Abstract
Objectives:
To examine relationship between the quality of marital relationship and anxiety among women with breast cancer (BC) in the Kingdom of Saudi Arabia (KSA).
Methods:
This cross-sectional study recruited a consecutive series of 49 married women with BC seen in the Al-Amoudi Breast Cancer Center of Excellence at King Abdulaziz University, Jeddah, KSA in early 2013. Participants completed the Hospital Anxiety and Depression Scale, Spouse Perception Scale, and Quality of Marriage Index forms, and answered questions on demographic and cancer characteristics.
Results:
Anxiety symptoms indicating “possible” anxiety disorder were present in 10.4% and “probable” anxiety disorder in 14.6% (25% total). No significant relationship was found between the quality of marital relationship and anxiety symptoms (B=-0.04, standard error=0.05, t=-0.81, p=0.42). Anxiety was primarily driven by low education, poor socioeconomic status, and young age.
Conclusion:
Anxiety symptoms are prevalent among married women with BC seen in a university-based clinic in the KSA. Further research is needed to determine whether a diagnosis of BC adversely affects marital relationship, and whether this is the cause for anxiety in these women.
Breast cancer (BC) is the most common cause of cancer death in women worldwide,1 and the Kingdom of Saudi Arabia (KSA) is no exception.2 Breast cancer has become a particular problem in Arab countries due to its late stage at presentation and its increased occurrence among young women.3 Both during and after treatment, even if the cancer goes into remission, concerns regarding recurrence, effect on the marital relationship, and frequent medical visits for monitoring, often result in high levels of anxiety (including post-traumatic stress-like symptoms).4-8 Anxiety and other mood symptoms are not benign in women with BC, as they are associated with increased mortality and cancer recurrence.9,10
Studies in Western countries (United States, Canada, England, Australia, and Germany) indicate a prevalence of significant anxiety ranging from 4-45% in BC patients, depending on anxiety measure, cutoff score, geographical region, and time since diagnosis11-14 (compared with 15-37% of cancer patients in general with anxiety during the first year after diagnosis).15 The most commonly used measure of anxiety symptoms in BC patients is the Hospital Anxiety and Depression Scale (HADS), which assesses for “possible” and “probable” anxiety disorder (with a sensitivity and specificity of approximately 80%).12,16,17 Using this measure, the prevalence of “probable” anxiety disorder in BC patients ranges from 2-23% and “possible” anxiety disorder is present in an additional 19-22% (21-45% combined).11,13,18 Although factors that increase risk of anxiety in women with BC are poorly understood, a few studies largely from Western countries report more symptoms in younger persons and Caucasians, immigrants, those with lower education, later disease stage, and lower social support.8,11,13,19 In one of the few studies from an Eastern country,20 anxiety levels among BC patients from Bangkok, Thailand, were significantly higher among those with poor problem solving skills, more pain and fatigue, and poorer family functioning. Although research is limited almost entirely to the US and other Western countries, studies indicate that support from a spouse (especially emotional support) improves the adjustment of women to BC,21-25 and may even impact survival.26 Not all studies, however, report that having a marital partner buffers against the stress of BC.27,28 The demands of caregiving, the effects of BC and its treatments on sexual relationship, and coping with psychological changes in a BC patient can all lead to lower well-being in a spouse, and decrease his ability to provide support.24 Our exhaustive review of the literature uncovered several studies that have examined the prevalence of emotional reactions to BC in the Middle East, finding that 19-73% of women had significant anxiety symptoms.22,29-34 In those studies, anxiety was associated with poorer physical functioning, the presence of metastatic disease, higher education, lower social support, duration of marriage, and spouse’s level of anxiety. With regard to KSA, there has been a significant increase in the incidence of BC, which occurs at a younger age than in Western countries.35 A recent review of research on coping with BC, however, revealed not a single study from KSA.36 Our review identified only 2 studies37,38 that examined the prevalence or correlates of anxiety in Saudi cancer patients (none specifically in BC), and only one study39 that examined attitudes of Saudi males toward BC. The first study examined anxiety in 30 hospitalized patients with cancer (9 with BC) at the King Khalid National Guard Hospital in Jeddah, KSA.37 Researchers found that anxiety symptoms assessed by the Hamilton Anxiety Scale were significantly higher in cancer patients compared with 39 patients with a range of chronic illnesses; 3 patients with cancer (10%) had a clinical diagnosis of generalized anxiety disorder based on Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) criteria. The second study examined non-pain symptoms in 124 cancer patients (27% with BC) at King Faisal Specialist Hospital in Riyadh, KSA.38 The most frequently reported non-pain symptoms were fatigue (80%), loss of appetite (72%), dry mouth (69%), and anxiety (61%). Finally, researchers examined attitudes toward BC among males accompanying female patients to outpatient clinics at King Abdulaziz Hospital in Jeddah, KSA. When men were asked what they would do if their wives were diagnosed with BC, 9.4% said they would leave their wives.39
Given the current knowledge gap on this subject in KSA, we decided to: 1) determine the prevalence of anxiety symptoms in married women seen in an urban-based university outpatient clinic in Jeddah; 2) identify the correlates of anxiety symptoms (especially marital quality [MQ]); and 3) determine whether the relationship between MQ and anxiety differed between Saudi nationals and immigrants. We hypothesized that anxiety symptoms would be prevalent, that higher MQ would be strongly and inversely related to anxiety symptoms, and that this relationship would be particularly strong in women who were Saudi nationals (where cultural factors might have the most influence).
Methods
Identification of prior research studies was performed using the search terms: anxiety; BC; marital relationship; spouse; MQ; Middle East; and KSA in various combinations. These search words were entered into PubMed and Google Scholar to locate all relevant studies. A convenience sample of women with BC (volunteers) was recruited between January 2013 and March 2013 from King Abdulaziz University’s (KAU) Sheikh Mohammed Hussein Al-Amoudi Breast Cancer Center of Excellence in Jeddah, KSA. Consecutive women presenting to the outpatient clinic for initial assessment or follow-up were approached for inclusion in the study. The inclusion criteria were: age 18 to 65 years; diagnosis of BC documented in the medical record; currently married; and attending the clinic on the day that the interviewers were present in the clinic. The exclusion criteria were women without BC, those outside the age range above, those who were not currently married, and all those being seen on days and times when interviewers were not present. The average length of time that participants were diagnosed with and/or experienced symptoms of BC were 38.4 months (range 2 weeks to 180 months). The questionnaire was translated into Arabic, and was self-completed by participants. Medical students (trained by KAU psychiatry faculty on how to approach patients, obtain consent, and administer the questionnaire) explained the study to the participants and obtained informed consent before proceeding. The institutional review board of KAU Hospital approved the study following the principles of the Helsinki Declaration.
Questionnaire
Participants were asked regarding their age (27-65 years), nationality/citizenship (Saudi=1 versus immigrant=0), education level (none=1, primary school only=2, high school only=3, university=4, post-graduate=5), employment status (yes=1 versus no=0), and family income per month (<3,000 Saudi Arabian Riyals (SAR)=1; 3,000 to 5,000=2; >5,000=3). Also assessed were duration of illness in months (0.5-180) and type of treatment received (radiation therapy, chemotherapy, surgery).
Anxiety
The HADS16 is a self-rated scale commonly used to measure anxiety and depressive symptoms in outpatient medical populations including those in the Middle East.30,31,32 Scores of 0-7 are considered normal, 8-10 signify “possible” anxiety disorder, and 11-21 indicate “probable” anxiety disorder (range 0-21). The Cronbach’s alpha for anxiety subscale (HADS-A) is reported to be high (0.85).40 The reliability and validity of HADS in Arabic has been previously established.41 In the current study, HADS-A subscale’s alpha was 0.78 (standardized), which is above the recommended threshold of 0.70.42
Marital relations
Two standard scales were used to measure marital adjustment. The Spousal Perception Scale (SPS) is a self-rated 12-item measure of emotional support and emotional strain in the relationship with a spouse.43 In the present study, we administered the 6-item emotional support subscale where each item is rated from one (not at all) to 4 (a lot), with a score range from 6-24 (higher scores indicating greater perceived spousal support). The average score in the original validation study was approximately 20.43 The Cronbach’s alpha of the scale is reported to be 0.91.44 In the present study, the internal reliability was similarly high (alpha=0.85). The second scale administered was the Quality of Marriage Index (QMI).45 The QMI is a 6-item self-rated scale that assesses the “essential goodness of a relationship.” Each item is rated on a scale from one (very strong disagreement) to 7 (very strong agreement) with a theoretical score range of 7-42 (higher scores indicating a more positive marital relationship). Average scores have been reported to range from 28-37, with higher scores in men.46-48 Internal reliability of the QMI ranges from 0.91-0.97.44 The alpha in the present sample was 0.89. For inclusion in multivariate analyses, the SPS and QMI were combined to form a 12-item scale that ranged from 6-66 (alpha=0.91). Although the psychometric properties of the Arabic versions of the above 2 scales have not been established, we chose these measures based on their “content” validity; as noted above, both scales’ reliability in the present sample was acceptable.
Statistical analyses
The characteristics of the sample were described by means + standard deviations (SD) or percentages (Table 1). A correlation matrix (Pearson r) was constructed for all study variables (Table 2). In multivariate analyses, income was dichotomized into low (<3,000=0) versus high (>3,000=1), and education was dichotomized into low (0=no education or only primary school) versus high (one=high school or beyond). Blocks of independent variables were entered in a stepwise fashion into 3 general linear models predicting the dependent variable (anxiety symptoms): model one included only the sample demographics (age, nationality, education, employment, income); model 2 included demographics and cancer-related factors; and model 3 included demographics, cancer-related factors, and overall MQ (Table 3). Given the sample size, only independent variables significant at p<0.10 were carried forward into later models. Since these analyses were largely exploratory, the significance level was set at p=0.05, and analyses were not adjusted for multiple comparisons. All analyses were performed using the Statistical Analysis System version 9.3 (SAS Institute Inc., Cary, North Carolina, USA).
Table 1.
Characteristics of the participants included in a study on anxiety in Jeddah, Kingdom of Saudi Arabia (n=49).
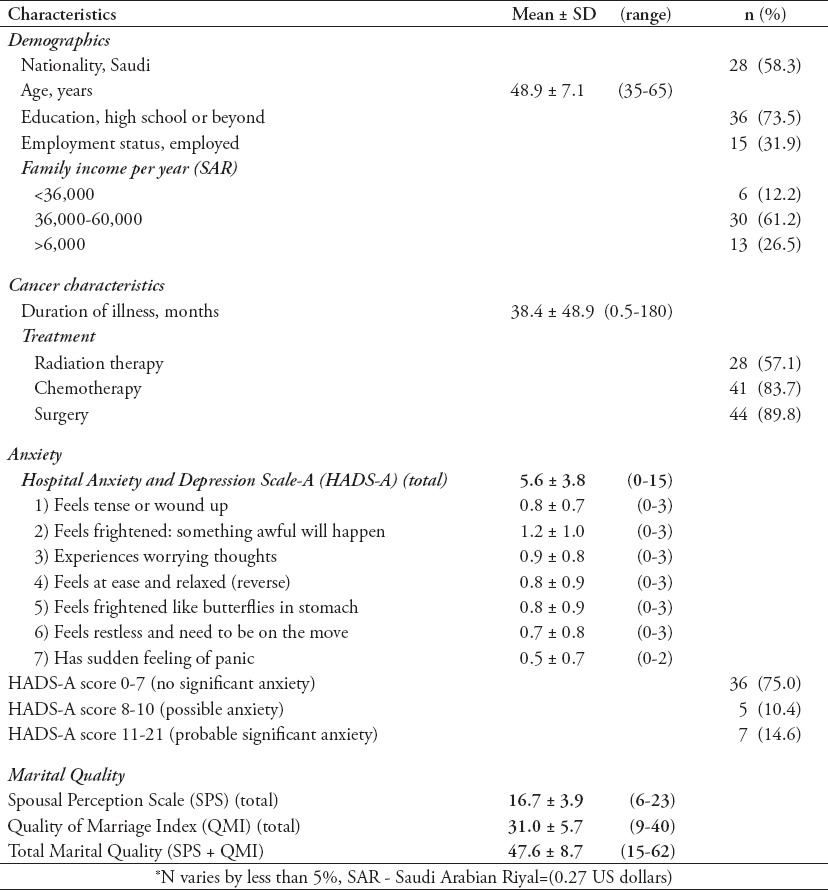
Table 2.
Bivariate correlations between all study variables as found in a study on anxiety in Jeddah, Kingdom of Saudi Arabia.
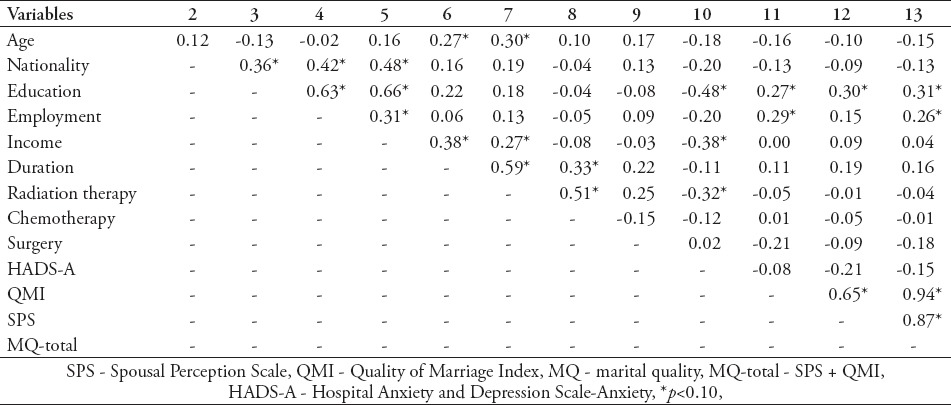
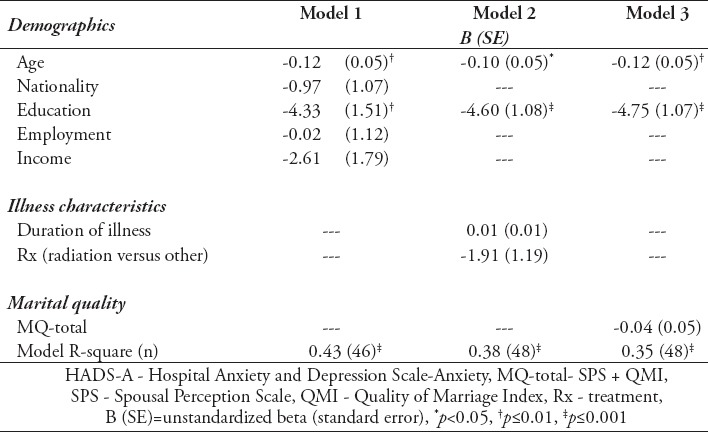
Table 3.
Multivariate model examining relationship between anxiety (HADS-A) and overall marital quality (MQ-total) of the study sample.
Results
Of the 50 women approached to participate in the study, all (100%) agreed to complete the questionnaire. One participant, however, completed only part of the questionnaire, leaving a final sample of 49. The average age of participants was 48.9 (SD=7.1) years, with a range from 35-65 (Table 1). Most participants were Saudi citizens (58.3%). Three-quarters (73.5%) had graduated from high school or attended college, although only one-third (31.9%) were employed. The average yearly family income was 48,000 SAR (approximately $12,000 per year). The average duration of illness since diagnosis of BC was 3 years (38.4 months). The most common type of cancer treatment was surgery (89.8%), followed by chemotherapy (83.7%) and radiation therapy (57.1%). Marital adjustment, on average, was low to moderate. Perception of spouse support SPS averaged 16.7 (SD=3.9) on a theoretical range of 6-24, indicating low to moderate support compared with an average of 20 in Western samples.43 The QMI averaged 31.0 (SD=5.7), indicating moderate MQ compared with scores in Western samples that have ranged from 28-37.46-48 The overall quality of the marital relationship (summing the SPS and QMI) averaged 47.6 (SD=8.7) with a theoretical score ranging from 12-66. The average number of anxiety symptoms was 5.6 (SD=3.8), ranging from 0-15 (where the theoretical score range was 0-21). The prevalence of ‘possible’ anxiety disorder (HADS-A score 8-10) was 10.4% and ‘probable’ anxiety disorder (HADS-A score 11-21) was 14.6%. The most common anxiety symptom was feeling frightened something awful would happen, while the least common symptom was having a sudden feeling of panic. Bivariate correlates of anxiety symptoms were lower education (r=-0.48, p=0.0005), lower income (r=-0.38, p=0.007), and not receiving radiation therapy (r=-0.32, p=0.03) (Table 2). There were weak, non-significant inverse relationships between symptoms of anxiety and the perception that the spouse cares and understands (r=-.21, p=0.15), perceived MQ (r=-0.08, p=0.58), and overall quality of the relationship (r=-0.15, p=0.32) (Figure 1), where average anxiety scores are plotted again MQ in decile (tenths). Multivariate analyses indicated that only age (B=-0.12, standard error [SE]=0.05, p=0.01) and education (B=-4.75, SE=1.07, p<0.0001) were independently associated with anxiety symptoms (Table 3) Model 3. As in bivariate analyses, no significant relationship was found between the overall quality of the marital relationship and anxiety symptoms (B=-0.04, SE=0.05, t=-0.81, p=0.42). Nationality did not moderate this relationship (interaction B=0.07, SE=12.7, t=0.59, p=0.56). In other words, the inverse relationship between marital relationship quality and anxiety was not stronger in women who were Saudi citizens compared with those who were immigrants.
Figure 1.
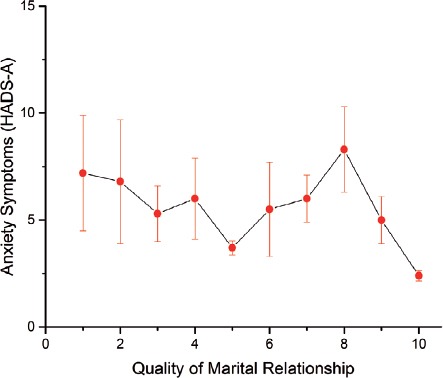
Relationship between quality of the marital relationship and anxiety symptoms, with standard errors. HADS-A - Hospital Anxiety and Depression Scale - Anxiety subscale.
Discussion
Approximately one in 7 women (14.6%) had anxiety symptoms that were frequent enough to qualify them for a “probable” anxiety disorder, and an additional 10.4% had symptoms on the HADS that indicated a “possible” anxiety disorder, resulting in a total of 25% with significant anxiety symptoms. This prevalence rate of anxiety symptoms is similar to that reported in Western countries using the HADS (2-23% for probable anxiety disorder; 19-22% for possible disorder, 21-45% combined), although is on the low side.11,13,18 Contrary to our predictions, the quality of the marital relationship was not significantly related to anxiety symptoms, and nationality (Saudi versus immigrant) did not moderate this relationship. More important as a risk factor for anxiety were age and education. Younger women were more likely to experience anxiety symptoms, as were women with lower education, lower income, and lack of employment (which education probably acted as a proxy for in multivariate analyses). No other characteristic (including time since diagnosis) was related to anxiety symptoms.
Our failure to find a relationship between anxiety symptoms and perceived support from the spouse, or quality of the marriage may be due to several factors. First, religious and cultural traditions in this patriarchal society may have led women to accept and successfully cope with lack of spousal support, and therefore adapt to their cancer in other ways - perhaps through support from other family members, or their religious beliefs. A second possibility was our sample size, which reduced the power of this study to detect significant relationships. However, the very weak relationship between overall marital adjustment and anxiety symptoms (B=-0.04, SE=0.05) reduces the likelihood that statistically or clinically significant relationships would be found even in a much larger sample. Third, women who participated in this study had been living with a diagnosis of BC for an average of 3 years and were still married. Not included were women whose diagnosis of BC led to marital discord and divorce. Such a selection effect would reduce the variability in anxiety symptoms and marital discord in our sample of married women whose marriages had endured and stabilized over time. The net effect of all these factors would be to lower our ability to detect an adverse effect of the BC diagnosis on anxiety symptoms and MQ.
The inverse relationship between age and anxiety found here has been reported by other researchers in Western countries, including studies in the United States,8 Germany,13 and Australia.11 However, this is the first time that an inverse association has been reported in the Middle East and Far East since the published studies from Iran31 and Thailand20 did not find an association between anxiety and age. There are several reasons why younger women with BC are likely to have higher levels of anxiety. First, the diagnosis of BC at a young age is not “on time” as it might be in later life when cancer is more common and expected. Having one’s life cut short by cancer can interfere with future dreams and hopes for family and work. Second, having BC diagnosed at a young age during the reproductive years can interfere with body image (following mastectomy), female identity, and sexual intimacy, and convey a sense of loss of control that may increase anxiety levels. Younger women may also be less likely to agree to, and comply with hormonal therapies that interfere with their sexual activity,49 and may cause premature menopause,50 increasing anxiety toward the course of the cancer and premature mortality. Finally, the strongest risk factor we identified for anxiety was lower education. Again, this finding is consistent with reports from Western countries, such as Germany13 and Australia,11 although is inconsistent with one of the only studies on anxiety in BC patients in the Middle East, where higher levels of education were associated with more anxiety (Iran).31 Women with lower education may not be aware of the surgical, chemotherapeutic, and radiation therapies available that successfully cure BC or improve its prognosis, or in some instances, may not be able to afford such treatments. Imagining a death sentence with BC, or a poor prognosis when nothing can be done could certainly increase anxiety.
Limitations
We acknowledge several limitations of the present study. First, the sample was a relatively small convenience sample and acquired from only one university-based urban BC clinic, which limits our ability to generalize the study findings to women with BC in rural areas, or those seeking care in other government-supported and private settings. Second, the cross-sectional nature of these analyses precludes speculation regarding the direction of effects in the relationships detected (namely, a hereditary predisposition to anxiety could just as well impair women’s ability to complete their education, as lack of education could lead to greater anxiety). Third, detailed information on cancer stage, severity of disability, or interference with mobility, and the presence of other medical co-morbidities were not assessed, limiting our ability to control for these factors in multivariate analyses. Finally, the way in which anxiety was measured (by a count of symptoms and their severity) did not allow for an assessment of interference with social, occupational, or recreational functioning, precluding our ability to determine the true prevalence of anxiety disorder. Nevertheless, this study also has a number of strengths. First, we used standard psychometrically valid measures to assess anxiety symptoms and MQ, and carefully analyzed the data using stepwise multivariate statistics. Second, the use of the HADS-A to assess anxiety symptoms allows for comparison of our results with past studies, and those to be conducted in the future. Third, to our knowledge, this is the first report from KSA on the prevalence or correlates of anxiety symptoms and the relationship between MQ and anxiety symptoms in married women with BC. Given the important role that religion, cultural, and social forces play in this part of the world,51 these initial preliminary findings should help to stimulate future research on anxiety in women with BC in this country and throughout the Middle East.
In conclusion, anxiety symptoms are present in a significant number of married women with BC being followed up in a university-based BC clinic in Jeddah, KSA, especially those who are younger and with lower education. Although weak trends were found in the expected direction, no significant relationship was found between perceptions of spousal support or quality of the marital relationship and anxiety symptoms. Cultural factors, low power due to sample size, high quality of care, and a selection effect may at least partially explain these findings. Given that between 15% and 25% of women with BC experience significant anxiety symptoms, these findings should stimulate clinicians to screen women with BC for anxiety and other mood symptoms, and then treat significant symptoms with psychotherapy and/or appropriate doses of a serotonin re-uptake inhibitor.
Footnotes
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Abulkhair OA, Al Tahan FM, Young SE, Musaad SM, Jazieh AR. The first national public breast cancer screening program in Saudi Arabia. Ann Saudi Med. 2010;30:350–357. doi: 10.4103/0256-4947.67078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Najjar H, Easson A. Age at diagnosis of breast cancer in Arab nations. Int J Surg. 2010;8:448–452. doi: 10.1016/j.ijsu.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 4.Stanton AL, Bower JE. Psychological Adjustment in Breast Cancer Survivors. Adv Exp Med Biol. 2015;862:231–242. doi: 10.1007/978-3-319-16366-6_15. [DOI] [PubMed] [Google Scholar]
- 5.Silva SM, Crespo C, Canavarro MC. Pathways for psychological adjustment in breast cancer: A longitudinal study on coping strategies and posttraumatic growth. Psychol Health. 2012;27:1323–1341. doi: 10.1080/08870446.2012.676644. [DOI] [PubMed] [Google Scholar]
- 6.Kraemer LM, Stanton AL, Meyerowitz BE, Rowland JH, Ganz PA. A longitudinal examination of couples’ coping strategies as predictors of adjustment to breast cancer. J Fam Psychol. 2011;25:963–972. doi: 10.1037/a0025551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robbins ML, Mehl MR, Smith HL, Weihs KL. Linguistic indicators of patient, couple, and family adjustment following breast cancer. Psychooncology. 2013;22:1501–1508. doi: 10.1002/pon.3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brintzenhofe-Szoc KM, Levin TT, Li Y, Kissane DW, Zabora JR. Mixed anxiety/depression symptoms in a large cancer cohort: prevalence by cancer type. Psychosomatics. 2009;50:383–391. doi: 10.1176/appi.psy.50.4.383. [DOI] [PubMed] [Google Scholar]
- 9.Giese-Davis J, Collie K, Rancourt KM, Neri E, Kraemer HC, Spiegel D. Decrease in depression symptoms is associated with longer survival in patients with metastatic breast cancer: a secondary analysis. J Clin Oncol. 2011;29:413–420. doi: 10.1200/JCO.2010.28.4455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Astin JA, Shapiro J, Shapiro D. Psychological control and morbidity/mortality in breast cancer patients: a 20-year follow-up study. Behav Med. 2013;39:7–10. doi: 10.1080/08964289.2012.708683. [DOI] [PubMed] [Google Scholar]
- 11.Osborne RH, Elsworth GR, Hopper JL. Age-specific norms and determinants of anxiety and depression in 731 women with breast cancer recruited through a population-based cancer registry. Eur J Cancer. 2003;39:755–762. doi: 10.1016/s0959-8049(02)00814-6. [DOI] [PubMed] [Google Scholar]
- 12.Alexander S, Palmer C, Stone PC. Evaluation of screening instruments for depression and anxiety in breast cancer survivors. Breast Cancer Res Treat. 2010;122:573–578. doi: 10.1007/s10549-009-0669-6. [DOI] [PubMed] [Google Scholar]
- 13.Mehnert A, Koch U. Psychological comorbidity and health-related quality of life and its association with awareness, utilization, and need for psychosocial support in a cancer register-based sample of long-term breast cancer survivors. J Psychosom Res. 2008;64:383–391. doi: 10.1016/j.jpsychores.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 14.Zabora J, Brintzenhofe-Szoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 15.Carlson LE, Waller A, Groff SL, Zhong L, Bultz BD. Online screening for distress, the 6th vital sign, in newly diagnosed oncology outpatients: Randomized controlled trial of computerized vs personalized triage. Br J Cancer. 2012;107:617–625. doi: 10.1038/bjc.2012.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 17.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 18.So WK, Marsh G, Ling WM, Leung FY, Lo JC, Yeung M, et al. The symptom cluster of fatigue, pain, anxiety, and depression and the effect on the quality of life of women receiving treatment for breast cancer: a multicenter study. Oncol Nurs Forum. 2009;36:E205–E214. doi: 10.1188/09.ONF.E205-E214. [DOI] [PubMed] [Google Scholar]
- 19.Härtl K, Schennach R, Müller M, Engel J, Reinecker H, Sommer H, et al. Quality of life, anxiety, and oncological factors: a follow-up study of breast cancer patients. Psychosomatics. 2010;51:112–123. doi: 10.1176/appi.psy.51.2.112. [DOI] [PubMed] [Google Scholar]
- 20.Lueboonthavatchai P. Prevalence and psychosocial factors of anxiety and depression in breast cancer patients. J Med Assoc Thai. 2007;90:2164–2174. [PubMed] [Google Scholar]
- 21.Kudel I, Edwards R, Raja S, Heinberg LJ, Haythornwaite J. The association of perceived partner-related social support with self-reported outcomes in women post-mastectomy. J Health Psychol. 2008;13:1030–1039. doi: 10.1177/1359105308097968. [DOI] [PubMed] [Google Scholar]
- 22.Bozo O, Gündogdu E, Büyükasik-Colak C. The moderating role of different sources of perceived social support on the dispositional optimism--posttraumatic growth relationship in postoperative breast cancer patients. J Health Psychol. 2009;14:1009–1020. doi: 10.1177/1359105309342295. [DOI] [PubMed] [Google Scholar]
- 23.Talley A, Molix L, Schlegel RJ, Bettencourt A. The influence of breast cancer survivors’ perceived partner social support and need satisfaction on depressive symptoms: a longitudinal analysis. Psychol Health. 2010;25:433–449. doi: 10.1080/08870440802582682. [DOI] [PubMed] [Google Scholar]
- 24.Hasson-Ohayon I, Goldzweig G, Braun M, Galinsky D. Women with advanced breast cancer and their spouses: diversity of support and psychological distress. Psychooncology. 2010;19:1195–1204. doi: 10.1002/pon.1678. [DOI] [PubMed] [Google Scholar]
- 25.Manne S, Sherman M, Ross S, Ostroff J, Heyman RE, Fox K. Couples’ support-related communication, psychological distress, and relationship satisfaction among women with early stage breast cancer. J Consult Clin Psychol. 2004;72:660–670. doi: 10.1037/0022-006X.72.4.660. [DOI] [PubMed] [Google Scholar]
- 26.Kroenke CH, Michael Y, Tindle H, Gage E, Chlebowski R, Garcia L, et al. Social networks, social support and burden in relationships, and mortality after breast cancer diagnosis. Breast Cancer Res Treat. 2012;133:375–385. doi: 10.1007/s10549-012-1962-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fergus KD, Gray RE. Relationship vulnerabilities during breast cancer: patient and partner perspectives. Psychooncology. 2009;18:1311–1322. doi: 10.1002/pon.1555. [DOI] [PubMed] [Google Scholar]
- 28.Badr H, Carmack CL, Kashy DA, Cristofanilli M, Revenson TA. Dyadic coping in metastatic breast cancer. Health Psychol. 2010;29:169–180. doi: 10.1037/a0018165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Montazeri A, Harirchi I, Vahdani M, Khaleghi F, Jarvandi S, Ebrahimi M, et al. Anxiety and depression in Iranian breast cancer patients before and after diagnosis. Eur J Cancer Care (Engl) 2000;9:151–157. doi: 10.1046/j.1365-2354.2000.00219.x. [DOI] [PubMed] [Google Scholar]
- 30.Hadi N, Asadollahi R, Talei AR. Anxiety, depression and anger in breast cancer patients compared with the general population in Shiraz, Southern Iran. Iranian Red Crescent Medical Journal. 2009;11:312–317. [Google Scholar]
- 31.Montazeri A, Jarvandi S, Haghighat S, Vahdani M, Sajadian A, Ebrahimi M, et al. Anxiety and depression in breast cancer patients before and after participation in a cancer support group. Patient Educ Couns. 2001;45:195–198. doi: 10.1016/s0738-3991(01)00121-5. [DOI] [PubMed] [Google Scholar]
- 32.Vahdaninia M, Omidvari S, Montazeri A. What do predict anxiety and depression in breast cancer patients? A follow-up study. Soc Psychiatry Psychiatr Epidemiol. 2010;45:355–361. doi: 10.1007/s00127-009-0068-7. [DOI] [PubMed] [Google Scholar]
- 33.Karakoyun-Celik O, Gorken I, Sahin S, Orcin E, Alanyali H, Kinay M. Depression and anxiety levels in woman under follow-up for breast cancer: relationship to coping with cancer and quality of life. Med Oncol. 2010;27:108–113. doi: 10.1007/s12032-009-9181-4. [DOI] [PubMed] [Google Scholar]
- 34.El-Hadidy MA, Elnahas W, Hegazy MA, Hafez MT, Refky B, Wahab KM. Psychiatric morbidity among Egyptian breast cancer patients and their partners and its impact on surgical decision-making. Breast Cancer (Dove Med Press) 2012;4:25–32. doi: 10.2147/BCTT.S29890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Al-Rikabi A, Husain S. Increasing prevalence of breast cancer among Saudi patients attending a tertiary referral hospital: a retrospective epidemiologic study. Croat Med J. 2012;53:239–243. doi: 10.3325/cmj.2012.53.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Al-Azri M, Al-Awisi H, Al-Moundhri M. Coping with a diagnosis of breast cancer-literature review and implications for developing countries. Breast J. 2009;15:615–622. doi: 10.1111/j.1524-4741.2009.00812.x. [DOI] [PubMed] [Google Scholar]
- 37.Sherif T, Jehani T, Saadani M, Andejani AW. Adult oncology and chronically ill patients: comparison of depression, anxiety and caregiver’s quality of life. Eastern Mediterr Health J. 2001;7:502–509. [PubMed] [Google Scholar]
- 38.Al-Shahri MZ, Eldali AM, Al-Zahrani O. Nonpain Symptoms of New and Follow-up Cancer Patients Attending a Palliative Care Outpatient Clinic in Saudi Arabia. Indian J Palliat Care. 2012;18:98–102. doi: 10.4103/0973-1075.100822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Al-Amoudi SM, Abduljabbar HS. Men’s knowledge and attitude towards breast cancer in Saudi Arabia. A cross-sectional study. Saudi Med J. 2012;33:547–550. [PubMed] [Google Scholar]
- 40.Gough K, Hudson P. Psychometric properties of the Hospital Anxiety and Depression Scale in family caregivers of palliative care patients. J Pain Symptom Manage. 2009;37:797–806. doi: 10.1016/j.jpainsymman.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 41.el-Rufaie OE, Absood GH. Retesting the validity of the Arabic version of the Hospital Anxiety and Depression (HAD) scale in primary health care. Soc Psychiatry Psychiatr Epidemiol. 1995;30:26–31. doi: 10.1007/BF00784431. [DOI] [PubMed] [Google Scholar]
- 42.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 43.Midlife in the United States. Inter-university Consortium for Political and Social Research ([ICPSR] (1994/1995). Midlife in the United States: A national study of health and well-being, 1994/1995 [data file] [Accessed 2015 March 9]. Available from: www.midus.wisc.edu/data/
- 44.Matzek AE, Cooney TM. Spousal perceptions of marital stress and support among grandparent caregivers: variations by life stage. Int J Aging Hum Dev. 2009;68:109–126. doi: 10.2190/AG.68.2.a. [DOI] [PubMed] [Google Scholar]
- 45.Norton R. Measuring Marital Quality: A Critical Look at the Dependent Variable. Journal of Marriage and Family. 1983;45:141–151. [Google Scholar]
- 46.Heyman RE, Sayers SL, Bellack AS. Global marital satisfaction versus marital adjustment: An empirical comparison of three measures. Journal of Family Psychology. 1994;8:432–446. [Google Scholar]
- 47.Funk JL, Rogge RD. Testing the ruler with item response theory: increasing precision of measurement for relationship satisfaction with the Couples Satisfaction Index. J Fam Psychol. 2007;21:572–583. doi: 10.1037/0893-3200.21.4.572. [DOI] [PubMed] [Google Scholar]
- 48.Fincham FD, Paleari FG, Regalia C. Forgiveness in marriage: The role of relationship quality, attributions, and empathy. Personal Relationships. 2002;9:27–37. [Google Scholar]
- 49.Compas BE, Stoll MF, Thomsen AH, Oppedisano G, Epping-Jordan JE, Krag DN. Adjustment to breast cancer: age-related differences in coping and emotional distress. Breast Cancer Research and Treatment. 1999;54:195–203. doi: 10.1023/a:1006164928474. [DOI] [PubMed] [Google Scholar]
- 50.Ganz PA, Rowland JH, Meyerowitz BE, Desmond KA. Impact of Different Adjuvant Therapy Strategies on Quality of Life in Breast Cancer Survivors. Recent Results in Cancer Research. 1998;152:396–411. doi: 10.1007/978-3-642-45769-2_38. [DOI] [PubMed] [Google Scholar]
- 51.Silbermann M, Hassan EA. Cultural perspectives in cancer care: impact of Islamic traditions and practices in Middle Eastern countries. J Pediatr Hematol Oncol. 2011;33:S81–S86. doi: 10.1097/MPH.0b013e318230dab6. [DOI] [PubMed] [Google Scholar]


