–776. [DOI] [PubMed] [Google Scholar]
- 4.Straube S, Moore RA, Derry S, et al. Vitamin D and chronic pain. Pain 2009; 141:10–13. [DOI] [PubMed] [Google Scholar]
- 5.Iglar PJ, Hogan KJ. Vitamin D status and surgical outcomes: a systematic review. Patient Saf Surg 2015; 9:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allain TJ, Beresford PA, Newman JH, et al. Vitamin D levels in patients undergoing knee arthroplasty: does vitamin D status effect postoperative outcomes? Eur e-J Clin Nutr Metab 2008; 3:e17–e21. [Google Scholar]
- 7.Nawabi DH, Chin KF, Keen RW, et al. Vitamin D deficiency in patients with osteoarthritis undergoing total hip replacement: a cause for concern? J Bone Joint Surg Br 2010; 92:496–499. [DOI] [PubMed] [Google Scholar]
- 8.Lavernia CJ, Villa JM, Iacobelli DA, et al. Vitamin D insufficiency in patients with THA: prevalence and effects on outcome. Clin Orthop Relat Res 2014; 472:681–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reid D, Toole BJ, Knox S, et al. The relation between acute changes in the systemic inflammatory response and plasma 25-hydroxyvitamin D concentrations after elective knee arthroplasty. Am J Clin Nutr 2011; 93:1006–1011. [DOI] [PubMed] [Google Scholar]
- 10.Kugisaki H, Sonohata M, Komine M, et al. Serum concentrations of interleukin-6 in patients following unilateral versus bilateral total knee arthroplasty. J Orthop Sci 2009; 14:437–442. [DOI] [PubMed] [Google Scholar]
- 11.Lee YC, Lu B, Bathon JM, et al. Pain sensitivity and pain reactivity in osteoarthritis. Arthritis Care Res (Hoboken) 2011; 63:320–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ong L, Saw S, Sahabdeen NB, et al. Current 25-hydroxyvitamin D assays: do they pass the test? Clin Chim Acta 2012; 413:1127–1134. [DOI] [PubMed] [Google Scholar]
- 13.Nowson CA, McGrath JJ, Ebeling PR, et al. Vitamin D and health in adults in Australia and New Zealand: a position statement. Med J Aust 2012; 196:686–687. [DOI] [PubMed] [Google Scholar]
- 14.Moore A, Moore O, McQuay H, et al. Deriving dichotomous outcome measures from continuous data in randomised controlled trials of analgesics: use of pain intensity and visual analogue scales. Pain 1997; 69:311–315. [DOI] [PubMed] [Google Scholar]
- 15.Chan MT, Lo CC, Lok CK, et al. Psychometric testing of the Chinese quality of recovery score. Anesth Analg 2008; 107:1189–1195. [DOI] [PubMed] [Google Scholar]
- 16.Myles PS, Reeves MD, Anderson H, et al. Measurement of quality of recovery in 5672 patients after anaesthesia and surgery. Anaesth Intensive Care 2000; 28:276–280. [DOI] [PubMed] [Google Scholar]
- 17.Brooks R, Rabin R, de Charro F. The measurement and valuation of health status using EQ-5D: a European perspective. Dordrecht: Kluwer Academic Publishers; 2003. [Google Scholar]
- 18.Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care 2005; 43:203–220. [DOI] [PubMed] [Google Scholar]
- 19.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes following total hip or knee arthroplasty in osteoarthritis. J Orthopaed Rheumatol 1988; 1:95–108. [PubMed] [Google Scholar]
- 20.Wylde V, Hewlett S, Learmonth ID, et al. Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain 2011; 152:566–572. [DOI] [PubMed] [Google Scholar]
- 21.Katz MH. Multivariable Analysis: a practical guide for clinicians and public health researchers. 3rd edNew York: Cambridge University Press; 2011. [Google Scholar]
- 22.Shrier I, Platt RW. Reducing bias through directed acyclic graphs. BMC Med Res Methodol 2008; 8:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Unnanuntana A, Saleh A, Nguyen JT, et al. Low Vitamin D Status does not adversely affect short-term functional outcome after total hip arthroplasty. J Arthroplasty 2013; 28:315–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bogunovic L, Kim AD, Beamer BS, et al. Hypovitaminosis D in patients scheduled to undergo orthopaedic surgery: a single-center analysis. J Bone Joint Surg Am 2010; 92:2300–2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Escobar A, Quintana JM, Bilbao A, et al. Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis Cartilage 2007; 15:273–280. [DOI] [PubMed] [Google Scholar]
- 26.Lin FJ, Samp J, Munoz A, et al. Evaluating change using patient-reported outcome measures in knee replacement: the complementary nature of the EQ-5D index and VAS scores. Eur J Health Econ 2014; 15:489–496. [DOI] [PubMed] [Google Scholar]
- 27.Lewis GN, Rice DA, McNair PJ, et al. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth 2015; 114:551–561. [DOI] [PubMed] [Google Scholar]
- 28.LeFevre ML. Screening for Vitamin D Deficiency in Adults: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 2014; 162:133–140. [DOI] [PubMed] [Google Scholar]
- 29.Sachs MC, Shoben A, Levin GP, et al. Estimating mean annual 25-hydroxyvitamin D concentrations from single measurements: the Multi-Ethnic Study of Atherosclerosis. Am J Clin Nutr 2013; 97:1243–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shipton EA, Shipton EE, Vitamin D. Pain: Vitamin D and its role in the aetiology and maintenance of chronic pain states and associated comorbidities. Pain Res Treat 2015; 2015:904967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Straube S, Derry S, Straube C, et al. Vitamin D for the treatment of chronic painful conditions in adults. Cochrane Database Syst Rev 2015; 5:CD007771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zin CS, Nissen LM, O’Callaghan JP, et al. Preliminary study of the plasma and cerebrospinal fluid concentrations of IL-6 and IL-10 in patients with chronic pain receiving intrathecal opioid infusions by chronically implanted pump for pain management. Pain Med 2010; 11:550–561. [DOI] [PubMed] [Google Scholar]


