Abstract
Background:
Early puberty is a common worldwide problem. Different parameters as genetics, metabolic diseases, obesity, as well as environmental factors may affect the age of puberty. This systematic review aims to survey the related literature on the effects of environmental pollutants and especially organohalogens and phthalates on early puberty.
Materials and Methods:
A systematic review of papers published in the English language was completed in January 2014. Studies on the associations of organohalogens and phthalates with the puberty time were included. A literature search was conducted in EMBASE, PubMed, Scopus, ISI Web of Science, and Cochrane Library from 1995 to January 2014; moreover manual search through references of relevant manuscripts was considered. The literature search identified 212 papers, of which 13 papers fulfilled the inclusion criteria of the current study. Two reviewers independently identified relevant papers for potential inclusion and assessed the methodological quality.
Results:
This review included 6572 participants in nine countries from three continents (Europe, North America, and Asia). Different studies determined the effects of pollutants on maturation signs and pubertal stages and confirmed the association of organohalogens and phthalates with early puberty.
Conclusion:
Based on the studied literature, environmental pollutants surround and accumulate in human societies and their adverse health effects are well documented. It can be concluded that organohalogens and phthalates are disturbing the normal process of puberty timing; especially their influence on early maturation in girls should be underscored.
Keywords: Early puberty, organohalogens, phthalates, systematic review
INTRODUCTION
Puberty is an important landmark that occurs in the transition from childhood to adulthood.[1,2] Human puberty consequences for health and wellbeing are thoughtful and contradictory. In addition to obtaining physical maturation with enhanced strength, speed, and fitness, puberty is also accompanied with emotional and cognitive changes.[3]
Puberty onset has specific signs, which differs in terms of gender.[4] Timing of puberty may be important in expecting longitudinal health risks like obesity and cancers in adulthood.[2] Longer exposure to steroidal hormones might increase the risk of steroidseries dependent cancers such as breast and ovarian cancers in women, and possibly prostate cancer in men. Furthermore, increased rates of obesity in early developers might amplify oxidative stresses that in turn would exacerbate the risks for a range of cancers.[3] True precocious puberty in girls is typically defined as the appearance of secondary sexual characteristics before the age of 6 years.[5] During the past decades, secular trends of earlier age at onset of puberty have been observed.[4] Different research studies have reported the reduction in the age of puberty around the world.[6,7,8,9,10] Precocious puberty in boys is generally defined as the appearance of secondary sexual characteristics before the age of 9 years.[11,12,13]
Different factors are contributed in the decreasing age of puberty in the recent years. Genetic factors play a main role in the timing of maturation. However, the rapid worldwide decrease in pubertal timing over the past decades clearly indicates that it should have an environmental etiology. Significant diversities in the age of pubertal stages of girls living in various regions with different ethnicity and geographic characteristics are documented. Moreover, obesity as an epidemic event has received special attention and is related both to early puberty and environmental factors. Furthermore, changes in nutrition and dietary habits, physical activity, and exposure to endocrine disrupting chemicals (EDCs) are possible factors influencing the maturation time of the reproductive system.[2,3,14,15] EDCs are natural and synthetic chemicals that would disturb the normal function of the endocrine system. These compounds interfere with normal hormonal function through influence on the activity of estrogen receptors.[16] EDCs are exogenous chemicals that usually imitate hormones, block hormonal action sites or trigger inappropriate hormone activity.[17] Different studies determined the role of some pollutants as polychlorinated biphenyls (PCBs), polybrominated biphenyl (PBB), dioxins, phthalates, etc., on pubertal growth and its signs.[14,18,19] Of important groups of these compounds are organohalogens and phthalates. These compounds are usually highly lipophilic and hydrophobic; they accumulate sometimes to a high concentration in lipid-rich tissues.[20] This study aims to systematically review the literature that assessed the associations of organohalogens and phthalates with the timing of puberty.
MATERIALS AND METHODS
Literature search
We attempted to explore papers in which the associations of organohalogens exposure on pubertal signs have been reported. A literature search was done in following databases: EMBASE, PubMed, Scopus, ISI Web of Science, and Cochrane Library from 1995 to January 2014, with the major concentration on latest papers. The following keywords or their combinations were used: Early puberty, precocious puberty, menarche, organohalogens, PCBs, dichlorodiphenyltrichloroethane, dichloro diphenyldichloro ethylene, organochlorine, dioxin, phthalates, girl, boy, children, adolescents. Further studies were observed by a manual search through references of relevant manuscripts, relevant reviews, and consultation with experts in this field. Search evaluation was done randomly by two independent researchers, and it was confirmed that all relevant studies were considered.
Study design
Two independent reviewers (PP and EA) determined the appropriateness of the study according to the prearranged criteria and subsequently extracted characteristics: Related data of participants (number, age, type of disorder), study features (type, duration, applied intervention), measured parameters (first menarche, breast development, testicular development, Tanner stage signs, body size) and outcomes. Differences in judgments were solved via discussion and consensus. Paper language selection was limited to English.
Data collection
Inclusion criteria for data collection were as follows
Exposure to one or more than one organohalogens during childhood or adolescence.
Measurement of related criteria as first menarche, breast development, testicular development, Tanner stage signs, body size.
No history of using drugs or other determined compounds with the effects on endocrine systems.
Studies without above mentioned criteria were not included in this systematic review.
RESULTS
Study selection
The flowchart of the search is depicted in Figure 1. At first, 215 likely relevant articles were found. Of those, 202 articles were removed by evaluating abstracts, and it was cleared that those papers could not meet the inclusion criteria of the current study. Finally, 13 articles were selected to read their full texts and to determine the eligible articles to be included in this systematic review.
Figure 1.
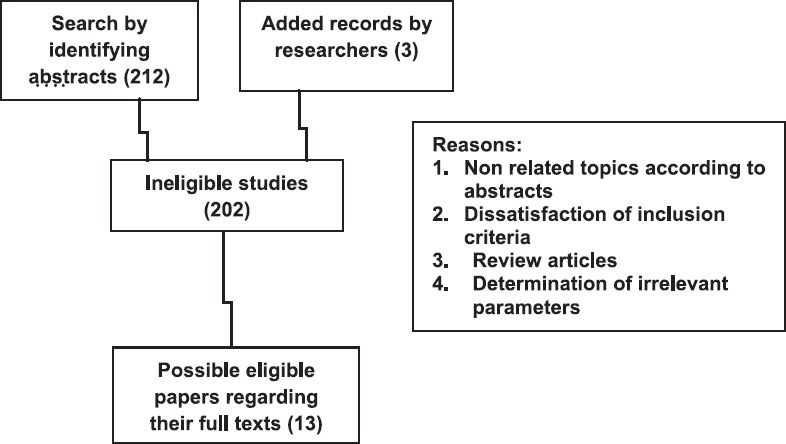
Flowchart and characteristics of studies included/excluded for review
Study features
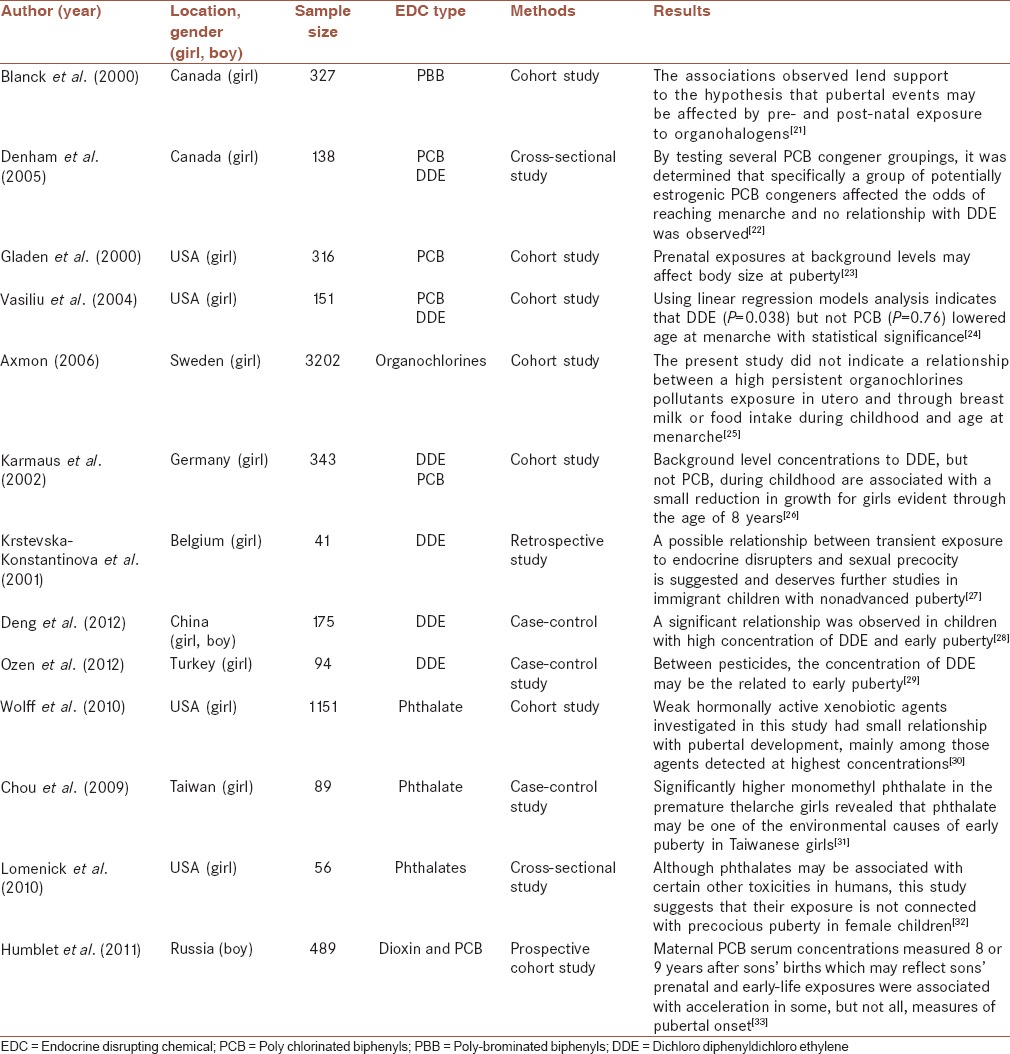
As aforementioned, 13 articles were selected according to the inclusion criteria. This review included 6572 participants in nine countries from three continents (Europe, North America, and Asia). Of these, seven studies had a cohort design, two were cross-sectional, one was retrospective, and three were case-control. Details of the studies are presented in Table 1.
Table 1.
Summary of studies on the association of exposure to organohalogens and phthalates with puberty time
DISCUSSION
This review confirmed the effects of pollutants on maturation signs and pubertal stages and confirmed the association of organohalogens and phthalates with early puberty, notably in girls. Such an effect may have short-term and long-term health effects, and warrants interventions to reduce these pollutants.
Puberty time is a transition step between childhood and the adult reproductive stage. It is an important stage of life with elevated increased risk of health and psychosocial problems.[34,35,36,37,38] It is documented that an independent relationship might exist between early puberty and adult metabolic syndrome-related derangements both in males and females. This finding underlined that the mechanisms accelerating puberty may also contribute to adult metabolic disorders.[38]
We reviewed several articles from different areas of the world, and it is unanimous that variation in puberty timing trends is a global issue, both in developed and developing countries. Though the age of puberty is related to different parameters including genetic factors,[39] disorders and malformations of central nervous system,[13] and some metabolic diseases,[40] the important role of environmental pollutants and EDCs should be taken into account.
Environmental pollutants including PBC, PBB, dioxin, and phthalates are widespread in different societies and have several adverse health effects.[28,29,33,41] One of the important consequences of EDCs is disturbing the normal process of puberty timing, especially their influence on early maturation in both sexes, particularly in girls. In boys, pollutants exposure is associated with reaching to genital stages earlier than normal time.[28,33] In girls, a higher concentration of EDCs in the body is associated with early menarche and breast development with or without growth of pubic hair.[21,32]
A recent review studied the trends of puberty and its relationship with environmental pollutants and concluded that the age at pubertal onset has been declining in the last two decades in USA and Europe. Thus, age at breast development is now going on 1-2 years earlier in comparison with previous studies. Prominently, the age at menarche has changed by 0.3-0.6 years in the same period, signifying a prolonged duration of the pubertal transition and found that development of glandular breast tissue at much younger ages at short period of time are highly suggested to have environmental origins.[19]
Weight status is associated with the pubertal age, given that environmental pollutants may increase the risk of overweight,[42,43,44] therefore the decline in the age of puberty may be explained, at least in part, by excess weight due to exposure to some environmental pollutants.
It should be acknowledged that in original studies included in the current review, the exact time and the duration of exposure were not considered; moreover recall bias may exist in reporting the age of puberty. Chronic diseases origin in early life, and it is well documented that exposure of children and adolescents to environmental pollutants is related with risk factors of noncommunicable diseases.[45,46,47,48] Furthermore, the age of puberty, which in turn might be related to exposure to environmental factors, is associated with chronic diseases.[49,50]
CONCLUSION
The findings of this review propose that organohalogens and phthalates are disturbing the normal process of puberty timing with special influence on early maturation in girls. The current decline in the age of puberty might be related, at least in part, to exposure to some environmental chemicals, and in turn it might increase the risk of noncommunicable diseases in the future. These findings underscore the necessity of implementing wide-ranging interventions to reduce the pollution burden for health promotion and disease prevention at the global level.
Financials support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
AUTHOR'S CONTRIBUTION
All authors contributed in the study concept and design, in conducting the literature search, in drafting the paper and its revision. All authors approved the final version for submission, and accept the responsibility for the paper content.
REFERENCES
- 1.Yousefi M, Karmaus W, Zhang H, Roberts G, Matthews S, Clayton B, et al. Relationships between age of puberty onset and height at age 18 years in girls and boys. World J Pediatr. 2013;9:230–8. doi: 10.1007/s12519-013-0399-z. [DOI] [PubMed] [Google Scholar]
- 2.Sørensen K, Mouritsen A, Aksglaede L, Hagen CP, Mogensen SS, Juul A. Recent secular trends in pubertal timing: Implications for evaluation and diagnosis of precocious puberty. Horm Res Paediatr. 2012;77:137–45. doi: 10.1159/000336325. [DOI] [PubMed] [Google Scholar]
- 3.Patton GC, Viner R. Pubertal transitions in health. Lancet. 2007;369:1130–9. doi: 10.1016/S0140-6736(07)60366-3. [DOI] [PubMed] [Google Scholar]
- 4.Parent AS, Teilmann G, Juul A, Skakkebaek NE, Toppari J, Bourguignon JP. The timing of normal puberty and the age limits of sexual precocity: Variations around the world, secular trends, and changes after migration. Endocr Rev. 2003;24:668–93. doi: 10.1210/er.2002-0019. [DOI] [PubMed] [Google Scholar]
- 5.Mogensen SS, Aksglaede L, Mouritsen A, Sørensen K, Main KM, Gideon P, et al. Diagnostic work-up of 449 consecutive girls who were referred to be evaluated for precocious puberty. J Clin Endocrinol Metab. 2011;96:1393–401. doi: 10.1210/jc.2010-2745. [DOI] [PubMed] [Google Scholar]
- 6.Foster TA, Voors AW, Webber LS, Frerichs RR, Berenson GS. Anthropometric and maturation measurements of children, ages 5 to 14 years, in a biracial community — The Bogalusa Heart Study. Am J Clin Nutr. 1977;30:582–91. doi: 10.1093/ajcn/30.4.582. [DOI] [PubMed] [Google Scholar]
- 7.Aksglaede L, Olsen LW, Sørensen TI, Juul A. Forty years trends in timing of pubertal growth spurt in 157,000 Danish school children. PLoS One. 2008;3:e2728. doi: 10.1371/journal.pone.0002728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Semiz S, Kurt F, Kurt DT, Zencir M, Sevinç O. Pubertal development of Turkish children. J Pediatr Endocrinol Metab. 2008;21:951–61. doi: 10.1515/jpem.2008.21.10.951. [DOI] [PubMed] [Google Scholar]
- 9.Castellino N, Bellone S, Rapa A, Vercellotti A, Binotti M, Petri A, et al. Puberty onset in Northern Italy: A random sample of 3597 Italian children. J Endocrinol Invest. 2005;28:589–94. doi: 10.1007/BF03347256. [DOI] [PubMed] [Google Scholar]
- 10.Herman-Giddens ME, Slora EJ, Wasserman RC, Bourdony CJ, Bhapkar MV, Koch GG, et al. Secondary sexual characteristics and menses in young girls seen in office practice: A study from the Pediatric Research in Office Settings network. Pediatrics. 1997;99:505–12. doi: 10.1542/peds.99.4.505. [DOI] [PubMed] [Google Scholar]
- 11.Rey RA, Grinspon RP, Gottlieb S, Pasqualini T, Knoblovits P, Aszpis S, et al. Male hypogonadism: An extended classification based on a developmental, endocrine physiology-based approach. Andrology. 2013;1:3–16. doi: 10.1111/j.2047-2927.2012.00008.x. [DOI] [PubMed] [Google Scholar]
- 12.Magnusson U, Ljungvall K. Environmental pollutants and dysregulation of male puberty — A comparison among species. Reprod Toxicol. 2014;44:23–32. doi: 10.1016/j.reprotox.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Menon PS, Vijayakumar M. Precocious puberty — Perspectives on diagnosis and management. Indian J Pediatr. 2014;81:76–83. doi: 10.1007/s12098-013-1177-6. [DOI] [PubMed] [Google Scholar]
- 14.Walvoord EC. The timing of puberty: Is it changing?. Does it matter. J Adolesc Health. 2010;47:433–9. doi: 10.1016/j.jadohealth.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 15.Motlagh ME, Rabbani A, Kelishadi R, Mirmoghtadaee P, Shahryari S, Ardalan G, et al. Timing of puberty in Iranian girls according to their living area: A national study. J Res Med Sci. 2011;16:276–81. [PMC free article] [PubMed] [Google Scholar]
- 16.Li Y, Luh CJ, Burns KA, Arao Y, Jiang Z, Teng CT, et al. Endocrine-disrupting chemicals (EDCs): In vitro mechanism of estrogenic activation and differential effects on ER target genes. Environ Health Perspect. 2013;121:459–66. doi: 10.1289/ehp.1205951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharara FI, Seifer DB, Flaws JA. Environmental toxicants and female reproduction. Fertil Steril. 1998;70:613–22. doi: 10.1016/s0015-0282(98)00253-2. [DOI] [PubMed] [Google Scholar]
- 18.Butte NF, Garza C, de Onis M. Evaluation of the feasibility of international growth standards for school-aged children and adolescents. J Nutr. 2007;137:153–7. doi: 10.1093/jn/137.1.153. [DOI] [PubMed] [Google Scholar]
- 19.Toppari J, Juul A. Trends in puberty timing in humans and environmental modifiers. Mol Cell Endocrinol. 2010;324:39–44. doi: 10.1016/j.mce.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 20.Jepson PD, Deaville R, Barnett J, Davison NJ, Paterson IA, Penrose RS, et al. Persistent organic pollutants in UK-stranded cetaceans (1990-2008): Linking exposure with toxic effects. Chemical Pollution and Marine Mammals. Final report to the Department for Environment, Food and Rural Affairs. 2013:9. [Google Scholar]
- 21.Blanck HM, Marcus M, Tolbert PE, Rubin C, Henderson AK, Hertzberg VS, et al. Age at menarche and tanner stage in girls exposed in utero and postnatally to polybrominated biphenyl. Epidemiology. 2000;11:641–7. doi: 10.1097/00001648-200011000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Denham M, Schell LM, Deane G, Gallo MV, Ravenscroft J, DeCaprio AP, et al. Relationship of lead, mercury, mirex, dichlorodiphenyldichloroethylene, hexachlorobenzene, and polychlorinated biphenyls to timing of menarche among Akwesasne Mohawk girls. Pediatrics. 2005;115:e127–34. doi: 10.1542/peds.2004-1161. [DOI] [PubMed] [Google Scholar]
- 23.Gladen BC, Ragan NB, Rogan WJ. Pubertal growth and development and prenatal and lactational exposure to polychlorinated biphenyls and dichlorodiphenyl dichloroethene. J Pediatr. 2000;136:490–6. doi: 10.1016/s0022-3476(00)90012-x. [DOI] [PubMed] [Google Scholar]
- 24.Vasiliu O, Muttineni J, Karmaus W. In utero exposure to organochlorines and age at menarche. Hum Reprod. 2004;19:1506–12. doi: 10.1093/humrep/deh292. [DOI] [PubMed] [Google Scholar]
- 25.Axmon A. Menarche in women with high exposure to persistent organochlorine pollutants in utero and during childhood. Environ Res. 2006;102:77–82. doi: 10.1016/j.envres.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 26.Karmaus W, Asakevich S, Indurkhya A, Witten J, Kruse H. Childhood growth and exposure to dichlorodiphenyl dichloroethene and polychlorinated biphenyls. J Pediatr. 2002;140:33–9. doi: 10.1067/mpd.2002.120764. [DOI] [PubMed] [Google Scholar]
- 27.Krstevska-Konstantinova M, Charlier C, Craen M, Du Caju M, Heinrichs C, de Beaufort C, et al. Sexual precocity after immigration from developing countries to Belgium: Evidence of previous exposure to organochlorine pesticides. Hum Reprod. 2001;16:1020–6. doi: 10.1093/humrep/16.5.1020. [DOI] [PubMed] [Google Scholar]
- 28.Deng F, Tao FB, Liu DY, Xu YY, Hao JH, Sun Y, et al. Effects of growth environments and two environmental endocrine disruptors on children with idiopathic precocious puberty. Eur J Endocrinol. 2012;166:803–9. doi: 10.1530/EJE-11-0876. [DOI] [PubMed] [Google Scholar]
- 29.Ozen S, Darcan S, Bayindir P, Karasulu E, Simsek DG, Gurler T. Effects of pesticides used in agriculture on the development of precocious puberty. Environ Monit Assess. 2012;184:4223–32. doi: 10.1007/s10661-011-2257-6. [DOI] [PubMed] [Google Scholar]
- 30.Wolff MS, Teitelbaum SL, Pinney SM, Windham G, Liao L, Biro F, et al. Investigation of relationships between urinary biomarkers of phytoestrogens, phthalates, and phenols and pubertal stages in girls. Environ Health Perspect. 2010;118:1039–46. doi: 10.1289/ehp.0901690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chou YY, Huang PC, Lee CC, Wu MH, Lin SJ. Phthalate exposure in girls during early puberty. J Pediatr Endocrinol Metab. 2009;22:69–77. doi: 10.1515/jpem.2009.22.1.69. [DOI] [PubMed] [Google Scholar]
- 32.Lomenick JP, Calafat AM, Melguizo Castro MS, Mier R, Stenger P, Foster MB, et al. Phthalate exposure and precocious puberty in females. J Pediatr. 2010;156:221–5. doi: 10.1016/j.jpeds.2009.09.047. [DOI] [PubMed] [Google Scholar]
- 33.Humblet O, Williams PL, Korrick SA, Sergeyev O, Emond C, Birnbaum LS, et al. Dioxin and polychlorinated biphenyl concentrations in mother's serum and the timing of pubertal onset in sons. Epidemiology. 2011;22:827–35. doi: 10.1097/EDE.0b013e318230b0d1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schoeters G, Den Hond E, Dhooge W, van Larebeke N, Leijs M. Endocrine disruptors and abnormalities of pubertal development. Basic Clin Pharmacol Toxicol. 2008;102:168–75. doi: 10.1111/j.1742-7843.2007.00180.x. [DOI] [PubMed] [Google Scholar]
- 35.Bordini B, Rosenfield RL. Normal pubertal development: Part II: Clinical aspects of puberty. Pediatr Rev. 2011;32:281–92. doi: 10.1542/pir.32-7-281. [DOI] [PubMed] [Google Scholar]
- 36.Allison CM, Hyde JS. Early menarche: Confluence of biological and contextual factors. Sex Roles. 2013;68:55–64. [Google Scholar]
- 37.Ong KK, Elks CE, Wills AK, Wong A, Wareham NJ, Loos RJ, et al. Associations between the pubertal timing-related variant in LIN28B and BMI vary across the life course. J Clin Endocrinol Metab. 2011;96:E125–9. doi: 10.1210/jc.2010-0941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Widén E, Silventoinen K, Sovio U, Ripatti S, Cousminer DL, Hartikainen AL, et al. Pubertal timing and growth influences cardiometabolic risk factors in adult males and females. Diabetes Care. 2012;35:850–6. doi: 10.2337/dc11-1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Palmert MR, Boepple PA. Variation in the timing of puberty: Clinical spectrum and genetic investigation. J Clin Endocrinol Metab. 2001;86:2364–8. doi: 10.1210/jcem.86.6.7603. [DOI] [PubMed] [Google Scholar]
- 40.Burt Solorzano CM, McCartney CR. Obesity and the pubertal transition in girls and boys. Reproduction. 2010;140:399–410. doi: 10.1530/REP-10-0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aronson KJ, Miller AB, Woolcott CG, Sterns EE, McCready DR, Lickley LA, et al. Breast adipose tissue concentrations of polychlorinated biphenyls and other organochlorines and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2000;9:55–63. [PubMed] [Google Scholar]
- 42.de Cock M, van de Bor M. Obesogenic effects of endocrine disruptors, what do we know from animal and human studies? Environ Int. 2014;70:15–24. doi: 10.1016/j.envint.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 43.Kelishadi R, Poursafa P, Jamshidi F. Role of environmental chemicals in obesity: A systematic review on the current evidence. J Environ Public Health. 2013;2013:896789. doi: 10.1155/2013/896789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sharpe RM, Drake AJ. Obesogens and obesity — An alternative view? Obesity (Silver Spring) 2013;21:1081–3. doi: 10.1002/oby.20373. [DOI] [PubMed] [Google Scholar]
- 45.Calderón-Garcidueñas L, Villarreal-Calderon R, Valencia-Salazar G, Henríquez-Roldán C, Gutiérrez-Castrellón P, Torres-Jardón R, et al. Systemic inflammation, endothelial dysfunction, and activation in clinically healthy children exposed to air pollutants. Inhal Toxicol. 2008;20:499–506. doi: 10.1080/08958370701864797. [DOI] [PubMed] [Google Scholar]
- 46.Kelishadi R, Mirghaffari N, Poursafa P, Gidding SS. Lifestyle and environmental factors associated with inflammation, oxidative stress and insulin resistance in children. Atherosclerosis. 2009;203:311–9. doi: 10.1016/j.atherosclerosis.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 47.Sun Z, Mukherjee B, Brook RD, Gatts GA, Yang F, Sun Q, et al. Air-Pollution and Cardiometabolic Diseases (AIRCMD): A prospective study investigating the impact of air pollution exposure and propensity for type II diabetes. Sci Total Environ. 2013;448:72–8. doi: 10.1016/j.scitotenv.2012.10.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kelishadi R, Hashemi M, Javanmard SH, Mansourian M, Afshani M, Poursafa P, et al. Effect of particulate air pollution and passive smoking on surrogate biomarkers of endothelial dysfunction in healthy children. Paediatr Int Child Health. 2014;34:165–9. doi: 10.1179/2046905513Y.0000000104. [DOI] [PubMed] [Google Scholar]
- 49.Charalampopoulos D, McLoughlin A, Elks CE, Ong KK. Age at menarche and risks of all-cause and cardiovascular death: A systematic review and meta-analysis. Am J Epidemiol. 2014;180:29–40. doi: 10.1093/aje/kwu113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mueller NT, Duncan BB, Barreto SM, Chor D, Bessel M, Aquino EM, et al. Earlier age at menarche is associated with higher diabetes risk and cardiometabolic disease risk factors in Brazilian adults: Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) Cardiovasc Diabetol. 2014;13:22. doi: 10.1186/1475-2840-13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]


