Abstract
Background:
To date, few results on well-being in individuals with neurological disease have been published, while several studies in other groups have indicated that well-being may not be the only absence of psychological distress, but also positive psychological function. The aim of the present study was to compare the psychological well-being (PWB) between the people with Multiple sclerosis (MS) and normal individuals and identify correlated demographic factors to PWB in people with MS disorder.
Materials and Methods:
A case-control study was performed in July 2012 on 55 people with MS who were referred to MS clinic (located at the Kashani Hospital), Isfahan Neurosciences Research Centre and 83 normal individuals with matched mean of age, level of education, and gender. The participants filled up the 18-item Ryff's PWB and demographic profile. The data were analyzed by SPSS software based on the independent t-test, and ANOVA.
Results:
There is significant different in all PWB dimensions between people with MS and normal groups. There were no significant differences in PWB in people with MS in relation to gender and marital status, but individuals with higher level of education scored higher in total PWB, positive relationship with others and purpose in life.
Conclusion:
People with MS are at risk of lower level of PWB. Interventional programs for improving PWB are strongly recommended.
Keywords: Multiple Sclerosis, psychological well-being, quality of life
INTRODUCTION
Multiple sclerosis (MS) is an immune-mediated, neurodegenerative disease that affects an estimated 2.5 million adults worldwide.[1] In Isfahan/Iran, an increase in prevalence and incidence figures (73.3; 9.1: 2004-2005 vs. 43.8; 3.64: 2003-2010/1,00,000) was reported.[2,3] MS typically has its onset in early adulthood, and affects more women than men. Although rarely fatal, MS produces a range of unpleasant and disabling symptoms. The course of MS is idiosyncratic and unpredictable. This disease manifests in a wide range of symptoms including muscle weakness, extreme fatigue, imbalance, visual, speech disturbances, and cognitive impairment. Such symptoms often lead to poor health-related quality of life (HRQOL),[3,4,5] neurologic disability, and high health care costs.[7]
MS poses multiple challenges for both physical and psychological well-being (PWB) people with MS experience unpleasant and unpredictable symptoms, difficult treatment regimes, and drug side effects, and increasing levels of physical disability. They also face psychosocial consequences including disruptions to life goals, employment, income, relationships, leisure activities, and daily living activities. Psychological difficulties are extremely common in MS compared to both healthy populations and other chronic diseases. The empirical literature attests to elevated rates of depression and distress,[8] increased anxiety,[9] low subjective well-being, quality of life (QOL),[8,10] social role and relationship difficulties.[11] Nonetheless, a substantial proportion of people with MS manage to adapt well to living with the illness.[12] Illness factors such as the extent of neurological disability, symptom severity, remission status, and length of illness can influence levels of psychological adjustment in MS.[13] However, these factors are inconsistently associated with adjustment, and are often only modest predictors.[14] Research demonstrates that psychological factors are often better predictors of individual differences in adjustment than illness factors.[15] Psychological factors, unlike illness factors, are potentially modifiable through psychological interventions. Studies on emotional distress and HRQOL broadened the traditional biomedical focus in MS research, but little attention was paid to total well-being indicators. Although research on these topics has broadened the traditional biomedical focus to include subjective evaluations of living conditions, the limitations of such approach are increasingly evident. First, in MS literature QOL is substantially related to health issues, while other relevant life domains are neglected.[16] Second, research and intervention primarily target physical and emotional symptoms, namely the negative aspects of illness. Such focus implicitly equates health with the absence or reduction of disease/infirmity, and not with a state of complete physical, mental, and social well-being, as defined by the WHO. In this respect, psychologists recently called for a shift in attention from human shortcomings and deficits to personal resources and potentials, showing through empirical studies that well-being is not the opposite of ill-being; rather, it comprises unique dimensions.[17,18] Well-being studies refer to two conceptual approaches. The hedonic one focuses on emotions and operationalizes well-being as life satisfaction and prevalence of positive over negative affect (hedonic balance).[19] The eudaimonic approach focuses on meaning-making and goal pursuit.[20,21] One of the eudaimonic constructs is PWB, purport by Ryff[22] that well-being is a multi-dimensional construct made up of life attitudes necessary for positive functioning. This conception of QOL has been termed by Ryff as “PWB” and has received extensive empirical support.[22,23,24,25] Ryff[22] suggests a model representative of six dimensions of well-being:
Self-acceptance (SA); the ability to feel good about oneself while being aware of one's limitations,
Environmental mastery (EM); the attempt to shape one's environment to meet personal needs and wishes,
Positive relations with others (PR); having affirming relationships with others,
Personal growth (PG); making the most of one's capability and skills,
Purpose in life (PL); ability to find meaning in one's struggles or hardships, and
Autonomy (A); seeking a sense of personal authority and independence.
The experience of having MS has the potential to impact seriously each one of these aspects of well-being, but little research has examined these constructs in MS population. Research has shown that conditions such as chronic disease are not necessarily perceived as stressful threats.[20] They can also be interpreted as challenges and opportunities for growth, thus not hampering well-being, especially its eudaimonic components such as meaning-making, interpersonal relations, and engagement in daily activities.[23] Accordingly, in the few studies targeting hedonic well-being in MS research, people with MS were more dissatisfied with their lives than healthy individuals.[24,25] As for eudaimonic well-being, only a few studies were carried out: It showed that people with MS and healthy controls reported similar levels of PG.[26] Well-being (both hedonic and eudaimonic aspects) decreased with a higher disability. Psychological distress was moderately related to eudemonic well-being.[27] Hart et al. found that treating depression was significantly associated with improvements in 4 of the 6 scales of PWB included EM, positive relations, PL, and self acceptance.[28] Because there is no published research on PWB in the Iranian population, we decided to examine PWB in people with MS in comparing to normal individuals. The aims of the present study were to compare PWB in people with MS with normal people in Isfahan, Iran, and to determine whether there are relationships between demographic variables and PWB in MS population.
MATERIALS AND METHODS
Fifty-five male and female people with MS and 83 people with no neurological diseases aged 18-60 years were included in this case-control study, which was conducted in July 2012. The people with MS randomly were selected from MS clinic (Kashani Hospital, Isfahan Neurosciences Research Centre). Sample selection was based on their agreement to participate in this study. Criteria for the participants with MS were:
Diagnosed by a neurologist based on systemic examination and laboratory findings such as magnetic resonance imaging and
No other neurological and psychiatric disorders. The normal sample also was selected through multistage sampling from 15 municipal zones in Isfahan.
18-item version of the PWB scales developed by Ryff[22] was used to assess PWB. Ryff's measure defines well-being as a composition of six different psychological constructs include A: Independence and self-determination, SA: Positive attitude towards oneself and one's past life, EM: the ability to manage one's life, PR: Having satisfying high quality relationships, PG: Being open to new experiences, PL: Believing that one's life is meaningful. The participants were asked to grade their agreement to the sentences in seven categories, from strong disagreement to a strong agreement. The responses were coded from 0 to 6 and summed across the three items of each dimension. Some items were reversed, and all items randomly distributed in an attempt to keep participants from seeing a pattern. The instrument, in this study showed varied internal consistency reliability for the six subscales:
A (Cronbach's α = 0.34),
EM (Cronbach's α = 0.56),
SA (Cronbach's α = 0.78),
PL (Cronbach's α = 0.42),
PG (Cronbach's α = 0.58), and
PR (Cronbach's α = 0.34).
A total psychological well-being (TPWB) score was calculated by adding all six constructs (Cronbach's α =.7). The same results seen in reported in other studies.[29] The data were analyzed by SPSS software (version 19.0; SPSS Inc., Chicago, IL, USA). T-test was performed to examine the differences in PWB scales in two normal and MS samples. ANOVAs were conducted to examine differences in PWB scales in MS group with regard to gender, married status, and level of education.
This study was approved by the local Ethics Committee and all patients in this study, and all subjects gave their written consent.
RESULTS
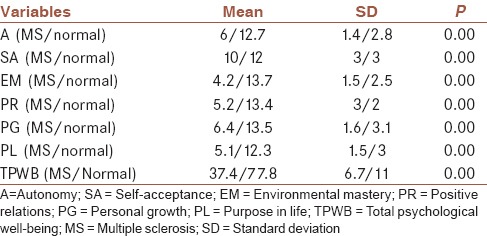
Demograghic characteristics of two samples are presented in Table 1. As shown in Table 2, people with MS reported lower level PWB in all subscales than the normal group.
Table 1.
Demographic characteristics of two samples
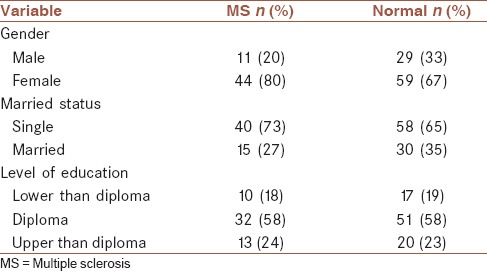
Table 2.
A comparison of the mean scores for the psychological well-being scales in patients with MS
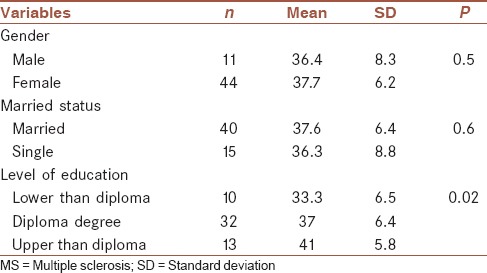
According to the Table 3 there is no significant difference in TPWB in people with MS regard to gender and married status, but individuals with a higher level of education reported higher TPWB. For exploring relationship between the level of education and PWB in details, ANOVAs were conducted for subscales of PWB. The results showed that patients with higher level of education reported a higher level of PR and PL.
Table 3.
Total psychological well-being regard to gender, married status and level of education in MS sample
DISCUSSION AND CONCLUSION
Our results indicate a reduction in all aspects of PWB of people with MS in comparison to the normal population and only the level of education has significantly positive relationship to PWB in MS group. Reduction in PWB compared with the general population had been seen in other studies.[10,24,25,26,27] The burden of living with MS affects patient's physical and mental health. Reduction in PWB could be attributed directly and indirectly to the symptoms and outcomes of MS disease. People with MS are faced with uncertainty about the future, unpleasant and unpredictable symptoms, difficult treatment regimes, and drug side effects. MS can have profound consequences, including disruption of life goals, employment, income, relationships, social, leisure activities, and activities of daily living. This may be particularly significant because, for the majority of people with MS, the disease begins in young adulthood, a period that is often important for career development and starting families. Therefore, it is not surprising that many patients experience many difficulties in PWB.[30] Individuals with low positive well-being were 7.16 times more likely to be depressed 10-years later.[31]
Research demonstrated elevated levels of depression[5] in people with MS. Thus interventional programs for promoting PWB could be a result to decrease depression. Historically the management of MS has been predominantly about limiting disability by the symptomatic management of acute relapses and attempting to influence the long-term course. Even though this type of management is important, we suggest this is accompanied by an equal effort at improving participation PWB. Because the previous studies showed that both physical and psychological aspects are important and interact with each other.[32]
It is necessary to continue the research on PWB in people with MS to evaluate the impact of factors such as the type of pharmacological treatment and rehabilitation.
Regarding the correlation between PWB and level of education, we believe that firstly it is assumed that MS symptoms are to be diagnosed sooner in people with higher education, thus treatment affairs sooner be started and consequence impairment in PWB would be minimized. In the other hand, there is more purpose for people with higher education especially who enter to universities in life, and they have a broader range of relationship options. The limitations of this study were the lack of a control group. The limitations of this study were the lack of a control group. Furthermore, patients who participated in this research in terms of disability were mild to moderate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
AUTHORS’ CONTRIBUTION
SRD contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work as first author. FH contributed in the conception of the work, conducting the study, Data analysis and agreed for all aspects of the work.FA contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.VSh contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. All authors have read and approved the content of the manuscript and are accountable for all aspects of the work.
Acknowledgments
The authors would like to thank all participants that paticipated in this study.
REFERENCES
- 1.National MS Society. Who Gets MS? [Last retrieved on 2008 May 20]. Available from: http://www.nationalmssocietyorg/about-multiple-sclerosis/who-getsms/index.aspx .
- 2.Etemadifar M, Janghorbani M, Shaygannejad V, Ashtari F. Prevalence of multiple sclerosis in Isfahan, Iran. Neuroepidemiology. 2006;27:39–44. doi: 10.1159/000094235. [DOI] [PubMed] [Google Scholar]
- 3.Etemadifar M, Maghzi AH. Sharp increase in the incidence and prevalence of multiple sclerosis in Isfahan, Iran. Mult Scler. 2011;17:1022–7. doi: 10.1177/1352458511401460. [DOI] [PubMed] [Google Scholar]
- 4.Campbell JD, Ghushchyan V, Brett McQueen R, Cahoon-Metzger S, Livingston T, Vollmer T, et al. Burden of multiple sclerosis on direct, indirect costs and quality of life: National US estimates. Mult Scler Relat Disord. 2014;3:227–36. doi: 10.1016/j.msard.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Benito-León J, Morales JM, Rivera-Navarro J, Mitchell A. A review about the impact of multiple sclerosis on health-related quality of life. Disabil Rehabil. 2003;25:1291–303. doi: 10.1080/09638280310001608591. [DOI] [PubMed] [Google Scholar]
- 6.Motl RW, McAuley E. Symptom cluster and quality of life: Preliminary evidence in multiple sclerosis. J Neurosci Nurs. 2010;42:212–6. doi: 10.1097/jnn.0b013e3181e26c5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Campbell JD, Ghushchyan V, Brett McQueen R, Cahoon-Metzger S, Livingston T, Vollmer T, et al. Burden of multiple sclerosis on direct, indirect costs and quality of life: National US estimates. Mult Scler Relat Disord. 2014;3:227–36. doi: 10.1016/j.msard.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Janssens AC, van Doorn PA, de Boer JB, van der Meché FG, Passchier J, Hintzen RQ. Impact of recently diagnosed multiple sclerosis on quality of life, anxiety, depression and distress of patients and partners. Acta Neurol Scand. 2003;108:389–95. doi: 10.1034/j.1600-0404.2003.00166.x. [DOI] [PubMed] [Google Scholar]
- 9.Zorzon M, de Masi R, Nasuelli D, Ukmar M, Mucelli RP, Cazzato G, et al. Depression and anxiety in multiple sclerosis. A clinical and MRI study in 95 subjects. J Neurol. 2001;248:416–21. doi: 10.1007/s004150170184. [DOI] [PubMed] [Google Scholar]
- 10.Benito-León J, Morales JM, Rivera-Navarro J, Mitchell A. A review about the impact of multiple sclerosis on health-related quality of life. Disabil Rehabil. 2003;25:1291–303. doi: 10.1080/09638280310001608591. [DOI] [PubMed] [Google Scholar]
- 11.Hakim EA, Bakheit AM, Bryant TN, Roberts MW, McIntosh-Michaelis SA, Spackman AJ, et al. The social impact of multiple sclerosis — A study of 305 patients and their relatives. Disabil Rehabil. 2000;22:288–93. doi: 10.1080/096382800296755. [DOI] [PubMed] [Google Scholar]
- 12.Dennison L, Moss-Morris R, Chalder T. A review of psychological correlates of adjustment in patients with multiple sclerosis. Clin Psychol Rev. 2009;29:141–53. doi: 10.1016/j.cpr.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Chwastiak L, Ehde DM, Gibbons LE, Sullivan M, Bowen JD, Kraft GH. Depressive symptoms and severity of illness in multiple sclerosis: Epidemiologic study of a large community sample. Am J Psychiatry. 2002;159:1862–8. doi: 10.1176/appi.ajp.159.11.1862. [DOI] [PubMed] [Google Scholar]
- 14.Jopson NM, Moss-Morris R. The role of illness severity and illness representations in adjusting to multiple sclerosis. J Psychosom Res. 2003;54:503–11. doi: 10.1016/s0022-3999(02)00455-5. [DOI] [PubMed] [Google Scholar]
- 15.Thomas PW, Thomas S, Hillier C, Galvin K, Baker R. Psychological interventions for multiple sclerosis. Cochrane Database Syst Rev. 2006;25:1. doi: 10.1002/14651858.CD004431.pub2. CD004431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hart S, Fonareva I, Merluzzi N, Mohr DC. Treatment for depression and its relationship to improvement in quality of life and psychological well-being in multiple sclerosis patients. Qual Life Res. 2005;14:695–703. doi: 10.1007/s11136-004-1364-z. [DOI] [PubMed] [Google Scholar]
- 17.Seligman ME, Csikszentmihalyi M. Positive psychology. An introduction. Am Psychol. 2000;55:5–14. doi: 10.1037//0003-066x.55.1.5. [DOI] [PubMed] [Google Scholar]
- 18.Keyes CL. Promoting and protecting mental health as flourishing: A complementary strategy for improving national mental health. Am Psychol. 2007;62:95–108. doi: 10.1037/0003-066X.62.2.95. [DOI] [PubMed] [Google Scholar]
- 19.Diener E. Vol. 37. Dordrecht, NL: Springer; 2009. The Science of Well-Being. [Google Scholar]
- 20.Delle Fave A, Massimini F, Bassi M. Dordrecht, NL: Springer; 2011. Psychological Selection and Optimal Experience Across Cultures: Social Empowerment Through Personal Growth. [Google Scholar]
- 21.Csikszentmihalyi M. San Francisco: Jossey-Bass; 1975. Beyond Boredom and Anxiety. [Google Scholar]
- 22.Ryff CD. Happiness is everything, or is it?. Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57:1069–81. [Google Scholar]
- 23.Huta V, Ryan R. Pursuing pleasure or virtue: The differential and overlapping well being benefits of hedonic and eudaimonic motives. J Happiness Stud. 2010;11:735–62. [Google Scholar]
- 24.Sherman TE, Rapport LJ, Hanks RA, Ryan KA, Keenan PA, Khan O, et al. Predictors of well-being among significant others of persons with multiple sclerosis. Mult Scler. 2007;13:238–49. doi: 10.1177/1352458506070754. [DOI] [PubMed] [Google Scholar]
- 25.Ryan KA, Rapport LJ, Sherman TE, Hanks RA, Lisak R, Khan O. Predictors of subjective well-being among individuals with multiple sclerosis. Clin Neuropsychol. 2007;21:239–62. doi: 10.1080/13854040600582460. [DOI] [PubMed] [Google Scholar]
- 26.Barak Y, Achiron A. Happiness and personal growth are attainable in interferon beta-1a treated multiple sclerosis patients. J Happiness Stud. 2011;12:887–95. [Google Scholar]
- 27.Mitosek-Szewczyk K, Kulakowska A, Bartosik-Psujek H, Hozejowski R, Drozdowski W, Stelmasiak Z. Quality of life in polish patients with multiple sclerosis. Adv Med Sci. 2014;59:34–8. doi: 10.1016/j.advms.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 28.Hart S, Fonareva I, Merluzzi N, Mohr DC. Treatment for depression and its relationship to improvement in quality of life and psychological well-being in multiple sclerosis patients. Qual Life Res. 2005;14:695–703. doi: 10.1007/s11136-004-1364-z. [DOI] [PubMed] [Google Scholar]
- 29.Clarke PJ, Marshall VW, Ryff CD, Wheaton B. Measuring psychological well-being in the Canadian study of health and aging. Int Psychogeriatr. 2001;13(Supp 1):79–90. doi: 10.1017/s1041610202008013. [DOI] [PubMed] [Google Scholar]
- 30.Dennison L, Moss-Morris R. Cognitive-behavioral therapy: What benefits can it offer people with multiple sclerosis? Expert Rev Neurother. 2010;10:1383–90. doi: 10.1586/ern.10.111. [DOI] [PubMed] [Google Scholar]
- 31.Wood AM, Joseph S. The absence of positive psychological (eudemonic) well-being as a risk factor for depression: A ten year cohort study. J Affect Disord. 2010;122:213–7. doi: 10.1016/j.jad.2009.06.032. [DOI] [PubMed] [Google Scholar]
- 32.Mitchell AJ, Benito-León J, González JM, Rivera-Navarro J. Quality of life and its assessment in multiple sclerosis: Integrating physical and psychological components of wellbeing. Lancet Neurol. 2005;4:556–66. doi: 10.1016/S1474-4422(05)70166-6. [DOI] [PubMed] [Google Scholar]


