Abstract
Objective
This study examined the individual and combined effects of two non-pharmacological treatments for Attention-Deficit/Hyperactivity Disorder (ADHD): Cogmed working memory training (CWMT) for adolescents, and behavioral parent training (BPT) for mothers.
Method
Ninety-one adolescents (ages 11–15) and their mothers were randomized to one of four CWMT and BPT treatment and active control (placebo) group combinations of 5-week interventions. At pre- and post-test, mothers and teachers completed rating forms, and adolescents completed neuropsychological measures of working memory (WM).
Results
Individual intervention effects showed that treatment CWMT significantly improved WM spans, whereas there were no significant differences for treatment or control BPT on reports of parenting-related outcomes. Combined treatment effects indicated an overall pattern of greatest improvements for the control CWMT/treatment BPT group, as compared to the other three groups, on adolescent WM deficit, behavioral regulation problems, and global executive deficit. Most significant effects for outcomes were main effects of improvements over time. Conclusions: Combination CWMT and BPT did not result in increased treatment gains. However, potential effects of combined treatment may have been masked by greater perceived benefits arising from lack of struggle in the non-adaptive, CWMT active control condition. Future combined intervention research should focus on specific, theoretically-driven WM deficits among individuals with ADHD, include possible adaptations to the standard CWMT program, examine effectiveness of cognitive treatments combined with contextual interventions, and utilize appropriate control groups to fully understand the unique and combined effects of interventions.
Keywords: ADHD, combined interventions, working memory, behavioral parent training, randomized controlled trial
Combined Cognitive and Parent Training Interventions for Adolescents with ADHD and Their Mothers: A Randomized Controlled Trial
Children and adolescents with Attention-Deficit/Hyperactivity Disorder (ADHD) often demonstrate impairment in multiple domains, including executive functioning deficits, disruptive behaviors, and maladaptive parent-child relations (Dishion & Patterson, 2006; Johnston & Mash, 2001; Kasper, Alderson, & Hudec, 2012). Given the scope of impairments, the development of complementary and augmentative treatments targeting multiple outcomes is essential. In this study, we evaluated the individual and combined efficacy of two non-pharmacological treatments for ADHD: a computerized working memory training program for adolescents (Cogmed-RM; Klingberg et al., 2005), and a novel behavioral parent training program for their mothers.
A large evidence base indicates substantial impairment in working memory (WM) among individuals with ADHD (Kasper et al., 2012; Martinussen, Hayden, Hogg-Johnson, & Tannock, 2005). Accordingly, researchers have explored the potential for improving WM and concurrent ADHD symptoms through WM training (for reviews and meta-analyses, see Melby-Lervåg & Hulme, 2012; Morrison & Chein, 2011; Rapport, Orban, Kofler, & Friedman, 2013; Shipstead, Redick, & Engle, 2012). To date, the Cogmed-RM program (hereafter, CWMT; Klingberg et al., 2005) is the most developed of such interventions, and has received the greatest research attention (for reviews, see Chacko, Feirsen, et al., 2013; Shipstead, Hicks, & Engle, 2012).
Results of CWMT study evaluations indicate that it reliably targets the attentional control components of WM, or those most important for short-term maintenance of goal-relevant information (Chacko, Bedard, et al., 2013; Gibson et al., 2011; 2013; Gibson, Gondoli, Johnson, Steeger, & Morrissey, 2012; Gibson, Kronenberger, et al., 2012; Gray et al. 2012; Holmes et al., 2010; see also Kane & Engle, 2002). However, the particular aspects of WM most impaired in ADHD may reflect deficits in retrieval of information and not problems in active maintenance (Gibson et al., 2011; 2013; Gibson, Gondoli, et al., 2012; Gibson, Kronenberger, et al., 2012). Retrieval processes concern retrieval of information lost from active maintenance, yet vital for the pursuit of goal-directed behavior (Unsworth & Engle, 2007). The disparity between the focus of CWMT training and the WM components particularly impaired in ADHD may help explain the mixed findings concerning the program’s efficacy for treating ADHD symptoms (Gibson et al., 2011; 2013; Gibson, Gondoli, et al. 2012; Gibson, Kronenberger, et al., 2012). Cogmed helps individuals with ADHD better maintain information via attentional control processes, and may thus decrease the need for activation of their impaired retrieval processes; that is, strengthened maintenance may partially compensate for poor retrieval (Gibson et al., 2011; 2013; Gibson, Gondoli, et al., 2012; Gibson, Kronenberger et al., 2012). Although such compensation is not inconsequential, Cogmed may not be the most potent stand-alone cognitive treatment for ADHD symptoms. There are, however, other problems associated with ADHD that may be improved by optimizing attentional control. In particular, we argue that Cogmed may be useful as a child-focused, augmentative treatment for the parenting-related impairments found among families of children with ADHD.
Findings obtained from typically-developing samples, as well as samples of children with ADHD, indicate that greater child attentional control is associated with more favorable parenting (Belsky, Fearon, & Bell, 2007; Eisenberg et al., 2005; Graziano, Calkins, & Keane, 2011). Reciprocal connections between child attentional processes and parenting have also been described; over time, higher positive parenting predicted greater child attentional control, while higher child attentional control predicted greater positive parenting (Belsky et al., 2007). In addition, better child attentional control at earlier time points predicted fewer subsequent teacher-reported externalizing problems (Belsky et al., 2007).
Given relations among child attentional control and parenting-related variables, improving a child’s attentional control could potentially benefit family functioning. Medication regimens for children with ADHD have resulted in improved child executive functioning, and have also been associated with concurrent improvements in child disruptive behavior and parenting (Holmes et al., 2010; Pelham et al., 2005; Van der Oord, Prins, Oosterlaan, & Emmelkamp, 2008). Cogmed training, to the extent it improves attentional control, might also have salutary effects on child behavior and parenting. However, it is also possible that Cogmed alone, while producing some beneficial effects on cognitive outcomes, may not be potent or comprehensive enough to result in improvements in child regulation or parenting. That is, the potential beneficial effects of cognitive training for children might be made more substantial and wide-ranging by combining it with additional child treatments or with interventions designed to strengthen the child’s social contexts, including family and school settings (Chacko, Kofler, & Jarrett, 2014; Gathercole, 2014; see also Neville et al., 2013). In the present study, we posit that Cogmed might be productively combined with Behavioral Parent Training (BPT), to influence both adolescent and family context outcomes.
Support for our novel approach is provided from a recent study by Neville and colleagues (2013). Focusing on at-risk preschoolers enrolled in Head Start and their parents, Neville et al. combined a classroom-based, selective attention training program for children with a group-based BPT program for their parents. Results of this controlled study indicated that the children in the combined attention-training plus BPT group demonstrated greater improvements in neurological measures of attention, standardized assessments of executive functioning, and parent ratings of behavioral regulation than did either an attention-training only comparison group, or a passive control group (i.e., Head Start as usual). Furthermore, parents in the combined attention-training plus BPT group demonstrated greater improvements in parenting and reduced parenting stress, when compared with both the attention-training only group, and the passive control group. Such results certainly suggest that child cognitive training may be productively combined with BPT. Furthermore, cognitive training, while helpful, is likely insufficient as a stand-alone treatment for the substantial relational and behavioral impairments found among children at-risk for ADHD diagnoses and their parents.
In fact, considerable evidence indicates that child ADHD symptoms and impairments contribute to the development and maintenance of maladaptive family relations (for review, see Deault, 2010). Hyperactive and impulsive behaviors are difficult for parents to manage, and inattentive behaviors make parent instruction and direction more challenging and less effective. Accordingly, parents of children with ADHD have been described as less responsive, and more negative, lax, reactive, and stressed than parents of typically-developing children (Johnston & Mash, 2001). In turn, compromised parenting underlies escalated levels of child oppositional behavior and parent-child conflict (Barkley, Guevremont, Anastopoulos, & Fletcher, 1992; Dishion & Patterson, 2006). In families in which such negative interactions have become routine, parents need guidance in order to reduce maladaptive patterns and replace them with functional behaviors (Lee, Niew, Yang, Chen, & Lin, 2012; Patterson, 1982).
BPT is intended to improve parenting behaviors, child compliance, and the parent-child relationship (Evans, Owens, & Bunford, 2014). Common content across BPT programs includes strategies to help parents increase positivity, apply appropriate contingencies and incentives, and reduce negative emotional reactivity. The overarching aim of BPT is to enhance family functioning and thus optimize this developmental context for children.
BPT programs have demonstrated effectiveness in improving parenting and parent-child relationships among families of children with ADHD (e.g., Cunningham, 2006; Thorell, 2009; see also Evans et al., 2014; Lee et al., 2012). Although not intended as a direct treatment of the underlying neurocognitive causes of ADHD, BPT has nonetheless resulted in improvement in parent perceptions of child ADHD symptoms and impairments (for review, see Evans et al., 2014; Lee et al., 2012). For example, Thorell (2009) implemented the Community Parent Education Program (COPE; Cunningham, 2006) among parents of school-age children with ADHD and other disruptive behaviors. Most relevant to the present study, COPE-enrolled parents recruited from the community improved on parenting stress and sense of control, and also reported improvements in child hyperactive/impulsive (H/I) symptoms and conduct problems, relative to a waitlist control group. However, COPE did not appear effective for reducing child inattention, suggesting that concurrent cognitive treatments might be warranted. Furthermore, the small effect sizes reported for child variables other than H/I and Oppositional Defiant Disorder (ODD) symptoms suggest that the positive effects of BPT may need to be augmented, perhaps by concurrent direct treatment of child symptoms and impairments.
Despite the potential theoretical impact of combined treatment approaches, however, empirical evidence for the efficacy of combination treatment remains inconsistent. For instance, the most ambitious and well-known multimodal treatment initiative for ADHD, the MTA study (MTA Cooperative Group, 1999), included BPT, other psychosocial treatments (e.g., child psychotherapy and social skills training), and child stimulant medication management in the treatment protocol. In early MTA reports, there was some evidence that BPT combined with other interventions yielded greater short-term improvements in child behavioral and parenting outcomes than did single treatments alone (Hinshaw et al., 2000; MTA Cooperative Group, 1999). However, longer-term follow-up from the MTA study found no evidence of greater efficacy for combined treatments (e.g., Molina et al., 2009). Additional combination treatment studies on a much smaller scale have also yielded inconsistent findings. For instance, Pelham et al. (2005) reported that combination treatments (including BPT) were superior to single treatments in several domains of functioning. However, Abikoff et al. (2004), reported that combined psychosocial treatment (including BPT) plus medication management was not superior to medication management alone.
The mixed findings surrounding combinations of BPT and other treatments suggest that further development of combination treatments is warranted. Particularly needed are novel combinations of treatments for ADHD which combine direct, non-pharmacological targeting of underlying neurocognitive impairments with psychosocial interventions intended to optimize the contexts of development for affected children (Chacko et al., 2014; Gathercole, 2014; Neville et al., 2013). Such approaches are particularly needed when medication is not feasible or effective (Smith, Waschbusch, Willoughby & Evans, 2000).
The Present Study
In this research, we evaluated the unique and combined efficacy of CWMT and a group-based BPT program. We focused on whether these cognitive and behavioral approaches have independent effects, and whether they may also be made more effective by their combination (Chacko et al., 2014; Gathercole, 2014; Neville et al., 2013). Our rigorous design included random assignment to structurally equivalent treatment and active control groups and consideration of CWMT and BPT as separate and potentially multiplicative factors. We employed a 2 × 2 mixed group factorial design, which included CWMT and BPT interventions as the between-subjects factors, and pretest-posttest (time) as the within subjects factor.
It was hypothesized that, compared to control CWMT, treatment CWMT would result in greater improvements in adolescent WM outcomes reflecting attentional control (i.e., neuropsychological measures of simple span). Although we did not expect CWMT to improve ADHD symptoms given the extant literature (e.g., Chacko, Bedard, et al., 2013; van Dongen-Boomsma et al., 2014), for completeness, we examined CWMT’s effect on these outcomes. Given prior relations between BPT and improved child ADHD symptoms, we hypothesized that, compared to control BPT, treatment BPT would result in greater improvements in mother-rated adolescent ADHD symptom outcomes. Furthermore, given some prior evidence that combined BPT plus child neuropsychological treatments (e.g., medication; selective attention training) yielded enhanced treatment effects, we examined interactions among BPT condition, CWMT condition, and time for ADHD symptoms.
In regard to parenting-related outcomes, we hypothesized that, compared to control BPT, treatment BPT would result in greater improvements in mother’s parenting behaviors, adolescent oppositional behaviors, and mother-adolescent conflict. Based on prior evidence that combinations of BPT and child neuropsychological treatments enhanced treatment effects in family domains, we examined potential interactions among BPT condition, CWMT condition, and time for parenting-related outcomes.
We also assessed adolescent global outcomes with measures of behavior regulation and global executive functioning. Global outcomes that have both cognitive and behavioral underpinnings may particularly benefit from a combination of neurocognitive and behavioral interventions. Therefore, we hypothesized that adolescents in the full treatment group (treatment CWMT plus treatment BPT) would show greater improvements on global outcomes relative to adolescents in the other three groups (i.e., those which contained at least one placebo treatment).
In addition, consistent with calls for greater attention to intervention process and participant perceptions (e.g., Morrison & Chein, 2011), we examined treatment fidelity, as well as participant motivation, compliance, engagement, and blindness to condition.
Method
Participants
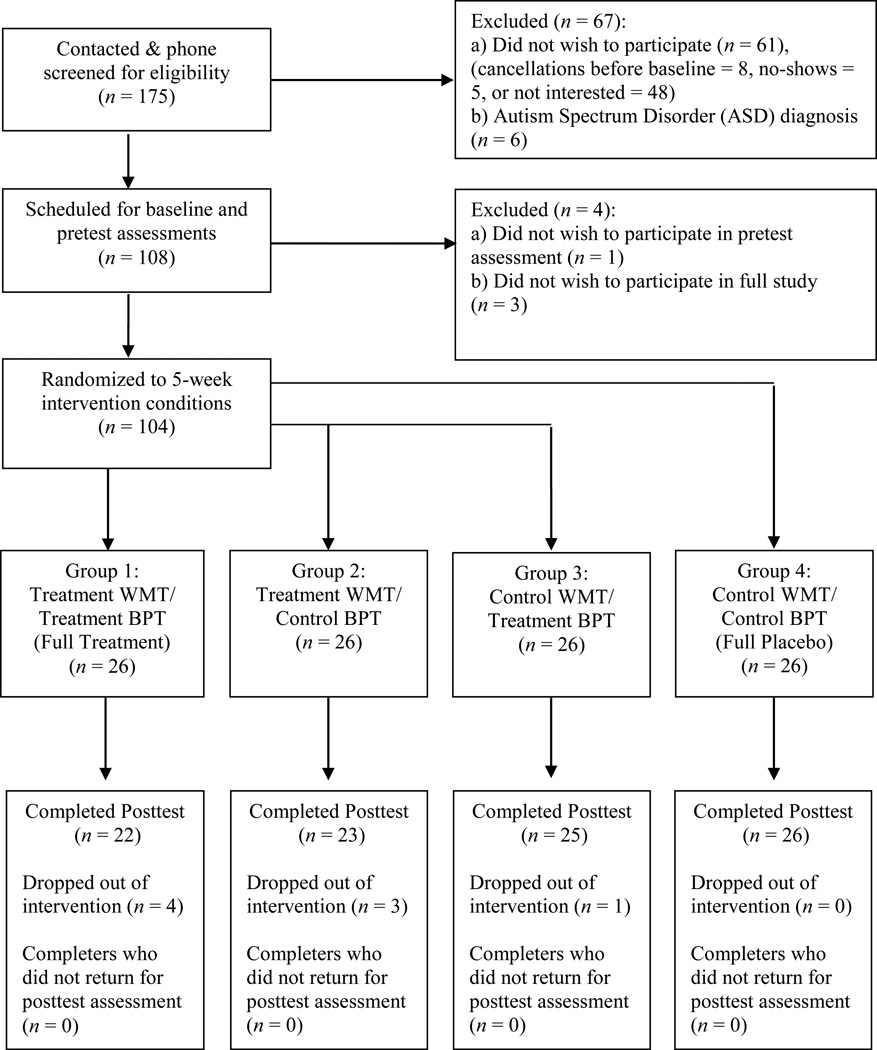
We recruited 108 adolescents in grades 5–9 (ages 11–15) and their mothers from local schools via initial contact letters direct-mailed to students’ home addresses. The initial contact letter described our interest in adolescents with an ADHD diagnosis, and mentioned that the study included assessment visits as well as cognitive training and group-based parent education. Interested mothers subsequently contacted our research office by phone. If the phone screening indicated that the adolescent had suspected ADHD and no ASD diagnosis, the dyad was scheduled for a baseline assessment. Between the baseline assessment and a subsequent pretest assessment, 4 dyads withdrew, leaving 104 dyads that were randomly assigned to intervention conditions. Eight dyads withdrew after the interventions began, and 5 dyads did not meet inclusion criteria for the present analyses (n = 3 adolescents with IQ < 70; n = 2 mothers with < 75% BPT attendance). Thus, outcome analyses were based on 91 dyads (see Figure 1 for participant flowchart). The research protocol for the present study was approved by the University Institutional Review Board.
Figure 1.
Flowchart and 2 × 2 mixed factorial study design.
Procedure
The study included an unmedicated baseline assessment, a pretest assessment, five weeks of interventions, and a posttest assessment (see Figure 1). Adolescents, mothers, and teachers were intentionally blind to adolescent WMT condition and maternal BPT condition throughout the duration of the study. Assessors were also blind to participant conditions.
Baseline assessment
Mothers were instructed to withhold their adolescents’ typical ADHD medications 24 hours prior to the baseline assessment. During a 2-hour visit to our university research laboratory, mothers and adolescents provided informed consent and assent, respectively. To confirm the adolescent ADHD diagnosis and identify comorbid DSM-IV (American Psychiatric Association, 2000) based diagnoses, faculty investigators or advanced doctoral students administered the Computerized Diagnostic Interview Schedule for Children, Version 4 to mothers (C-DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). The C-DISC-IV has been documented as a reliable and valid measure of child and adolescent psychopathology (Shaffer et al., 2000). ADHD subtype was determined by the C-DISC-IV inattentive and/or hyperactive/impulsive (H/I) symptom counts in the ADHD module. Symptom counts included six or more inattentive symptoms for the inattentive subtype, six or more H/I symptoms for the H/I subtype, and six or more symptoms in both inattentive and H/I impulsive domains for the combined subtype. Mothers also completed demographic questions.
Adolescents separately and independently completed the Kaufman Brief Intelligence Test (KBIT-2; Kaufman & Kaufman, 2004) administered by advanced doctoral students. Dyads were compensated $20 for completing the baseline assessment.
Pretest and posttest assessments
Within two weeks before and after the 5-week interventions, adolescents and their mothers returned to the laboratory to complete 2-hour pretest and posttest assessments. Mothers were instructed to follow the adolescent’s normal medication treatment plan before arriving to the pretest and posttest assessments. Mothers completed questionnaires to assess adolescent executive functioning, ADHD symptoms, behavior problems, maternal parenting practices, and mother-adolescent conflict. Adolescents completed laboratory-based neuropsychological measures of WM, and a questionnaire packet that was read aloud by research assistants. Additionally, teachers completed measures of adolescent executive functioning and ADHD symptoms. Dyads were compensated $40 at pretest and $60 at posttest. Teachers were compensated $20 ($10 at pretest and posttest).
Measures of Treatment Outcome
Adolescent neuropsychological WM measures. Adolescents completed two neuropsychological, performance-based simple span verbal and spatial measures of WM (WISC-IV integrated; Wechsler et al., 2004). Adolescents repeated increasingly long sequences of numbers (digit span; verbal WM) and locations of blocks (spatial WM), both forward and backward. Each response per verbal and spatial span trial was scored as a “0” for an incorrect response and a “1” for a correct response. Researchers administered two trials of an item until the adolescent incorrectly recalled both trials. The cumulative raw score of number of correct trial responses was recorded for each span task at pretest and posttest.
Ratings of adolescent executive functioning
Mothers and teachers completed the 86-item Behavior Rating Inventory of Executive Functioning (BRIEF; Gioia, Isquith, Guy, & Kenworthy, 2000a). Items were rated from 1 (never) to 3 (often), with higher scores indicating greater deficit. The present study utilized three measures from the BRIEF: WM (10 items), the Behavior Regulation Index (28 items assessing adolescent inhibition, set-shifting, and emotion control), and the Global Executive Composite (72 items assessing WM, initiation, planning/organizing, organization of materials, monitoring, inhibition, set-shifting, and emotion control). Gioia, Isquith, Guy, and Kenworthy (2000b) reported good convergent and discriminant validity between the BRIEF and similar behavioral rating scales in clinical ADHD populations. Cronbach’s alpha in the current study indicated high internal consistency (.87 to .98) for mother and teacher ratings of BRIEF dimensions at pretest and posttest.
Ratings of adolescent ADHD symptoms
Mothers and teachers completed the 18-item DuPaul ADHD Rating Scale-IV to rate adolescent inattentive and H/I symptoms (ADHD-RS; DuPaul, Power, Anastopoulos, & Reid, 1998). The ADHD-RS has demonstrated good validity and test-retest reliability and is widely used in ADHD research (DuPaul et al., 1998; Faries, Yalcin, Harder, & Heiligenstein, 2001). Items were rated from 0 (never or rarely) to 3 (very often), with higher scores indicating greater symptoms. Cronbach’s alpha indicated high internal consistency (.87 to .93) for mother and teacher ratings for inattentive and H/I symptoms at pretest and posttest.
Parenting behaviors
The Alabama Parenting Questionnaire (APQ; Frick, 1991; Shelton, Frick, & Wootton, 1996) assessed mothers’ perceptions of their parenting practices across four domains: Involvement (10 items), Positive Parenting (6 items), Poor Monitoring/Supervision (10 items), and Inconsistent Discipline (6 items). Items were rated from 1 (never) to 5 (always), with higher scores indicating higher levels of the parenting dimension. The APQ has shown good validity and test-retest reliability (Dadds, Maujean, & Fraser, 2003). Cronbach’s alpha indicated acceptable internal consistency (.70 to .84) for the APQ subscales at pretest and posttest.
Oppositional behaviors
The 5-item Oppositional Defiant Problems scale from the Child Behavior Checklist was completed by mothers to assess adolescent oppositional and defiant behaviors (CBCL; Achenbach & Rescorla, 2001). Items were rated from 0 (not true) to 3 (very true or often true), with higher scores indicating greater oppositional and defiant behaviors. The items reflect content of the DSM-IV-TR criteria for ODD, and have demonstrated good validity and test-retest reliability (Achenbach & Rescorla, 2001). At both pretest and posttest, Cronbach’s alpha in the current study was .76.
Mother-adolescent conflict
Mother–adolescent conflict was assessed with maternal reports on the 22-item Dyadic Behavior subscale of the Conflict Behavior Questionnaire (CBQ; Robin & Foster, 2002; Sturge-Apple, Gondoli, Bonds, & Salem, 2003). Items were rated from 1 (really true) to 4 (really false), with higher scores indicating greater conflict. The CBQ discriminates between distressed and non-distressed families (Robin & Foster, 2002) and demonstrates high test-retest reliability and excellent internal consistency (Steeger & Gondoli, 2013; Sturge-Apple et al., 2003). Cronbach’s alpha was .90 and .87 at pretest and posttest, respectively.
Measures of Intervention Process and Participant Perceptions of Treatment
Adolescent CWMT fidelity
Average WM spans across treatment days were calculated for participants in the treatment and control groups. Training spans were examined to ensure that the treatment group participants were indeed performing at higher levels than were the control group participants.
Adolescent motivation
At posttest, adolescents completed 12 items to assess perceived motivation during cognitive training. The items were adapted from the Intrinsic Motivation Inventory (IMI; Deci & Ryan, 2011). The IMI items can be adapted to fit different situations and tasks, and we adapted them to pertain to WMT. Adolescents completed two subscales: Interest/enjoyment (7 items), and effort (5 items), which were summed to form a composite measure. Each item was rated from 1 (not true at all) to 7 (very true), with higher scores indicating greater motivation. Sample items included “Cogmed was fun to do” and “I tried very hard on Cogmed.” Cronbach’s alpha for the 12-item scale was .91.
Adolescent compliance with training
At posttest, mothers completed two items designed for this study to assess difficulty of maintaining adolescent compliance with cognitive training (i.e., “It was difficult to motivate my child to do the Cogmed exercises” and “I had to put in a lot of effort to make my child do the Cogmed exercises”). Items were rated 1 (strongly disagree) to 5 (strongly agree), with higher scores indicating greater difficulty. This measure was added to the posttest assessment packet after several cases had completed the study, and was available for 73 mothers.
Mother engagement in parent training
Mothers’ attendance at weekly parent group meetings was recorded. Additionally, at posttest, mothers rated their homework completion and engagement using a 4-item subscale designed for this study. Items (e.g., “I was able to complete most homework” and “The homework was interesting”) were rated from 1 (strongly disagree) to 4 (strongly agree). Higher scores indicated greater engagement. Cronbach’s alpha was .80 at posttest.
Mother blindness to treatment
At posttest, mothers were asked to provide their best guess or “gut feeling” about whether their adolescents had received a more effective or less effective version of the cognitive training (i.e., “My child completed a more effective version of Cogmed” versus “My child completed a less effective version of Cogmed”). Mothers were also asked at posttest to provide their best guess or gut feeling about whether they had received a more effective or less effective parent training program (i.e., “I completed a more effective version of the mom group program” versus “I completed a less effective version of the mom group program”). These measures of blindness were added after the study commenced, and were available for 73 mothers.
CWMT Intervention
Over five weeks, adolescents completed a high- or low-dose version of Cogmed-RM, an at-home, 25-day, computerized WM training program (Cogmed RoboMemo; Cogmed Cognitive Medical Systems AB, Stockholm, Sweden; Pearson Education, Upper Saddle River, NJ). We selected CWMT for the current study because the program is appropriate for use with adolescents, currently has the largest empirical evidence base among cognitive training programs for ADHD, and appears to train the attentional control components of WM (Chacko, Feirsen, et al., 2013; Gibson et al., 2011; 2012b; 2013; Klingberg, 2010). Adolescents were randomly assigned to CWMT condition using a random numbers table. Each day of training, participants in both conditions completed a total of eight spatial and verbal WM exercises (e.g., remembering the sequence and locations of dots, backward digit span). Each participant completed the same 11 exercises; however, the length of the spatial or verbal list and adaptiveness or non-adaptiveness of the training program varied with version received. In the high-dose, treatment CWMT condition, the length of the list was automatically adjusted by the program on a trial-by-trial basis, to match the WM span of the participant on that particular exercise (i.e., adaptive CWMT). In the low-dose, non-adaptive, active control condition, the length of the list was set to a maximum of level three, with only three lights, letters, or numbers, maximum, appearing for the duration of the training. All participants completed their exercises on a computer with an Internet connection. The program provided positive feedback verbally, after most successful trials. In addition, participants also received “energy” on all successful trials that they could use in a video game involving racing robots at the end of each day of training.
Participants completed a total of 120 trials per day (15 trials in each eight daily exercises) before they were allowed to progress to the next day of training. Performance on the training exercises was automatically uploaded to a secure website that was monitored for compliance by project researchers. All researchers involved in training were certified by Cogmed to administer the intervention and provide “coach calls.” Researchers made weekly phone calls to the adolescents to provide positive feedback for completing each week of training. Phone calls lasted an average of 5 minutes, and coaches provided the same scripted feedback for both treatment and active control conditions to equalize encouragement and motivation for participants. Actual training performance was not discussed with participants. All adolescents, regardless of condition, received a $50 bonus for completing all 25 days of training. Mothers were encouraged to provide small weekly incentives to their adolescents to encourage training compliance (e.g., additional privileges). All participants were instructed to complete 25 training days, although a minimum of 20 days was required for inclusion in study analyses.
Behavioral Parent Training Intervention
Mothers completed five consecutive, once-weekly, 90-minute parent education sessions. The treatment and active control BPT groups met on Sundays (at different times) in the same university classroom. The faculty principal investigator of this study and an advanced doctoral student were the facilitator and co-facilitator, respectively, for both BPT conditions. Based on their availability, mothers were alternated into the two meeting times such that the groups were approximately equal. Subsequently, a blinded researcher with no participant contact randomly assigned treatment to meeting time by a coin flip. Mothers received a $50 bonus for attending all sessions. Mothers were required to complete at least four sessions to be included in analyses.
Treatment BPT description
Our 5-week treatment BPT program combined aspects of several promising programs into a comprehensive and condensed group approach. We drew heavily from COPE (Cunningham, 2006), as well as therapy manuals and parent self-help guides focused on defiant adolescents (Barkley, Edwards, & Robin, 1999; Barkley, Robin, & Benton, 2008). Content was aimed at increasing positive mother-adolescent interactions, adolescent compliance, and maternal control, while reducing mother-adolescent conflict and adolescent oppositional and defiant behavior (see Table 1). Sessions were participatory and involved presentations, discussion, and role-plays of specific parenting skills. Weekly homework was assigned to mothers to practice content with their adolescents in between the group sessions.
Table 1.
Brief Summary of Timetable for Treatment Behavioral Parent Training
| Week | Content of Session |
|---|---|
| 1 | Increasing positive interactions; decreasing negative interactions; ignoring minor misbehavior, minimizing nattering |
| 2 | Behavioral reinforcement (anticipate behaviors and consequences); reducing negative interactions; effective commands; immediate timing; increasing positive commands |
| 3 | Communication skills; reflective listening and responsiveness; “I-messages” and non-judgmental statements to encourage communication |
| 4 | Reducing maternal reactivity; reframing maternal unreasonable beliefs and expectations |
| 5 | Advanced contingencies; point systems and contracts; Premack principle; rights versus privileges; predictability of consequences |
Active control BPT description
The active control BPT program consisted of 5 weeks of didactic lectures on adolescent physical, cognitive, emotional, and social development. For homework, weekly readings were assigned from a self-help adolescent development guide for parents (Steinberg, 2011). There were no opportunities for practice or feedback concerning specific parenting skills during the didactic sessions.
Results
Sample descriptive characteristics at pretest of each of the four groups and the sample as a whole are reported in Table 2. Although the sample reflected a range of income and other resources, participants were generally from middle-class households and mothers were well-educated.
Table 2.
Participant Characteristics by Treatment (Tx)/Control (Ctrl) Group Combination
| Group 1: Tx WMT/ Tx BPT n = 22 |
Group 2: Tx WMT/ Ctrl BPT n = 22 |
Group 3: Ctrl WMT/ Tx BPT n = 24 |
Group 4: Ctrl WMT/ Ctrl BPT n = 23 |
Total Sample N = 91 |
Group difference F tests |
|||
|---|---|---|---|---|---|---|---|---|
| Measure | M(SD) | M(SD) | M(SD) | M(SD) | M(SD) | F | df | p |
| Adolescent age (years) | 12.6(1.3) | 12.0(1.0) | 12.6(1.3) | 12.7(1.0) | 12.5(1.2) | 2.09 | 90 | .11 |
| Adolescent school grade | 7.0(1.0) | 6.5(1.1) | 7.4(1.2) | 7.4(1.1) | 7.1(1.2) | 3.82 | 90 | .01* |
| Adolescent Full Scale IQ | 102.5(16.9) | 106.0(11.7) | 108.2(14.3) | 109.4(12.0) | 106.5(13.9) | 1.10 | 90 | .35 |
| Mother age (years) | 43.3(8.5) | 40.4(4.8) | 44.3(6.0) | 43.1(7.8) | 42.8(7.0) | 1.31 | 90 | .28 |
| Mother education (years) | 14.7(3.2) | 16.2(3.0) | 16.5(3.1) | 15.3(2.2) | 15.7(2.9) | 1.90 | 90 | .14 |
| Family total income (dollars) | 78,550(60,129) | 91,952(73,685) | 81,643(40,425) | 75,818(52,363) | 81,874(56,855) | 0.32 | 90 | .81 |
| Adolescent gender | 77% Male | 55% Male | 71% Male | 74% Male | 69% Male | |||
| Adolescent race/ethnicity | 95% Caucasian 5% Biracial |
77% Caucasian 5% Hispanic 18% Biracial |
88% Caucasian 8% African American 4% Biracial |
91% Caucasian 9% Biracial |
86% Caucasian 3% African American 1% Hispanic 10% Biracial |
|||
| ADHD subtype | 45% Inattentive 55% Combined |
36% Inattentive 64% Combined |
33% Inattentive 67% Combined |
39% Inattentive 52% Combined 9% H/I |
39% Inattentive 59% Combined 2% H/I |
|||
| Oppositional Defiant Disorder (ODD) diagnosis | 41% | 50% | 29% | 39% | 40% | |||
| Other adolescent comorbidity | 5% Depression 9% GAD |
5% Conduct Disorder 5% Depression 9% GAD 5% Tic Disorder |
4% Conduct Disorder 4% GAD 4% Tic Disorder 4% Tourettes |
4% Tic Disorder 4% Tourettes |
2% Conduct Disorder 2% Depression 6% GAD 3% Tic Disorder 2% Tourettes |
|||
| % Medicated | 86% | 86% | 92% | 70% | 84% | |||
| Mother marital status | 77% Married 14% Divorced 5% Single 4% Widowed |
73% Married 18% Divorced 5% Single 4% Widowed |
83% Married 13% Divorced 4% Single |
78% Married 18% Divorced 4% Single |
78% Married 16% Divorced 4% Single 2% Widowed |
|||
Note. N = 91 mother-adolescent dyads; H/I = Hyperactive/impulsive; GAD = Generalized Anxiety Disorder.
p < .05
Intervention Process and Participant Perceptions of Treatment
Adolescent CWMT fidelity
A total of 44 adolescents in the treatment condition and 47 adolescents in the control condition completed at least 20 days of the CWMT. The average spans achieved on the exercises were analyzed using a two-way mixed ANOVA, with training duration (day 1 to day 20) as the within-subjects factor and training condition (treatment vs. control) as the between subjects factor. We used the Greenhouse-Geisser corrected p-value associated with within subject effects due to violation of the sphericity assumption in our data. As expected, there was a significant main effect of training condition, F(1, 89) = 165.31, p < .001, ηp2 = .65, such that the treatment condition achieved significantly higher average spans than the control condition (M = 4.64 items and M = 2.73 items, respectively). There was also a significant interaction between training duration and training condition, F(19, 441) = 18.96, p < .001, ηp2 = .18, which showed that the average span length over time improved for the treatment condition.
Adolescent motivation
A 2 × 2 between-groups ANOVA was conducted to examine adolescent-reported motivation. Results indicated no main effects of either intervention, but a marginally significant interaction between the two, F(1, 87) = 3.83, p = .054. Motivation was higher in the treatment BPT condition (M=60.54, SD = 11.37), than the control BPT condition (M=54.35, SD =10.29), for those in the control CWMT condition [t(47) = 1.955, p = .056]. However, motivation did not differ significantly in the control BPT condition (M=58.14, SD = 14.91) versus the treatment BPT condition (M = 53.77, SD = 14.50), for those in the treatment CWMT condition [t(44) = −.984, p = .331]. Thus, trends suggested that motivation for training was higher when at least one treatment was full-strength, but not when both treatments were full-strength, with highest motivation for training occurring in the control CWMT/treatment BPT condition.
Adolescent compliance with training
A 2 × 2 between-groups ANOVA was conducted to examine mothers’ perceptions of difficulty in maintaining adolescent training compliance. There was a main effect of CWMT condition, F(1, 69) = 9.71, p < .01, indicating that perceived difficulty of maintaining compliance was higher in the treatment (M = 7.28, SD = 2.59) than the control condition (M = 5.24, SD = 2.99). However, the effect of CWMT condition was qualified by a marginally significant interaction between CWMT condition and BPT condition, F(1, 69) = 2.80, p = .099. Difficulty was lower in the control CWMT condition (M = 4.68, SD =2.69), than in the treatment CWMT condition (M = 7.82, SD = 2.32), for those in the treatment BPT condition [t(36) = 3.73, p < .001]. However, difficulty was not significantly different in the control CWMT condition (M = 5.83, SD = 3.24), versus the treatment CWMT condition (M = 6.79, SD =2.78), for those in the control BPT condition [t(37) = .965, p = .341]. Thus, maintaining adolescent compliance was easiest in the control CWMT/treatment BPT condition.
Mother engagement in parent training
ANOVAs revealed no differences in mothers’ program attendance or weekly homework completion/interest as a function of CWMT condition, BPT condition, or their interaction. Mean attendance for all mothers was 4.65 sessions (SD = .480). Mean homework completion/interest for all mothers was 13.18 (SD = 1.87). Given that the potential range of the homework completion/interest variable was 4–16, participating mothers reported substantial homework completion/interest.
Mother blindness to treatment
Recall that mothers were asked for perceptions of whether their adolescents had received a more or less effective version of Cogmed-RM. Assessment of maternal blindness to CWMT condition was conducted by examination of the number of cases in each of four cells created by crossing actual treatment by perceived efficacy of treatment. We compared the observed frequencies to the expected frequencies generated by specification of four alternative models: full knowledge of treatment, no knowledge of treatment, positive bias, and negative bias. Chi-square analysis was conducted to determine the fit of the observed data to each model. For blindness to CWMT condition, the observed data fit the no knowledge model (χ2 (1, N = 73) = .35, p >.05). The no knowledge model constrained the expected frequencies in each of the four cells to be equal. The frequencies we observed in each cell were as follows: received treatment CWMT/perceived more effective CWMT (19); received treatment CWMT/perceived less effective CWMT (17); received control CWMT/perceived less effective CWMT (20); received control CWMT/perceived more effective CWMT (17). None of the other models (i.e., full knowledge, positive bias, or negative bias) fit the observed data (χ2 > 66.50, p < .05, for all three models).
Mothers were also asked for their perception of BPT version received. Again, we used chi-square analysis to compare observed frequencies to the expected frequencies generated by the four models. For BPT, the observed data fit the positive bias model (χ2 (1, N = 73) = 2.08, p >.05). The positive bias model predicted that the majority of cases would cluster in the two cells indicating perceived effective BPT. Our observed data revealed that 31 mothers were in the received treatment BPT/perceived more effective BPT cell, and 29 mothers were in the received control BPT/perceived more effective BPT cell. Only 13 cases were found in the two cells indicating perceptions of less effective BPT (5 incorrect and 8 correct). Fit of the observed data to all other models was poor (χ2 > 30, p < .05 for all three models). Thus, mothers demonstrated a bias toward believing they received effective BPT, regardless of actual BPT assignment.
Primary Statistical Analyses
Data analysis included a series of General Linear Model (GLM) procedures to examine change in primary outcomes. This framework is optimal given the need to accommodate for unequal group sizes at the posttest time point due to participant attrition. Specifically, we tested difference scores from pretest to posttest using repeated measures analysis of variance (RM ANOVA), with the CWMT and BPT intervention condition (treatment and active control of each) as the between-subjects factors, and time (pretest and posttest) as the within-subjects factor. Univariate RM ANOVA analyses were used because each outcome was conceptualized as distinct from one another (i.e., there were no consistent significant correlations among outcomes, nor among parent and teacher reports of outcomes). The above mixed-effect tests yielded potential main effects of time, 2-way CWMT or BPT condition by time interactions and 3-way CWMT condition by BPT condition by time interactions. Effect sizes were reported as partial eta-squared (ηp2), with values of .01 indicating a small effect, .06 indicating a medium effect, and .14 indicating a large effect (Cohen, 1988). Significant 3-way interactions were probed with Fisher LSD post-hoc analyses. Means and standard deviations for all outcomes by treatment group are reported in Table 3.
Table 3.
Means and Standard Deviations for Study Outcomes at Pretest and Posttest
| Outcome Measures | Mean Pretest (SD) | Mean Posttest (SD) | ||||||
|---|---|---|---|---|---|---|---|---|
| Group 1: Tx WMT/ Tx BPT |
Group 2: Tx WMT/ Ctrl BPT |
Group 3: Ctrl WMT/ Tx BPT |
Group 4: Ctrl WMT/ Ctrl BPT |
Group 1: Tx WMT/ Tx BPT |
Group 2: Tx WMT/ Ctrl BPT |
Group 3: Ctrl WMT/ Tx BPT |
Group 4: Ctrl WMT/ Ctrl BPT |
|
| WISC-IV WM Span | ||||||||
| Forward digit span | 8.23(2.8) | 9.18(2.6) | 8.63(2.7) | 8.83(1.2) | 9.05(2.8) | 10.00(2.1) | 9.63(2.7) | 9.43(2.2) |
| Backward digit span | 7.14(2.1) | 7.45(1.8) | 7.46(1.7) | 7.65(2.0) | 8.36(2.7) | 9.09(1.9) | 8.46(2.4) | 7.87(2.1) |
| Forward spatial span | 6.86(1.8) | 7.14(2.3) | 7.79(1.6) | 7.48(2.8) | 8.50(2.0) | 9.18(1.6) | 8.04(2.3) | 7.91(2.3) |
| Backward spatial span | 6.68(1.6) | 7.27(1.9) | 6.87(2.3) | 6.78(2.2) | 8.23(2.9) | 8.09(2.0) | 7.58(2.9) | 7.04(2.3) |
| WM Deficit Ratings | ||||||||
| Mother | 24.05(4.0) | 25.09(4.0) | 24.46(3.9) | 23.48(3.7) | 22.23(4.9) | 21.91(4.2) | 19.88(4.8) | 20.96(3.8) |
| Teacher | 18.64(5.8) | 18.64(5.0) | 18.13(5.3) | 16.95(4.8) | 17.73(6.1) | 17.00(4.3) | 16.96(5.0) | 16.33(5.0) |
| Inattentive Symptoms | ||||||||
| Mother | 20.95(5.4) | 21.64(3.6) | 19.29(5.7) | 18.43(5.8) | 14.50(5.8) | 13.91(5.1) | 11.92(5.9) | 12.78(3.7) |
| Teacher | 10.63(6.9) | 11.05(6.4) | 11.13(7.2) | 8.76(6.5) | 9.77(7.5) | 7.77(5.7) | 9.00(6.8) | 6.81(4.8) |
| Hyperactive/Impulsive Symptoms | ||||||||
| Mother | 13.45(8.0) | 15.00(6.9) | 14.50(6.0) | 12.96(6.3) | 9.55(6.1) | 9.81(5.9) | 7.83(5.2) | 8.87(5.0) |
| Teacher | 5.41(5.3) | 6.50(5.9) | 6.67(6.4) | 4.47(4.8) | 4.55(5.3) | 4.95(4.8) | 4.13(4.0) | 3.86(4.7) |
| Parenting Behaviors | ||||||||
| Involvement | 40.77(3.0) | 40.41(3.7) | 41.00(5.8) | 38.43(4.1) | 39.86(3.7) | 40.36(4.5) | 41.13(5.0) | 37.78(3.9) |
| Positive Parenting | 24.86(3.0) | 25.18(2.9) | 25.00(3.8) | 23.61(3.5) | 25.00(3.3) | 25.05(2.9) | 24.79(3.3) | 23.00(3.6) |
| Poor monitoring/supervision | 14.41(3.7) | 15.64(3.6) | 16.08(4.3) | 14.43(3.3) | 14.36(4.4) | 15.23(2.7) | 14.25(3.6) | 14.17(3.0) |
| Inconsistent discipline | 14.18(3.5) | 14.41(4.2) | 12.26(3.8) | 13.39(3.9) | 12.91(3.3) | 13.14(3.8) | 11.61(3.0) | 12.43(3.4) |
| Oppositional Behaviors | 3.59(2.4) | 4.45(2.2) | 4.21(2.5) | 4.26(2.0) | 3.50(2.5) | 3.81(2.5) | 3.17(2.3) | 3.91(1.5) |
| Mother-Adolescent Conflict | 36.05(8.9) | 36.68(9.4) | 34.54(8.7) | 36.13(8.6) | 35.18(6.6) | 34.73(7.2) | 32.67(6.8) | 34.87(7.0) |
| Behavior Regulation Problems | ||||||||
| Mother | 55.73(12.5) | 57.32(10.8) | 54.33(11.5) | 54.43(11.0) | 49.77(12.5) | 47.77(9.8) | 43.29(9.6) | 48.00(8.9) |
| Teacher | 40.09(11.0) | 43.09(12.1) | 43.58(14.7) | 39.33(10.6) | 38.86(10.4) | 43.00(11.7) | 42.63(12.3) | 38.29(9.3) |
| Global Executive Deficit | ||||||||
| Mother | 159.18(25.0) | 164.59(19.9) | 156.50(23.2) | 153.61(17.5) | 146.55(27.5) | 142.18(20.4) | 130.71(21.8) | 140.09(18.0) |
| Teacher | 119.72(29.9) | 122.00(30.8) | 122.92(34.8) | 111.33(25.3) | 114.45(30.3) | 116.00(29.5) | 117.50(32.5) | 106.29(24.5) |
Note. N = 91 mother-adolescent dyads, and 89 teachers; Tx = treatment condition; Ctrl = control condition. Mothers reported on all parenting behaviors, oppositional behaviors, and conflict.
Adolescent WM Outcomes
Results indicated main effects of time for WM assessed as forward digit span, F(1, 87) = 29.90, p < .01, ηp2 = .26, backward digit span, F(1, 87) = 28.69, p < .01, ηp2 = .25, forward spatial span, F(1, 87) = 25.59, p < .01, ηp2 = .23, and backward spatial span, F(1, 87) = 18.66, p < .01, ηp2 = .18, such that all adolescents improved on spans over time (see Table 3). However, main effects were qualified by significant 2-way CWMT condition by time interactions for backward digit span, F(1, 87) = 4.67, p < .05, ηp2 = .05, and forward spatial span, F(1, 87) = 12.06, p < .01, ηp2 = .12, but not forward digit span, F < 1, or backward spatial span, F(1, 87) = 3.27, p = .074, ηp2 = .04. The interactions showed that, as hypothesized, from pretest to posttest, adolescents in the CWMT treatment condition generally achieved higher WM spans than did adolescents in the control condition.
Regarding subjective ratings of adolescent WM deficit, mother reports indicated a main effect of time, F(1, 87) = 69.22, p < .001, ηp2 = .44, showing that all adolescents decreased on WM deficit from pretest to posttest. There was no evidence of a 2-way CWMT condition by time interaction for mother ratings of WM deficit, F(1, 87) = 2.09, p = .152, ηp2 = .02. However, a 3-way interaction also emerged among CWMT condition, BPT condition, and time F(1, 87) = 5.54, p < .05, ηp2 = .06. Probing revealed that the largest pretest-posttest reductions in mother-reported WM deficit occurred in the control CWMT/treatment BPT group. LSD post-hoc analyses indicated that the control CWMT/treatment BPT group showed significantly larger pretest-posttest reductions in mother-reported WM deficit compared to both the treatment WMT/treatment BPT group (p < .01) and the control CWMT/control BPT group (p < .05). This finding was unexpected and will be discussed below.
Results for teacher reports of WM deficit showed a main effect of time, F(1, 85) = 8.22, p < .01, ηp2 = .09, such that all adolescents improved on WM deficit from pretest to posttest (see Table 3). No significant 2- or 3-way interactions for teacher ratings of adolescent WM were detected, all Fs < 1.
Adolescent ADHD Symptom Outcomes
Next, we examined mother and teacher reports of adolescent inattentive and H/I symptoms from pretest to posttest. Main effects of time were present for mother reports of inattentive symptoms, F(1, 87) = 73.06, p < .001, ηp2 = .57, and H/I symptoms, F(1, 87) = 63.47, p < .001, ηp2 = .42, which indicated that all adolescents showed decreased inattentive and H/I symptoms from pretest to posttest (see Table 3). There were no significant interactions between CWMT condition and time for ADHD symptoms, Fs < 1. Contrary to hypothesis, no significant BPT condition by time interactions were detected for mother reports of ADHD symptoms, Fs < 1. The 3-way interactions among CWMT condition, BPT condition, and time were also not significant for mother-rated ADHD symptoms, Fs < 1. Teacher reports of ADHD symptoms showed similar patterns of results as mother-reported symptoms. Specifically, main effects of time were found for inattentive symptoms, F(1, 85) = 15.21, p < .001, ηp2 = .15, and H/I symptoms, F(1, 85) = 13.49, p < .001, ηp2 = .14 (see Table 3). However, no significant 2- or 3-way interactions for teacher reports of ADHD symptoms were detected, all Fs < 1.
Mother and Adolescent Parenting-Related Outcomes
Parenting behavior outcomes included maternal involvement, positive parenting, poor monitoring/supervision, and inconsistent discipline. Contrary to hypothesis, there was no significant 2-way interaction between BPT condition and time for maternal involvement, F < 1. Furthermore, there was no significant 3-way interaction among CWMT condition, BPT condition, and time, F(1, 87) = 2.08, p = .153, ηp2 = .02 for involvement. Similarly, results for positive parenting showed neither 2- nor 3-way interactions, all Fs < 1.
For maternal poor monitoring/supervision, we found a main effect of time, F(1, 87) = 4.83, p < .05, ηp2 = .05, which indicated that all mothers decreased on poor monitoring/supervision from pretest to posttest (see Table 3). Contrary to hypothesis, there was no 2-way interaction between BPT condition and time, F(1, 87) = 1.09, p = .300, ηp2 = .01. There was also no significant 3-way interaction among CWMT condition, BPT condition, and time, F(1, 87) = 2.79, p = .098, ηp2 = .03, for poor monitoring/supervision.
Results for maternal inconsistent discipline showed a significant main effect of time, F(1, 87) = 18.94, p < .01, ηp2 = .18, which indicated that all mothers improved on maternal inconsistent discipline from pretest to posttest (see Table 3). Contrary to hypothesis, there was no significant 2-way interaction between BPT condition and time, F < 1. A significant 3-way interaction was also not detected, F < 1.
Analysis of adolescent oppositional behaviors revealed a main effect of time, F(1, 87) = 7.03, p = .010, ηp2 = .08. The main effect indicated that all mothers, regardless of condition, reported fewer adolescent oppositional behaviors over time (see Table 3). Contrary to hypothesis, we found no 2-way interaction between BPT condition and time, F < 1. There was also no significant 3-way interaction among CWMT condition, BPT condition, and time, F(1, 87) = 2.41, p = .124, ηp2 = .03.
Lastly, we examined change in mother-adolescent conflict. Results showed a main effect of time, F(1, 87) = 8.09, p < .05, ηp2 = .09, such that all mothers, regardless of group condition, reported decreased conflict from pretest to posttest (see Table 3). Contrary to hypothesis, we found no significant 2-way interaction between BPT condition and time, F < 1. We also detected no significant 3-way interaction among CWMT, BPT, and time, F < 1.
Adolescent Global Functioning Outcomes
Mother reports concerning change in adolescent behavior regulation showed a significant main effect of time, F(1, 87) = 83.10, p < .01, ηp2 = .49, indicating that all adolescents decreased on behavior regulation problems (see Table 3). There was also a significant 3-way interaction among CWMT condition, BPT condition, and time, F(1, 87) = 5.14, p < .05, ηp2 = .06. LSD post-hoc analyses showed that the control CWMT/treatment BPT group had significantly larger pretest-posttest reductions in mother-reported behavior regulation problems compared to the treatment CWMT/treatment BPT group (p < .05). This finding was unexpected and will be discussed below. Contrary to hypothesis, for teacher reports of adolescent behavior regulation problems, there was no significant 3-way interaction, F < 1.
Finally, for adolescent global executive deficit, mother reports showed a significant main effect of time, F(1, 87) = 85.67, p < .01, ηp2 = .50, which indicated that all adolescents decreased on global executive problems (see Table 3). Results also revealed a significant 3-way interaction among CWMT condition, BPT condition, and time, F(1, 87) = 7.53, p < .05, ηp2 = .08. LSD post-hoc analyses revealed that the control CWMT/treatment BPT group had significantly larger pretest-posttest reductions in mother-reported global executive deficit compared to both the treatment CWMT/treatment BPT group and the control CWMT/control BPT group (all ps < .05). This finding was unanticipated, and will be discussed below. Finally, teacher reports of adolescent global executive deficit demonstrated a significant main effect of time, F(1, 85) = 7.27, p < .01, ηp2 = .08, such that all adolescents decreased on global executive problems from pretest to posttest. Contrary to hypothesis, there was no significant 3-way interaction for teacher-reported global executive deficit, F < 1 (see Table 3)
Discussion
In this study, we examined the separate and combined effects of CWMT and BPT for adolescents with ADHD and their mothers. As expected, CWMT alone increased WM when performance was measured with laboratory assessments of active maintenance of information. Furthermore, we found no evidence that CWMT alone affected ADHD symptoms. Turning to our BPT intervention, there was no evidence of improvement in parenting-related outcomes as a function of BPT alone. There were main effects of time on many study outcomes, indicating improvement regardless of assignment to treatment or control conditions.
We also found no evidence of synergistic effects of treatment CWMT combined with treatment BPT. However, we found a pattern in which greatest improvements on selected outcomes occurred in the control CWMT/treatment BPT group. Our findings concerning this particular group have important implications for the use of non-adaptive control conditions in evaluations of CWMT, and for the use of control groups in evaluations of cognitive interventions more generally. Below, we discuss our main findings and their implications, and suggest directions for future research.
Working Memory, Behavior Regulation, and Global Executive Functioning Outcomes
Outcomes focused on adolescent WM differed depending on assessment method. Objective laboratory span tasks generally revealed higher post-training spans in the CWMT treatment condition, a finding consistent with prior research indicating improvement when posttest assessments are similar to trained tasks and primarily assess active maintenance of information (for review, see Melby-Lervåg & Hulme, 2012; Shipstead et al., 2012). In contrast, maternal ratings of WM (as well as behavior regulation and global executive functioning) were most improved in the control CWMT/treatment BPT group. The control CWMT condition was intended to produce a structurally equivalent condition lacking potency to affect executive function and regulation. Why then would mothers in the control CWMT/treatment BPT group report greater functioning, when objective improvements as a function of control CWMT alone were not detected?
Our analysis of training process and perceptions revealed that mothers of adolescents in the treatment CWMT condition perceived the training to be more difficult to accomplish than did mothers of adolescents in the control CWMT condition. Such differing perceptions are sensible, given that the adaptive, treatment CWMT condition becomes progressively more difficult over time. In adaptive training, although an individual’s WM spans typically increase over the training period, so does the challenge. Thus, participants completing treatment CWMT (and their mothers) may have been sensitized, in part, to difficulties in executive functioning. In contrast, those in the control, non-adaptive condition may have come away from the experience with the perception that adolescent functioning was not that impaired, given the relative ease of the task over five weeks. At the same time, mothers in treatment BPT were being encouraged to become more positive about their adolescent and their relationship. When an adolescent is not struggling with the cognitive training, and, when a mother is simultaneously adopting a more positive viewpoint, a mother may be inclined to rate adolescent deficits as less substantial at posttest. This pattern may be especially likely to occur if mothers remain blind to cognitive treatment condition, as did the mothers in our study. Thus, we may have strengthened a dynamic in which certain mothers of those in the non-adaptive, control CWMT condition perceived that their adolescents were doing well at executive functioning tasks expected to be challenging.
Our interpretation of the patterns yielded by maternal ratings is bolstered by our findings concerning teacher ratings of WM and global executive function, which demonstrated only main effects of improvement over time. Teachers were aware that their students were completing an intervention, but did not have exposure to training progress, and were not given any intervention themselves. In this context, teachers’ improved ratings may have been influenced by expectancy or by nonspecific improvements in adolescent functioning. The fact that improvement in the control CWMT/treatment BPT group was not replicated between mother and teacher ratings is consistent with our explanation that mothers’ post-intervention perceptions may have been influenced by their particular experience of their adolescents’ cognitive training, juxtaposed with their parent training.
Although our interpretation of unanticipated findings (i.e., greatest improvements on several outcomes for the control CWMT/treatment BPT group) is necessarily preliminary and must be taken with caution, we note that other recent CWMT evaluations using non-adaptive controls have found similar trends indicating improvements in the control condition (Chacko, Bedard, et al., 2013; van Dongen-Boomsma et al., 2014). In Chacko et al. (2013), children with ADHD completed adaptive or non-adaptive CWMT, as did the adolescents in our study. The intervention included an “enhanced engagement procedure” which mothers completed prior to initiation of CWMT. The engagement procedure consisted of individual sessions designed to foster maternal motivation for continued participation and reduce perceived barriers to treatment.
Of most relevance to the present study, Chacko et al. (2013) reported that treatment effects were not significant for maternal ratings of child inattentive and hyperactive symptoms. However, Chacko et al. also reported negative effect size estimates for mother-rated ADHD symptoms, with negative coefficients indicating beneficial effects of the control, relative to the treatment condition. Given the engagement procedure, the mothers in the study may have formed an expectation that CWMT would be difficult, and indeed had been prepared by study researchers to overcome expected difficulties. We argue that when the training at home is not difficult (i.e., when the child completes non-adaptive training), parents may interpret the lack of difficulty as indicating improvement in functioning, or decrease in symptoms. Furthermore, such uncontrolled potential bias operating in a non-adaptive control group may reduce the opportunity to find treatment effects. Discussion of appropriate control groups in the WM training literature has rightly centered on ruling out non-specific factors (e.g., practice, blindness, motivation) that might inadvertently bias results toward apparent treatment effects (Morrison & Chein, 2011; Rapport et al., 2013). We note that it is also important to avoid bias against treatment effects, and that appropriate control groups will help counter bias in both directions.
For future research, we recommend that if a study uses non-adaptive WM training as the control condition and includes parent ratings, the training should be implemented outside of the home (e.g., at school), so that parents are never directly aware of the experience of training (Gray et al., 2012). If training occurs at home and includes parent ratings, we recommend that all participants receive adaptive, equally difficult, structurally equivalent, and credible training that targets the components of WM that are either theoretically relevant (treatment condition) or irrelevant (control condition) to ADHD (Gibson et al., 2011; 2013; Gibson, Gondoli, et al., 2012; Gibson, Kronenberger et al., 2012).
ADHD Symptom Outcomes
Both mother and teacher ratings of inattentive and H/I symptoms showed only main effects of time. Although some CWMT studies with waitlist control conditions have found ADHD symptom improvement following treatment (e.g., Beck et al., 2010), other studies with active control groups found no effect of treatment (e.g., Green et al., 2012). Furthermore, although some prior studies revealed positive effects of BPT on parent ratings of child ADHD symptoms, these studies used waitlist controls (Sibley et al., 2011; Thorell, 2009), or included several psychosocial treatments (e.g., MTA Cooperative Group, 1999), making it difficult to ascertain the specific effectiveness of BPT on parent-rated ADHD symptoms. Clearly, further controlled studies on the effects of cognitive training and BPT on ADHD symptoms and impairments, whether singly or in combination, are needed.
Parenting-Related Outcomes
Although we expected that treatment BPT would produce better parenting-related outcomes than would control BPT, we found no evidence of this pattern. Rather, effects concerning BPT were main effects indicating improvement over time for both treatment and control conditions. In contrast to recent similar combined treatment studies (e.g., Neville et al., 2013), we also found no evidence that high levels of both CWMT and BPT produced a synergistic effect.
Several possibilities may account for lack of differential effectiveness of our treatment BPT. Perhaps the mothers in the control BPT condition independently applied information that was covered in the didactic presentations and the homework readings. In addition, although brief BPT interventions have some support (Chronis-Tuscano et al., 2011), several other programs were longer than our program (Chacko et al., 2009; Sibley et al., 2013). Thus, it is possible that our treatment was not long enough to be maximally effective. Too, our measures of parenting, although widely used and appropriate, may not have been sensitive to change in the particular skills trained in the treatment condition. We also note that we used a structurally equivalent, active, and credible control condition, and this stringent approach may have made it difficult to obtain effects of treatment. When active controls are utilized, positive expectancies and nonspecific benefits such as enhanced social support are likely equalized across groups (Borkowski & Farris, 2013), and such may diminish distinctiveness of treatment. However, although designs including active control conditions clearly present challenges, we argue that accurate information about treatment effectiveness cannot be gained in the absence of appropriate controls. Use of active control conditions does require substantial power and sensitive measurement, and research going forward should reflect these characteristics.
Conclusions
Similar to other recent CWMT studies (Chacko, Bedard et al., 2013; Gray et al. 2012; van Dongen-Boosma et al., 2014), we found no evidence that CWMT, either singly, or in combination with BPT, positively affected diverse domains of functioning. Lack of positive evidence for CWMT has prompted suggestions that this approach should not be considered an efficacious treatment for ADHD or its underlying cognitive impairments (Chacko, Feirsen et al., 2013; Gray et al., 2012; Melby-Lervåg & Hulme, 2012). However, CWMT may not be expected to demonstrate wide-ranging effects unless combined with additional treatments which address varied domains of impairment (Gathercole, 2014). Thus, cognitive training may still have potential therapeutic utility if paired with other individualized treatments. Furthermore, adaptations to the standard CWMT program have been proposed, which might better target domains of WM functioning theoretically relevant to ADHD (i.e., impaired retrieval from secondary memory; Gibson et al., 2011; 2013; Gibson, Gondoli, et al., 2012; Gibson, Kronenberger et al., 2012). Perhaps a more potent CWMT intervention, combined with BPT or other ancillary treatment, might yield more promising outcomes (Chacko et al., 2014). In any case, mixed findings in the current literature, as well as the continuing need for efficacious, non-pharmacological treatments for ADHD, argue for continued study.
Our study demonstrated the feasibility of combining cognitive training for adolescents with BPT for their mothers. We focused on adolescents, who remain under-researched in the ADHD treatment literature (Evans et al., 2014). We included active control groups, and we considered the separate and combined effectiveness of two distinct treatments. We assessed aspects of treatment process that have been neglected in the literature, including blindness and motivation. Our study also yielded important methodological information concerning control conditions in cognitive training. Our study also has some limitations. Although we included participants with a range of resources, the sample was relatively affluent, and findings may not generalize to predominantly at-risk samples. Furthermore, given our inclusion of only mother-adolescent dyads, our findings may not generalize to father-adolescent dyads.
Finally, our study highlights the complexities of treating adolescents with ADHD. Developmental considerations during adolescence (e.g., sensitive period for prefrontal and parietal cortex brain development, greater parent-adolescent conflict, poor medication adherence) contribute to the need for novel multimodal treatments for adolescents with ADHD and their families (Rutledge, van den Bos, McClure, & Schweitzer, 2012; Smith et al., 2000). Critical needs for future research and treatment include development of integrated, ecologically valid interventions, and controlled evaluations. Implementation of theory-based interventions, coupled with consideration of a range of outcomes, will be useful in determining the full extent of intervention effects on individual and family functional domains.
Acknowledgments
Funding for the project was provided to the authors from Translational Research Pilot Fund, Indiana Clinical and Translational Sciences Institute (I-CTSI) [NIH Award RR025761]; Predoctoral Training Fellowship in Translational Research (NIH/NCRR-I-CTSI)-TL1 Program (A. Shekhar, PI); Fahs-Beck Fund for Research and Experimentation; and the Institute for Scholarship in the Liberal Arts, Office of Research, Swarm Graduate Research Award Program, and Kill Family Fund for ADHD research, all at the University of Notre Dame. Manuscript preparation was supported in part by an NIH/NIDA T32 Research Training Program in Substance Abuse Prevention Research (Yale University School of Medicine). The content is solely the responsibility of the authors and does not necessarily represent the official views of any of the funding entities. The authors wish to thank the participants of this study, and Pearson/Cogmed for their partnership. They would also like to thank their research team, and make special acknowledgement of the generous research support from the Kill family. The authors received no honoraria or compensation.
Footnotes
The authors have declared no competing or potential conflicts of interest.
References
- Abikoff H, Hechtman L, Klein RG, Weiss G, Fleiss K, Etcovitch J, Pollack S. Symptomatic improvement in children with ADHD treated with long-term methylphenidate and multimodal psychosocial treatment. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:802–811. doi: 10.1097/01.chi.0000128791.10014.ac. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 2000. (text rev.) [Google Scholar]
- Barkley RA, Edwards GH, Robin AL. Defiant teens: A clinician's manual for assessment and family intervention. New York, NY: Guilford Press; 1999. [Google Scholar]
- Barkley RA, Guevremont DC, Anastopoulos AD, Fletcher KE. A comparison of three family therapy programs for treating family conflicts in adolescents with attention-deficit hyperactivity disorder. Journal of Consulting and Clinical Psychology. 1992;60:450–462. doi: 10.1037/0022-006X.60.3.450. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Robin AL, Benton CM. Your defiant teen: 10 steps to resolve conflict and rebuild your relationship. New York, NY: Guilford Press; 2008. [Google Scholar]
- Beck SJ, Hanson CA, Puffenberger SS, Benninger KL, Benninger WB. A controlled trial of working memory training for children and adolescents with ADHD. Journal of Clinical Child & Adolescent Psychology. 2010;39:825–836. doi: 10.1080/15374416.2010.517162. [DOI] [PubMed] [Google Scholar]
- Belsky J, Pasco Fearon RM, Bell B. Parenting, attention and externalizing problems: Testing mediation longitudinally, repeatedly and reciprocally. Journal of Child Psychology and Psychiatry. 2007;48:1233–1242. doi: 10.1111/j.1469-7610.2007.01807.x. [DOI] [PubMed] [Google Scholar]
- Borkowski JG, Farris JR. Executive Summary to the Pew Center on the States on an Early, Intensive Parenting Intervention to Prevent Child Neglect: Five Year Mother-Child Outcomes. 2013 Retrieved from http://www.pewstates.org/uploadedFiles/PCS_Assets/2013/My_Baby_and_Me_executive_summary.pdf. [Google Scholar]
- Chacko A, Bedard AC, Marks DJ, Feirsen N, Uderman JZ, Chimiklis A, Ramon M. A randomized clinical trial of Cogmed working memory training in school-age children with ADHD: A replication in a diverse sample using a control condition. Journal of Child Psychology and Psychiatry. 2013;55:247–255. doi: 10.1111/jcpp.12146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chacko A, Feirsen N, Bedard AC, Marks D, Uderman JZ, Chimiklis A. Cogmed working memory training for youth with ADHD: A closer examination of efficacy utilizing evidence-based criteria. Journal of Clinical Child & Adolescent Psychology. 2013;42:769–783. doi: 10.1080/15374416.2013.787622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chacko A, Kofler M, Jarrett M. Improving outcomes for youth with ADHD: A conceptual framework for combined neurocognitive and skill-based treatment approaches. [August, 2014];Clinical Child and Family Psychology Review. 2014 doi: 10.1007/s10567-014-0171-5. published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chacko A, Wymbs BT, Wymbs FA, Pelham WE, Swanger-Gagne MS, Girio E, O'Connor B. Enhancing traditional behavioral parent training for single mothers of children with ADHD. Journal of Clinical Child & Adolescent Psychology. 2009;38:206–218. doi: 10.1080/15374410802698388. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, O’Brien KA, Johnston C, Jones HA, Clarke TL, Raggi VL, Seymour KE. The relation between maternal ADHD symptoms and improvement in child behavior following brief behavioral parent training is mediated by change in negative parenting. Journal of Abnormal Child Psychology. 2011;39:1047–1057. doi: 10.1007/s10802-011-9518-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cunningham CE. COPE: Large-group, community-based, family-centered parent training. In: Barkley RA, editor. Attention deficit/hyperactivity disorder: A handbook for diagnosis and treatment. 3rd ed. New York, NY: Guilford Press; 2006. pp. 480–498. [Google Scholar]
- Dadds MR, Maujean A, Fraser JA. Parenting and conduct problems in children: Australian data and psychometric properties of the Alabama Parenting Questionnaire. Australian Psychologist. 2003;38:238–241. [Google Scholar]
- Deault LC. A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder (ADHD) Child Psychiatry & Human Development. 2010;41:168–192. doi: 10.1007/s10578-009-0159-4. [DOI] [PubMed] [Google Scholar]
- Deci EL, Ryan RM. [on October 14, 2011];Intrinsic motivation inventory (IMI) (n.d.). Retrieved from http://www.psych.rochester.edu/SDT/measures/IMI_description.php. [Google Scholar]
- Dishion TJ, Patterson GR. The development and ecology of antisocial behavior in children and adolescents. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Vol. 3, Risk, disorder, and adaptation. 2nd ed. Hoboken, NJ: John Wiley & Sons; 2006. pp. 503–541. [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos AD, Reid R. ADHD rating scale—IV: Checklist, norms, and clinical interpretation. New York, NY: Guilford Press; 1998. [Google Scholar]
- Eisenberg N, Zhou Q, Spinrad TL, Valiente C, Fabes RA, Liew J. Relations among positive parenting, children's effortful control, and externalizing problems: A three-wave longitudinal study. Child Development. 2005;76:1055–1071. doi: 10.1111/j.1467-8624.2005.00897.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SW, Owens JS, Bunford N. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology. 2014;43:527–551. doi: 10.1080/15374416.2013.850700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faries DE, Yalcin I, Harder D, Heiligenstein JH. Validation of the ADHD rating scale as a clinician administered and scored instrument. Journal of Attention Disorders. 2001;5:107–115. [Google Scholar]
- Frick PJ. The Alabama parenting questionnaire. Tuscaloosa, AL: University of Alabama; 1991. Unpublished rating scale. [Google Scholar]
- Gathercole SE. Commentary: Working memory training and ADHD— where does its potential lie? Reflections on Chacko et al. (2014) Journal of Child Psychology and Psychiatry. 2014;55:256–257. doi: 10.1111/jcpp.12196. [DOI] [PubMed] [Google Scholar]
- Gibson BS, Gondoli DM, Johnson AC, Steeger CM, Dobrzenski BA, Morrissey RA, Thompson AN. Component analysis of verbal versus spatial working memory training in adolescents with ADHD: A randomized, controlled trial. Child Neuropsychology. 2011;17:546–563. doi: 10.1080/09297049.2010.551186. [DOI] [PubMed] [Google Scholar]
- Gibson BS, Gondoli DM, Johnson AC, Steeger CM, Morrissey RA. The future promise of Cogmed working memory training. Journal of Applied Research in Memory and Cognition. 2012;1:214–216. doi: 10.1016/j.jarmac.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson BS, Gondoli DM, Kronenberger WG, Johnson AC, Steeger CM, Morrissey RA. Exploration of an adaptive training regimen that can target the secondary memory component of working memory capacity. Memory & Cognition. 2013;41:726–737. doi: 10.3758/s13421-013-0295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson BS, Kronenberger WG, Gondoli DM, Johnson AC, Morrissey RA, Steeger CM. Component analysis of simple span vs. complex span adaptive working memory exercises: A randomized, controlled trial. Journal of Applied Research in Memory and Cognition. 2012;1:179–184. doi: 10.1016/j.jarmac.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, Kentworthy L. Behavior rating inventory of executive function. Child Neuropsychology. 2000a;6:235–238. doi: 10.1076/chin.6.3.235.3152. [DOI] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior rating inventory of executive function: Professional manual. Lutz, FL: Psychological Assessment Resources; 2000b. [Google Scholar]
- Gray SA, Chaban P, Martinussen R, Goldberg R, Gotlieb H, Kronitz R, Tannock R. Effects of a computerized working memory training program on working memory, attention, and academics in adolescents with severe LD and comorbid ADHD: A randomized controlled trial. Journal of Child Psychology and Psychiatry. 2012;53:1277–1284. doi: 10.1111/j.1469-7610.2012.02592.x. [DOI] [PubMed] [Google Scholar]
- Graziano PA, Calkins SD, Keane SP. Sustained attention development during the toddlerhood to preschool period: Associations with toddlers’ emotion regulation strategies and maternal behavior. Infant and Child Development. 2011;20:389–408. doi: 10.1002/icd.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green CT, Long DL, Green D, Iosif AM, Dixon JF, Miller MR, Schweitzer JB. Will working memory training generalize to improve off-task behavior in children with attention-deficit/hyperactivity disorder? Neurotherapeutics. 2012;9:639–648. doi: 10.1007/s13311-012-0124-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Wells KC, Kraemer HC, Abikoff HB, Arnold LE, Wigal T. Family processes and treatment outcome in the MTA: Negative/ineffective parenting practices in relation to multimodal treatment. Journal of Abnormal Child Psychology. 2000;28:555–568. doi: 10.1023/a:1005183115230. [DOI] [PubMed] [Google Scholar]
- Holmes J, Gathercole SE, Place M, Dunning DL, Hilton KA, Elliott JG. Working memory deficits can be overcome: Impacts of training and medication on working memory in children with ADHD. Applied Cognitive Psychology. 2010;24:827–836. [Google Scholar]
- Johnston C, Mash EJ. Families of children with attention-deficit/hyperactivity disorder: Review and recommendations for future research. Clinical Child and Family Psychology Review. 2001;4:183–207. doi: 10.1023/a:1017592030434. [DOI] [PubMed] [Google Scholar]
- Kane MJ, Engle RW. The role of prefrontal cortex in working-memory capacity, executive attention, and general fluid intelligence: An individual-differences perspective. Psychonomic Bulletin & Review. 2002;9:637–671. doi: 10.3758/bf03196323. [DOI] [PubMed] [Google Scholar]
- Kasper LJ, Alderson RM, Hudec KL. Moderators of working memory deficits in children with attention-deficit/hyperactivity disorder (ADHD): A meta-analytic review. Clinical Psychology Review. 2012;32:605–617. doi: 10.1016/j.cpr.2012.07.001. [DOI] [PubMed] [Google Scholar]
- Kaufman AS, Kaufman NL. Kaufman brief intelligence test- second edition (KBIT-2) Circle Pines, MN: American Guidance Service Publishing; 2004. [Google Scholar]
- Klingberg T. Training and plasticity of working memory. Trends in Cognitive Science. 2010;14:317–324. doi: 10.1016/j.tics.2010.05.002. [DOI] [PubMed] [Google Scholar]
- Klingberg T, Fernell E, Olesen PJ, Johnson M, Gustafsson P, Dahlstrom K, Westerberg H. Computerized training of working memory in children with ADHD— A randomized, controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:177–186. doi: 10.1097/00004583-200502000-00010. [DOI] [PubMed] [Google Scholar]
- Lee P, Niew W, Yang H, Chen V, Lin K. A meta-analysis of behavioral parent training for children with attention deficit hyperactivity disorder. Research in Developmental Disabilities. 2012;33:2040–2049. doi: 10.1016/j.ridd.2012.05.011. [DOI] [PubMed] [Google Scholar]
- Martinussen R, Hayden J, Hogg-Johnson S, Tannock R. A meta-analysis of working memory impairments in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:377–384. doi: 10.1097/01.chi.0000153228.72591.73. [DOI] [PubMed] [Google Scholar]
- Melby-Lervåg M, Hulme C. Is working memory training effective? A meta-analytic review. Developmental Psychology. 2012;49:270–291. doi: 10.1037/a0028228. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, Houck PR. The MTA at 8 years: Prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison AB, Chein JM. Does working memory training work? The promise and challenges of enhancing cognition by training working memory. Psychonomic Bulletin & Review. 2011;18:46–60. doi: 10.3758/s13423-010-0034-0. [DOI] [PubMed] [Google Scholar]
- The MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 1999;56:1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- Neville HJ, Stevens C, Pakula E, Bell TA, Fanning J, Klein S, Isbell E. Family-based training program improves brain function, cognition, and behavior in lower socioeconomic status preschoolers. Proceedings of the National Academy of Sciences. 2013;110:12138–12143. doi: 10.1073/pnas.1304437110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR. Coercive family processes. Eugene, OR: Castalia; 1982. [Google Scholar]
- Pelham WE, Burrows-MacLean L, Gnagy EM, Fabiano GA, Coles EK, Tresco KE, Hoffman MT. Transdermal methylphenidate, behavioral, and combined treatment for children with ADHD. Experimental and Clinical Psychopharmacology. 2005;13:111. doi: 10.1037/1064-1297.13.2.111. [DOI] [PubMed] [Google Scholar]
- Rapport MD, Orban SA, Kofler MJ, Friedman LM. Do programs designed to train working memory, other executive functions, and attention benefit children with ADHD? A meta-analytic review of cognitive, academic, and behavioral outcomes. Clinical Psychology Review. 2013;33:1237–1252. doi: 10.1016/j.cpr.2013.08.005. [DOI] [PubMed] [Google Scholar]
- Robin AL, Foster SL. Negotiating parent-adolescent conflict: A behavioral-family systems approach. New York, NY: Guilford Press; 2002. [Google Scholar]
- Rutledge KJ, van den Bos W, McClure SM, Schweitzer JB. Training cognition in ADHD: Current findings, borrowed concepts, and future directions. Neurotherapeutics. 2012;9:542–558. doi: 10.1007/s13311-012-0134-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH diagnostic interview schedule for children version IV (DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Shelton KK, Frick PJ, Wootton J. Assessment of parenting practices in families of elementary school-aged children. Journal of Clinical Child Psychology. 1996;25:317–329. [Google Scholar]
- Shipstead Z, Hicks KL, Engle RW. Working memory training remains a work in progress. Journal of Applied Research in Memory and Cognition. 2012;1:217–219. [Google Scholar]
- Shipstead Z, Redick TS, Engle RW. Is working memory training effective? Psychological Bulletin. 2012;138:628. doi: 10.1037/a0027473. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Evans SW, Gnagy EM, Ross JM, Greiner AR. An evaluation of a summer treatment program for adolescents with ADHD. Cognitive and Behavioral Practice. 2011;18:530–544. [Google Scholar]
- Sibley MH, Ross JM, Gnagy EM, Dixon LJ, Conn B, Pelham WE. An intensive summer treatment program for ADHD reduces parent–adolescent conflict. Journal of Psychopathology and Behavioral Assessment. 2013;35:10–19. [Google Scholar]
- Smith BH, Waschbusch DA, Willoughby MT, Evans S. The efficacy, safety, and practicality of treatments for adolescents with attention-deficit/hyperactivity disorder (ADHD) Clinical Child and Family Psychology Review. 2000;3:243–267. doi: 10.1023/a:1026477121224. [DOI] [PubMed] [Google Scholar]
- Steeger CM, Gondoli DM. Mother-adolescent conflict as a mediator between adolescent problem behaviors and maternal psychological control. Developmental Psychology. 2013;49:804–814. doi: 10.1037/a0028599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L. You and Your Adolescent: A Parent’s Guide for Ages 10–25. New York, NY: Simon & Schuster; 2011. [Google Scholar]
- Sturge-Apple ML, Gondoli DM, Bonds DD, Salem LN. Mothers’ responsive parenting practices and psychological experience of parenting as mediators of the relation between marital conflict and mother-preadolescent relational negativity. Parenting: Science and Practice. 2003;3:327–355. [Google Scholar]
- Thorell LB. The community parent education program (COPE): Treatment effects in a clinical and a community-based sample. Journal of Clinical Child Psychology and Psychiatry. 2009;14:373–387. doi: 10.1177/1359104509104047. [DOI] [PubMed] [Google Scholar]
- Unsworth N, Engle RW. On the division of short-term and working memory: An examination of simple and complex span and their relation to higher order abilities. Psychological Bulletin. 2007;133:1038–1066. doi: 10.1037/0033-2909.133.6.1038. [DOI] [PubMed] [Google Scholar]
- Van der Oord S, Prins PJ, Oosterlaan J, Emmelkamp PM. Efficacy of methylphenidate, psychosocial treatments and their combination in school-aged children with ADHD: A meta-analysis. Clinical Psychology Review. 2008;28:783–800. doi: 10.1016/j.cpr.2007.10.007. [DOI] [PubMed] [Google Scholar]
- van Dongen-Boomsma M, Vollebregt MA, Buitelaar JK, Slaats-Willemse D. Working memory training in young children with ADHD: A randomized placebo-controlled trial. Journal of Child Psychology and Psychiatry. 2014;55:886–896. doi: 10.1111/jcpp.12218. [DOI] [PubMed] [Google Scholar]
- Wechsler D, Kaplan E, Fein D, Kramer J, Morris R, Delis D, Maerlender A. Wechsler intelligence scales for children– Fourth edition integrated. San Antonio, TX: Psychological Corporation; 2004. [Google Scholar]