Abstract
Background
Elafin is a potent endogenous neutrophil elastase inhibitor that protects against myocardial inflammation and injury in preclinical models of ischaemic-reperfusion injury. We investigated whether elafin could inhibit myocardial ischaemia-reperfusion injury induced during coronary artery bypass graft (CABG) surgery.
Methods and results
In a randomised double-blind placebo-controlled parallel group clinical trial, 87 patients undergoing CABG surgery were randomised 1:1 to intravenous elafin 200 mg or saline placebo administered after induction of anaesthesia and prior to sternotomy. Myocardial injury was measured as cardiac troponin I release over 48 h (area under the curve (AUC)) and myocardial infarction identified with MRI. Postischaemic inflammation was measured by plasma markers including AUC high-sensitive C reactive protein (hs-CRP) and myeloperoxidase (MPO). Elafin infusion was safe and resulted in >3000-fold increase in plasma elafin concentrations and >50% inhibition of elastase activity in the first 24 h. This did not reduce myocardial injury over 48 h (ratio of geometric means (elafin/placebo) of AUC troponin I 0.74 (95% CI 0.47 to 1.15, p=0.18)) although post hoc analysis of the high-sensitive assay revealed lower troponin I concentrations at 6 h in elafin-treated patients (median 2.4 vs 4.1 μg/L, p=0.035). Elafin had no effect on myocardial infarction (elafin, 7/34 vs placebo, 5/35 patients) or on markers of inflammation: mean differences for AUC hs-CRP of 499 mg/L/48 h (95% CI −207 to 1205, p=0.16), and AUC MPO of 238 ng/mL/48 h (95% CI −235 to 711, p=0.320).
Conclusions
There was no strong evidence that neutrophil elastase inhibition with a single-dose elafin treatment reduced myocardial injury and inflammation following CABG-induced ischaemia-reperfusion injury.
Trial registration number
(EudraCT 2010-019527-58, ISRCTN82061264).
Introduction
Ischaemia-reperfusion injury occurs when blood flow is restored to organs and tissues that have sustained a period of interrupted blood supply. This occurs following therapies for acute myocardial infarction and ischaemic stroke, and is a necessary consequence of solid organ transplantation. Mechanisms of cell and tissue injury include a neutrophil-mediated postischaemic inflammatory response and activation of cellular death pathways following reperfusion.1 Protecting organs from ischaemia-reperfusion injury to improve clinical outcome is a high priority. Despite intense research efforts and huge promise from preclinical and early-phase clinical trials, there are currently no effective therapies that can limit this injurious response.
During coronary artery bypass graft (CABG) surgery and cardiopulmonary bypass, coronary blood flow is interrupted and the heart is put into circulatory arrest. This causes ischaemia-reperfusion injury that is exacerbated by adverse neutrophil-mediated myocardial inflammation and injury.2–4 CABG surgery therefore represents a programmed clinical model of ischaemia-reperfusion injury that lends itself to testing the efficacy of potential therapeutic interventions.5
Elafin is an endogenous anti-inflammatory protein that was first isolated in the search for inhibitors of neutrophil elastase activity in the lung and skin.6 7 It has inhibitory activity against both human neutrophil elastase and proteinase-3 as well as suppressing production of inflammatory cytokines such as interleukin (IL)-8 and tumour necrosis factor alpha (TNF-α).8 Elafin is produced locally at sites of inflammation, raising a local defence of ‘alarm’ antiproteases in order to contain and inhibit neutrophil-mediated inflammation.9 Cardiovascular tissues do not express elafin or other neutrophil elastase inhibitors, and are therefore more vulnerable to neutrophil-mediated injury.
Augmentation of human elafin has consistently demonstrated impressive protective effects in rodent models of ischaemic and inflammatory elastase-mediated vascular injury. Elafin infusion reduced muscular injury and neutrophil recruitment in the rat ischaemic hindlimb and myocardial ischaemia–reperfusion injury models.10 11 Transgenic mice overexpressing human elafin under the control of the vascular pre-proendothelin promoter have relatively preserved LV size and function following myocardial infarction.12 Compared with wild-type littermates, these animals are also protected from viral myocarditis and hypoxia-induced pulmonary hypertension and exhibit less restenosis following wire-induced carotid artery denudation.13–15 Elafin augmentation, therefore, protects the cardiovascular system from a range of conditions characterised by neutrophil elastase-mediated inflammation and injury.
The purpose of the Elafin Myocardial Protection from Ischemia Reperfusion (EMPIRE) randomised-controlled clinical trial was to provide proof of concept that Elafin treatment could reduce myocardial ischaemia-reperfusion inflammation and injury in patients undergoing CABG surgery.
Methods
Trial population
Between June 2011 and September 2013, consecutive patients referred for elective CABG surgery were recruited from two clinics at Edinburgh Heart Centre. Patients were 18 years or older, and were referred for isolated CABG surgery requiring two or more grafts. Exclusion criteria included patients with recent myocardial infarction (within 1 month of surgery), emergency or concomitant valve surgery, significant renal impairment (estimated glomerular filtration rate<40 mL/min), severe respiratory disease (maintenance corticosteroid therapy or forced expiratory volume in 1 s <50% predicted), severe LV impairment (EF <40%), contraindication to magnetic resonance scanning, treatment for chronic inflammatory disease, women of childbearing potential and inability to provide consent.
Study drug and randomisation
Intravenous recombinant human elafin (Proteo Biotech AG, Germany) 200 mg or saline placebo was prepared and infused as aqueous solution of 250 mL 0.9% saline. Patients were randomised (1:1) to receive elafin or matched placebo by Edinburgh Clinical Trials Unit to ensure allocation concealment. Randomisation incorporated minimisation for age, presence of diabetes mellitus, extent of coronary artery disease, renal function and surgeon A or B. To ensure blinding, study drugs were prepared by staff independent of the study investigators or clinical team responsible for the patient’s care.
Intravenous elafin 200 mg causes complete inhibition of plasma elastase activity for 2 h and >50% inhibition for 6 h. This dosage regimen was selected to cover the increased elastase release following CABG surgery that peaks at the time of weaning from cardiopulmonary bypass and has returned to baseline by 6–7 h. The study drug was administered to the patient through a central venous cannula over a period of 30 min. The intravenous infusion was started at first skin incision and completed at least 20 min before cardiopulmonary bypass commenced.
Anaesthesia and coronary artery bypass surgery
General anaesthesia was maintained with isoflurane and propofol infusion during bypass. Surgical approach was via a median sternotomy and cardiopulmonary bypass was started after heparin administration with a non-pulsatile flow and a membrane oxygenator. Cardioprotection was provided by cold blood cardioplegia (1:4), which was administered antegradely, after cross-clamping the aorta, into the coronary arteries or by cross-clamp fibrillation.
Blood samples
Blood samples were taken at baseline (time 0, skin incision) and at 2, 6, 24 and 48 h postoperatively. Plasma cardiac troponin I (cTnI) concentrations were measured with the ARCHITECTSTAT troponin I assay and ARCHITECTSTAT high-sensitive troponin I assay (Abbott Laboratories, Abbott Park, Illinois, USA) validated in our institution.16 17 Plasma concentrations of high-sensitive C reactive protein, IL-6, IL-8, myeloperoxidase and elastase were quantified using ELISAs (R&D Systems, UK; Elastase ELISA, Cambridge Biosciences, UK). Plasma elastase activity and serum elafin concentrations were measured by the Department of Dermatology, University of Kiel, Germany.
Cardiac MRI and analysis
Each patient underwent cardiac MRI twice: within 6 weeks before surgery and from 5 days after surgery. Patients were scanned using a research-dedicated 3T Siemens Verio scanner (Siemens Medical, Germany). Quantification of LV mass, EF and late gadolinium enhancement infarct size were determined using established protocols and dedicated cardiac analysis software by two trained independent blinded observers.
Statistical analysis
The primary outcome variable was the 48 h area under the curve (AUC) for plasma cTnI concentration. It was analysed using a generalised linear model, including terms for the treatment allocation and the variables on which the randomisation was minimised. Log transformations were applied as the data were skewed, and the results have been unlogged and presented as geometric means. Secondary outcome measures involving the AUC (hs-CRP, IL-6, IL-8, myeloperoxidase and elastase) were analysed similarly, taking log transformation if the data were skewed. LVEF and mass were analysed using QMass software (Medis Medical Imaging Systems, the Netherlands). The change in volume of infarction from preoperative and first postoperative magnetic resonance scans was categorised as increased, no change or reduced according to detection threshold based on interobserver variability. Post hoc analyses of individual time points used Wilcoxon tests.
The primary analysis included all randomised patients on an intention-to-treat basis regardless of compliance with allocated treatment and post-randomisation events. A secondary pre-specified exploratory analysis of AUC cTnI release excluded patients who had myocardial infarction or a cardiac arrest, resulting in loss of cardiac output for >1 min. Type V myocardial infarction was defined according to the third universal definition.18 Finally, post hoc, we examined treatment effect for each time point using the high-sensitive cTnI assay.
Power calculations were based on a recent study of patients undergoing remote ischaemic preconditioning before coronary artery bypass surgery.5 Mean cardiac troponin T release quantified as AUC was 36.12 µg/L (SD 26.08) and 20.58 µg/L (SD 9.58) in the control and treated patients, respectively. No contemporary AUC data were available for cTnI release in this patient group, but the measurements are equivalent in terms of quantifying myocardial injury. With a sample size of 80 patients, we had 90% power to detect this 40% difference in AUC cTnI with a significance level of 5%, using a t test with unequal variances and allowing for four dropouts in each arm.
Results
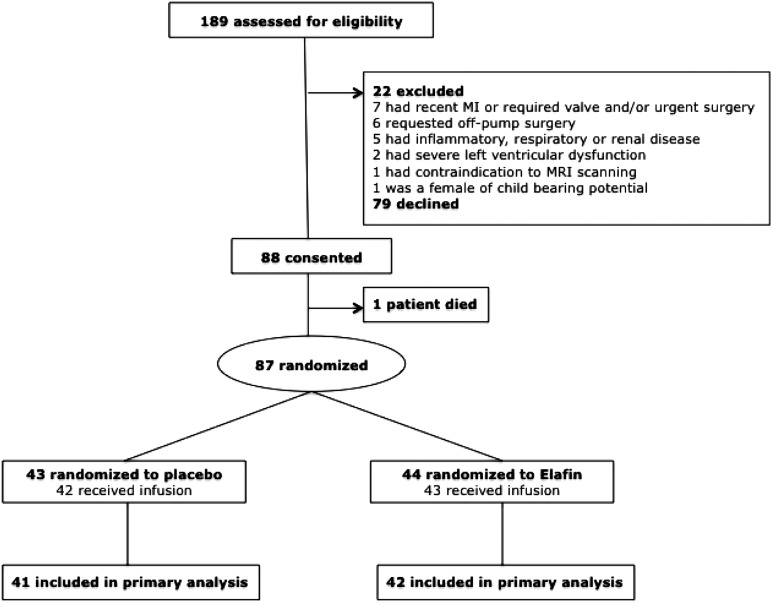
A participant flow diagram is shown in figure 1. In 85 of the 87 patients, the trial infusion was administered as planned. Patient characteristics and intraoperative details are shown in table 1. Full data to calculate the AUC for cTnI (primary outcome) were obtained in 83 patients (95%). Data quality was similarly good for all secondary end points with missing data evenly balanced across the treatment arms.
Figure 1.
Trial flow diagram.
Table 1.
Baseline characteristics and intraoperative details by treatment group
| Baseline characteristics | Placebo | Elafin |
|---|---|---|
| Age | 63.6±8.4 | 63.9±7.7 |
| Two-vessel coronary disease | 12(27.9) | 11(25.0) |
| Three-vessel coronary disease | 31(72.1) | 33(75.0) |
| Creatinine (mg/dL) | 0.92±0.18 | 0.94±0.23 |
| Diabetes mellitus | 9 (20.9) | 11 (25.0) |
| Surgeon A | 16 (37.2) | 18 (40.9) |
| Surgeon B | 27 (62.8) | 26 (59.1) |
| Male gender | 36 (83.7) | 38 (86.4) |
| EuroSCORE | 2.21±1.73 | 2.64±2.06 |
| Intraoperative details | ||
| Number of bypass grafts | ||
| One | 1 | 2 |
| Two | 19 | 14 |
| Three | 14 | 22 |
| Four | 9 | 5 |
| Five | 0 | 1 |
| Cardiopulmonary bypass time (min) | 77±26 | 78±26 |
| Cross clamp time (min) | 45±15 | 47±16 |
Data are number of patients (%) or mean±SD.
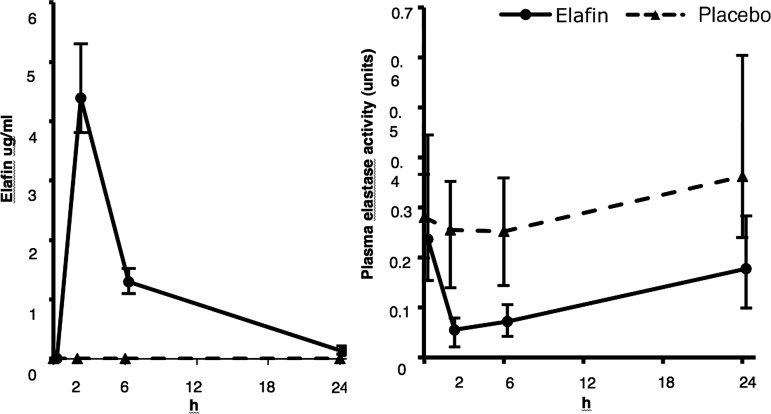
Elafin infusion resulted in >3000-fold higher plasma concentrations (mean AUC at 24 h; 31.1±9.6 vs 0.01±0.07 μg/mL for placebo) that was associated with a marked reduction in plasma elastase activity (mean AUC at 24 h; 4.28±5.13 vs 9.66±9.21 units/mL; figure 2).
Figure 2.
Perioperative plasma elafin concentration (left) and plasma elastase activity (right) between groups. Data are median plus IQR from the first skin incision (time 0 h) to 24 h. Placebo group n=41; elafin group, n=43.
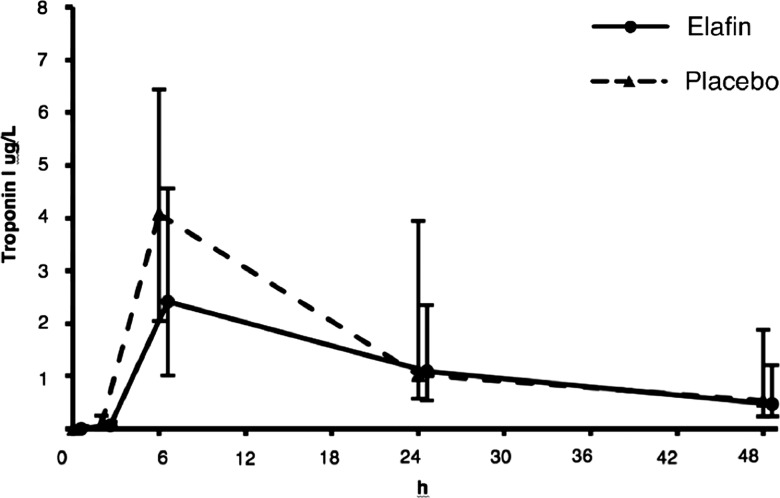
There was no change in mean AUC troponin concentrations over the first 48 h in Elafin-treated patients (adjusted ratio of geometric means (elafin/placebo) 0.74, 95% CI 0.47 to 1.15, p=0.18; figure 3). There remained no evidence of a difference in a pre-specified secondary analysis where three patients who sustained a clinical myocardial infarction or had a cardiac arrest were excluded from analysis. Post hoc analysis using the high-sensitive assay demonstrated a reduction of plasma cTnI concentrations in elafin-treated patients at 6 h (median 2.4 vs placebo 4.1 μg/L, p=0.035; table 2).
Figure 3.
Myocardial injury. Cardiac troponin I release following coronary artery bypass graft surgery between treatment groups from first skin incision (time 0 h) to 48 h. Data are median plus IQR. Placebo group, n=42; elafin group, n=44.
Table 2.
Post hoc analysis of plasma cardiac troponin I concentration (μg/L, median and IQR, high-sensitive assay) to 48 h
| Time (h) | Placebo (n=43) | Elafin (n=44) | p Wilcoxon |
|---|---|---|---|
| 0 | 0.00 (0.0–0.0) | 0.00 (0.0–0.0) | 0.861 |
| 2 | 0.08 (0.0–0.2) | 0.07 (0.0–0.1) | 0.228 |
| 6 | 4.07 (2.0–6.4) | 2.41 (1.0–4.6) | 0.035 |
| 24 | 1.02 (0.6–3.9) | 1.08 (0.5–2.3) | 0.421 |
| 48 | 0.53 (0.2–1.9) | 0.47 (0.2–1.2) | 0.648 |
Data from preoperative and postoperative scans were available for 34 (77.3%) elafin-treated and 35 (81.4%) placebo-treated patients (table 3). There was no difference in postoperative LV mass. The intra-class correlation coefficient for late gadolinium enhancement was 0.99 and the coefficient of repeatability of 1.78 mL (1.87 g) giving a threshold of 1.8 mL (1.9 g) for an increase in late gadolinium enhancement. Using this threshold, the incidence of increased myocardial infarction volume was 20.3% in elafin-treated and 14.3% in placebo-treated patients.
Table 3.
MRI analysis of postoperative EF, LV mass and infarct volume
| Placebo (n=35) | Elafin (n=34) | |
|---|---|---|
| Change in EF (%) | −0.62±6.2 | −2.4±6.3 |
| Change in LV mass (g) | 1.2±3.8 | 2.0±3.8 |
| Change in infarct volume (%) | ||
| Reduced volume | 2.9 | 0 |
| No change | 82.9 | 79.4 |
| Increased volume | 14.3 | 20.6 |
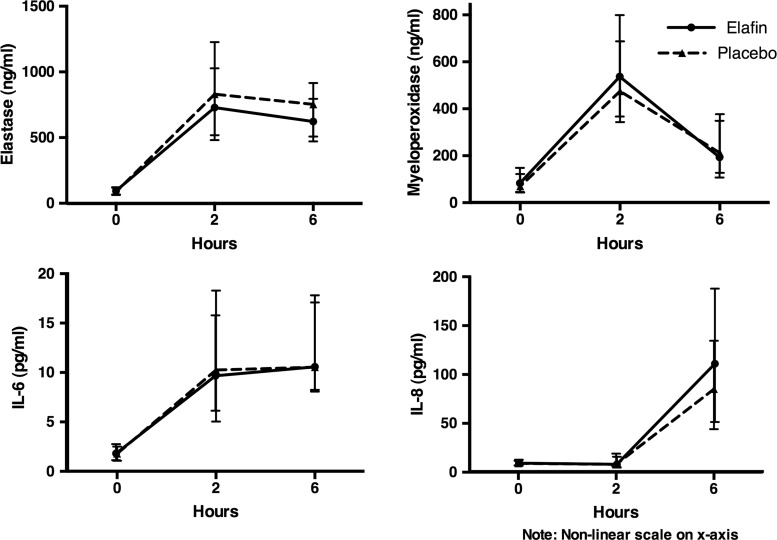
There was no effect on peak myeloperoxidase concentrations (mean difference 54.73 ng/L, 95% CI −60.0 to 169.5, p=0.35) but peak elastase concentration was reduced (mean difference −168.4 ng/mL, 95% CI −323.4 to −13.47, p=0.03; figure 4). In contrast, there was no effect on the 6 h AUC for plasma elastase concentration (mean difference –524.0 ng/mL/48 h, 95% CI −1239 to 191.3, p=0.15). Although hs-CRP, IL-6 and IL-8 concentrations rose following CABG surgery (p<0.001 for all), there was no treatment effect of elafin (mean differences for 48 h AUC hs-CRP of 499 mg/L/48 h, 95% CI −207 to 1205, p=0.16) and p>0.05 for both IL-6 and IL-8; figure 4.
Figure 4.
Perioperative circulating concentrations of neutrophil granule proteins elastase (top left), myeloperoxidase (top right), inflammatory cytokines interleukin (IL)-6 (bottom left) and IL-8 (bottom right) between treatment groups out to 6 h. Data are median plus IQR. Placebo group, n=42; elafin group, n=44.
Median duration of stay in the intensive care unit was 24 and 23 h for patients treated with elafin and placebo, respectively (HR 1.25, 95% CI 0.81 to 1.94, p=0.32). Clinical outcomes and the incidence of perioperative complications in the first 48 h were also similar (table 4).
Table 4.
Postoperative complications and outcomes by treatment
| Placebo | Elafin | |||
|---|---|---|---|---|
| Postoperative complications and outcomes (48 h) | ||||
| Death | 0 | (0) | 0 | (0) |
| Stroke | 0 | (0) | 0 | (0) |
| Myocardial infarction | 0 | (0) | 1 | (2.3) |
| Inotrope or balloon pump support for >24 h | 10 | (27.3) | 12 | (23.3) |
| Red cell transfusion postoperative | 12 | (27.9) | 12 | (27.3) |
| Reoperation for bleeding | 2 | (4.7) | 1 | (2.3) |
| Respiratory complications | 3 | (7.0) | 5 | (11.4) |
| Antibiotic administration | 2 | (4.7) | 4 | (9.1) |
| Atrial fibrillation | 4 | (9.3) | 3 | (6.8) |
| Serum creatinine (mg/dL) | ||||
| 24 h | 0.90±0.32 | 0.87±0.32 | ||
| 48 h | 0.96±0.48 | 0.88±0.42 | ||
Data are number of patients (%) or mean±SD.
Discussion
This is the first phase II clinical trial investigating the effect of elafin, an endogenous neutrophil elastase inhibitor, on myocardial ischaemia-reperfusion injury in patients undergoing CABG surgery. Despite achieving >3000-fold increase in plasma concentrations sufficient to more than halve plasma elastase activity, we did not demonstrate clear evidence of beneficial effect of human recombinant elafin in our patients. Specifically, we were unable to attenuate the systemic inflammatory response despite evidence of anti-inflammatory activity in preclinical disease models.19 Nor could we conclusively detect a reduction in two very sensitive, complementary and gold standard measures of myocardial injury: AUC for plasma cTnI concentrations and late gadolinium enhancement on MRI despite preclinical studies with elafin reducing myocardial inflammation and injury after myocardial infarction.11 12 Differences between preclinical studies and the clinical CABG surgery model may have been responsible for different results. Elafin has never been tested in large animal models or in the setting of cardiopulmonary bypass surgery. The surgical population was relatively low risk, and the use of isoflurane anaesthesia may provide cardioprotection.20 Nevertheless, ischaemia-reperfusion injury in CABG surgery produced conditions where elafin would be expected to exert a treatment effect: neutrophil activation, elastase release and heightened circulating elastase activity together with activation of inflammatory cytokine pathways.
Elafin was safe and well tolerated in this high-risk clinical setting and post hoc analysis indicated reduced myocardial injury at 6 h, raising the possibility that more extensive treatment effect could have been seen with multiple doses or bolus and sustained infusions.
All patients in our trial exhibited evidence of myocardial injury demonstrated by cTnI release. This was associated with a marginal reduction in LVEF detected on postoperative MRI. Small increases in delayed gadolinium enhancement indicative of new myocardial infarction were detected in a fifth of patients in keeping with subclinical myocardial injury and infarction that follows circulatory arrest and ischaemia-reperfusion during CABG surgery. The current MRI results contrast with an earlier study reporting increased infarct volume in 78% of patients undergoing planned CABG.21 A key difference that may explain this discrepancy is the detailed patient characterisation in our study with availability of preoperative MRI scans allowing identification of small areas of pre-existing infarct that would be missed by using clinical history, echocardiography or ECGs to screen for pre-existing infarction.
Our data indicate that with single bolus administration elafin does not confer myocardial protection in the first 48 h following CABG surgery. This result was unchanged in a secondary analysis excluding patients who had sustained clinical events thought to be unrelated to study drug that would have contributed to large additional cTnI elevations. The absence of a convincing beneficial effect conflicts with preclinical ischaemia-reperfusion studies where elafin infusion was associated with a 27% reduction in myocardial infarct size and improved LV performance. Our clinical CABG model allows recapitulation of a key condition in preclinical models where elafin is administered upfront or expressed in tissues prior to the onset of cardiopulmonary bypass and ischaemic tissue injury. However, despite this, we were unable to demonstrate clear efficacy using two complementary and highly sensitive measures of myocardial injury. Post hoc analysis identified a reduction in plasma cTnI concentrations at 6 h in elafin-treated patients. Preclinical studies used continuous elafin delivery by infusion or gene expression and the reduced cTnI concentration at an early postoperative time point raises the question whether continuous elafin infusion following the bolus may have extended the treatment effect to 48 h.
Elafin is one of several agents targeting inflammatory pathways that have been investigated in ischaemia-reperfusion injury during cardiac surgery without success. Pexelizumab, a recombinant, single-chain anti-C5 monoclonal antibody, was studied in two multicentre, randomised clinical trials of patients undergoing CABG surgery with or without valve surgery on cardiopulmonary bypass. There was no difference in the primary outcome of death or myocardial infarction between the pexelizumab and placebo treatment groups.22 Failure of treatment effect with elafin and pexelizumab may reflect different mechanisms responsible for myocardial injury during CABG. Myocardial ischaemia and necrosis undoubtedly occur during CABG surgery, and the magnitude of cTnI release is correlated with subsequent morbidity and mortality.23 Mechanism of ischaemia in preclinical models commonly involves complete interruption of coronary blood flow with a ligature to the beating heart. In CABG surgery, the heart is in a state of circulatory arrest with protective cardioplegia and the impact of blood flow interruption is less severe. Despite evidence of neutrophil-mediated inflammatory injury post-CABG, it may be activation of cellular survival pathways within cardiomyocytes that determines the outcome of ischaemia-reperfusion in this setting. Ischaemic preconditioning refers to resistance to acute myocardial ischaemia reperfusion conferred by the application of brief repeated episodes of ischaemia. This approach has been used successfully in CABG surgery to limit cardiac marker release.5 We demonstrated substantial (>50%) inhibition of circulating elastase activity by elafin following CABG surgery, and our data therefore indicate that neutrophil-derived elastase injury is not a prominent cause of myocardial injury in this setting.
The patients in our study did have evidence of neutrophil activation and degranulation with increased plasma concentrations of the primary granule contents, elastase and myeloperoxidase. Peak elastase concentrations were reduced in elafin-treated patients, although there was no demonstrable effect on peak myeloperoxidase concentrations. This discrepancy is explained by differences in the origin of these two neutrophil primary granule proteins. Circulating human neutrophil elastase is derived largely from acute neutrophil degranulation. A pool of neutrophil-derived myeloperoxidase is transcytosed and bound to the subendothelial matrix.24 This contributes to the circulating pool and is released following heparin administration during cardiopulmonary bypass.25
Elafin-mediated reductions in elastolytic activity and myeloperoxidase staining (as a marker of neutrophil infiltration) have been consistent findings in preclinical models. Elafin infusion produced impressive reductions in myocardial inflammation and necrosis in rabbits undergoing heterotopic cardiac transplantation.26 This was associated with a marked attenuation of myocardial elastolytic activity in transplanted hearts. Transgenic mice overexpressing full-length human elafin under the control of the vascular pre-proendothelin promoter exhibit complete inhibition of tissue elastolytic activity following acute myocardial infarction and carotid arterial wire denudation.12 15 These favourable treatment effects consistently occurred with reduced tissue myeloperoxidase content in keeping with less neutrophil recruitment. We were not able to access myocardial tissue for assessment of neutrophil infiltration and elastolytic activity, but the significant reduction in peak elastase concentration leaves open the possibility of an elafin effect on neutrophil activation and degranulation, which, if present, was not large enough to translate into a reduction in AUC elastase at 6 h.
The EMPIRE patients exhibited increased IL-8 and IL-6 production and increased levels of circulating hs-CRP in keeping with a postischaemic inflammatory response following CABG surgery. A systemic inflammatory response follows CABG surgery driven both by major surgical insult and contact activation of blood with artificial surfaces of the extracorporeal circuit.27 Belief that the magnitude of this response may drive clinical outcome has led to trials examining interventions to reduce postoperative inflammation. Peak and AUC hs-CRP, IL-6 and IL-8 release were similar between treatment groups. This result for elafin contrasts with previous work indicating broad-ranging anti-inflammatory activity in human endothelial cells and monocyte-derived macrophages.8 The failure of elafin to suppress IL-8 production during CABG surgery may indicate that additional inflammatory pathways are active or that despite impacting on circulating elastase activity elafin is not reaching or is not active in the subcellular space between neutrophils and their target tissue.
Given lack of a conclusive therapeutic effect on myocardial injury and postischaemic inflammation, it is not surprising that the exploratory clinical end point of postoperative ITU stay was no different between treatment groups. Elafin infusion was safe. There were no drug-related adverse events in this high-risk surgical group and no evidence of excessive bleeding, cardiovascular complications or renal dysfunction.
In conclusion, despite the body of work indicating therapeutic potential from several groups using different models, species and modes of augmentation, elafin's promise as a therapeutic agent to attenuate myocardial ischaemia-reperfusion injury and inflammation was not translated in this first phase II clinical trial. Post hoc analysis identified reduced cTnI concentrations at 6 h in elafin-treated patients, and it is possible that a bigger dose could have conferred protection out to 48 h. Elafin was safe and lack of treatment effect was seen despite achieving high plasma elafin concentrations and halving of circulating elastase activity.
Key messages.
What is already known on this subject?
Ischaemia-reperfusion contributes to myocardial injury during cardiac surgery. Therapies to reduce injury remain elusive despite promise from preclinical studies. Elafin is an endogenous neutrophil elastase inhibitor with broad-ranging anti-inflammatory activity. Elafin reduces myocardial injury and infarct size and is associated with better myocardial function in preclinical models of ischaemia-reperfusion injury.
What might this study add?
We investigated elafin in myocardial ischaemia-reperfusion injury induced during coronary artery bypass graft surgery. A single dose of elafin was safe and reduced circulating elastase activity but did not attenuate ischaemia-reperfusion injury or postoperative inflammation following coronary artery bypass surgery.
How might this impact on clinical practice?
Elafin's promise as a therapeutic agent was not translated in this first phase II clinical trial. Post hoc analysis revealed reduced myocardial injury at an early time point in elafin-treated patients. Further studies with continuous infusion and alternative clinical models are needed to elucidate whether elafin can confer protection form ischaemia-reperfusion injury.
Footnotes
Contributors: SA, DEN and PAH: substantial contributions to the conception or design of the work, or the acquisition, analysis or interpretation of data; drafting the work or revising it critically for important intellectual content; final approval of the version published and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. SCL, AK, KG, KO, RH, NMM and CM: drafting the work or revising it critically for important intellectual content and final approval of the version published. VZ, RP, MRD, LM, ST, SS, OW, CS and SM: substantial contributions to the conception or design of the work, or the acquisition, analysis or interpretation of data; drafting the work or revising it critically for important intellectual content and final approval of the version published.
Funding: Medical Research Council (UK) Developmental Clinical Studies grant G1001339 and Chest Heart and Stroke Scotland (UK) grant R11/A135. DEN is funded by the British Heart Foundation (CH/09/002). Proteo Biotech AG supported the study by supplying the elafin required free of charge. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. The content of this manuscript is solely the responsibility of the authors.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: This single-centre clinical trial was performed with the approval of the national research ethics committee (11/MRE00/5), in accordance with the Declaration of Helsinki (2000), under a Clinical Trial Authorisation (27586/0015/001-0001) from the Medicine and Healthcare products Regulatory Authority (MHRA, UK).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hansen PR. Role of neutrophils in myocardial ischemia and reperfusion. Circulation 1995;91:1872 10.1161/01.CIR.91.6.1872 [DOI] [PubMed] [Google Scholar]
- 2.Vinten-Johansen J. Involvement of neutrophils in the pathogenesis of lethal myocardial reperfusion injury. Cardiovasc Res 2004;61:481–97. 10.1016/j.cardiores.2003.10.011 [DOI] [PubMed] [Google Scholar]
- 3.Butler J, Parker D, Pillai R, et al. . Effect of cardiopulmonary bypass on systemic release of neutrophil elastase and tumor necrosis factor. J Thorac Cardiovasc Surg 1993;105:25–30. [PubMed] [Google Scholar]
- 4.Wakayama F, Fukuda I, Suzuki Y, et al. . Neutrophil elastase inhibitor, sivelestat, attenuates acute lung injury after cardiopulmonary bypass in the rabbit endotoxemia model. Ann Thorac Surg 2007;83:153–60. 10.1016/j.athoracsur.2006.08.023 [DOI] [PubMed] [Google Scholar]
- 5.Hausenloy DJ, Mwamure PK, Venugopal V, et al. . Effect of remote ischaemic preconditioning on myocardial injury in patients undergoing coronary artery bypass graft surgery: a randomised controlled trial. Lancet 2007;370:575–9. 10.1016/S0140-6736(07)61296-3 [DOI] [PubMed] [Google Scholar]
- 6.Sallenave JM, Ryle AP. Purification and characterization of elastase-specific inhibitor. Sequence homology with mucus proteinase inhibitor. Biol Chem Hoppe Seyler 1991;372:13–21. 10.1515/bchm3.1991.372.1.13 [DOI] [PubMed] [Google Scholar]
- 7.Wiedow O, Luademann J, Utecht B. Elafin is a potent inhibitor of proteinase 3. Biochem Biophys Res Commun 1991;174:6–10. 10.1016/0006-291X(91)90476-N [DOI] [PubMed] [Google Scholar]
- 8.Henriksen PA, Hitt M, Xing Z, et al. . Adenoviral gene delivery of elafin and secretory leukocyte protease inhibitor attenuates NF- B-dependent inflammatory responses of human endothelial cells and macrophages to atherogenic stimuli. J Immunol 2004;172:4535 10.4049/jimmunol.172.7.4535 [DOI] [PubMed] [Google Scholar]
- 9.Sallenave JM. The role of secretory leukocyte proteinase inhibitor and elafin (elastase-specific inhibitor/skin-derived antileukoprotease) as alarm antiproteinases in inflammatory lung disease. Respir Res 2000;1:87–92. 10.1186/rr18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crinnion J, Homer-Vanniasinkam S, Hatton R, et al. . Role of neutrophil depletion and elastase inhibition in modifying skeletal muscle reperfusion injury. Cardiovasc Surg 1994;2:749. [PubMed] [Google Scholar]
- 11.Tiefenbacher CP, Ebert M, Niroomand F, et al. . Inhibition of elastase improves myocardial function after repetitive ischaemia and myocardial infarction in the rat heart. Pflugers Arch 1997;433:563–70. 10.1007/s004240050315 [DOI] [PubMed] [Google Scholar]
- 12.Ohta K, Nakajima T, Cheah AY, et al. . Elafin-overexpressing mice have improved cardiac function after myocardial infarction. Am J Physiol Heart Circ Physiol 2004;287:H286–92. 10.1152/ajpheart.00479.2002 [DOI] [PubMed] [Google Scholar]
- 13.Zaidi SH, Hui CC, Cheah AY, et al. . Targeted overexpression of elafin protects mice against cardiac dysfunction and mortality following viral myocarditis. J Clin Invest 1999;103:1211–19. 10.1172/JCI5099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zaidi SH, You XM, Ciura S, et al. . Overexpression of the serine elastase inhibitor elafin protects transgenic mice from hypoxic pulmonary hypertension. Circulation 2002;105:516–21. 10.1161/hc0402.102866 [DOI] [PubMed] [Google Scholar]
- 15.Zaidi SH, You XM, Ciura S, et al. . Suppressed smooth muscle proliferation and inflammatory cell invasion after arterial injury in elafin-overexpressing mice. J Clin Invest 2000;105:1687–95. 10.1172/JCI9147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mills NL, Churchhouse AM, Lee KK, et al. . Implementation of a sensitive troponin I assay and risk of recurrent myocardial infarction and death in patients with suspected acute coronary syndrome. JAMA 2011;305:1210–16. 10.1001/jama.2011.338 [DOI] [PubMed] [Google Scholar]
- 17.Mills NL, Lee KK, McAllister DA, et al. . Implications of lowering threshold of plasma troponin concentration in diagnosis of myocardial infarction: cohort study. BMJ 2012;344:e1533 10.1136/bmj.e1533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thygesen K, Alpert JS, Jaffe AS, et al. . Third universal definition of myocardial infarction. J Am Coll Cardiol 2012;60:1581–98. 10.1016/j.jacc.2012.08.001 [DOI] [PubMed] [Google Scholar]
- 19.Alam SR, Newby DE, Henriksen PA. Role of the endogenous elastase inhibitor, elafin, in cardiovascular injury: from epithelium to endothelium. Biochem Pharmacol 2012;83:695–704. 10.1016/j.bcp.2011.11.003 [DOI] [PubMed] [Google Scholar]
- 20.Kersten JR, Schmeling TJ, Pagel PS, et al. . Isoflurane mimics ischemic preconditioning via activation of K(ATP) channels: reduction of myocardial infarct size with an acute memory phase. Anesthesiology 1997;87:361–70. 10.1097/00000542-199708000-00024 [DOI] [PubMed] [Google Scholar]
- 21.Steuer J, Bjerner T, Duvernoy O, et al. . Visualisation and quantification of peri-operative myocardial infarction after coronary artery bypass surgery with contrast-enhanced magnetic resonance imaging. Eur Heart J 2004;25:1293–9. 10.1016/j.ehj.2004.05.015 [DOI] [PubMed] [Google Scholar]
- 22.Verrier ED, Shernan SK, Taylor KM, et al. . Terminal complement blockade with pexelizumab during coronary artery bypass graft surgery requiring cardiopulmonary bypass: a randomized trial. JAMA 2004;291:2319–27. 10.1001/jama.291.19.2319 [DOI] [PubMed] [Google Scholar]
- 23.Croal BL, Hillis GS, Gibson PH, et al. . Relationship between postoperative cardiac troponin I levels and outcome of cardiac surgery. Circulation 2006;114:1468–75. 10.1161/CIRCULATIONAHA.105.602370 [DOI] [PubMed] [Google Scholar]
- 24.Baldus S, Eiserich JP, Mani A, et al. . Endothelial transcytosis of myeloperoxidase confers specificity to vascular ECM proteins as targets of tyrosine nitration. J Clin Invest 2001;108:1759–70. 10.1172/JCI200112617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rudolph TK, Schaper N, Klinke A, et al. . Liberation of vessel-adherent myeloperoxidase reflects plaque burden in patients with stable coronary artery disease. Atherosclerosis 2013;231:354–8. 10.1016/j.atherosclerosis.2013.09.016 [DOI] [PubMed] [Google Scholar]
- 26.Cowan B, Baron O, Crack J, et al. . Elafin, a serine elastase inhibitor, attenuates post-cardiac transplant coronary arteriopathy and reduces myocardial necrosis in rabbits afer heterotopic cardiac transplantation. J Clin Invest 1996;97:2452–68. 10.1172/JCI118692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Day JR, Taylor KM. The systemic inflammatory response syndrome and cardiopulmonary bypass. Int J Surg 2005;3:129–40. 10.1016/j.ijsu.2005.04.002 [DOI] [PubMed] [Google Scholar]