Abstract
A history of sexual assault (SA) is often associated with increased distress and heavy drinking. One’s ability to cope with the distress and seek social support has been associated with drinking more generally. However, SA-related distress, drinking, and the extent to which a woman engages in adaptive coping or seeks social support is known to vary day-to-day. The goal of the present investigation was to examine the moderating influence of perceived coping control and social support on the event-level association between SA-related distress and drinking. This study included 133 college women with a history of SA who reported recent heavy drinking. Participants provided daily reports of their SA-related distress, perceived coping control, perceived social support, and alcohol consumption every day for 30-days. Results of generalized estimating equation models suggest that coping control moderated the association between distress and drinking such that those with less perceived coping control drank more as their SA-related distress increased from their average. Although social support did not moderate between distress and drinking, decreases in perceived social support were associated with more drinking on that day. Results suggest that daily deviations in SA-related distress may influence alcohol consumption more than average levels of distress, especially among women with low coping control. Interventions for women with SA histories should help them build coping skills as well as adequate social support in order to reduce drinking.
Keywords: sexual assault, distress, drinking, coping behavior, social support
1. Introduction
Sexual assault (SA) and heavy alcohol use are significant public health concerns among college women. Studies suggest that 50% of college women have experienced some form of sexual aggression, with 12–28% of these women reporting attempted or completed forced sexual intercourse since the age of 14 (Abbey, Ross, McDuffie, & McAuslan, 1996; Brener, McMahon, Warren, & Douglas, 1999; Walsh et al., 2012). An assessment of SA among college women suggested that 27% had experienced some form of SA since enrolling in college (Gross, Winslett, Roberts, & Gohm, 2006). SA has been associated with elevated drinking rates. For example, freshmen women with SA were more likely to report drinking and in particular heavy episodic drinking (i.e., consuming 4 or more drinks within 2 hours) than freshmen women with no SA (Ross et al., 2011). Further, sexual assault can result in increased distress including symptoms of posttraumatic stress disorder (PTSD; Messman-Moore, Long, & Siegfried, 2000), which in turn is also associated with increased drinking and alcohol-related problems (Hruska & Delahanty, 2012; Messman-Moore, Ward, & Brown, 2009; Read, Ouimette, White, Colder, & Farrow, 2011).
The use and success of coping strategies implemented in response to post-assault distress may play an important role in survivors’ psychological adjustment and alcohol use following SA. Engagement in avoidant coping, such as denial, self-distraction, self-blame, problem avoidance, social withdrawal, and behavioral disengagement, has generally been associated with greater distress (e.g., Bedard-Gilligan, Cronce, Lehavot, Blayney, & Kaysen, 2014; Frazier, Mortensen, & Steward, 2005; Ullman, 1996; Ullman, Townsend, Filipas, & Starzynski, 2007; Ullman & Peter-Hagene, 2014; Valentiner, Foa, Riggs, & Gershuny, 1996) among SA survivors. Avoidance behaviors may lead to withdrawal from support networks (Ullman et al., 2007) and have been associated with reduced perceptions of control (Frazier et al., 2005), thereby potentially compounding negative affect and leading to increased alcohol use. The use of approach-oriented coping strategies following SA, such as joining a support group, seeking mental health services, and emotional expression, has been associated with improved outcomes (e.g., Ullman, 1996; Frazier, et. al., 2005). However, more recent conceptualizations of coping emphasize the importance of situational factors that influence an individuals’ use and success of specific coping strategies such as interpersonal and social resources (Skinner, Edge, Altman & Sherwood, 2003) and the availability and quality of social support (Ullman, 1996; Ullman et al., 2007; Ullman & Peter-Hagene, 2014).
Few studies have examined the role of coping in daily use of alcohol to reduce event-level SA-related distress; however avoidant coping efforts have been implicated in the comorbidity between PTSD symptoms and alcohol use disorders generally (Hruska, Fallon, Spoonster, Sledjeski, & Delahanty, 2011). Among a sample of motor vehicle accident survivors, the relationship between avoidant coping and PTSD symptoms was stronger for those with a history of alcohol use disorders (Hruska et al., 2011). Endorsement of drinking to cope was also found to mediate between child sexual abuse and alcohol problems (Grayson & Nolen-Hoeksema, 2005). We are aware of only one study to have examined the role of coping in the link between alcohol use and distress among SA survivors. In this study, findings revealed positive associations between avoidant coping, PTSD symptoms, and sexual assault among a large sample of college women; however, no meaningful associations were found between avoidant coping and alcohol use (Bedard-Gilligan et al., 2014). Accordingly, little is known regarding the use or success of coping in relation to alcohol use and SA-related distress.
Social support is a resource and specific coping strategy that may help to mitigate or buffer distress associated with SA (Coyne & Downey, 1991). For example, disclosure of SA has been associated with receipt of more positive social reactions, which may help to reduce SA-related distress (Ullman & Filipas, 2001). Relationships comprise an important aspect of women’s social development. During ages in which socialization commonly includes alcohol use, such as among college-age women, drinking to cope when emotional support is not available may seem normative. As a result, women with low support from family and friends may turn to drinking in the absence of supportive intimacy (Gleason, 1994). Further, PTSD is associated with social withdrawal and may result in loss of social supports over time (King, Taft, King, Hammond, & Stone, 2006; Laffaye, Cavella, Drescher, & Rosen, 2008; Lansford et al., 2002), which could lead to increases in daily drinking (Mohr et al., 2001). In contrast, women who receive social support may be less likely to drink as the perception that one has received emotional support when needed is likely to attenuate SA-related distress.
The majority of studies evaluating relationships between sexual assault and drinking have utilized cross-sectional methodologies, which cannot assess how SA-related distress and drinking covary in real time. Event-level studies generally suggest that negative affect is associated with alcohol consumption (Armeli, Conner, Cullum, & Tennen, 2010; Armeli, Tennen, Affleck, & Kranzler, 2000; Mohr et al., 2001; Rankin & Maggs, 2006; Simons, Gaher, Oliver, Bush, & Palmer, 2005; Swendsen et al., 2000) and daily reports of stress and negative affect have been associated with increased cravings to drink (Cleveland & Harris, 2010; Oslin, Cary, Slaymaker, Colleran, & Blow, 2009). Fluctuations from daily averages in PTSD symptoms have also been shown to predict daily drinking urges and drinking behavior (Kaysen et al., 2014; Simpson, Stappenbeck, Luterek, Lehavot, & Kaysen, 2014). The relationship between daily level SA-related distress and drinking may vary depending on use of alternative coping or receiving social support. College women tend to cope with distress within their social context and alcohol risks should be assessed in real-time to assess dynamic fluctuations among distress, social support, and drinking (DeLongis & Holtzman, 2005). The inclusion of measures of coping and social support at the event level adds this necessary contextual or temporal specificity.
The present study sought to examine the influence of perceived coping control and social support on the daily association between distress associated with women’s SA experiences and drinking. To our knowledge, no known studies have examined these associations at the event-level, which is needed given the day-to-day variability in the use and success of coping strategies and availability of social support. Understanding these associations at the daily level is critical for intervention development and refinement. This study sought to examine several hypotheses: (H1) Greater SA-related distress will be associated with more drinking on the same day; (H2) Less coping control will be associated with more drinking that same day and will moderate the association between SA distress and drinking such that greater SA distress will be associated with more drinking among those with less coping control; and (H3) Less social support will be associated with more drinking that same day and will moderate the association between distress and drinking such that greater distress will be associated with more drinking for those with less social support.
2. Method
2.1 Participants and Procedures
A total of 11,544 undergraduate women were randomly selected from a registrar list of students attending a large northwest university and were mailed and e-mailed an invitation to complete a 20-minute online screening survey. Of those, 729 completed the screening survey, met study criteria of being 18 years or older, consuming 4 or more drinks on one occasion at least twice in the past month, and reported experiencing sexual victimization (at least one incident of childhood sexual abuse OR adult sexual assault prior to the past three months), and completed a pre-monitoring assessment. In order to be considered eligible for participation, the participants’ reported sexual assault had to have occurred more than three months prior to the screening in order to select a sample of women whose PTSD symptoms had persisted past the point at which natural recovery following trauma was most likely to occur (Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992). Additional information regarding participant recruitment procedures is described in Kaysen et al., 2014. Participants with a history of sexual victimization and at least one intrusive and one hyperarousal PTSD symptom in the past month (n=264) were invited to participate in 30 days of electronic daily dairy assessment, and 136 (51.5%) participated. Of those, 3 were excluded for having significant missing data on the dependent variable (i.e., only 10% or fewer available observations) resulting in a final sample of 133 women.
The mean age for the final sample was 20.1 years old (SD=1.4). Ethnicity included 71.8% White, 11.5% Asian, 2.3% Black, and 14.4% multi-ethnic or other ethnicity. At the time of screening, 12.2% were freshmen, 25.2% sophomores, 37.4% juniors, and 25.2% seniors. A majority of the women had experienced some type of adult sexual victimization (94.0%). These included completed rapes (21.8%), alcohol involved rapes (53.4%), alcohol involved assaults that did not involve penetration (64.7%), and coercive sexual assaults (60.9%). Just under half of the participants (43.6%) experienced child sexual abuse. Over half of the women (57.1%) met diagnostic criteria for PTSD according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV; American Psychiatric Association [APA], 1994).
The daily monitoring portion of the study consisted of two daily assessments, one before noon and one after seven p.m., for 30 days. Each participant received a personal digital assistant (PDA) device. In the training session, participants selected a two-hour period in both the morning and evening to complete assessments. An alarm was set for the start of their assessment window to alert them to complete their surveys. PDA assessments took on average 4 minutes to complete. Participants were paid $45 for screening and pre-monitoring assessments, $1 for each daily assessment completed, a $2 bonus for completing both assessments in one day, and a $10 bonus for completing 14 assessments (or 7 days) in a row. Participants could earn a total of $215 for completing all assessments. All procedures were approved by the university’s Institutional Review Board.
2.2 Screening Assessment
The study was comprised of three phases, a screening assessment to determine eligibility criteria, a pre-monitoring assessment, and then a four week monitoring period. The screening survey contained measures on demographics, trauma exposure, and alcohol consumption, whereas the pre-monitoring assessment included a measure of PTSD. Daily monitoring assessments included measures of distress related to their worst sexual assault experience, alcohol consumption, coping, and social support received.
2.2.1 Alcohol use
The Quantity Frequency Questionnaire (QF; Dimeff, Baer, Kivilhan, & Marlatt 1999) was used as a measure of peak drinking over the past month. Participants were included who endorsed drinking four or more drinks at least twice over the past month. A drink was defined as 12 oz. of beer, 10 oz. of microbrew or wine cooler, 4 oz. of wine, or 1 cocktail with 1 oz. of 100-proof liquor or 1.25 oz. of 80-proof liquor.
2.2.2 Sexual assault
Sexual assault in adulthood was assessed by the Sexual Experiences Survey (SES; Koss & Gidycz, 1985; Koss & Oros, 1982). Adult sexual assault was defined as “unwanted oral-genital contact, vaginal/anal intercourse, and/or penetration by objects since the age of 14.” Sexual victimization included attempted and completed unwanted oral, vaginal, and anal sexual intercourse. Response options for each of 18 experiences were 1= yes and 0= no.
2.2.3 Childhood sexual abuse
The Childhood Victimization Questionnaire (CVQ; Finkelhor, 1979) assessed sexual victimization prior to age 14. Childhood sexual abuse was defined as “any sexual activity that seemed coercive or forced and occurred before the age of 14 with someone 5 or more years older.” Participants were asked which, if any, of eleven unwanted sexual experiences, ranging from a sexual invitation to intercourse, had happened to them. Response options were 1= yes and 0= no.
2.3 Pre-Monitoring Assessment
2.3.1 PTSD symptomatology
The Posttraumatic Diagnostic Scale (PDS; Foa, Cashman, Jaycox, & Perry, 1997) was used to assess PTSD diagnostic status and symptom severity. Participants were asked to focus on their worst unwanted sexual experience and indicate how much each of the 17 PTSD symptoms had bothered them in the last month. Response options ranged from 0= not at all to 3= almost always. PTSD diagnostic status was assigned based on meeting criteria B (1 intrusive symptom), C (3 avoidance symptoms), and D (2 hyperarousal symptoms) of the DSM-IV (APA, 1994). The 17 items were summed for a total PTSD symptom severity score and demonstrated excellent internal reliability (α = .92).
2.4 Daily Monitoring Assessments
2.4.1 Alcohol consumption
Once a day participants were asked, “How many standard drinks have you had in the past 24 hours?” The same definition of a standard drink used in screening was provided. Standard drinks could be typed into the PDA. If the participant did not consume alcohol, they could either type in 0 or click the response “I did not drink.”
2.4.2 Sexual assault related distress
At each assessment a single item was used to assess how often participants experienced distress regarding their worst unwanted sexual experience since the last monitoring assessment. Response options ranged from 0 = not at all to 4 = almost always. Responses to the morning and evening assessments were averaged to represent daily distress.
2.4.3 Coping control
At each assessment, participants were asked to think about all of the things they did to cope or deal with their distress that day and then indicated how much control they felt they had over their distress (“Based on all the things you did to cope, or deal, with distress today, how much control do you feel you had over it?”) from 0 = no control to 6 = complete control, and how much they were able to decrease their distress (“Based on all the things you did to cope, or deal, with distress today, how much were you able to decrease it?”) from 0 = not at all to 6 = completely. Responses to the two items at both the morning and evening assessments were highly correlated, r = .82, p < .001, and so were averaged to reflect the average coping control for each day.
2.4.4 Social support
At each assessment, participants were asked to indicate how much they agree with the statement “Since the last assessment, you have gotten emotional support from your family and friends.” Response options ranged from 0 = strongly disagree to 5 = strongly agree.
2.5 Data Analyses
Our primary analytic goal was to examine whether there were daily associations between SA-related distress and drinking, and if this association was moderated by coping control or social support. We conducted separate generalized estimating equation (GEE; Hardin & Hilbe, 2003) models for coping control and social support, which account for the nested nature of our data (i.e., repeated daily assessments within individuals). We first ran models that included only the main effects of SA-related distress and either coping control or social support on drinking, and then ran models that included the interactions between SA-related distress and either coping control or social support. Because drinking was a positively skewed count variable, GEE models were estimated using a negative binomial distribution with a log link function. These models provide incidence rate ratios (IRRs), which serve as a standardized effect size and reflect the percentage increase or decrease in the rate of drinking as a function of another variable while holding all other variables constant.
To examine the within-person association between changes in daily SA-related distress and the number of drinks consumed each day, we centered SA-related distress at the person mean (i.e., subtracted an individual’s overall mean from each of their SA-related distress score). We also included average (i.e., person-mean) SA-related distress in both models to examine between-person associations. To examine whether social support or coping control moderated these within- or between-person associations, both social support and coping control were centered at the person mean and interactions between them and both the average and daily SA-related distress variables were included. Also included in the models were measures of baseline PTSD severity centered at the grand mean, an indicator for weekend versus weekday (0 = weekday and 1 = weekend), and a monitoring day variable to account for any possible change in responding over time (e.g., reporting less drinking toward the end of their assessment period).
3. Results
Out of a possible 3,990 monitoring days, data were collected for 2,494 (62.5%) days. On average participants provided data for 18.8 (SD=7.7) days during their 30-day daily monitoring assessment period. Participants reported drinking an average of 1.7 (SD=1.5) days per week and consumed on average 7.3 (SD=8.0) drinks per week. Descriptive statistics for the primary variables are provided in Table 1.
Table 1.
Descriptive statistics of study variables
| Observed Range | Mean | SD | |
|---|---|---|---|
| Average number of drinks per day | 0 – 25 | 1.2 | 2.6 |
| Baseline PTSD symptom severity | 2 – 38 | 13.4 | 8.0 |
| Average SA-related distress | 0 – 4 | 0.5 | 0.8 |
| Coping control | 0 – 6 | 3.2 | 1.4 |
| Social support | 0 – 5 | 2.2 | 1.4 |
Note. PTSD = posttraumatic stress disorder; SA = sexual assault; SD = standard deviation.
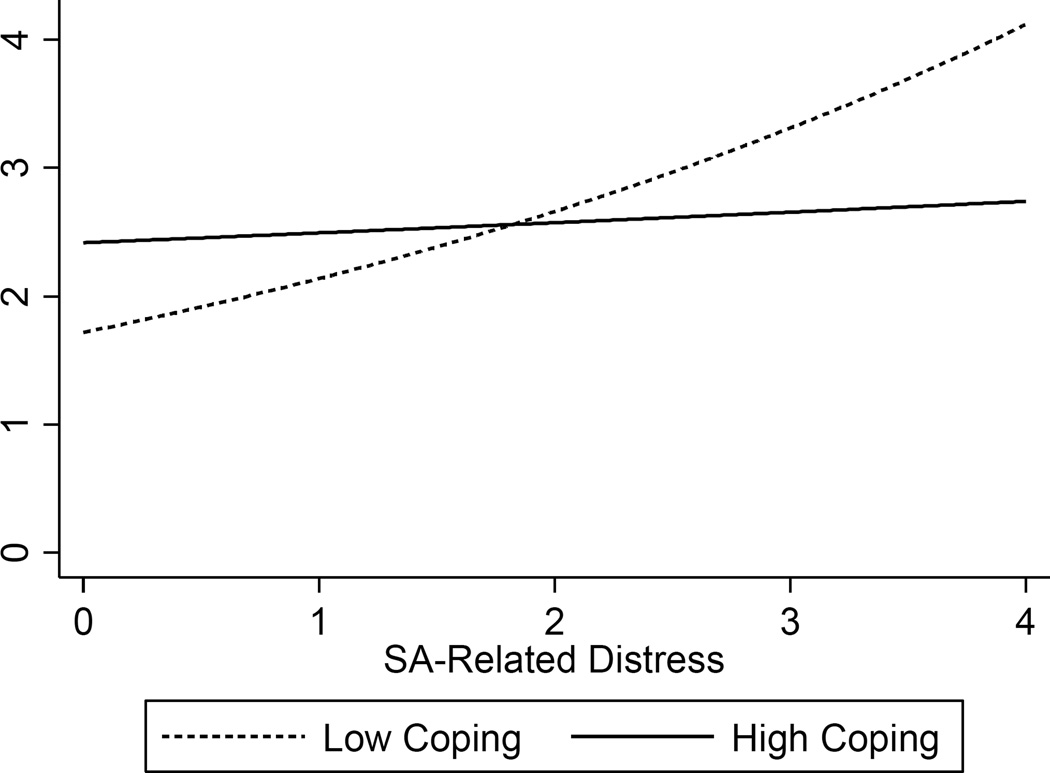
We conducted two GEE models to examine the association between SA-related distress and coping control on drinking (Table 2, Model 1), and whether daily coping moderated the association between average and daily SA-related distress and drinking (Table 2, Model 2). Results suggest that drinking decreased over the 30 days of monitoring, and more drinking was reported on the weekend compared to weekdays. As hypothesized, there was a significant main effect of daily SA-related distress on drinking. The more a woman’s level of distress increased above her average, the more she drank on that day. Additionally, there was a main effect of coping control on drinking such that the more a woman’s coping control increased above her average, the more she drank on that day. Also, as hypothesized there was a significant interaction between SA-related distress and coping control. As shown in Figure 1, women who reported less coping control drank more as their SA-related distress increased that day. Specifically, among those with less coping control, the number of drinks consumed increased by 9% for every 1-point increase in SA-related distress. However, women who reported more coping control drank about the same regardless of their level of SA-related distress. Baseline PTSD symptom severity and average SA-related distress were not associated with drinking.
Table 2.
GEE model for coping predicting daily number of drinks consumed
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| b | IRR [95% CI] | b | IRR [95% CI] | |
| Monitoring day | −0.01*** | 0.99 [0.99, 0.99] | −0.01*** | 0.99 [0.99, 0.99] |
| Weekend | 0.55*** | 1.73 [1.54, 1.95] | 0.56*** | 1.74 [1.55, 1.96] |
| Baseline PTSD symptom severity | 0.01 | 1.00 [0.996, 1.01] | 0.01 | 1.00 [0.996, 1.01] |
| Average SA-related distress | 0.07 | 1.07 [0.94, 1.22] | 0.06 | 1.06 [0.93, 1.20] |
| Daily SA-related distress | 0.13** | 1.14 [1.04, 1.24] | 0.12** | 1.13 [1.04, 1.23] |
| Coping control | 0.13*** | 1.13 [1.07, 1.20] | 0.12*** | 1.13 [1.07, 1.20] |
| Average distress × coping control | −0.03 | 0.97 [0.86, 1.09] | ||
| Daily distress × coping control | −0.10* | 0.91 [0.84, 0.99] | ||
Note. IRR = incidence rate ratio; CI = confidence interval; PTSD = posttraumatic stress disorder; SA = sexual assault.
p < .05.
p < .01.
p < .001.
Figure 1.
Coping control moderates the association between daily SA-related distress and the number of standard drinks consumed that day. For illustrative purposes, coping control is shown at 1 standard deviation above (i.e., High Coping) and below (i.e., Low Coping) the mean.
We conducted two additional GEE models to examine the association between social support and drinking (Table 3, Model 3), and whether social support moderated the association between average and daily SA-related distress and drinking (Table 3, Model 4). Results suggest that there was a significant main effect of daily SA-related distress on drinking with greater daily deviations from their own average level of SA-related distress associated with more drinking. There was also a significant main effect of social support such that less support was associated with more drinking. Social support did not moderate the association from a person’s average level of SA-related distress or their daily deviation in SA-related distress and drinking.
Table 3.
GEE model for social support predicting daily number of drinks consumed
| Model 3 | Model 4 | |||
|---|---|---|---|---|
| b | IRR [95% CI] | b | IRR [95% CI] | |
| Monitoring day | −0.01*** | 0.99 [0.99, 0.99] | −0.01*** | 0.99 [0.99, 0.99] |
| Weekend | 0.57*** | 1.76 [1.57, 1.98] | 0.57*** | 1.76 [1.57, 1.98] |
| Baseline PTSD symptom severity | 0.01 | 1.01 [0.997, 1.01] | 0.01 | 1.01 [0.997, 1.01] |
| Average SA-related distress | 0.06 | 1.06 [0.94, 1.21] | 0.06 | 1.06 [0.93, 1.21] |
| Daily SA-related distress | 0.11* | 1.12 [1.03, 1.22] | 0.11* | 1.12 [1.03, 1.22] |
| Social support | −0.06* | 0.95 [0.90, 0.999] | −0.06* | 0.95 [0.89, 0.998] |
| Average distress × social support | −0.02 | 0.98 [0.87, 1.10] | ||
| Daily distress × social support | 0.01 | 1.01 [0.93, 1.09] | ||
Note. IRR = incidence rate ratio; CI = confidence interval; PTSD = posttraumatic stress disorder; SA = sexual assault.
p < .05.
p < .001.
4. Discussion
This study is the first to examine the moderating influence of coping control and social support on the daily association between SA-related distress and alcohol use. Consistent with hypotheses, as daily SA-related distress increased from the person’s average level, alcohol consumption increased (H1). Coping control moderated this association such that drinking increased as daily SA-related distress increased among those who reported less coping control, whereas daily SA-related distress was not associated with drinking among those with more coping control (H2). Social support did not moderate the association between SA-related distress and drinking as expected; however, less social support on a given day was associated with increased drinking (H3). Findings shed light on the impact of SA-related distress on drinking, and suggest that increases in distress above and beyond the person’s average is an important predictor of daily drinking among survivors of SA.
Our findings that increased SA-related distress was associated with increased drinking is consistent with prior research demonstrating increased alcohol consumption, alcohol-related problems, and likelihood to drink to intoxication among SA survivors (e.g., Bedard-Gilligan, Kaysen, Desai, & Lee, 2011; Hughes, McCabe, Wilsnack, West, & Boyd, 2010; Kilpatrick, Acierno, Resnick, Saunders, & Best, 1997; Maniglio, 2011; Reed, Amaro, Matsumoto, & Kaysen, 2009; Ross et al., 2011). Further, our results suggest that an increase in SA-related distress above and beyond a person’s average level is significantly associated with drinking that same day, whereas the overall average level of distress was not. This provides further support and refinement of the self-medication hypothesis (Khantzian, 2003), which posits that survivors of SA drink in order to alleviate their distress. Future studies should continue to assess for differences in associations between average distress and drinking, as compared to associations between daily deviations in distress and drinking. This difference has implications for interventions that aim to reduce alcohol consumption among survivors of SA. Clinicians could help women to monitor for elevated distress in order to plan adaptive coping responses or seek social support to reduce drinking on those high-risk days.
Results also highlighted the role of perceptions of coping control and social support in drinking behavior among survivors of SA. Contrary to our expectations, as women’s coping control increased above their average levels, the number of drinks they consumed on that day increased. Because we did not ask participants what they did to cope, it is possible that they coped by drinking. However, in relation to their SA-related distress, it was women who reported less coping control who drank more as their SA-related distress increased above their average, while those who reported more coping control drank about the same regardless of their level of SA-related distress. This suggests that women who have less perceived coping control are influenced by day-to-day increases in distress more than women who have more perceived coping control. Future studies should attempt to determine which specific coping strategies are used on a given day and how the types of strategies used may interact with SA-related distress to influence drinking behavior. With regards to social support, results indicated that participants who reported less perceived support engaged in more drinking on that day. These findings are consistent with prior studies documenting the link between receiving positive social support and reduced psychological distress among SA survivors (Ullman, 1996; Ullman & Filipas, 2001). Accordingly, women with reduced access to effective coping strategies and sources of support may turn to alcohol use as a means to cope with their distress. Coping and social support both represent adaptive coping strategies that can serve to protect survivors of SA from increased drinking and potential problems associated with heavy drinking. Interventions aimed at reducing drinking among women with a history of SA should include coping skills acquisition and efforts designed to increase access to and utilization of social support.
Results from the present study are subject to limitations. First, our sample was comprised of college women from one university who endorsed a recent heavy drinking episode and either child or adult SA. This may limit the generalizability of results to other college samples, non-college women, male SA survivors, those without a history of heavy drinking, or those who experienced traumas other than SA. Additionally, the current study relied exclusively on self-report measures of psychological distress, alcohol use, coping control, and social support, which may be subject to under- or over-reporting given the sensitive nature of these topics. Although the daily assessment of these variables is a notable strength of our study, it also required that we limit our assessments of each construct in order to minimize participant burden. For example, we were not able to query women regarding the specific coping strategies they used. Further, daily assessments may introduce some bias in that participants could have attributed their drinking to elevated SA-related distress and then responded to items in a manner consistent with this belief. Given the decrease in drinking observed across the daily monitoring assessment period, it is possible that being asked to monitor ones alcohol consumption every day influenced participants’ actual behavior. Although we attempted to address this issue by controlling for monitoring day in our analyses, it is possible that the associations of interest were impacted by the observed decrease in drinking.
4.1 Conclusion
In conclusion, findings highlight the importance of coping abilities and social support in the drinking behavior of female survivors of SA. Additionally, daily deviation in SA-related distress appears to be an important factor in alcohol consumption beyond average levels of distress, especially among those who have less coping control. Interventions for women with SA histories should include self-monitoring skills for days with heightened need for coping skills or social support to reduce drinking.
References
- Abbey A, Ross LT, McDuffie D, McAuslan P. Alcohol and dating risk factors for sexual assault among college women. Psychology of Women Quarterly. 1996;20:147–169. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Armeli S, Conner TS, Cullum J, Tennen H. A longitudinal analysis of drinking motives moderating the negative affect-drinking association among college students. Psychology of Addictive Behaviors. 2010;24:38–47. doi: 10.1037/a0017530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armeli S, Tennen H, Affleck G, Kranzler HR. Does affect mediate the association between daily events and alcohol use? Journal of Studies on Alcohol and Drugs. 2000;61:862–871. doi: 10.15288/jsa.2000.61.862. [DOI] [PubMed] [Google Scholar]
- Bedard-Gilligan M, Cronce JM, Lehavot K, Blayney JA, Kaysen D. The relationship between assault and physical health complaints in a sample of female drinkers: Roles of avoidant coping and alcohol use. Journal of Interpersonal Violence. 2014;29:1359–1379. doi: 10.1177/0886260513507139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedard-Gilligan M, Kaysen D, Desai S, Lee CM. Alcohol-involved assault: Associations with posttrauma alcohol use, consequences, and expectancies. Addictive Behaviors. 2011;36:1076–1082. doi: 10.1016/j.addbeh.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener ND, McMahon PM, Warren CW, Douglas KA. Forced sexual intercourse and associated health-risk behaviors among female college students in the United States. Journal of Consulting and Clinical Psychology. 1999;67:252–259. doi: 10.1037//0022-006x.67.2.252. [DOI] [PubMed] [Google Scholar]
- Cleveland HH, Harris KS. The role of coping in moderating within-day associations between negative triggers and substance use cravings: A daily diary investigation. Addictive Behaviors. 2010;35:60–63. doi: 10.1016/j.addbeh.2009.08.010. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Downey G. Social factors and psychopathology: stress, social support, and coping processes. Annual Review of Psychology. 1991;42:401–425. doi: 10.1146/annurev.ps.42.020191.002153. [DOI] [PubMed] [Google Scholar]
- DeLongis A, Holtzman S. Coping in context: the role of stress, social support, and personality in coping. Journal of Personality. 2005;73:1633–1656. doi: 10.1111/j.1467-6494.2005.00361.x. [DOI] [PubMed] [Google Scholar]
- Dimeff L, Baer J, Kivlihan D, Marlatt AG. Brief alcohol screening and intervention for college students: A harm reduction approach (BASICS) New York, NY: Guilford Press; 1999. [Google Scholar]
- Finkelhor D. Sexually Victimized Children. New York: The Free Press; 1979. A survey on children’s victimization; pp. 34–72. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9:445–451. [Google Scholar]
- Frazier PA, Mortensen H, Steward J. Coping strategies as mediators of the relations among perceived control and distress in sexual assault survivors. Journal of Counseling Psychology. 2005;52:267–278. [Google Scholar]
- Gross AM, Winslett A, Roberts M, Gohm CL. An examination of sexual violence against college women. Violence Against Women. 2006;12:288–300. doi: 10.1177/1077801205277358. [DOI] [PubMed] [Google Scholar]
- Gleason NA. College women and alcohol: A relational perspective. Journal of American College Health. 1994;42:279–289. doi: 10.1080/07448481.1994.9936360. [DOI] [PubMed] [Google Scholar]
- Grayson CE, Nolen-Hoeksema S. Motives to drink as mediators between childhood sexual assault and alcohol problems in adult women. Journal of Traumatic Stress. 2005;18(2):137–145. doi: 10.1002/jts.20021. [DOI] [PubMed] [Google Scholar]
- Hardin JW, Hilbe JM. Generalized estimating equations. Boca Raton, FL: Chapman & Hall/CRC; 2003. [Google Scholar]
- Hruska B, Delahanty DL. Application of the stressor vulnerability model to understanding posttraumatic stress disorder (PTSD) and alcohol-related problems in an undergraduate population. Psychology of Addictive Behaviors. 2012;26:734–746. doi: 10.1037/a0027584. [DOI] [PubMed] [Google Scholar]
- Hruska B, Fallon W, Spoonster E, Sledjeski EM, Delahanty DL. Alcohol use disorder history moderates the relationship between avoidance coping and posttraumatic stress symptoms. Psychology of Addictive Behaviors. 2011;25:405–414. doi: 10.1037/a0022439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes T, McCabe SE, Wilsnack SC, West BT, Boyd CJ. Victimization and substance use disorders in a national sample of heterosexual and sexual minority women and men. Addiction. 2010;105:2130–2140. doi: 10.1111/j.1360-0443.2010.03088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, Atkins DC, Simpson TL, Stappenbeck CA, Blayney JA, Lee CM, Larimer ME. Proximal relationships between PTSD symptoms and drinking among female college students: Results from a daily monitoring study. Psychology of Addictive Behaviors. 2014;28:62–73. doi: 10.1037/a0033588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis revisited: The dually diagnosed patient. Primary Psychiatry. 2003;10(9):47–54. [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, Best CL. A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. Journal of Consulting and Clinical Psychology. 1997;65:834–847. doi: 10.1037//0022-006x.65.5.834. [DOI] [PubMed] [Google Scholar]
- King DW, Taft C, King LA, Hammond C, Stone ER. Directionality of the association between social support and posttraumatic stress disorder: A longitudinal investigation. Journal of Applied Social Psychology. 2006;36:2980–2992. [Google Scholar]
- Koss MP, Gidycz CA. Sexual experiences survey: reliability and validity. Journal of Consulting and Clinical Psychology. 1985;53:422–423. doi: 10.1037//0022-006x.53.3.422. [DOI] [PubMed] [Google Scholar]
- Koss MP, Oros CJ. Sexual Experiences Survey: A research instrument investigating sexual aggression and victimization. Journal of Consulting and Clinical Psychology. 1982;50:455–457. doi: 10.1037//0022-006x.50.3.455. [DOI] [PubMed] [Google Scholar]
- Laffaye C, Cavella S, Drescher K, Rosen C. Relationships among PTSD symptoms, social support, and support source in veterans with chronic PTSD. Journal of Traumatic Stress. 2008;21:394–401. doi: 10.1002/jts.20348. [DOI] [PubMed] [Google Scholar]
- Lansford JE, Dodge KA, Pettit GS, Bates JE, Crozier J, Kaplow J. A 12-year prospective study of the long-term effects of early child physical maltreatment on psychological, behavioral, and academic problems in adolescence. Archives of Pediatrics & Adolescent Medicine. 2002;156:824–830. doi: 10.1001/archpedi.156.8.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maniglio R. The role of child sexual abuse in the etiology of substance-related disorders. Journal of Addictive Diseases. 2011;30:216–228. doi: 10.1080/10550887.2011.581987. [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Long PJ, Siegfried NJ. The revictimization of child sexual abuse survivors: An examination of the adjustment of college women with child sexual abuse, adult sexual assault, and adult physical abuse. Child Maltreatment. 2000;5:18–27. doi: 10.1177/1077559500005001003. [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Ward RM, Brown AL. Substance use and PTSD symptoms impact the likelihood of rape and revictimization in college women. Journal of Interpersonal Violence. 2009;24:499–521. doi: 10.1177/0886260508317199. [DOI] [PubMed] [Google Scholar]
- Mohr CD, Armeli S, Tennen H, Carney MA, Afflect G, Hromi A. Daily interpersonal experiences, context, and alcohol consumption: Crying in your beer and toasting good times. Journal of Personality and Social Psychology. 2001;80:489–500. doi: 10.1037/0022-3514.80.3.489. [DOI] [PubMed] [Google Scholar]
- Oslin DW, Cary M, Slaymaker V, Colleran C, Blow FC. Daily ratings measures of alcohol craving during an inpatient stay define subtypes of alcohol addiction that predict subsequent risk for resumption of drinking. Drug and Alcohol Dependence. 2009;103:131–136. doi: 10.1016/j.drugalcdep.2009.03.009. [DOI] [PubMed] [Google Scholar]
- Rankin LA, Maggs JL. First-year college student affect and alcohol use: Paradoxical within-and between-person associations. Journal of Youth and Adolescence. 2006;35:925–937. [Google Scholar]
- Read JP, Ouimette P, White J, Colder C, Farrow S. Rates of DSM–IV–TR trauma exposure and posttraumatic stress disorder among newly matriculated college students. Psychological Trauma: Theory, Research, Practice, and Policy. 2011;3:148–156. doi: 10.1037/a0021260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed E, Amaro H, Matsumoto A, Kaysen D. The relation between interpersonal violence and substance use among a sample of university students: Examination of the role of victim and perpetrator substance use. Addictive Behaviors. 2009;34:316–318. doi: 10.1016/j.addbeh.2008.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LT, Kolars CLK, Krahn DD, Gomberg ESL, Clark G, Niehaus A. Nonconsensual sexual experiences and alcohol consumption among women entering college. Journal of Interpersonal Violence. 2011;26:399–413. doi: 10.1177/0886260510363418. [DOI] [PubMed] [Google Scholar]
- Rothbaum BO, Foa EB, Riggs DS, Murdock T, Walsh W. A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress. 1992;5:455–475. [Google Scholar]
- Skinner EA, Edge K, Altman J, Sherwood H. Searching for the structure of coping: a review and critique of category systems for classifying ways of coping. Psychological Bulletin. 2003;129:216–269. doi: 10.1037/0033-2909.129.2.216. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM, Oliver MNI, Bush JA, Palmer MA. An experience sampling study of associations between affect and alcohol use and problems among college students. Journal of Studies on Alcohol. 2005;66:459–469. doi: 10.15288/jsa.2005.66.459. [DOI] [PubMed] [Google Scholar]
- Simpson TL, Stappenbeck CA, Luterek JA, Lehavot K, Kaysen DL. Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. Journal of Abnormal Psychology. 2014;123:237–247. doi: 10.1037/a0035193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swendsen JD, Tennen H, Carney MA, Affleck G, Willard A, Hromi A. Mood and alcohol consumption: An experience sampling test of the self-medication hypothesis. Journal of Abnormal Psychology. 2000;109:198–204. [PubMed] [Google Scholar]
- Ullman SE. Social reactions, coping strategies, and self-blame attributions in adjustment to sexual assault. Psychology of Women Quarterly. 1996;20:505–526. [Google Scholar]
- Ullman S, Filipas HH. Predictors of PTSD Symptom Severity and Social Reactions in Sexual Assault Victims. Journal of Traumatic Stress. 2001;14:369–389. doi: 10.1023/A:1011125220522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, Peter-Hagene L. Social reactions to sexual assault disclosure, coping, and PTSD symptoms in sexual assault victims. Journal of Community Psychology. 2014;42:495–508. doi: 10.1002/jcop.21624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, Townsend SM, Filipas HH, Starzynski LL. Structural models of the relations of assault severity, social support, avoidance coping, self-blame, and PTSD among sexual assault survivors. Psychology of Women Quarterly. 2007;31:23–37. [Google Scholar]
- Valentiner DP, Foa EB, Riggs DS, Gershuny BS. Coping strategies and posttraumatic stress disorder in female victims of sexual and nonsexual assault. Journal of Abnormal Psychology. 1996;105:455–458. doi: 10.1037//0021-843x.105.3.455. [DOI] [PubMed] [Google Scholar]
- Walsh K, Danielson C, McCauley JL, Saunders BE, Kilpatrick DG, Resnick HS. National prevalence of posttraumatic stress disorder among sexually revictimized adolescent, college, and adult household-residing women. Archives of General Psychiatry. 2012;69:935–942. doi: 10.1001/archgenpsychiatry.2012.132. [DOI] [PMC free article] [PubMed] [Google Scholar]