Abstract
A controlled trial of Seeking Safety (SS) and Male-Trauma Recovery Empowerment Model (M-TREM) examined implementation and effectiveness of integrated group therapy for comorbid post-traumatic stress disorder (PTSD) and substance use disorder (SUD) on PTSD and mental health symptoms plus self-esteem and efficacy for incarcerated men. The study sample (n = 230) was male inmates 18 years or older who were primarily non-white, high school graduates or equivalents, had childhood trauma histories, committed violent crimes, had serious mental illnesses, and resided in a maximum security prison. Incarcerated men, who screened positive for PTSD and SUD, were assigned randomly (n = 142) or by preference (n = 88) to receive SS or M-TREM, with a waitlist group of (n = 93). Manualized interventions were group-administered for 14 weeks. Primary outcomes were PTSD and other mental health symptoms. Secondary outcomes were self-esteem, coping, and self-efficacy. SUD outcomes cannot be measured in a correctional setting. Implementation feasibility was exhibited by the ability to recruit, screen, assign, and retain participants. Effectiveness findings depended on sample, design, and method for analysis. Using a waitlist control group and no follow-up period, we found no aggregate effect of treatment on PTSD symptoms, although, when disaggregated, M-TREM was found to improve PTSD severity and SS improved general mental health symptoms and psychological functioning. Using intent-to-treat and completer analyses, no significant differences were found in the relative performance between SS and M-TREM on primary or secondary outcomes. When longitudinal data were maximized and modeled in ways that reflect the hierarchical nature of the data, we found that SS and M-TREM performed better than no treatment on PTSD severity and secondary outcomes, and that treatment benefits endured. Findings cautiously support implementing either Seeking Safety or M-TREM to treat incarcerated men with co-morbid PTSD and addiction problems.
Keywords: PTSD, Seeking Safety, Trauma Recovery and Empowerment Model (MTREM), Incarcerated men, Integrated treatment
1. Introduction
Trauma exposure and the prevalence of post-traumatic stress disorder (PTSD) among incarcerated men is receiving attention in part because men are vastly overrepresented in prisons and jails and drawn disproportionately from socially and economically distressed communities where violence is part of the culture (Wolff, Huening, Shi, & Frueh, 2014). Trauma, especially violent trauma, is widespread among men in general. Lifetime exposure to at least one traumatic event for males in community samples range from 43% to 92%, depending on the study sample (Breslau, 2009). Compared to women, men are more likely to report assaultive violence (i.e., mugging, threatened with a weapon, shot or stabbed, or badly beaten up). For men, the likelihood of experiencing assaultive violence increases with the following characteristics: nonwhite, low education, low income, and urban residence (Breslau et al., 1998); characteristics that are prevalent among incarcerated populations (National Research Council, 2014). A history of childhood abuse, while less common, is also prevalent among men, with rates as high as 14% and 22% for childhood sexual abuse and physical abuse, respectively (Briere & Elliott, 2003).
Lifetime trauma exposure rates for incarcerated men vary from 62% to 100% (Wolff et al., 2014). The prevalence of trauma among incarcerated men has been found to be higher for physical trauma compared to sexual trauma, in persons with mental disorders than without disorders, and those experiencing childhood abuse than with no childhood abuse (Wolff, Shi, & Siegel, 2009). Childhood trauma, in particular, is extensive among incarcerated male populations. Approximately, 7 in 10 incarcerated males self-report childhood physical, sexual abuse, or neglect (Dutton & Hart, 1992; Weeks & Widom, 1998; Wolff et al., 2014). Numerous studies have shown that exposure to abuse in childhood increases the likelihood of aggression and arrest in adulthood (Dutton & Hart, 1992; Maxfield & Widom, 1996; Sarchiapone, Carli, Cuomo, Marchetti, & Roy, 2009). More specifically, victims of childhood abuse are two to three times more likely to be arrested for violence as adults (Dutton & Hart, 1992; Maxfield & Widom, 1996).
Trauma is the etiological link to PTSD. While most men living in the community have experienced a traumatic event during their lifetimes, only 3–6% of those exposed develop symptoms that meet the criteria for lifetime PTSD (Breslau, 2009). Rates are significantly higher for males residing in correctional settings. In correctional studies based on samples with fewer than 220 participants and using varying diagnostic methodologies, rates of PTSD among incarcerated men are estimated from 21% (general prison population) to 39% (jailed veterans) for current PTSD, with a lifetime PTSD rate of 33% (general prison population) (Gibson et al., 1999; Powell, Holt, & Fondacato, 1997; Saxon et al., 2001). Using a larger male prison sample (n = 592) and a psychometrically robust screen for PTSD (PTSD Checklist-Civilian Version [PCL-C]), Wolff et al. (2014) estimated conditional probabilities for PTSD symptoms with exposure to physical violence at 60% for moderate symptoms (PCL-C > 35) and 30% for severe symptoms (PCL-C > 50) of PTSD. Conditional probabilities for PTSD symptoms were higher yet for men who experienced a sexually traumatic event, with conditional probabilities of 75% and 43% for screening positive for PTSD with, respectively, moderate to severe symptoms.
Men with PTSD are also likely to have a co-morbid substance use disorder (SUD). According to findings from the National Comorbidity Study, among men with PTSD, 52% met criteria for lifetime alcohol use disorder and 34.5% for substance abuse disorder (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). In SUD treatment samples, a current substance abuse diagnosis is often comorbid with PTSD, with rates ranging from 20% to 58% (Brady, Dansky, Sonne, & Saladin, 1998; McGovern et al., 2009; Najavits et al., 1998; Rash, Coffey, Baschnagel, Drobes, & Saladin, 2008; Reynolds et al., 2005; Triffleman, Marmar, Delucchi, & Ronfeldt, 1995). Higher co-morbidity rates have been found for incarcerated males. Gibson and et al. (1999) reported correlation between lifetime PTSD and alcohol abuse/dependence at 85% and 70% for drug abuse/dependence. Another study of incarcerated men enrolled in a drug treatment program reported that 53% of these men reported symptoms that met PTSD criteria (Pimlott Kubiak, 2004). Although the research evidence remains mixed regarding whether PTSD precedes SUD (associated with the “self-medication hypothesis” – substances are used to relieve distressing psychological symptoms) or SUD precedes PTSD (captured by the “lifestyle hypothesis” – substance users engage in risky behaviors to support their habits), either pathway is associated with a heightened risk of criminality (Chilcoat & Breslau, 1998).
The substantially higher rates of trauma and PTSD among incarcerated men, compared to their counterparts in the general population, is not surprising given the disproportionate draw of incarcerated men from inner city areas characterized by poverty, low educational achievement, and non-white residents–risk factors for trauma exposure, which increase the likelihood of violence and arrest. Similarly, lifetime rates of drug or alcohol dependence among incarcerated men, ranging from 37% to 57% (Lo & Stephens, 2000; Mumola & Karberg, 2006; Peters, Greenbaum, Edens, Carter, & Ortiz, 1998) are also considerably higher than rates estimated for the general population (19% age 18–26 and 7% age 26+) (Substance Abuse and Mental Health Services Administration, 2013). It is estimated that roughly half of males housed in state prisons met full diagnostic criteria for SUD immediately prior to their incarceration (Mumola & Karberg, 2006).
The large number of incarcerated males (~1.4 million), combined with their high rates of trauma exposure, PTSD, and related SUD, suggests a significant need for trauma treatment geared for men in correctional settings. There is a need to screen for and treat trauma-related symptoms, as well as create a correctional environment that is more trauma-informed (Miller & Najavits, 2012; SAMHSA National GAINS Center, 2011). Screening for trauma and PTSD is a critical first step. A recent study explored the feasibility, reliability, and validity of screening for PTSD among incarcerated men using computerized-administration of the PTSD Checklist (PCL) (Wolff et al., 2014). This study, based on a sample of 400 incarcerated men, found that computer-administered screening, compared to interviewer-administered screening, was feasible and yielded equally reliable and valid (compared to CAPS diagnostic criteria) information on PTSD symptoms, increased the efficiency of screening for PTSD among incarcerated men and identified those at risk for treatment.
Treatment guidelines for PTSD have been established by a variety of professional organizations. These guidelines highly rank psychotherapy interventions incorporating cognitive–behavioral orientations (Foa, Keane, Friedman, & Cohen, 2005; Schnurr, 2008). Further, the literature suggests that: (1) integrated treatment for co-morbid conditions is optimal, compared to parallel, sequential, or single treatment models (Morrissey et al., 2005; Mueser, Drake, Sigmon, & Brunette, 2005); (2) trauma-related difficulties are best treated in stages, with the first stage focusing on safety through recognition, education, and skill building that develop coping skills to replace use of substances or other self-harming behaviors (Harris & Fallot, 2001; Herman, 1997); and (3) environment matters in the selection of type of intervention (Foa et al., 2005). With this guidance in mind, there are several interventions that have potential for incarcerated men with comorbid PTSD and SUD.
The most robust evidence-base supports exposure therapy, a past-focused intervention that explores emotions and thought processes related to traumatic experiences (Institute of Medicine, 2007). This intervention is categorized as a second stage intervention, which must be delivered in safe and supportive environments (Bradley, Greene, Russ, Dutra, & Western, 2005). Authoritative and punitive settings, like prisons, do not meet standards for exposure processing (Miller & Najavits, 2012; Wolff et al., 2009). At least initially, first stage trauma interventions, which are present-focused, are more appropriate for prison environments as they focus on building coping skills, drawing cognitive connections among trauma experiences, behaviors, and treatment, and empowering clients to manage choices that affect their lives. Several integrated PTSD and SUD interventions have a supporting evidence bases and have been adapted for men (Najavits et al., 2009; SAMHSA National GAINS Center, 2011).
The two most prominent first stage (present-focused) interventions are Seeking Safety (SS) and Trauma Recovery and Empowerment Model (TREM), both of which are manualized, integrate treatment for PTSD and SUD, and rely heavily on cognitive–behavioral techniques and skill-building orientations to foster empowerment and safety. While both focus on trauma-related psychopathology, their underlying philosophy and content are different. SS integrates cognitive–behavioral techniques and psycho-educational principles with emphasis on reducing PTSD and SUD symptoms by building safe coping skills (Najavits, 2002, 2007). The SS manual covers topics that address cognitive, behavioral, and interpersonal needs of persons with PTSD and SUD, and focuses on deficits found in the incarcerated population, including impulsiveness, social maladjustment, and emotional dysregulation (Najavits, 2002). By contrast, TREM (M-TREM, for males) integrates empowerment, trauma education, and skill building using the techniques of cognitive restructuring, psycho-education, coping skills training, and meditation. It draws heavily from psychodynamic and experiential techniques, along with the use of peer support (Fallot & Harris, 2002). Both interventions include clinician guides, manuals, instructional videos, and have been adapted for men.
Research on the effectiveness of integrated PTSD/SUD interventions is growing but modest. A recent literature review identified 29 published studies of five present-focused integrated PTSD/SUD interventions (Najavits & Hien, 2013). Scientific inquiry has concentrated predominately on SS; 21 of the 29 (72%) published studies evaluated SS, with TREM the next most studied intervention with three (10%) studies. Of the TREM and SS studies (n = 24), half (n = 12) had comparison groups and one-quarter (n = 6) randomly assigned participants to these conditions. The three studies of TREM and three of the nine studies evaluating SS had control groups, but no randomization, while the other six studies of SS had control groups and randomization. With one notable exception (Boden et al., 2012), these studies only enrolled females and typically females engaged in some form of behavioral health treatment (Amaro et al., 2007; Fallot, McHugo, Harris, & Xie, 2011; Gatz et al., 2007; Ghee, Bolling, & Johnson, 2009; Hien, Cohen, & Campbell, 2009; Hien, Cohen, Miele, Litt, & Capstick, 2004; Najavits, Gallop, & Weiss, 2006; Toussaint, VanDeMark, Bornemann, & Graeber, 2007; Zlotnick, Johnson, & Najavits, 2009). Two of the studies were conducted on incarcerated female samples (Lynch, Heath, Matthews, & Cepeda, 2012; Zlotnick et al., 2009)
Based on female samples, the evidence on SS and TREM is promising. Of the eight randomized and non-randomized controlled studies of SS, compared to the control condition, SS had superior outcomes for PTSD symptoms in six studies (Desai, Harpaz-Rotem, Najavits, & Rosenheck, 2008; Gatz et al., 2007; Ghee et al., 2009; Hien et al., 2004; Lynch et al., 2012; Najavits et al., 2006) and superior substance use outcomes in two (Hien et al., 2004; Najavits et al., 2006). In addition, SS outperformed the control condition on several secondary outcomes, such as social support (Desai et al., 2008), dimensions of psychopathology (Desai et al., 2008; Hien et al., 2004, 2009; Lynch et al., 2012; Najavits et al., 2006; Zlotnick et al., 2009), and coping (Lynch et al., 2012). For TREM, while the evidence base is thinner, it mirrors that for SS. All three studies found improvements over the control conditions in domains related to trauma and mental health symptoms (Amaro et al., 2007; Fallot et al., 2011; Toussaint et al., 2007), and one study found TREM outperformed the control condition on substance use outcomes (Fallot et al., 2011). While the findings from these studies are encouraging, the test conditions for SS and TREM have not been optimal. The dose of the interventions and their fidelity to the manual have been partial in two of the three TREM studies (Amaro et al., 2007; Toussaint et al., 2007) and three of the nine SS studies (Ghee et al., 2009; Hien et al., 2009; Zlotnick et al., 2009).
Similar evidence is not available for men, although both interventions have been adapted for men (Najavits et al., 2009). There have been no published studies on M-TREM. For SS, there are five studies with male samples; two enrolled male veterans (Boden et al., 2012), one enrolled male and female veterans (Cook, Walser, Kane, Ruzek, & Woody, 2006), one enrolled young African American males under drug court supervision (Hamilton, 2006), and one enrolled civilian men with histories of childhood trauma (Najavits, Schmitz, Gotthardt, & Weiss, 2005). Only the study among men conducted by Boden et al. (2012) used a random controlled study design. In this study of male veterans, SS had superior outcomes on drug use and coping skills, compared to the control condition: standard VA substance abuse treatment (Boden et al., 2012). This study and the other pilot studies indicate the feasibility of SS with male subjects but more rigorous research is needed to substantiate claims of effectiveness.
Overall, SS and M-TREM have effectiveness evidence that supports their potential benefit for incarcerated males. Both interventions have been adapted for men, with the smallest adjustments to the SS intervention (which was designed initially for both genders but implemented primarily with females). Overall, SS has been found to translate very clearly and effectively to males, requiring only modest content and formatting changes (Najavits et al., 2009). Men’s Trauma Recovery and Empowerment Model (M-TREM) has been tailored for men and has a separate manual. The eight core assumptions of M-TREM address the differences in gender-role experiences of trauma, where men face a “disconnection dilemma,” where “in order to retain the feelings of fear, vulnerability, and powerlessness associated with trauma, they must disconnect from male gender role expectations that preclude such feelings” (Fallot et al., 2001). While there is modest but growing evidence base in support of both first stage interventions, each program has a different approach to engaging men in trauma recovery. It is unclear whether either approach is effective in an incarcerated male population and if those differences are clinically meaningful.
We, therefore, conducted a randomized control trial of SS and M-TREM, compared to a waitlist control group and a “head-to-head” comparison group, using an incarcerated male sample that meets screening criteria for PTSD and SUD and tests (a) the ability to implement manualized treatment in a prison setting and (b) changes in primary (e.g., PTSD severity, mental health symptoms) and secondary outcomes (e.g., self-esteem, coping, self-efficacy) over time. SUD is not included as an outcome measure because use of drugs or alcohol while incarcerated is a chargeable offense and researchers are required to report any known use of alcohol or drug use to prison authorities.
2. Method
2.1. Study overview
This controlled trial tested the effectiveness of group-based integrated treatment for PTSD and addiction disorders among incarcerated men housed at a high security prison operated by the Pennsylvania Department of Corrections from February 2012 to October 2013. Incarcerated men who screened positive for PTSD and SUD, were assigned randomly to either random assignment (n = 142) or preference assignment (n = 88) to receive SS or M-TREM, with a waitlist group of (n = 93). Manualized interventions were group-administered for 14-weeks. The waitlist design controls for threats to internal validity; the waitlist group includes subjects who were eligible for treatment assignment but participated only in study assessments for the 3 months, while the treatment group is assigned to a 3-month intervention (SS or M-TREM). The comparison group trial uses random and preference assignment to SS and M-TREM to test for measurable differences in primary and secondary outcomes post-intervention and at 3-and 6-month follow-up. Intent-to-treat and completer analyses are conducted, as well as analyses that controlled for the nesting of data within individuals and interventions.
2.2. Participants
Incarcerated men were screened for eligibility (see Consolidated Statement on Reporting Trials (CONSORT) diagram, Fig. 1). Residents eligible for the screening were English-speaking men, 18 years or older, and had at least 10 months remaining on their mandatory minimum sentence at the host facility (to ensure sufficient time to complete the study prior to release). Excluded were residents with active psychosis or organic brain impairment or on suicide watch within the past 3 months.
Fig. 1.

CONSORT diagram for recruitment.
According to prison administrative records, of the estimated 4000 residents, 1887 were eligible for the study. Half of these men (n = 944) were randomly invited to be screened and 592 gave written consent and participated in the screening interviews, for a participation rate of 63%. Of those screened, 327 (55%) screened positive for current PTSD symptoms (PCL-C > 34) and a substance abuse problem (ASSIST ≥ 11 for alcohol and ASSIST > 4 for a substance abuse problem) and, of those, 230 (70% of those who screened positive for PTSD symptoms and a substance/alcohol abuse problem) agreed to participate in the treatment phase of the study (i.e., the intent-to-treat (ITT) sample).
There were no significant differences in the age, years incarcerated, and veteran status characteristics between the eligible (n = 230) and declined participation (n = 97) groups, although the eligible group, compared to the decliner group, was more likely to include African Americans (52% vs. 36%, p < 0.05) and violent offenders (56% vs. 43%, P < 0.05), and less likely to include drug offenders (14% vs. 25%, p < 0.05) and without a high school or GED (18% vs. 28%, p < 0.05). Those who declined mentioned several reasons for not participating including not being ready to address trauma issues, not needing treatment, expecting to be released or transferred, or scheduling conflicts with other required programs. Subjects volunteered for screening and treatment and did not receive monetary compensation or prison credits (i.e., “good time credits”) for their participation. They did receive a calendar and a Pennsylvania reentry manual for completing the screening interviews.
The protocols for recruitment and interviewing were approved by the appropriate institutional review boards. All participants signed informed consent forms after the conditions of participation (including confidentiality, duty to inform, privacy, risks, benefits, and right to withdraw or refuse to answer questions) were reviewed with them by research staff.
2.3. Measures
Effectiveness was measured using three primary outcomes: the PTSD Checklist for Civilians (PCL-C), the Clinician-Administered PTSD Scale (CAPS), the Global Severity Index (GSI) of the Brief Symptom Inventory (BSI), an established self-report measure of psychological symptoms (Derogatis, 1993), and three secondary outcomes: Rosenberg Self-Esteem Scale (SES) (Crandal, 1973), Proactive Coping Inventory (PCI) (Greenglass & Schwarzer, 1998), and Generalized Perceived Self-Efficacy (GPEF) (Schwarzer & Jerusalem, 1995) to measure changes in, respectively, self-esteem, coping proactivity, and self-efficacy. All the clinical measures are commonly used to assess traumatized populations (Elhai, Gray, Kashdan, & Franklin, 2005), have robust psychometric properties, and were scored in standard fashion.
To assess the presence of current PTSD symptoms, we used the PCL-C, a 17-item self-report measure of PTSD symptoms based on DSM-IV criteria that uses a 5-point Likert scale format generating a score ranging from 17 to 85, with higher scores indicating greater symptom severity (Wilkins, Lang, & Norman, 2011). The Clinician-Administered PTSD Scale (CAPS) (Weathers & Litz, 1994; First, Spitzer, Gibbon, & Williams, 2002), the gold-standard measure for the diagnosis of PTSD, was used to assess PTSD severity and diagnose current full or sub-threshold PTSD (Blake et al., 1990; Weathers & Litz, 1994) based on DSM-IV criteria. Sub-threshold PTSD classification required a qualifying traumatic event, one re-experiencing symptom and either three avoidance or two arousal symptoms with the presence of co-occurring significant distress or impairment in functioning (Grubaugh, Elhai, Cusack, Wells, & Frueh, 2007).
The screening interview battery also included: background questions on criminal history (e.g., years incarcerated, type of offense), self-reported health status and treatment conditions, demographics (e.g., education, race, ethnicity, age, citizenship, veteran status, marital status, employment history), the Trauma History Questionnaire (Green, 1996; Hooper, Stockton, Krupnick, & Green, 2011), a modified version of the National Violence Against Women and Men Survey (NVAWM) (Tjaden & Thoennes, 2002), the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) (World Health Organization, 2010), and the Structured Clinical Interview for DSM-IV-Non-Patient Version with Psychotic Screen (SCID-NP) (First et al., 2002) to establish comorbid psychiatric diagnoses.
2.4. Assessment procedures
Participants were screened first and if eligible and consented were assigned to the treatment phase of the study. Screening involved an initial computer-administered screening interview, followed by a clinical assessment interview. Assessments, administered in part by computer and in part by clinician, occurred at baseline (study entry) and at 3-, 6-, and 9-months post baseline, which corresponds with the start of the study, completion of treatment or the waitlist period, and 3- and 6-month post-intervention.
2.4.1. Computer-administered interviewing
All measures with the exception of the CAPS and SCID-NP were administered by computer. Questionnaire Development System software and computer-assisted self-interviewing (CASI) technology were used to administer these surveys by laptop computers with mouse devices. The surveys were available in English. In less than 1% of cases, literacy issues arose that resulted in research assistants helping subjects complete the CASI surveys. Two research assistants were in the room with 25 computer stations. Research staff was available to provide assistance with the computer as needed and to save the survey and clean the work stations at the end of the interview. Interviews were completed in approximately 1 h.
2.4.2. Clinician-administered interviewing
The CAPS and SCID-NP (administered only during the screening interview) were administered in a private room by master’s-level, clinically trained social workers or psychologists and one bachelor’s-level researcher with 3 years of experience administering psychological instruments. Interviewers were trained and supervised by doctoral-level researchers with experience administering these instruments in clinical and research settings. Interviews were conducted in private rooms and were completed in approximately 2 h.
2.4.3. Focus groups
Focus groups were conducted with participants who completed the interventions to elicit their opinions about the intervention and group experience. Prior to the focus groups, participants were asked to complete the Client Satisfaction Questionnaire (Larsen, Attkisson, Hargreaves, & Nguyen, 1979), and the End-of-Treatment Questionnaire (Najavits, 1994). Focus groups were conducted with five to 10 participants from the same intervention group, lasted approximately 45–60 min, were audio-taped and transcribed, and were conducted within 1 week of completing the program.
2.5. Assignment procedure
Participants were screened over a 12-month period and assigned to SS or M-TREM within 3 months of being determined eligible for the study (see Fig. 2). Participants were assigned to groups in four cohorts; the first two cohorts (1 and 2) were assigned randomly first to either waitlist or treatment, then to either SS or M-TREM in blocks of 4 (2 to SS and 2 to M-TREM) and the second two cohorts (3 and 4) were assigned based on preference. Participants in cohorts 3 and 4 were shown an informational brochure describing the interventions in terms of content areas, materials, and expectations (e.g., homework). After reviewing the information brochures, they selected an intervention. Participants selecting SS (52% chose SS) reported a preference for handouts to read and keep, while those selecting M-TREM (48%) preferred no reading homework and the coverage of “male messaging.” For the first two cohorts, there were eight concurrent groups; four SS and four M-TREM; for the third cohort, there were five SS and four M-TREM groups, with one SS and one M-TREM group in cohort 4. Groups were closed after the first week. All groups started the same week; start dates and times were determined administratively.
Fig. 2.
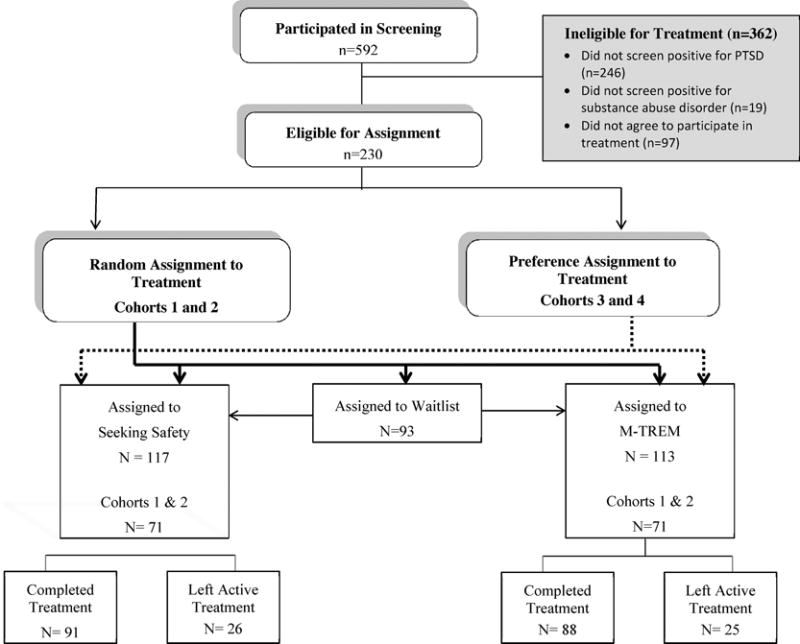
Participation, assignment to treatment, and retention.
2.6. Intervention
Both SS and M-TREM interventions were organized in (closed) group sessions (~8–13 subjects per group) and were available in English only. Therapists received structured training in either SS or M-TREM and were blind to the other intervention. Therapists had master’s-level training in social work or psychology with expertise in trauma and substance abuse disorders. Two therapists led the 14 SS groups and three therapists led the 13 M-TREM groups held from April 2012 to September 2013. The SS therapists completed the DVD SS training modules, received a 2-day structured training by an associate of Dr. Lisa Najavits, founder of SS, and were supervised by a Ph.D. level clinician (associate of Dr. Najavits) with over 10 years of experience in trauma counseling. The M-TREM therapists received a 2-day structured training provided by Dr. Roger Fallot, the co-founder of M-TREM, who supervised the group leaders during the intervention. Supervision was provided every week for 1 h and 5% of sessions were randomly audio-taped and reviewed by either Dr. Roger Fallot or an associate of Dr. Najavits, with written feedback provided to therapists.
The SS participants were provided with a composition book, pen, and SS manual. Of the 25 handouts within the manual, 23 (excluding handouts on Community Resources and the Life Choices Game) were organized in a spiral binder. The order of the first eight handouts was predetermined (order: Safety, PTSD, Grounding, Substances, Boundaries, Anger, Self-Nurturing), after which handouts were selected by group preference. The M-TREM participants received a composition book and pen. M-TREM includes 24 sessions that are motivated by discussion questions written on an easel. Each intervention comprised 28 sessions, with several topics/handouts covered in two sessions. Groups met for 90-min, twice a week for 14 weeks (a 42-h intervention). Because cohort 1 participants expressed frustration about not being permitted to talk about their traumas (other than brief “headlining”), participants in cohorts 2 through 4 were provided with an optional group session in which they could talk in more detail about their trauma experiences. Attendance to this session was optional, and its timing was determined by the group members in collaboration with the group leader but after completing the first eight sessions.
2.7. Sample size
Our primary outcome is PTSD symptom severity over time measured by the CAPS. We used the CAPS total score as the dependent variable and the baseline CAPS score as a covariate, with intervention group (SS or M-TREM vs. wait-list) as the between-subjects factor. Prior studies indicate that the average standardized post-treatment effect size (d) for SS or M-TREM is medium, that is a half standard deviation reduction in mean CAPS scores (i.e., roughly a 10 point decline on the CAPS for the treatment group). We estimated power for analysis of covariance (ANCOVA) with an effect size f = .25, α = .05 two-tailed, and a correlation between baseline and post-treatment CAPS = .50. We used n = 40 for the intervention group (Cohort 1) and n = 80 for the control group (wait-list), and find power = .81. This is the fewest number of cases for tests of the pre-vs. post-treatment effect, but it is sufficient to detect the treatment effect of the interventions compared to wait-list controls. Subsequent cohorts or combined waves have larger n’s and additional power, even when attrition is taken into account. Larger samples sizes (n ~ 300) are required for head-to-head intervention comparisons, especially when treatments are similar in their effectiveness (Schnurr, 2008). For this reason, we consider the head-to-head comparisons preliminary and use trajectories of change analyses to more fully explore the data.
2.8. Analysis
Baseline differences between samples and groups were analyzed using chi-square or Fisher’s exact tests for categorical data and t-tests for continuous variables. Intent-to-treat and completer sample analyses were conducted. People “completed” the intervention if they had attended at least half of the sessions and attended sessions during the first and last weeks of the program.
The primary outcome variables were pre-post intervention change in the mean score for the PCL-C, CAPS, and GSI (mean of all 53 items of the BSI), and the percent of sample with current full and sub-threshold PTSD (based on the CAPS). The SES, PCI, and GPEF scores assessed changes in the secondary outcome variables pre-post intervention. The pre- and post-scores were used in the analysis. To test for the (absolute) effectiveness of treatment, the control group was the waitlist group – participants who screened positive but were assigned to intervention groups 3 months post-screening. This group completed the baseline survey twice, 3-months apart. Two methods were used to test for absolute effectiveness: (1) t-test for continuous variables and the Cochran–Armitage test for trend for categorical variables and (2) ANCOVA or logistic regression using the baseline measure for the outcome of interest as a covariate. Regression analysis was also used to control for differences between the waitlist and treatment groups and to test for outcome differences by intervention type. The effect size was calculated from the ANCOVA using eta squared (proportion of the total variance explained by the full model) and partial eta squared (proportion of the total variance attributed to the treatment factor only). The benchmarks defined by Cohen (1969, pp. 278–280) to define small, medium, and large effects for the partial eta squared are, respectively, 0.0099, 0.0588, and 0.1379.
To test for the relative effectiveness between interventions over time, we first employed a repeated measures ANCOVA for the intent-to-treat and completer samples. Here, we compared post-intervention outcomes by condition while controlling for differences on the same measure between groups at baseline or between groups resulting from attrition. The repeated measures analyses included all data points (baseline, 3-, 6-, and 9-months) to maximize power, and explored the main effects of time and intervention, and two-way interactions between time and intervention. Next, to more rigorously examine the effect of treatment on outcomes, hierarchical linear modeling was used to account for dependence among interviews within the same person, which would underestimate the standard errors and inflate the significance of estimators. HLM adjusts for the clustering within the individual by fitting a systematic time trajectory with a random error. The dependent variables are the primary and secondary outcomes. All these variables are continuous.
In our preliminary analysis, the level-1 predictors had similar impacts on the outcome variables across time. The intercept is the only level-1 coefficient treated as random and modeled at level-2 (Raudenbush & Bryk, 2002). The level-1 variables were time, measured at 0, 1, 2, 3, 4, 5 corresponding to pre-baseline1, pre-baseline2, baseline, T1, T3, T6) and treatment (assigned to SS or M-TREM, compared to no assignment). Level-2 coefficients were entered to control for between group differences in lifetime alcohol abuse and both alcohol and substance dependence, and preference assignment (vs. random assignment). Dichotomous predictors entered in the original format. The mathematical formula for the hierarchical linear model is as the following:
Level 1: Yti = π0i + π1iTimeti + π2iSSti + π3iMTREMti + ∈ti
Level 2: π0i = β00 + β01Alcsubdep1i + β02Alcabu2i + β03Assign3i + γ0i where γ0i ~ N(0, τ00)
where Yti represents the continuous scale (PCL-C, CAPS, GSI, SES, PCI, GPEF) that interview t of participant i reported, the π s represent the level-1 coefficients, in which π0i is the intercept of the level-1 equation and other variables are fixed-effect predictors (e.g., time, intervention), π0i is the only coefficient modeled in level-2 with intercept β00 and predictors, and γ0i is the level-2 error term, which is assumed to be normally distributed with mean 0 and variance τ00.
The models include three independent (individual-level) variables. We examined the effect of multicollinearity by using weighted least squares regression. All the independent variables have tolerance values greater than 0.6, which suggests that multicollinearity does not bias the estimation of individual level parameters in the models. Means and percentages were estimated on the basis of valid numbers. The significance level used to assess the validity of null hypotheses was p < 0.05 and p < 0.01. Proc means, freq, ttest, glm, logistic and mixed of SAS 9.3 were used to construct all statistics.
3. Results
Table 1 provides demographic and criminal history information for the treatment and waitlist samples. With the exception of age and veteran status (active duty), there were no significant differences among measured attributes. The only significant differences between the attributes of the completer (n = 179) and non-completer (n = 51) samples were years incarcerated, with completers having served more years in prison compared to the non-completers (16.2 years vs. 12.6 years, p = 0.023), and drug offense status, non-completers were more likely to have a drug offense charge (22.5% vs. 11.2%, p = 0.043 from chi-square test and p = 0.059 from Fisher’s exact test). The ITT sample included 230 males who were predominately middle age (mean age = 42.5), African American, had at least a high school diploma or GED, were convicted of a violent crime, and had served, on average, 15 years in prison. Roughly half the sample each participated in SS (n = 117) or M-TREM (n = 113), and there were no significant differences between these treatment groups in terms of demographic or criminal history characteristics (see Table 2). The clinical and trauma characteristics of the ITT and completer samples appear in Table 3. Again, with the notable exception of lifetime alcohol abuse and lifetime alcohol and substance dependence, there were no significant differences in the trauma and behavioral health characteristics between the SS and M-TREM samples. There was one significant difference between the completers and non-completers; completers were more likely to report a serious injury due a sexual assault (34.9% vs. 0%, p = 0.046 from Fisher’s exact test).
Table 1.
Demographic and criminal history characteristics: treatment and waitlist samples.
| Characteristics | Intent-to-treat sample, N=179
|
Treatment sample, N=86
|
|||
|---|---|---|---|---|---|
| Full sample, N=179 | Waitlist sample, N=93 | Treatment sample, N=86 | Seeking Safety, N=42 | M-TREM, N=44 | |
| Age years, mean (±SD) | 43.0 (12.9) | 40.0** (12.4) | 46.3 (12.7) | 44.8 (11.0) | 47.7 (14.1) |
| Race/ethnicity, % | |||||
| Black/African American | 48.3 | 48.9 | 47.7 | 35.7* | 59.1 |
| Caucasian | 34.8 | 34.8 | 34.9 | 40.5 | 29.6 |
| Latino/Hispanic | 10.1 | 9.7 | 10.5 | 14.3 | 6.8 |
| Other | 16.9 | 16.3 | 17.4 | 23.8 | 11.4 |
| Education, % | |||||
| No high school or GED | 17.3 | 18.3 | 16.3 | 19.1 | 13.6 |
| High school or GED | 49.2 | 53.8 | 44.2 | 35.7 | 52.3 |
| Any college | 32.4 | 28.0 | 37.2 | 40.5 | 34.1 |
| Veteran, active duty, % | 25.6 | 16.7** | 34.9 | 33.3 | 36.4 |
| Years incarcerated since 18, mean (±SD) | 15.7 (12.2) | 14.5 (11.2) | 17.0 (13.2) | 16.5 (11.9) | 17.4 (14.5) |
| Violent crime, % | 59.3 | 56.5 | 62.4 | 61.9 | 62.8 |
| Drug crime, % | 13.6 | 17.4 | 9.4 | 11.9 | 7.0 |
Note. All mean and percentages are based on valid numbers.
p < 0.05 using t-test, chi-square, or Fisher’s exact test.
p < 0.01.
Table 2.
Demographic and criminal history characteristics: intent-to-treat and completer samples.
| Characteristics | Intent-to-treat sample, N= 230
|
Completer sample, N=179
|
||||
|---|---|---|---|---|---|---|
| Full sample, N=230 | Seeking Safety, N=117 | M-TREM, N=113 | Full sample, N=179 | Seeking Safety, N=91 | M-TREM, N=88 | |
| Age years, mean (±SD) | 42.5 (12.5) | 41.9 (11.7) | 43.2 (13.3) | 43.8 (12.5) | 42.4 (11.6) | 45.2 (13.2) |
| Race/ethnicity, % | ||||||
| Black/African American | 51.8 | 47.0 | 56.6 | 52.3 | 48.9 | 55.7 |
| Caucasian | 32.5 | 34.8 | 30.1 | 32.0 | 34.4 | 29.6 |
| Latino/Hispanic | 10.0 | 9.4 | 10.6 | 10.6 | 9.9 | 11.4 |
| Other | 15.8 | 18.3 | 13.3 | 15.7 | 16.7 | 14.8 |
| Education, % | ||||||
| No high school or GED | 18.3 | 20.5 | 15.9 | 15.6 | 15.4 | 15.9 |
| High school or GED | 50.0 | 47.0 | 53.1 | 52.5 | 52.8 | 52.3 |
| Any college | 30.4 | 30.8 | 30.1 | 30.2 | 29.7 | 30.7 |
| Veteran, active duty, % | 22.0 | 21.9 | 22.1 | 23.6 | 23.3 | 23.9 |
| Years incarcerated since 18, mean (±SD) | 15.4 (12.0) | 15.1 (11.2) | 15.7 (12.8) | 16.2 (12.6) | 15.6 (11.6) | 16.8 (13.7) |
| Violent crime, % | 56.4 | 56.0 | 56.8 | 59.0 | 60.4 | 57.5 |
| Drug crime, % | 13.7 | 11.2 | 16.2 | 11.2 | 9.9 | 12.6 |
Note: All mean and percentages are based on valid numbers.
Table 3.
Clinical characteristics: intent-to-treat and completer samples.
| Characteristics | Intent-to-treat sample, N=230
|
Completer sample, N=179
|
||||
|---|---|---|---|---|---|---|
| Full sample, N=230 | Seeking Safety, N=117 | M-TREM, N=113 | Full sample, N=179 | Seeking Safety, N=91 | M-TREM, N=88 | |
| Lifetime substance use, % | ||||||
| Dependence | ||||||
| Alcohol | 49.8 | 55.8 | 43.8 | 49.7 | 55.7 | 43.7 |
| Substances | 65.0 | 68.4 | 61.6 | 66.5 | 71.9 | 60.9 |
| Both alcohol and substances | 41.2 | 49.1* | 33.0 | 40.9 | 49.4* | 32.2 |
| Abuse | ||||||
| Alcohol | 18.2 | 10.6** | 25.9 | 20.6 | 11.4** | 29.9 |
| Substances | 16.4 | 14.0 | 18.8 | 15.9 | 12.4 | 19.5 |
| Both alcohol and substances | 4.4 | 1.8 | 7.1 | 5.1 | 2.3 | 8.1 |
| Serious mental illness, % | 62.0 | 60.5 | 63.4 | 63.6 | 61.8 | 65.5 |
| Other mental illnesses, % | 22.1 | 23.7 | 20.5 | 22.2 | 24.7 | 19.5 |
| PCL-C total score, mean (SD) | 44.0 (13.2) | 44.4 (13.5) | 43.6 (12.9) | 44.0 (13.3) | 44.8 (13.5) | 43.2 (13.1) |
| CAPS total score, mean (SD) | 44.2 (28.5) | 44.2 (29.5) | 44.1 (27.5) | 44.6 (28.6) | 45.8 (29.1) | 43.4 (28.3) |
| Trauma age of onset, mean (SD) | 14.3 (8.8) | 14.0 (8.8) | 14.6 (8.9) | 14.0 (9.1) | 13.6 (8.7) | 14.5 (9.5) |
| Trauma event type, % | ||||||
| Physical | 78.3 | 79.5 | 77.0 | 78.2 | 82.4 | 75.0 |
| Sexual | 22.6 | 23.1 | 22.1 | 24.0 | 25.3 | 22.7 |
| Both physical and sexual | 20.4 | 21.4 | 19.5 | 22.4 | 24.2 | 20.5 |
| Level of harm, physical, % | ||||||
| Life threatening | 96.1 | 95.7 | 96.6 | 95.7 | 96.0 | 95.5 |
| Serious injury | 77.8 | 74.2 | 81.6 | 76.4 | 73.3 | 80.3 |
| Threat to physical integrity | 7.2 | 6.5 | 8.1 | 7.9 | 8.0 | 7.6 |
| Level of harm, sexual, % | ||||||
| Life threatening | 38.5 | 29.6 | 48.0 | 41.9 | 30.4 | 55.0 |
| Serious injury | 28.9 | 18.5 | 40.0 | 34.9 | 21.7 | 50.0 |
| Threat to physical integrity | 98.1 | 96.3 | 100 | 97.7 | 95.7 | 100 |
| Childhood trauma, % | ||||||
| Physical | 75.1 | 74.4 | 75.9 | 74.9 | 76.9 | 72.7 |
| Sexual | 26.2 | 29.1 | 23.2 | 26.8 | 30.8 | 22.7 |
| Both | 23.1 | 25.6 | 20.5 | 23.5 | 27.5 | 19.3 |
| Adult trauma, % | ||||||
| Physical | 10.0 | 10.3 | 9.8 | 8.9 | 7.7 | 10.2 |
| Sexual | 3.1 | 4.3 | 1.8 | 3.4 | 5.5 | 1.1 |
| Both | 0.9 | 1.7 | 0 | 1.1 | 2.2 | 0 |
Note: All mean and percentages are based on valid numbers.
p < 0.05,
p < 0.01 comparing SS group to M-TREM group using t-test, chi-square, or Fisher’s exact test.
3.1. Adherence, retention, attendance, and group cohesion
Fidelity to the intervention manual was assessed through expert review of group sessions that were randomly audio-recorded. For Seeking Safety, 50 tapes were reviewed by a SS expert using the SS Adherence Scale Score sheet, which rates format, content, and process on a 4-point scale (0–3) for adherence/helpfulness. The total fidelity scores ranged from 40.8 to 52.5, with a mean of 48.8 (81%). Mean scores for the three domains were as follows: 2.34 for format, 2.35 for content, and 2.53 for process. Fidelity to the M-TREM intervention was reviewed by Dr. Fallot using the TREM Group Intervention Fidelity Scale, which assesses control, activity, question/comment ratio, session structuring, general psycho-education, trauma-specific education, empowerment and affirmation, positive problem-solving, leadership style, and goal achievement. These criteria are rated on a weighted 3-point scale (1, 3, or 5) for a maximum score of 80. Total scores for 20 audio-recorded sessions (randomly selected from a sample of 50) reviewed ranged from 44 to 80, with a mean of 66 (83%). Domains evaluated with an average score less than 5 were: session structuring , general psycho-education , trauma-specific education , and empowerment and affirmation , and leadership style .
In terms of retention, over three-quarters (78%) of participants assigned to SS (91 of 117) and M-TREM (88 of 113) completed the intervention. Exit interviews were conducted with non-completers. Of those who voluntarily dropped out and agreed to an exit interview (n = 51), the reasons provided were: did not wish to continue the work (n = 5); had scheduling conflicts (n = 5); moved to another prison, halfway house, or community (n = 13); and unspecified reasons (n = 28).
The SS and M-TREM completers, on average, attended, respectively, 87% and 86% of the 28 sessions (SS range = 11–28 and mean = 21; MTREM range = 11–26 and mean = 21). Variation in number of sessions existed across the groups due to prison conditions that limited prisoner movement within the facility. Excused individual absences included unit lock down, medical or court visits, movement disruptions, other unavoidable movement restrictions.
Group cohesion was explored in the focus groups. When asked to describe the group experience, words commonly used, independent of SS or M-TREM, were “safe,” “trusted,” “comfortable,” “open,” “honest,” and “non-judgmental.” SS participants reported “it was easy to feel comfortable to share,” “everybody was kinda quiet and then … we started opening up,” “we had so many similar issues,” it was “just a safe place,” they “got a lot of support from the group,” “that the honesty was contagious,” “everyone got a chance to share,” “we are forever linked with each other … we built a bond,” “we formed a relationship in here of trust, honesty and support and safety,” “this group is my family,” “the trust and the safety in this group was so powerful,” “we all came as one, like we all became comfortable enough to open up with each other and to put some type of trust in what we can tell each other … it stayed in this little circle,” and “there’s trust in this room, and a high level of respect.” Similar sentiments were expressed by M-TREM participants who reported they “felt safe,” “didn’t look at [each other] as another inmate, another number, another fella … we were actually people,” “could be honest with [the other group members] because we trusted each other,” “developed some new friendships” with group members, felt “nobody’s judging” and “everybody kept what was [said in group] inside the [group],” “got helpful information from group members” and “that people cared … and there was commonality across all the hurt,” experienced an “openness [that] brought us close,” built “camaraderie” and “learned to trust [each other].” One of the things participants most liked about the intervention was their groups, and what they least liked was the disbanding of their group. May reported that the ending of the group was “traumatic.”
3.2. Absolute effectiveness of treatment (compared to no treatment)
Table 4 presents comparisons for primary and secondary outcomes between the treatment and waitlist groups. Within the treatment group, there was significant improvement on all outcome variables compared to baseline measures. Most importantly, the mean score on the CAPS (PTSD severity) declined by 13 points (clinical significance is a 10-point decline (Schnurr et al., 2003)) and the percent of men with full-PTSD declined by 19% points. For the waitlist group, significant improvement was found for PTSD and mental health symptoms and self-efficacy over the 3-month waiting period. However, the level of clinical improvement in terms of PTSD severity was less substantive, with a 3-point decline in the mean CAPS score and a 10% point decline in the presentation of full-PTSD among the waitlist group. ANCOVA and t-tests (Cochran–Armitage trend test for categorical variables) were used to test whether incarcerated men who received treatment (SS or M-TREM) for 3 months differed on primary and secondary outcomes from those assigned to the waitlist at 3 months post baseline measurement. Significant improvements were found for the treatment group on CAPS total score and self-esteem based on simple t-test comparisons but, after controlling for differences in baseline measures, no differences between groups were detected for primary or secondary outcomes.
Table 4.
Mean comparisons of primary and secondary outcomes at baseline and end of intervention (or 3 months post-baseline) between treatment and control groups.
| Primary and secondary outcome measures |
Treatment group (Seeking Safety or M-TREM) |
Control group (waitlist)
|
Difference between treatment and control |
Effect size
|
||||
|---|---|---|---|---|---|---|---|---|
| Baseline, N=86 | Post-treatment completion, N=86 |
Baseline, N=93 |
3-Months post- baseline, N=93 |
t-Test p-value |
ANCOVA p-value |
Partial Eta-square |
Model Eta-square |
|
| Primary | ||||||||
| PCL-C, mean (SD) | 47.6 (11.8) | 40.2** (13.7) | 44.9 (12.2) | 40.4** | 0.103 | 0.250 | 0.0078 | 0.34 |
| CAPS score, mean (SD) |
N=83 53.0 (27.9) |
N=83 39.6** (28.3) |
N=90 43.8 (30.0) |
N=90 39.3 (26.5) |
0.017* | 0.106 | 0.0160 | 0.43 |
| PTSD full, % |
N=82 59.5 |
N=82 40.5** |
N=84 43.8 |
N=84 34.8 |
0.151a | 0.629b | ||
| PTSD sub-threshold, % |
N=84 10.7 |
N=84 10.7 |
N=89 13.5 |
N=89 18.0 |
0.492a | 0.206b | ||
| PTSD full or sub, % | 70.2 | 51.2** | 57.3 | 52.8 | 0.051a | 0.204b | 0.0054 | 0.49 |
| GSI, mean (SD) | 1.18 (0.64) | 0.89** (0.68) | 1.02 (0.56) | 0.84** (0.53) | 0.128 | 0.338 | ||
| Secondary | ||||||||
| SES, mean (SD) | 18.5 (5.27) | 19.9** (5.53) | 18.9 (5.44) | 19.2 (5.16) | 0.049* | 0.058 | 0.0210 | 0.55 |
| PCI, mean (SD) | 2.71 (0.52) | 2.87** (0.56) | 2.70 (0.54) | 2.77 (0.54) | 0.086 | 0.072 | 0.0189 | 0.67 |
| GPEF, mean (SD) | 2.92 (0.54) | 3.10** (0.54) | 3.01 (0.46) | 3.10* (0.45) | 0.199 | 0.397 | 0.0042 | 0.36 |
p < 0.05,
p < 0.01 comparing “post” measure to baseline measure using paired t-test or McNemar test.
Cochran–Armitage trend test.
Logistic regression.
Regression analysis was used to identify differences (pre-post) in outcomes between the waitlist and treatment (SS, M-TREM) groups controlling for differences in age, veteran status, and outcome measures at baseline (see Table 5). A significant difference was found between M-TREM and the waitlist group for the CAPS outcome (improved PTSD severity). Significant improvements were found on mental health symptoms (GSI), self-esteem (SES) and proactive coping skills (PCI) for the SS group compared to the wait-list group.
Table 5.
Regression analysis of any treatment effect on primary and secondary outcomes for treatment and control (waitlist) groups.
| Characteristics | Regression coefficients
|
|||||
|---|---|---|---|---|---|---|
| Primary outcomes
|
Secondary outcomes
|
|||||
| PCL-C, N=170 | CAPS, N=163 | GSI, N=170 | SES, N=170 | PCI, N=170 | GPEF, N=170 | |
| Age | −0.10 | −0.00007 | −0.002 | 0.005 | −0.002 | −0.003 |
| Veteran, active dutya | 2.65 | 4.83 | 0.08 | −0.07 | 0.02 | −0.01 |
| Seeking Safetyb | −3.70 | −3.87 | −0.19* | 1.40* | 0.14* | 0.09 |
| M-TREMb | 0.12 | −8.36* | 0.05 | 0.63 | 0.06 | 0.06 |
| Baseline measure of outcome | 0.61** | 0.61** | 0.70** | 0.75** | 0.85** | 0.60** |
| Model statistics | Df=5 | Df=5 | Df=5 | Df=5 | Df=5 | Df=5 |
| F= 19.44 | F= 24.13 | F=35.20 | F=41.36 | F= 68.63 | F= 18.45 | |
| P<0.0001 | P<0.0001 | P<0.0001 | P<0.0001 | P<0.0001 | P<0.0001 | |
| Effect size | ||||||
| Eta-square | 0.37 | 0.43 | 0.52 | 0.56 | 0.68 | 0.36 |
| Omega-square | 0.35 | 0.41 | 0.50 | 0.54 | 0.67 | 0.34 |
| 95% Confidence limits | (0.24,0.45) | (0.30,0.51) | (0.40,0.59) | (0.45,0.62) | (0.59,0.73) | (0.23,0.44) |
Note: N varies across models due to missing data.
Compared to no active duty.
Compared to no treatment.
p < 0.05.
p < 0.01.
3.3. Treatment comparative effectiveness
Intent-to-treat analysis was conducted on primary and secondary outcomes using two-way repeated measures of ANCOVA. We tested for main effects of intervention, time, and interaction effects between intervention and time. Across all outcome measures, there were no significant main effects for treatment except for self-efficacy (GPEF), indicating that M-TREM and SS performed equivalently on primary outcomes and two of the three secondary outcomes. Main effects for time were significant for all outcome measures, indicating that all incarcerated men showed significant improvement on PTSD and mental health symptom outcome measures, as well as self-esteem, prosocial coping skills, and self-efficacy outcomes regardless of whether they participated in SS or M-TREM. In terms of PTSD severity, over time (baseline to 6-months post-intervention), PTSD severity (measured by the CAPS) declined, on average, by 19 points for SS and 21 points for M-TREM, and the presentation of full PTSD declined by approximately 28% points for SS and M-TREM. Results were replicated with the completer sample (completer sample results are available from the first author upon request) (Table 6).
Table 6.
Mean comparisons of primary and secondary outcomes for intent-to-treat sample.
| Primary and secondary outcomes | Seeking Safety
|
M-TREM
|
Statistical test | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Treatment
|
Follow-up
|
Treatment
|
Follow-up
|
||||||
| Baseline, N=116 | End of treatment, N=93 | 3-Month, N=94 | 6-Month, N=87 | Baseline, N=113 | End of treatment, N=91 | 3-Month, N=87 | 6-Month, N=84 | ||
| Primary outcomes | |||||||||
| PCL, mean (SD) | 44.4 (13.5) N=115 | 38.8 (13.6) N=93 | 38.2 (14.1) N=92 | 36.6 (15.8) N=86 | 43.6 (12.9) N=111 | 38.1 (14.1) N=90 | 36.4 (14.6) N=87 | 36.0 (13.3) N=84 | IC: F(1,227) =0.06, ns Time: F(3,227)=26.08** X: F(3,227)= 0.25, ns |
| CAPS score, mean (SD) | 44.2 (29.5) N=111 |
33.2 (26.9) N=89 |
27.8 (24.7) N=92 |
25.4 (25.4) N=83 |
44.1 (27.5) N=109 |
27.5 (25.7) N=91 |
25.2 (24.9) N=85 |
23.2 (24.3) N=81 |
IC: F(1,223) =0.01, ns Time: F(3,223)=50.80** X: F(3,223)= 0.60, ns |
| PTSD full, % | 47.4 N=114 |
32.2 N=90 |
18.5 N=92 |
18.8 N=85 |
42.0 N=112 |
23.1 N=91 |
12.8 N=86 |
14.5 N=83 |
|
| PTSD full or sub, % | 62.3 | 44.4 | 39.1 | 31.8 | 59.8 | 31.9 | 32.6 | 25.3 | |
| GSI, mean (SD) | 1.03 (0.64) | 0.80 (0.65) | 0.80 (0.66) | 0.84 (0.80) | 1.00 (0.62) | 0.82 (0.67) | 0.76 (0.68) | 0.68 (0.54) | IC: F(1,227) =0.05, ns Time: F(3,227)=17.99** X: F(3,227)= 1.88, ns |
| Secondary outcomes | |||||||||
| SES, mean (SD) | 18.3 (5.12) | 20.1 (5.32) | 20.5 (5.04) | 20.0 (5.12) | 18.9 (5.58) | 20.1 (5.86) | 20.9 (6.01) | 21.1 (5.99) | IC: F(1,227)=3.38, ns Time: F(3,227)=13.81** X: F(3,227)= 0.84, ns |
| PCI, mean (SD) | 2.70 (0.57) | 2.88 (0.58) | 2.91 (0.49) | 2.93 (0.49) | 2.75 (0.54) | 2.82 (0.59) | 2.93 (0.54) | 2.91 (0.56) | IC: F(1,227) =1.40, ns Time: F(3,227)=20.18** X:F(3,227)= 0.47, ns |
| GPEF, mean (SD) | 3.03 (0.55) | 3.18 (0.55) | 3.16 (0.51) | 3.19 (0.47) | 2.94 (0.53) | 3.06 (0.59) | 3.11 (0.58) | 3.12 (0.56) | IC: F(1,227) =7.76** Time: F(3227)=10.90** X: F(3,227)= 0.43, ns |
p < .01.
To account for the nesting of data within individuals over time and in groups, HLM regression was used to examine the effects over time and within group (level 1 predictors), controlling for known differences between groups (level 2 predictors). Again, as shown in Table 7, PTSD severity (PCL and CAPS), mental health symptoms, and proactive coping significantly improved over time. Similarly, both intervention groups were associated with significant improvements in the primary outcome and secondary measures, compared to the no treatment group. There was no significant effect of preference assignment on outcomes.
Table 7.
Hierarchical linear model regression coefficients for primary and secondary outcome measures.
| Characteristic | Primary outcome measure (n=225)
|
Secondary outcome measure (N=225)
|
||||
|---|---|---|---|---|---|---|
| PCLa | CAPSa, N=223 | GSIa | SES | PCI | GPEF | |
| Level 1 predictors | ||||||
| Time | −1.56** | −3.09** | −0.05* | 0.12 | 0.04** | 0.02 |
| Any Seeking Safety (0=no tx) | −3.77** | −9.60** | −0.17** | 1.27** | 0.09* | 0.09* |
| Any M-TREM (0=no tx) | −3.24** | −9.20** | −0.15* | 1.25** | 0.07* | 0.10* |
| Level 2 predictors | ||||||
| Lifetime alcohol and substance dependence (0=no LSD) | 2.95 | 5.74 | 0.08 | −0.52* | −0.12 | −0.11 |
| Lifetime alcohol abuse (0=no LSA) | 0.80 | −0.33 | 0.03 | 0.82 | 0.07 | −0.04 |
| Preference assignment (cohort 3 and 4) (0=randomization; cohort 1 and 2) |
0.70 | −3.39 | 0.09 | −0.48 | −0.04 | 0.01 |
| Test statistics for random intercept or likelihood ratio test for HLM regression | ||||||
| Reliability | 0.845 | 0.857 | 0.860 | 0.875 | 0.901 | 0.841 |
| Chi-square | 1620.5 | 1695.8 | 1859.5 | 2078.4 | 2609.3 | 1594.6 |
| Df | 221 | 219 | 221 | 221 | 221 | 221 |
| p-Value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
p < 0.05.
p < 0.01.
Models were estimated using HLM.
To further explore the effect of cohort on the PTSD severity over time, we estimated a mixed model with all possible interactions between time and cohort, controlling for baseline CAPS. Intent to treatment analysis for PTSD severity (CAPS) at baseline, 3 (completed intervention), 6, and 9 months showed significant main effects of time (F2,310 = 3.62, p = 0.028) but not for treatment type (F1,168 = 2.02; p = 0.1571) or cohort (F3,170 = 1.37; p = 0.2536). None of the two-way or three-way interactions were significant. There were no differences between treatment effect in other cohorts.
3.4. Satisfaction with treatment
At the conclusion of the intervention, participants completed an end-of-treatment questionnaire, which consisted of questions about their experience with the intervention (SS or M-TREM), and their overall assessment of the materials, facilitator, and discussion groups. The mean score (based on a 4-point Likert scale with 1 = poor and 4 = excellent) for the Client Satisfaction Questionnaire was 3.7 (SD = 0.5) for SS and 3.6 (SD = 0.6) for M-TREM for “quality of the service received;” was 3.1 (SD = 0.7) for SS and M-TREM for “extent to which the intervention met your needs;” was 3.5 (SD = 0.6) for SS and 3.4 (SD = 0.7) for M-TREM for “intervention helped you to deal more effectively with your problem;” was 3.6 (SD = 0.6) for SS and 3.5 (SD = 0.7) for M-TREM for “satisfaction with intervention;” and was 3.8 (SD = 0.4) for SS and 3.8 (SD = 0.5) for M-TREM for “would you recommend the program to a friend.” There were no statistically significant differences in satisfaction between SS and M-TREM programs.
4. Discussion
4.1. Feasibility of treatment implementation
This is the first study to implement and test a group cognitive–behavioral integrated treatment for PTSD and addiction problems in a male prison population. The feasibility evidence is strong. Among the males invited to be screened, 63% (592/944) agreed to participate in screening and, of those, 55% (327/592) screened positive for current PTSD and lifetime substance/alcohol problems. After being informed of their eligibility for treatment, 70% (230/327) of the eligible sample agreed to participate in treatment and 78% (179/230) of those assigned to treatment completed the intervention. Ending treatment prematurely was not always a voluntary choice for participants; 14 participants were moved unexpectedly to other locations or had conflicts with other mandatory programs. Other participants voluntarily left treatment for personal reasons (n = 4); some did not like the group-nature of the intervention (n = 5), while others were not ready to deal with their trauma in prison (n = 1).
Overall, those who completed the group evaluated both SS and M-TREM favorably in terms of group dynamics. They reported feeling safe enough to participate honestly and openly in group discussions. Our ability to recruit and retain participants was enhanced by our practice of engaging men on the housing blocks, and working with and receiving endorsement from inmate organizations within the prison. There was considerable skepticism about the study and researchers initially but these sentiments declined over time once the staff and inmates had opportunities to interact with the research staff. Physical presence of the research staff on a day-to-day basis was vital for implementation.
4.2. Effectiveness
Overall, study results modestly support the effectiveness of SS and M-TREM for incarcerated males. In terms of absolute effectiveness (waitlist comparison), participants receiving integrated treatment (SS or M-TREM) showed statistically and clinically significant improvement in PTSD symptom severity over time, although the difference in improvements was not statistically significant compared to the waitlist group (controlling for baseline differences) and the effect size was small.
When treatment was disaggregated by intervention type, the effect of M-TREM on PTSD severity was double that found for SS (regression coefficient −8.36 vs. −3.87) and significantly different from the waitlist group. SS was found to outperform no treatment on three outcomes: mental health symptoms, self-esteem, and proactive coping. In terms of relative effectiveness (head-to-head comparison between SS and M-TREM), based on intent-to-treat and completer analyses, no statistical differences were found between the performance of SS and M-TREM on primary or second outcomes; both were associated with significant improvements in primary and secondary outcomes over time, but neither was superior to the other intervention on these measures.
These effects were tested more rigorously using HLM regression, which maximizes the use of longitudinal data (increasing power) and controls for the nesting of data within individuals and groups. These analyses revealed significant improvements in PTSD symptom severity over time and in mental health symptom severity, as well as self-esteem, proactive coping, and self-efficacy for both SS and M-TREM, compared to no treatment. No cohort or preference effects were found.
4.3. Study strengths
Putting the results of this study in context is critical to understanding their meaning. First, our goals were to test whether it was feasible to treat concurrent PTSD and addiction disorders among incarcerated men with a manualized group intervention and whether integrated cognitive–behavioral group therapy improved psychological symptoms and function for incarcerated men with comorbid PTSD and addiction disorders. In terms of feasibility, we were able to screen and recruit participants to the study without incident or difficulty. A representative and large sample of male residents from a maximum security prison volunteered to be screened, agreed to participate in treatment, and completed the treatment without incentives. Groups of roughly equal size met regularly and privately without movement or custody issues. One of the strengths of the study was our ability to minimize threats to internal validity by retaining participation and randomly assigning people to equal sized control and comparison groups, while also maintaining high levels of ecological validity in terms of setting (Schmuckler, 2001).
The manualized interventions were delivered with fidelity, enhancing external validity. Both SS and M-TREM were administered with strong adherence to their respective manuals with one notable exception: one voluntary exposure therapy session was added in response to strong participant sentiment. Not offering the session threatened participation and group cohesion. That exposure therapy was prioritized by the participants suggests that adding exposure therapy to an integrated cognitive–behavioral (group) intervention may be feasible among some incarcerated men. Also, the “dosage” was standardized: closed groups and strict attendance policy. Warnings were given to participants who had more than two unexcused absences (excused absences [e.g., legal or personal visits, medical appointments, illnesses] were monitored but not sanctioned). Earlier studies of M-TREM and SS abbreviated or hybridized the interventions (Amaro et al., 2007; Ghee et al., 2009; Hein et al., 2004, 2009; Lynch et al., 2012; Toussaint et al., 2007; Zlotnick et al., 2009) or allowed for open group enrollment and/or lenient attendance, adding imprecision to the dosage and weakening group cohesion (Hien et al., 2004, 2009; Lynch et al., 2012; Toussaint et al., 2007; Zlotnick et al., 2009). By standardizing the dose and implementing the manualized intervention to reflect attendance practices inside prison (i.e., mandatory attendance), our study was implemented with a tightly structured design.
Another feasibility and fidelity strength of our study was the use of both random and preference-based assignment to treatment intervention. Increasing attention has focused on gaps between clinical trials and community-based applications arising from differences in populations and treatment strategies. Allowing participants to reveal their preferences for different interventions has the potential to improve recruitment and adherence (and also adheres to correctional practices that allow men to choose involvement in voluntary programs). Since the 1970s, research has explored whether and to what extent preferences for treatment influence outcomes (Devine & Fernald, 1973; Chong, Chen, Naglie, & Krahn, 2009).
In general, empowering patients to choose treatment options has been found to increase their satisfaction with treatment and treatment outcomes (Doherty & Doherty, 2005; Swift & Callahan, 2009), although the size of the treatment effect varies (Glass, Arnkoff, & Shapiro, 2001; Leykin et al., 2007). Our study allowed 40% of participants to choose between SS and M-TREM. We found that, while participants did have preferences related to intervention type in terms of topics covered, reading requirements, and materials provided, their ability to choose did not significantly affect primary or second treatment outcomes. Many of the participants who had the option to choose, however, did acknowledge that the ability to choose made them feel more respected and enthusiastic about the group.
The second goal of our study was to test whether integrated cognitive–behavioral group therapy improved psychological symptoms and function for incarcerated men with comorbid PTSD and addiction disorders. Our study design combined elements of effectiveness designs (e.g., large sample size, manualized interventions, random and preference-based assignment, waitlist and comparison groups) in ways to rigorously test the absolute and relative effectiveness of SS and M-TREM in a realistic correctional environment. This is the first study of its kind to test the psychological effectiveness of (manualized) integrated group treatment for PTSD and addiction problems among incarcerated men in a prison setting.
The effectiveness results are conditioned by analysis, speaking to the importance of sample size, accounting for the nesting of data within individuals and groups, controlling for baseline difference, and including a follow-up period in effectiveness designs (Schnurr, 2008). Using a waitlist control group and no follow-up period, we found no aggregate (any treatment) and a marginal (M-TREM only) effect of treatment on PTSD symptoms, and some significant improvements in general mental health symptoms and psychological functioning for SS. Using intent-to-treat and completer analyses with a 6-month follow-up period, no significant differences were found in the relative performance between SS and M-TREM on primary or secondary outcomes. This finding was not unexpected as the sample size was insufficient to adequately test a head-to-head comparison between similar interventions. That said, it is worth noting that the levels of the outcomes between groups were very similar in magnitude. Yet when longitudinal data were maximized and modeled in ways that reflect the hierarchical nature of the data, we found that SS and M-TREM performed better than no treatment on PTSD and mental health symptom severity and secondary outcomes, and that the benefits from treatment endured over time.
4.4. Study limitations
Notwithstanding these substantial strengths, there are important methodological limitations to our study. First, we did not measure substance abuse outcomes or risk factors to substance abuse use (e.g., motivation to change, addiction-related beliefs). Correctional settings are drug-free zones and any use of drugs or alcohol is a chargeable offense. Researchers are required to inform authorities of any activity related to the use or distribution of drugs or alcohol among inmates. For this reason, we did not inquire about such activities. Future studies with this population might include measures of readiness-to-change and addiction-related thinking to explore intermediary changes that might mediate substance using behavior.
Second, while our follow-up period was standard (6 months), having a longer period would better measure the endurance of the measured changes in psychological well-being. By design, this study focused only on the first stage of PTSD intervention. Preventing relapse to old thinking and encouraging further healing are important steps for future research. Through SS and M-TREM groups, we established group cohesion and safety in a prison setting, which is rare, and to discard such social capital at the end of the 14 weeks is clinically wasteful. Many of the men in our study wanted to continue their trauma recovery with their groups, suggesting such follow-up intervention would be feasible. Adding booster or exposure therapy sessions concurrently or sequentially with SS or M-TREM merit experimentation with this population. Further intervention also may be necessary to preserve the psychological improvements generated by SS and M-TREM over time as prison environments are known for being traumatizing (Miller & Najavits, 2012).
Third, SS and M-TREM groups were facilitated by master’s-level clinicians with expertise in trauma and addiction disorders. They did not have any affiliation with the department of corrections; hence, they were not required to write individualized progress notes. The privacy and confidentiality afforded to the men through civilian facilitators differs substantially and fundamentally from the normal therapeutic relationship with correctional treatment staff inside prison. In the focus groups, respondents were adamant in their views that the clinical staff of the department of corrections could not produce the conditions of safety and confidentiality that they experienced with facilitators provided by the study. This violation of ecological validity threatens the generalizability of our findings and warrants testing whether similar process and outcome effects can be produced using correctional staff as group facilitators. Relatedly, our findings only pertain to incarcerated men who choose to address their trauma and addiction problems through treatment. If integrated PTSD and addiction treatment is made mandatory (for those who screen positive for both disorders), our findings may not be replicated if motivation towards treatment moderates the relationship between the intervention and outcome measures. Again, this requires further exploration.
Finally, three-quarters of our sample was non-minority (Black, Latino, and other) and all were literate in English. Our findings, therefore, do not extend to non-English speaking incarcerated men. Both interventions are available in Spanish but we did not have sufficient resources to include a representative sample of non-English men.
4.5. Future directions
Our findings, in light of the strength of the study design and analysis, cautiously support implementing either SS and/or M-TREM in adult correctional settings for men to improve the psychological wellness of incarcerated men with co-morbid PTSD and addiction problems. Caution is warranted, however, because we do not know whether the external staffing of the group interventions moderated the measured outcomes. The next step, therefore, is to conduct a randomized controlled longitudinal trial (12-month follow-up) that implements SS and/or M-TREM with concurrent or sequential booster or exposure therapy sessions facilitated by correctional treatment staff. Adding exposure therapy has potential given the apparent readiness of some incarcerated men to delve into their traumas and the strength of the effectiveness evidence in support of exposure therapy.
To enhance our understanding of mediating and moderating effects on measured outcomes, future effectiveness research should be guided by a conceptual model describing how process and intermediary variables might directly or indirectly affect primary and secondary outcomes. This would likely expand the study measures to include process (e.g., staff affiliation, expertise, therapeutic style), intermediary (e.g., criminal thinking, addictive thinking, readiness to change, motivation), and outcome (e.g., institutional violations, parole violations, depression, anxiety) variables. Studies designed in this way follow Seligman’s (1995) recommendation that psychotherapy research should merge the ecological realism of effectiveness research with the scientific rigor of efficacy trials.
While much remains unknown about the implementation and effectiveness of integrated PTSD and addiction treatment for incarcerated men, several facts bear repeating. First, there is a need for effective treatments for these comorbid conditions. Upwards of 50% of incarcerated men have moderate to severe symptoms of PTSD and of those, most have co-morbid substance use problems (Wolff et al., 2014). Second, incarcerated men are willing and able to participate in trauma-healing interventions, and manualized interventions can be implemented with fidelity in correctional environments. Third, the psychological health of incarcerated men can be improved through manualized integrated PTSD and addiction disorder interventions. And fourth, the elements of group cohesion – safety, trust, respect, and confidentiality – can be generated within groups of incarcerated men, making group therapy a viable (and cost-effective) form of intervention. At this point, there is insufficient data regarding whether specific interventions, such as Seeking Safety and M-TREM work under real world conditions. To move the field forward, effectiveness research needs to become more complex to reliably and validly inform practice. Getting realistic answers to what works, for whom, and under what conditions is the call of the future.
Acknowledgments
This study was supported by grant R01-MH095206 from the National Institute of Mental Health.
References
- Amaro H, Dai J, Arévalo S, Acevedo A, Matsumoto A, Nieves R, et al. Effects of integrated trauma treatment on outcomes in a racially/ethnically diverse sample of women in urban community-based substance abuse treatment. Journal of Urban Health. 2007;84:508–522. doi: 10.1007/s11524-007-9160-z. http://dx.doi.org/10.1007/s11524-007-9160-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake D, Weathers FW, Nagy LN, Kaloupek DG, Klauminzer G, Charney DS, Keane TM. A clinician rating scale for assessing current and lifetime PTSD: the CAPS-1. The Behavior Therapist. 1990;13:187–188. [Google Scholar]
- Boden MT, Kimerling R, Jacobs-Lentz J, Bowman D, Weaver C, Carney D, et al. Seeking safety treatment for male veterans with a substance abuse disorder and PTSD symptomatology. Addiction. 2012;107:578–586. doi: 10.1111/j.1360-0443.2011.03658.x. http://dx.doi.org/10.1111/j.1360-0443.2011.03658.x. [DOI] [PubMed] [Google Scholar]
- Brady KT, Dansky BS, Sonne SC, Saladin ME. Posttraumatic stress disorder and cocaine dependence: order of onset. American Journal of Addictions. 1998;7:128–135. http://dx.doi.org/10.1111/j.1521-0391.1998.tb00327. [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Western D. A multidimensional meta-analysis of psychotherapy for PTSD. The American Journal of Psychiatry. 2005;62(2):214–227. doi: 10.1176/appi.ajp.162.2.214. http://dx.doi.org/10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Breslau N. The epidemiology of trauma, PTSD, and other postrauma disorders. Trauma Violence Abuse. 2009;10:198–210. doi: 10.1177/1524838009334448. http://dx.doi.org/10.1177/1524838009334448. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. http://dx.doi.org/10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Briere J, Elliott DM. Prevalence and psychological sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse & Neglect. 2003;27:1205–1222. doi: 10.1016/j.chiabu.2003.09.008. http://dx.doi.org/10.1016/j.chiabu.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Chilcoat MD, Breslau N. Posttraumatic stress disorder and drug disorders: testing causal pathways. Archives of General Psychiatry. 1998;559(10):13–17. doi: 10.1001/archpsyc.55.10.913. http://archpsyc.ama-assn.org/cgi/reprint/55/10/913. [DOI] [PubMed] [Google Scholar]
- Chong CA, Chen I, Naglie G, Krahn MD. How well do guidelines incorporate evidence on patient preferences. Journal of General Internal Medicine. 2009;24(8):977–982. doi: 10.1007/s11606-009-0987-8. http://dx.doi.org/10.1007/s11606-009-0987-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioural sciences. New York: Academic Press; 1969. [Google Scholar]
- Cook JM, Walser RD, Kane V, Ruzek JI, Woody G. Dissemination of feasibility of a cognitive-behavioral treatment for substance use disorders and posttraumatic stress disorder in the Veterans Administration. Journal of Psychoactive Drugs. 2006;38:89–92. doi: 10.1080/02791072.2006.10399831. http://dx.doi.org/10.1080/02791072.2006.1039983. [DOI] [PubMed] [Google Scholar]
- Crandal R. The measurement of self-esteem and related constructs. In: Robinson JP, Shaver PR, editors. Measures of social psychological attitudes. Ann Arbor, MI: Institute for Social Research; 1973. pp. 80–82. (Revised Edition) [Google Scholar]
- Derogatis LR. A brief form of the SCL-90-R: a self-report symptom inventory designed to measure psychological stress: brief symptom inventory (BSI) Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- Desai RA, Harpaz-Rotem I, Najavits LM, Rosenheck RA. Impact of the seeking safety program on clinical outcomes among homeless female veterans with psychiatric disorders. Psychiatric Services. 2008;59:996–1003. doi: 10.1176/ps.2008.59.9.996. http://dx.doi.org/10.1176/appi.ps.59.9.996. [DOI] [PubMed] [Google Scholar]
- Devine DA, Fernald PS. Outcome effects of receiving a preferred, randomly assigned, or nonpreferred therapy. Journal of Consulting and Clinical Psychology. 1973;41(1):104–107. doi: 10.1037/h0035617. http://dx.doi.org/10.1037/h0035617. [DOI] [PubMed] [Google Scholar]
- Doherty C, Doherty W. Patients’ preference for involvement in clinical decision-making within secondary care and the factors that influence their preferences. Journal of Nursing Management. 2005;13(2):119–127. doi: 10.1111/j.1365-2934.2004.00498.x. http://dx.doi.org/10.1111/j.1365-2934.2004.00498.x. [DOI] [PubMed] [Google Scholar]
- Dutton DG, Hart SD. Evidence for long-term, specific effects of childhood abuse and neglect on criminal behavior in men. International Journal of Offender Therapy and Comparative Criminology. 1992;36:129–137. http://dx.doi.org/10.1177/0306624X9203600205. [Google Scholar]
- Elhai JD, Gray MJ, Kashdan TB, Franklin CL. Which instruments are most commonly used to assess traumatic event exposure and posttraumatic effects? A survey of traumatic stress professionals. Journal of Traumatic Stress. 2005;18:541–545. doi: 10.1002/jts.20062. http://dx.doi.org/10.1002/jts.20062. [DOI] [PubMed] [Google Scholar]
- Fallot RD, Harris M. Trauma Recovery and Empowerment Model (TREM): cConceptual and practical issues in a group intervention for women. Community Mental Health Journal. 2002;38(6):475–485. doi: 10.1023/a:1020880101769. http://dx.doi.org/10.1023/A:1020880101769. [DOI] [PubMed] [Google Scholar]
- Fallot Harris M, Affolter HU, Anglin J, Arledge E, Bebout R, et al. Men’s trauma recovery and empowerment model (M-TREM) Washington, DC: Community Connections; 2001. [Google Scholar]
- Fallot RD, McHugo GJ, Harris M, Xie H. The trauma recovery and empowerment model: a quasi-experimental effectiveness study. Journal of Dual Diagnosis. 2011;7:74–89. doi: 10.1080/15504263.2011.566056. http://dx.doi.org/10.1080/15504263.2011.566056. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition with psychotic screen. New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Foa EB, Keane TM, Friedman MJ, Cohen JA. Effective treatments for PTSD, practice guidelines from the International Society for Traumatic Stress Studies. New York, NY: Guilford Press; 2005. [Google Scholar]
- Gatz M, Brown V, Hennigan K, Rechberger E, O’Keefe M, Rose T, Bjelajac P. Effectiveness of an integrated trauma-informed approach to treating women with co-occurring disorders and histories of trauma: the Los Angeles site experience. Journal of Community Psychology. 2007;35(7):863–878. http://dx.doi.org/10.1002/jcop.20186. [Google Scholar]
- Ghee AC, Bolling LC, Johnson CS. The efficacy of a condensed seeking safety intervention for women in residential chemical dependency treatment at 30 days posttreatment. Journal of Child Sex Abuse. 2009;18:475–488. doi: 10.1080/10538710903183287. http://dx.doi.org/10.1080/10538710903183287. [DOI] [PubMed] [Google Scholar]
- Gibson LE, Holt JC, Fondacaro KM, Tang TS, Powell TA, Turbitt EL. An examination of antecedent traumas and psychiatric comorbidity among male inmates with PTSD. Journal of Traumatic Stress. 1999;12(3):473–484. doi: 10.1023/A:1024767020280. http://dx.doi.org/10.1023/A:1024767020280. [DOI] [PubMed] [Google Scholar]
- Glass S, Arnkoff DB, Shapiro SJ. Expectations and preferences. Psychotherapy: Theory/Research/Practice/Training. 2001;38(4):455–461. http://dx.doi.org/10.1037/0033-3204.38.4.455. [Google Scholar]
- Green B. Trauma history questionnaire. In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran Press; 1996. pp. 366–369. [Google Scholar]
- Greenglass E, Schwarzer R. The Proactive Coping Inventory (PCI) In: Schwarzer R, editor. Advances in health psychology research (CD:ROM) Berlin: Free University of Berlin, Institute for Arbeits, Organizations and Gesundheitspsychologie; 1998. [Google Scholar]
- Grubaugh AL, Elhai JD, Cusack KJ, Wells C, Frueh BC. Screening for PTSD in public-sector mental health settings: the diagnostic utility of the PTSD checklist. Depression and Anxiety. 2007;24(2):124–129. doi: 10.1002/da.20226. http://dx.doi.org/10.1002/da.20226. [DOI] [PubMed] [Google Scholar]
- Hamilton N. African-American Center for Excellence (AACE) Program (SAMHSA grant number TI14126; final report) Largo, Florida: Operation PAR; 2006. [Google Scholar]
- Harris M, Fallot RD. Designing trauma-informed addictions services. New Directions for Mental Health Services. 2001;2001(89):57–73. doi: 10.1002/yd.23320018907. http://dx.doi.org/10.1002/yd.23320018907. [DOI] [PubMed] [Google Scholar]
- Herman JL. Trauma and recovery: the aftermath of violence–from domestic abuse to political terror. New York. NY: Basic Books; 1997. [Google Scholar]
- Hien DA, Cohen L, Campbell A. Methodological innovation to increase the utility and efficiency of psychotherapy research for patients with co-occurring mental health and substance use disorders. Professional Psychology: Research and Practice. 2009;40:502–509. doi: 10.1037/a0014966. http://dx.doi.org/10.1037/a0014966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance abuse disorders. American Journal of Psychiatry. 2004;161:1426–1432. doi: 10.1176/appi.ajp.161.8.1426. http://dx.doi.org/10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- Hooper LM, Stockton P, Krupnick JL, Green BL. Development, use, and psychometric properties of the trauma history questionnaire. Journal of Loss and Trauma. 2011;16:258–283. http://dx.doi.org/10.1080/15325024.2011.572035. [Google Scholar]
- Institute of Medicine. PTSD compensation and military service. Washington, DC: National Academies Press; 2007. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Post-traumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. http://dx.doi.org/10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Evaluation and Program Planning. 1979;2(3):197–207. doi: 10.1016/0149-7189(79)90094-6. http://dx.doi.org/10.1016/0149-7189(79)90094. [DOI] [PubMed] [Google Scholar]
- Leykin Y, DeRubies RJ, Gallop R, Amsterdam JD, Shelton RC, Hollon SD. The relation of patients’ treatment preferences to outcome in a randomized clinical trial. Behavior Therapy. 2007;38(3):209–217. doi: 10.1016/j.beth.2006.08.002. http://dx.doi.org/10.1016/j.beth.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Lo C, Stephens R. Drugs and prisoners: treatment needs on entering prison. American Journal of Drug and Alcohol Abuse. 2000;26:229–245. doi: 10.1081/ada-100100602. http://dx.doi.org/10.1081/ADA-100100602. [DOI] [PubMed] [Google Scholar]
- Lynch SM, Heath NM, Mathews KC, Cepeda GJ. Seeking safety: an intervention for trauma-exposed incarcerated women? Journal of Trauma and Dissociation. 2012;13:88–101. doi: 10.1080/15299732.2011.608780. http://dx.doi.org/10.1080/15299732.2011.608780. [DOI] [PubMed] [Google Scholar]
- Maxfield MG, Widom CS. The cycle of violence: revisited six years later. Archives of Pediatric and Adolescent Medicine. 1996;150:390–395. doi: 10.1001/archpedi.1996.02170290056009. http://dx.doi.org/10.1001/archpedi.1996.02170290056009. [DOI] [PubMed] [Google Scholar]
- McGovern MP, Lambert-Harris C, Acquilano S, Xie H, Alterman AI, Weiss RD. A cognitive behavioral therapy for co-occurring substance use and posttraumatic stress disorders. Addictive Behaviors. 2009;34:892–897. doi: 10.1016/j.addbeh.2009.03.009. http://dx.doi.org/10.1016/j.addbeh.2009.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller NA, Najavits LM. Creating trauma-informed correctional care: a balance of goals and environment. European Journal of Psychotraumatology. 2012;3:1–8. doi: 10.3402/ejpt.v3i0.17246. http://dx.doi.org/10.3402/ejpt.v3i0.17246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrissey JP, Ellis AR, Gatz M, Amaro H, Reed BG, Savage A, Bank S. Outcomes for women with co-occurring disorders and trauma: program and person-level effects. Journal of Substance Abuse Treatment. 2005;28:121–133. doi: 10.1016/j.jsat.2004.08.012. http://dx.doi.org/10.1016/j.jsat.2004.08.012. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Drake RE, Sigmon SC, Brunette MF. Psychosocial interventions for adults with severe mental illnesses and co-occurring substance use disorders: a review of specific interventions. Journal of Dual Disorders. 2005;1(2):57–82. http://dx.doi.org/10.1300/J374v01n02_05. [Google Scholar]
- Mumola CJ, Karberg JC. Drug use and dependence, State and Federal prisoners, 2004. Washington, DC: U.S. Dept of Justice; 2006. NCJ 213530. [Google Scholar]
- Najavits LM. End-of-treatment questionnaire (unpublished measure) Boston, MA: Harvard Medical School; 1994. [Google Scholar]
- Najavits LM. Seeking safety, a treatment manual for PTSD and substance abuse. New York, NY: The Guilford Press; 2002. [Google Scholar]
- Najavits LM. Seeking safety: an evidence-based model for substance abuse and trauma/PTSD. In: Witkiewitz KA, Marlatt GA, editors. Therapists’ guide to evidence-based relapse prevention: practical resources for the mental health professional. San Diego, CA: Elsevier Press; 2007. pp. 141–167. [Google Scholar]
- Najavits LM, Gallop RJ, Weiss RD. Seeking safety therapy for adolescent girls with PTSD and substance use disorder: a randomized controlled trial. The Journal of Behavioral Health Services & Research. 2006;33:453–463. doi: 10.1007/s11414-006-9034-2. http://dx.doi.org/10.1007/s11414-006-9034-2. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Hien D. Helping vulnerable populations: a comprehensive review of the treatment outcome literature on substance use disorder and PTSD. Journal of Clinical Psychology. 2013;69:433–479. doi: 10.1002/jclp.21980. http://dx.doi.org/10.1002/jclp.21980. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Schmitz J, Gotthardt S, Weiss RD. Seeking safety plus exposure therapy: an outcome study on dual diagnosis men. Journal of Psychoactive Drugs. 2005;27:425–435. doi: 10.1080/02791072.2005.10399816. http://dx.doi.org/10.1080/02791072.2005.10399816. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Schmitz M, Johnson KM, Smith C, North T, Hamilton N, et al. Seeking safety therapy for men: Clinical and research experiences. In: Katlin LJ, editor. Men and addictions: new research. Haupppauge, NY: Nova Science Publishers; 2009. pp. 37–58. [Google Scholar]
- Najavits LM, Gastfriend DR, Barber JP, Reif S, Muenz L, Blaine R, Weiss RD. Cocaine dependence with and without PTSD among subjects in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. American Journal of Psychiatry. 1998;155(2):214–219. doi: 10.1176/ajp.155.2.214. http://journals.psychiatryonline.org/articleaspx?articleid=172698. [DOI] [PubMed] [Google Scholar]
- National Research Council. The growth of incarceration in the United States: exploring causes and consequences Committee on Causes and Consequences of High Rates of Incarceration. In: Travis J, Western B, Redburn S, editors. Committee on Law and Justice, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press; 2014. [Google Scholar]
- Peters, Greenbaum PE, Edens JF, Carter CR, Ortiz MM. Prevalence of DSM-IV substance abuse and dependence disorders among prison inmates. American Journal of Drug and Alcohol Abuse. 1998;24:573–587. doi: 10.3109/00952999809019608. http://dx.doi.org/10.3109/00952999809019608. [DOI] [PubMed] [Google Scholar]
- Pimlott Kubiak S. The effects of PTSD on treatment adherence, drug relapse, and criminal recidivism in a sample of incarcerated men and women. Research on Social Work Practice. 2004;14:424–433. http://dx.doi.org/10.1177/1049731504265837. [Google Scholar]
- Powell T, Holt J, Fondacato K. The prevalence of mental illness among inmates in a rural state. Law and Human Behavior. 1997;21:427–438. doi: 10.1023/a:1024811303834. http://dx.doi.org/10.1023/A:1024811303834. [DOI] [PubMed] [Google Scholar]
- Rash, Coffey SF, Baschnagel JS, Drobes DJ, Saladin ME. Psychometric properties of the IES-R in traumatized substance dependent individuals with and without PTSD. Addictive Behaviors. 2008;33:1039–1047. doi: 10.1016/j.addbeh.2008.04.006. http://dx.doi.org/10.1016/j.addbeh.2008.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: applications and data analysis methods. 2. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Reynolds M, Mezey G, Chapman M, Wheeler M, Drummond C, Baldacchino A. Co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug and Alcohol Dependence. 2005;77:251–258. doi: 10.1016/j.drugalcdep.2004.08.017. http://dx.doi.org/10.1016/j.drugalcdep.2004.08.017. [DOI] [PubMed] [Google Scholar]
- SAMHSA National GAINS Center. Trauma-specific interventions for justice-involved persons. Delmar, NJ: Author; 2011. Retrieved from http://gainscenter.samhsa.gov/pdfs/ebp/TraumaSpecificInterventions.pdf. [Google Scholar]
- Sarchiapone M, Carli V, Cuomo C, Marchetti M, Roy A. Association between childhood trauma and aggression in male prisoners. Psychiatry Research. 2009;165:187–192. doi: 10.1016/j.psychres.2008.04.026. http://dx.doi.org/10.1016/j.psychres.2008.04.026. [DOI] [PubMed] [Google Scholar]
- Saxon AJ, Davis TM, Sloan KL, McKnight KM, McFall ME, Kivlahan DR. Trauma, symptoms of posttraumatic stress disorder, and associated problems among incarcerated veterans. Psychiatric Services. 2001;52:959–964. doi: 10.1176/appi.ps.52.7.959. http://dx.doi.org/10.1176/appi.ps.52.7.959. [DOI] [PubMed] [Google Scholar]
- Schmuckler MA. What is ecological validity? A dimensional analysis. Infancy. 2001;2:419–436. doi: 10.1207/S15327078IN0204_02. http://dx.doi.org/10.1207/S15327078IN0204_02. [DOI] [PubMed] [Google Scholar]
- Schnurr PP. Treatments for PTSD: understanding the evidence psychotherapy. PTSD Research Quarterly. 2008;19:1–6. http://www.ptsd.va.gov/professional/newsletters/research-quarterly/V19N3.pdf. [Google Scholar]
- Schnurr PP, Friedman MJ, Foy DW, Shea MT, Hsieh FY, Lavori PW, et al. A randomized trial of trauma focus group therapy for posttraumatic stress disorder: results from a Department of Veterans Affairs Cooperative Study. Archives of General Psychiatry. 2003;60:481–489. doi: 10.1001/archpsyc.60.5.481. http://archpsyc.jamanetwork.com. [DOI] [PubMed] [Google Scholar]
- Schwarzer R, Jerusalem M. Generalized self-efficacy scale. In: Weinman J, Wright S, Johnston M, editors. Measures in health psychology: a user’s portfolio Causal and control beliefs. Windsor, UK: NFER-NELSON; 1995. pp. 35–37. [Google Scholar]
- Seligman ME. The effectiveness of psychotherapy: the Consumer Reports study. American Psychologist. 1995;50:965–974. doi: 10.1037//0003-066x.50.12.965. http://dx.doi.org/10.1037/0003-066X.50.12.965. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: summary of national findings. 2013 Retrieved from Figure 2.9, http://www.samhsa.gov/data/NSDUH/2012SummNatFindDetTables/NationalFindings/NSDUHresults2012.htm#ch2.3.
- Swift JK, Callahan JL. The impact of client treatment preferences on outcome: a meta-analysis. Journal of Clinical Psychology. 2009;65:368–381. doi: 10.1002/jclp.20553. http://dx.doi.org/10.1002/jclp.20553. [DOI] [PubMed] [Google Scholar]
- Tjaden P, Thoennes N. Full report of the prevalence, incidence, and consequences of violence against women: findings from the National Violence Against Women Survey (Publication No NCJ 183781) Washington, DC: U.S. Department of Justice and Center for Disease Control and Prevention, National Institute of Justice, Office of Justice Programs; 2002. [Google Scholar]
- Toussaint DW, VanDeMark NR, Bornemann A, Graeber CJ. Modifications to the Trauma Recovery and Empowerment Model (TREM) for substance-abusing women with histories of violence: outcomes and lessons learned at a Colorado substance abuse treatment center. Journal of Community Psychology. 2007;35:879–894. http://dx.doi.org/10.1003/jcop.20187. [Google Scholar]
- Triffleman EG, Marmar CR, Delucchi KL, Ronfeldt H. Childhood trauma and posttraumatic disorder in substance abuse patients. Journal of Nervous and Mental Disease. 1995;183:172–176. doi: 10.1097/00005053-199503000-00008. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT. Psychometric properties of the clinician-administered PTSD scale CAPS-1. PTSD Research Quarterly. 1994;5:2–6. [Google Scholar]
- Weeks R, Widom CS. Self-reports of early childhood victimization among incarcerated adult male felons. Journal of Interpersonal Violence. 1998;13:346–361. http://dx.doi.org/10.1177/088626098013003003. [Google Scholar]
- Wilkins KD, Lang AJ, Norman SB. Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depression and Anxiety. 2011;28:596–606. doi: 10.1002/da.20837. http://dx.doi.org/10.1002/da.20837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff N, Huening J, Shi J, Frueh C. Trauma exposure and post-traumatic stress disorder among incarcerated men. Journal of Urban Health. 2014 doi: 10.1007/s11524-014-9871-x. http://dx.doi.org/10.1007/s11524-014-9871-x. [DOI] [PMC free article] [PubMed]
- Wolff N, Shi J, Siegel J. Patterns of victimization among male and female inmates: Evidence of an enduring legacy. Violence and Victims. 2009;24:469–484. doi: 10.1891/0886-6708.24.4.469. http://dx.doi.org/10.1891/0886-6708.24.4.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. The ASSIST Project – alcohol, smoking and substance involvement screening test. 2010 Retrieved from http://www.who.int/substanceabuse/activities/assist/en/
- Zlotnick C, Johnson J, Najavits LM. Randomized controlled pilot study of cognitive–behavioral therapy in a sample of incarcerated women with substance use disorder and PSTD. Behavior Therapy. 2009;40(4):325–336. doi: 10.1016/j.beth.2008.09.004. http://dx.doi.org/10.1016/j.beth.2008.09.00. [DOI] [PMC free article] [PubMed] [Google Scholar]


