Abstract
OBJECTIVE:
To compare the mental health care US children receive from primary care providers (PCPs) and other mental health care providers.
METHODS:
Using nationally representative data from the Medical Expenditure Panel Survey (MEPS) from 2008 to 2011, we determined whether children and youth aged 2 to 21 years with outpatient visits for mental health problems in the past year saw PCPs, psychiatrists, and/or psychologists/social workers for these conditions. We compared the proportion of children prescribed psychotropic medications by provider type. Using logistic regression, we examined associations of provider type seen and medication prescribing with race/ethnicity, household income, insurance status, geographical area, and language at home.
RESULTS:
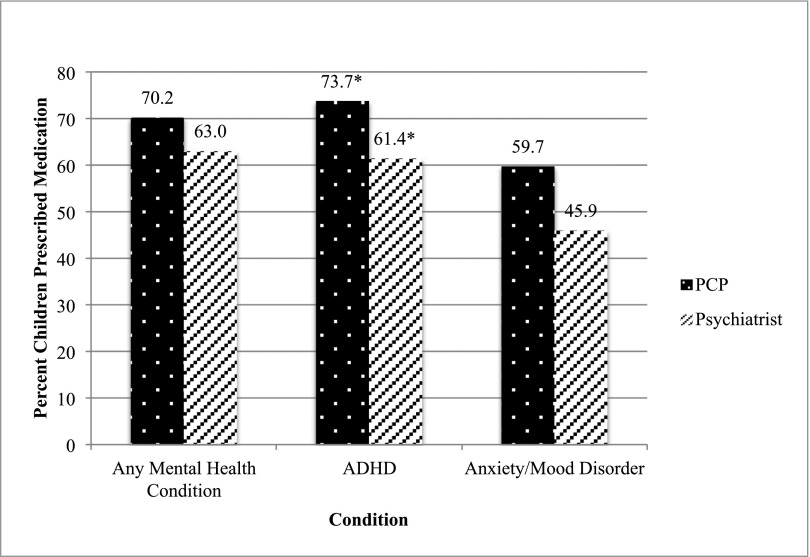
One-third (34.8%) of children receiving outpatient care for mental health conditions saw PCPs only, 26.2% saw psychiatrists only, and 15.2% saw psychologists/social workers only. Nearly a quarter (23.8%) of children saw multiple providers. A greater proportion of children with attention-deficit/hyperactivity disorder (ADHD) versus children with anxiety/mood disorders saw a PCP only (41.8% vs 17.2%). PCPs prescribed medications to a higher percentage of children than did psychiatrists. Children seeing a PCP for ADHD were more likely to receive stimulants or α-agonists than children with ADHD seeing psychiatrists (73.7% vs 61.4%). We found only limited associations of sociodemographic characteristics with provider type or medication use.
CONCLUSIONS:
PCPs appear to be sole physician managers for care of 4 in 10 US children with ADHD, and one-third with mental health conditions overall. Efforts supporting mental health in primary care will reach a substantial portion of children receiving mental health services.
What’s Known on This Subject:
Seven percent of children in the United States receive mental health services each year. There are more pediatric outpatient mental health care visits to primary care physicians (PCPs) than to psychiatrists. Mental health utilization patterns regarding different conditions and medication prescribing are unknown.
What This Study Adds:
One-third of children with mental health conditions see PCPs only. A greater proportion of children with attention-deficit/hyperactivity disorder see PCPs for this than do those with anxiety/mood disorders. Children seeing PCPs are prescribed psychotropic medications more often than those seeing psychiatrists.
Mental health conditions are among the most common chronic childhood illnesses, with 7% of children and youth having a current diagnosis of attention-deficit/hyperactivity disorder (ADHD), 3% having anxiety, and 2% having depression.1 Despite these substantial numbers, fewer than half of US children with mental health conditions receive the care they need.2,3 The American Academy of Pediatrics (AAP) has addressed this gap in services by encouraging primary care providers (PCPs) to take a more active role in preventing, identifying, and managing mental health conditions. The AAP released guidelines on the treatment of ADHD in 2000 and recommended a greater role for primary care for all mental health conditions in 2009, and an expert steering group in 2007 outlined ways PCPs could be involved with adolescents with depression.4–7 These guidelines suggest PCPs ask about mental health issues at all visits; screen for mental health conditions; diagnose and monitor common, mild-to-moderate conditions; provide a treatment plan including psychiatric medications when necessary; and consult with or refer to a mental health specialist in complex cases. The recommendations follow the promotion of psychosocial care and its inclusion in primary care over the past half-century and address the long-standing shortage of mental health professionals for children.8,9
Recent research examined the response in primary care to these recommendations. Numerous studies have addressed PCPs’ perspectives on treating mental health conditions, finding that PCPs are more comfortable managing ADHD than other mental health conditions.10–13 Other studies sought to quantify the pediatric mental health care PCPs undertake by analyzing mental health care visits and suggested that PCPs are the providers at more mental health visits than psychiatrists.14,15 The literature has also explored prescribing patterns of PCPs and psychiatrists, with conflicting results among the studies on which provider type is more likely to prescribe psychotropic medications.14,16,17
Despite attention to this area of research, no studies have yet used a nationally representative sample to characterize the population of children seen or prescribed medications by PCPs versus other types of mental health providers. Previous national studies have analyzed pediatric mental health use at the level of visits (and not children),14 have focused on solely 1 condition,15 or have used only a subset of children and youth (eg, youth in foster care) in their sample.3,18 Knowing nationally which children are treated by PCPs and which children are treated by other providers can help estimate how much PCPs are engaged in mental health care. Such estimates will inform efforts to implement the AAP guidelines and identify areas of potential to expand access to mental health resources in primary care.
This study uses nationally representative US data of children receiving care for mental health conditions, with a focus on ADHD and anxiety/mood disorders. We address 3 main questions: What proportion of US children and adolescents receiving outpatient mental health care attend visits for mental health conditions with PCPs versus other types of mental health providers? Are children seeing PCPs versus psychiatrists more or less likely to be prescribed psychotropic medications? Is the type of provider seen or whether a medication was prescribed associated with a patient’s condition, age, race/ethnicity, household income level, insurance type, geographic area, or primary language at home? As primary care guidelines for ADHD have been available for more than a decade, we hypothesized that children with ADHD would be the most likely to receive care from PCPs, and children with anxiety/mood disorders would more likely receive care exclusively from psychiatrists.
Methods
Sample
This study analyzed data from the Medical Expenditure Panel Survey (MEPS).19 By using a nationally representative sample and panel design, MEPS provides detailed information about medical events on both a person and family level. In a series of interviews, MEPS asks participants to report medical events they have had and follows up with probes to determine visit type, physician type, conditions discussed, and medications prescribed. MEPS then creates different files for different types of data (eg, medications prescribed, demographic information). For this study, the Prescriptions File, Office-Based Visits File, Outpatient Visits File, and Household Full-Year Consolidated File were merged by using common identifiers, and years 2008 to 2011 were combined, providing a sample size of 43 235 children and youth, ages 2 to 21 years. The response rate was 59.3% for 2008, 57.2% for 2009, 53.5% for 2010, and 54.9% for 2011. We chose 2008 as the start year to ensure all years included followed the Food and Drug Administration’s most recent Black Box warning on selective serotonin reuptake inhibitor antidepressants, which has been reported to affect physicians’ prescribing.11,20 We limited the dataset to those children who had an office-based or outpatient visit for a mental health condition. MEPS asks the respondents: “What conditions were discovered or led you to make this visit?” We considered a child to have received care for a mental health condition if he or she had any disorder from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition listed as the answer to this question. We excluded learning and cognitive impairment disorders, as these disorders are usually addressed through school system interventions,21 but included autism spectrum disorders, which MEPS classifies under Pervasive Developmental Disorders. We analyzed ADHD (including conduct and disruptive behavior disorder) and anxiety/mood disorders (including depression and bipolar disorders) separately because of their higher prevalence in pediatric populations, and thus guidelines’ focus on these conditions (see Supplement 1 for International Classification of Diseases, Ninth Revision codes).
Study Variables
Provider Type
We categorized providers at outpatient visits for mental health conditions as PCP, psychiatrist, or psychologist/licensed social worker. We categorized PCP visits as those to family medicine, internists, pediatricians, or other or general practice physicians; we followed the MEPS classifications for provider types and assumed that these providers working in an outpatient or office-based setting saw patients as a PCP. We categorized MEPS participants as having a PCP primarily manage their mental health condition if they solely saw a PCP within a given year for these conditions.
Medications Prescribed
We noted participant reports of psychotropic medication prescription at a mental health visit. The MEPS Prescriptions File contains information on the medications participants reported to have filled in a pharmacy, and we linked prescriptions to the Office-Based and Outpatient Visits Files through a common identifier to determine the medications prescribed at a particular visit. MEPS relies solely on participant report to associate prescriptions with specific visits. We included central nervous system stimulants, selective serotonin reuptake inhibitor/other antidepressants, antipsychotics, α-agonists, and anxiolytics/sedatives (see Supplement 2 for included prescriptions). We assumed medications prescribed at visits were managed by the provider type seen at that visit. Where participants received a medication at visits with both a psychiatrist and a PCP, we assumed management was primarily driven by the psychiatrist and associated this medication with the visit to the psychiatrist.
Independent Variables (for Question 3)
The main independent variables were race/ethnicity (categorized as Hispanic, non-Hispanic black, and non-Hispanic other), participant-reported annual household income (categorized by MEPS as <100% federal poverty line [FPL], 100%–200% FPL, >200%–400% FPL, and >400% FPL), insurance coverage (categorized as any private, any public, and uninsured), region (separated into Northeast, Midwest, South, and West), metropolitan statistical area (MSA) (categorized as non-MSA and MSA), and language spoken at home (categorized as English and Spanish). We chose these variables because of their association with differential access to mental health care and receipt of medications.9,18,22–25
Analyses
All analyses used Stata 13.1 (Stata Corp, College Station, TX) and included the appropriate person-level weights provided by MEPS. We initially determined the proportion of children who had a visit for a mental health condition in the past year generally and within sociodemographic categories. To answer the first study question, we determined whether children saw a PCP, psychiatrist, psychologist/social worker, or multiple provider types for mental health conditions. To answer the second study question, we compared the proportion of children prescribed a psychotropic medication by a PCP versus a psychiatrist. Logistic regression using provider type as the independent variable and medication prescribed as the dependent variable tested for the association between medication prescription and provider type.
To answer the third research question, we created logistic regression models to examine associations between the outcomes of a child’s provider type for mental health care and medication use with the sociodemographic variables previously described. The first model had as its primary dependent variable children who had seen only a PCP in the past year versus children who had seen a psychiatrist in the past year. Our second logistic regression compared children who had a visit for a mental health condition and had been prescribed medication with those who had a visit but did not receive medication. We included race/ethnicity, poverty status, insurance coverage, region, MSA, and language spoken at home in each logistic regression model. We also controlled for age and gender, which are correlated with prevalence of mental health conditions.26 Where relevant, we examined for significant interactions between sociodemographic variables and did not find any.
The study received expedited approval from the Partners Healthcare System’s Institutional Review Board.
Results
Sample
In the years 2008 to 2011, 1778, or a weighted 5.2% of US children and adolescents aged 2 to 21, had an office-based or outpatient visit for a mental health condition, with a mean of 5.4 visits per child with any mental health visits (Table 1). Children in higher-income households had more mental health visits than did those in lower-income homes. Children in the South had higher rates of visits than in other regions. Among mental health conditions, ADHD and anxiety/mood disorders accounted for a large majority of the conditions for which children received care (87.9%) (Table 2).
TABLE 1.
Characteristics of Children Who Had a Visit With a PCP, Psychiatrist, Psychologist, or Social Worker for a Mental Health Condition in the Previous Year
| Children Aged 2–21 Years With a Visit for a Mental Health Condition in the Past Year, n =1778 | ||
|---|---|---|
| Sample Size | Weighted Percent | |
| Gender | ||
| Boys | 1157 | 63.7 |
| Girls | 621 | 36.3 |
| Age | ||
| 2–6 | 163 | 7.7 |
| 7–11 | 605 | 7.8 |
| 12–17 | 718 | 40.2 |
| 18–21 | 292 | 21.3 |
| Race ethnicity | ||
| Hispanic | 372 | 11.1 |
| Non-Hispanic black | 327 | 8.9 |
| Non-Hispanic other | 1079 | 80.0 |
| Household income | ||
| <100% FPL | 530 | 19.8 |
| 100%–<200% FPL | 450 | 18.9 |
| 200%–<400% FPL | 434 | 28.8 |
| ≥400% FPL | 364 | 32.5 |
| Insurance | ||
| Any private | 836 | 63.1 |
| Any public | 875 | 32.8 |
| Uninsured | 67 | 4.1 |
| Region | ||
| Northeast | 281 | 17.2 |
| Midwest | 504 | 29.0 |
| South | 663 | 37.3 |
| West | 330 | 16.5 |
| MSA | ||
| Non-MSA | 264 | 16.8 |
| MSA (>250 000 population) | 1514 | 83.2 |
| Language at home | ||
| English | 1596 | 95.3 |
| Spanish | 164 | 4.0 |
TABLE 2.
Clinical Characteristics of Children With a Mental Health Visit in the Past Year
| Children Aged 2–21 Years With a Visit for a Mental Health Condition in the Past Year, n = 1778 | ||
|---|---|---|
| Sample Size | Weighted Percent | |
| Conditiona | ||
| ADHD | 1212 | 64.7 |
| Anxiety | 287 | 19.0 |
| Mood disorders | 403 | 24.3 |
| Pervasive developmental disorder | 107 | 6.9 |
| Psychoses | 25 | 1.3 |
| Alcohol and substance disorders | 10 | 0.3 |
| Other | 121 | 7.2 |
| Prescriptionsb | ||
| Stimulants | 753 | 47.3 |
| SSRI/other antidepressants | 269 | 21.7 |
| Antipsychotics | 195 | 12.2 |
| α-agonist | 115 | 7.1 |
| Any psychotropic medication | 999 | 66.6 |
SSRI, selective serotonin reuptake inhibitor.
Some children had visits for >1 condition.
b Children may have been prescribed 0, 1, or many medications.
Percentage of Care by Provider Type
Of children who had a visit for any mental health condition, 34.8% saw only a PCP, 26.2% saw only a psychiatrist, and 15.2% saw only a psychologist or social worker (Table 3). Close to half (46.6%) had a PCP involved in their mental health care (ie, at least 1 visit to a PCP). Although nearly one-quarter (23.8%) were managed by >1 provider, 6.7% were managed by both a PCP and psychiatrist. Among children with ADHD, 41.8% had visits with PCPs only, 27.6% had visits with psychiatrists only, and 10.4% had visits with only psychologists or social workers. Among children with anxiety/mood disorders, 17.2% saw only PCPs, 31.3% saw only psychiatrists, and 23.8% saw only psychologists or social workers. Management by >1 type of provider occurred for 20.2% of children with ADHD and 27.7% of children with anxiety/mood disorders. A greater proportion of children with ADHD had a PCP involved in their care than did children with anxiety/mood disorders (52.5% vs 28.1%), whereas children with anxiety/mood disorders more commonly had psychiatrists (53.3% vs 44.0%) and psychologists or social workers (47.7% vs 25.2%) involved in their care than did children with ADHD. Children with comorbid ADHD and anxiety/mood disorders primarily saw psychiatrists and psychologists or social workers.
TABLE 3.
Weighted Proportion of Children Seen by Various Providers and Combination of Providers in the Past Year for Mental Health Conditions in the United States, 2008–2011
| Type of Provider | Summary | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| PCP only | Psychiatrist Only | Psychologist or Social Worker Only | PCP and Psychiatrist | PCP and Psychologist or Social Worker | Psychiatrist and Psychologist or Social Worker | PCP, Psychiatrist, and Psychologist or Social Worker | Any PCP Involvement | Any Psychiatrist Involvement | Any Psychologist or Social Worker Involvement | Management by Multiple Providers | |
| Any mental health condition, n = 1778 | 627 (34.8) | 501 (26.2) | 253 (15.2) | 101 (5.2) | 73 (5.0) | 192 (12.0) | 31 (1.5) | 832 (46.6) | 825 (45.0) | 549 (33.7) | 397 (23.8) |
| ADHD, n = l212a | 499 (41.8) | 350 (27.6) | 123 (10.4) | 74 (5.4) | 41 (3.7) | 102 (9.5) | 23 (1.6) | 637 (52.5) | 549 (44.0) | 289 (25.2) | 240 (20.2) |
| Anxiety/mood disorder, n = 624a | 110 (17.2) | 207 (31.3) | 146 (23.8) | 28 (3.8) | 28 (5.8) | 96 (16.8) | 9 (1.4) | 175 (28.1) | 340 (53.3) | 279 (47.7) | 161 (27.7) |
| ADHD and anxiety/mood disorder, n = 195 | 19 (8.7) | 74 (39.7) | 31 (14.1) | 22 (8.7) | 5 (2.0) | 36 (23.7) | 8 (3.2) | 54 (22.6) | 140 (75.2) | 80 (42.9) | 71 (37.6) |
Values are n (%).
Children could have >1 condition.
Prescribing by Provider Type
Children who had a visit with a PCP were at least as likely or more likely to be prescribed a psychotropic medication than those who saw a psychiatrist: 70.2% vs 63.0% of children for any mental health condition, 73.7% vs 61.4% for ADHD, and 59.7% vs 45.9% for anxiety/mood disorders (Fig 1). Children with ADHD seen by PCPs had 1.5 times the odds of receiving a medication than did children seen by psychiatrists (95% confidence interval [CI] 1.08–2.08).
FIGURE 1.
Percentage of children with a mental health visit prescribed medication in the past year, by provider type. *Significant difference (P = .02) between percent prescribed by provider type. OR 1.49 (1.08–2.08)
Associations of Patterns of Use and Sociodemographic Characteristics
Household income, region, and language at home had some significant associations with type of provider seen, whereas race/ethnicity, MSA, and insurance status had no significant correlations across the conditions and sociodemographic variables considered. Children from families with incomes of 100% to 200% of the FPL or from the South had 3 times the odds of seeing a PCP versus a psychiatrist for anxiety/mood disorders (odds ratio [OR] 2.90, 95% CI 1.29–6.55; OR 2.77, 95% CI 1.08–7.11). Compared with children speaking English at home, those with a household speaking Spanish had increased odds of having their ADHD managed by a PCP (OR 2.50, 95% CI 1.08–5.79).
Associations of Medication Use and Sociodemographic Characteristics
Compared with children with private insurance, uninsured children had lower odds of being medicated for any mental health condition and ADHD specifically (OR 0.36, 95% CI 0.17–0.79; OR 0.37, 95% CI 0.14–0.95). Children living in the West had decreased odds of having a medication for any mental health condition and for anxiety/mood disorders (OR 0.50, 95% CI 0.30–0.83; OR 0.36, 95% CI 0.15–0.90). Considering income, children from families with an income 100% to 200% of the FPL had two-thirds the odds of being prescribed a medication for ADHD (OR 0.62, 95% CI 0.40–0.97). No other significant associations existed between medication prescribing and the sociodemographic variables analyzed.
Discussion
In this analysis of nationally representative data examining outpatient mental health care use among children and youth, we found that 5.2% had a visit in the past year for a mental health condition. We also found that PCPs have a substantial role in pediatric mental health care: 35% of children (42% of children with ADHD) saw only a PCP, and PCPs were involved in the care of nearly half of the children. PCPs and psychiatrists comanaged the conditions of only 6.7% of our sample. PCPs saw more children with ADHD than did psychiatrists or psychologists/social workers but fewer children with anxiety/mood disorders. Children seeing a PCP for ADHD received medications more often than those seeing psychiatrists. Finally, we found that few consistent associations exist between provider type or medication use and race/ethnicity, income level, insurance, region, MSA, and language at home.
Previous studies have reported that ∼7% of school-aged children receive mental health services in a given year,2 making our estimate of 5% comparable, as we included younger children. A recent study examined the proportion of adolescents having lifetime use of services from various mental health sectors with data from 2002 to 2004, and determined that psychiatrists are the most common providers of mental health care for adolescents.3 Our study found PCPs, and not psychiatrists, to be the most common providers for pediatric mental health care, perhaps reflecting a change over time or difference among age groups. Our finding that PCPs provide most care for ADHD and a minority of care for anxiety/mood disorders is consistent with other reports that PCPs are more comfortable treating ADHD.12,27,28 The release of the AAP guidelines on ADHD care several years before those for anxiety and depression, and extensive quality improvement efforts to implement the ADHD guidelines,29–31 help explain the degree of PCP involvement in the care of ADHD. These data support the importance of enhancing PCPs’ capacity for mental health care through collaborative care models, which have been shown to improve mental health outcomes relative to community care,32 as well as other strategies, such as expanding reimbursements beyond face-to-face visits.33
Studies vary on whether children with ADHD who see psychiatrists or PCPs are more likely to be prescribed medications. One study using a regional Medicaid sample suggested children receiving care from PCPs are more likely to be on medications for their ADHD,17 whereas a national study of adolescents concluded that those seeing psychiatrists are more likely to be prescribed these medications.16 The current study adds a perspective on this question by using a national sample of all ages of pediatric patients but provides no information on clinicians’ rationale for medication prescribing. The finding of substantial prescribing by PCPs supports the role of child psychiatry telephone-based access programs,34,35 along with electronic medical record tools that help guide clinicians’ decision-making.36,37
Considering previous literature, the lack of association between provider type seen and medication use and sociodemographic variables is surprising. A study in adult mental health care found a greater disparity in racial and ethnic minorities’ access to psychiatrists compared with other providers,38 and pediatric studies have concluded that disadvantaged groups less frequently see specialists or use prescription medications.25,39–44
This study has some limitations. First, MEPS does not provide information on children with mental health problems who see no one, and services obtained in school, juvenile justice, or child welfare settings are likely undercounted in MEPS.3,45,46 Second, MEPS does not differentiate among types of pediatricians (eg, developmental/behavioral pediatricians and general pediatricians) and psychiatrists (eg, child and adult psychiatrists). Thus, visits to developmental/behavioral pediatricians may be miscategorized as PCP visits. However, only ∼600 board-certified developmental/behavioral pediatricians practice in the United States,47 and they likely see a very small proportion of children with mental health conditions. Further, MEPS categorizes neurologists separately, but some pediatric neurologists, if boarded in both specialties, may be categorized as pediatricians. Third, MEPS data provide no information on condition severity, thus we could not examine severity in these analyses. Medication categories in MEPS may be imperfect; for example, diphenhydramine is included as a sedative. Additionally, we could not tell when providers were actively comanaging patients versus working in relative silos. Likewise, the extent of management by providers and the depth of discussion at PCP visits could not be determined. Although most of the sample had private insurance, it represents the US child population receiving outpatient mental health services. Furthermore, we could not account for insurance-related restrictions to care (eg, narrow provider networks or need for prior authorization). Finally, the potential for recall bias in the reporting of events or prescriptions is intrinsic to the MEPS design.
Conclusions
We examined the involvement of PCPs and other providers in pediatric mental health care among US children and youth. This study suggests PCPs alone care for a greater proportion of children receiving mental health care than do psychiatrists or psychologists/social workers, especially in the treatment of ADHD. However, fewer than half of children had any involvement from their PCP, and comanagement with other mental health specialists, especially psychiatrists, appears uncommon. Further, this study suggests that sociodemographic differences may not limit access to specialist care or medications among children who have already gained access to mental health care, although the findings indicate income and geographic differences in overall mental health care use. Further research regarding timeliness and family satisfaction with this care among various groups should be pursued. Finally, in an effort to assist PCPs in their involvement in pediatric mental health care, further emphasis should be placed on collaborative care models with psychotherapy and programs that provide point-of-care advice to PCPs from mental health experts.
Supplementary Data
Glossary
- AAP
American Academy of Pediatrics
- ADHD
attention-deficit/hyperactivity disorder
- CI
confidence interval
- FPL
federal poverty line
- MEPS
Medical Expenditure Panel Survey
- MSA
Metropolitan Statistical Area
- OR
odds ratio
- PCP
primary care provider
Footnotes
Ms Anderson conceptualized and designed the study, carried out the statistical analyses and interpreted the data, and drafted the initial manuscript; Dr Chen assisted in statistical analysis; Dr Perrin conceptualized and designed the study, and interpreted the data; Dr Van Cleave conceptualized and designed the study, interpreted the data, and supervised the study; and all authors critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
Dr Chen's current affiliations are Center for Surgery and Public Health, Brigham and Women's Hospital, Boston, Massachusetts, and Department of Surgery, Harvard Medical School, Boston, Massachusetts.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Ms Anderson received funding through the American Pediatric Society/Society for Pediatric Research Student Research Program (T35 HD 7446). Drs Van Cleave and Chen were supported by the National Institutes of Health (5K23MH083885–05). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Perou R, Bitsko RH, Blumberg SJ, et al. Centers for Disease Control and Prevention (CDC) . Mental health surveillance among children—United States, 2005–2011. MMWR Surveill Summ. 2013;62(62 suppl 2):1–35 [PubMed] [Google Scholar]
- 2.Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among US children: variation by ethnicity and insurance status. Am J Psychiatry. 2002;159(9):1548–1555 [DOI] [PubMed] [Google Scholar]
- 3.Merikangas KR, He JP, Burstein M, et al. Service utilization for lifetime mental disorders in US adolescents: results of the National Comorbidity Survey-Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2011;50(1):32–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Academy of Pediatrics . Clinical practice guideline: diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. Pediatrics. 2000;105(5):1158–1170 [DOI] [PubMed] [Google Scholar]
- 5.Committee on Psychosocial Aspects of Child and Family Health and Task Force on Mental Health . Policy statement—The future of pediatrics: mental health competencies for pediatric primary care. Pediatrics. 2009;124(1):410–421 [DOI] [PubMed] [Google Scholar]
- 6.Zuckerbrot RA, Cheung AH, Jensen PS, Stein RE, Laraque D, GLAD-PC Steering Group . Guidelines for Adolescent Depression in Primary Care (GLAD-PC): I. Identification, assessment, and initial management. Pediatrics. 2007;120(5). Available at: www.pediatrics.org/cgi/content/full/120/5/e1299 [DOI] [PubMed] [Google Scholar]
- 7.Cheung AH, Zuckerbrot RA, Jensen PS, Ghalib K, Laraque D, Stein RE, GLAD-PC Steering Group . Guidelines for Adolescent Depression in Primary Care (GLAD-PC): II. Treatment and ongoing management. Pediatrics. 2007;120(5). Available at: www.pediatrics.org/cgi/content/full/120/5/e1313 [DOI] [PubMed] [Google Scholar]
- 8.Committee on Psychosocial Aspects of Child and Family Health . American Academy of Pediatrics. The new morbidity revisited: a renewed commitment to the psychosocial aspects of pediatric care. Pediatrics. 2001;108(5):1227–1230 [DOI] [PubMed] [Google Scholar]
- 9.Thomas CR, Holzer CE, III. The continuing shortage of child and adolescent psychiatrists. J Am Acad Child Adolesc Psychiatry. 2006;45(9):1023–1031 [DOI] [PubMed] [Google Scholar]
- 10.Stein RE, Horwitz SM, Storfer-Isser A, Heneghan A, Olson L, Hoagwood KE. Do pediatricians think they are responsible for identification and management of child mental health problems? Results of the AAP periodic survey. Ambul Pediatr. 2008;8(1):11–17 [DOI] [PubMed] [Google Scholar]
- 11.Heneghan A, Garner AS, Storfer-Isser A, Kortepeter K, Stein RE, McCue Horwitz S. Use of selective serotonin reuptake inhibitors by pediatricians: comparing attitudes of primary care pediatricians and child and adolescent psychiatrists. Clin Pediatr (Phila). 2008;47(2):148–154 [DOI] [PubMed] [Google Scholar]
- 12.Radovic A, Farris C, Reynolds K, Reis EC, Miller E, Stein BD. Primary care providers’ initial treatment decisions and antidepressant prescribing for adolescent depression. J Dev Behav Pediatr. 2014;35(1):28–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams J, Klinepeter K, Palmes G, Pulley A, Meschan Foy J. Behavioral health practices in the midst of black box warnings and mental health reform. Clin Pediatr (Phila). 2007;46(5):424–430 [DOI] [PubMed] [Google Scholar]
- 14.Olfson M, Blanco C, Wang S, Laje G, Correll CU. National trends in the mental health care of children, adolescents, and adults by office-based physicians. JAMA Psychiatry. 2014;71(1):81–90 [DOI] [PubMed] [Google Scholar]
- 15.Garfield CF, Dorsey ER, Zhu S, et al. Trends in attention deficit hyperactivity disorder ambulatory diagnosis and medical treatment in the United States, 2000–2010. Acad Pediatr. 2012;12(2):110–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Merikangas KR, He JP, Rapoport J, Vitiello B, Olfson M. Medication use in US youth with mental disorders. JAMA Pediatr. 2013;167(2):141–148 [DOI] [PubMed] [Google Scholar]
- 17.Zima BT, Bussing R, Tang L, et al. Quality of care for childhood attention-deficit/hyperactivity disorder in a managed care medicaid program. J Am Acad Child Adolesc Psychiatry. 2010;49(12):1225–1237, 1237.e1–1237.e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raghavan R, Zima BT, Andersen RM, Leibowitz AA, Schuster MA, Landsverk J. Psychotropic medication use in a national probability sample of children in the child welfare system. J Child Adolesc Psychopharmacol. 2005;15(1):97–106 [DOI] [PubMed] [Google Scholar]
- 19.Agency for Healthcare Research and Quality, US Department of Health and Human Services. Medical Expenditure Panel Survey (MEPS). Available at: www.meps.ahrq.gov. Accessed June 3, 2014
- 20.Nemeroff CB, Kalali A, Keller MB, et al. Impact of publicity concerning pediatric suicidality data on physician practice patterns in the United States. Arch Gen Psychiatry. 2007;64(4):466–472 [DOI] [PubMed] [Google Scholar]
- 21.American Academy of Pediatrics. Committee on Children with Disabilities . The pediatrician’s role in development and implementation of an Individual Education Plan (IEP) and/or an Individual Family Service Plan (IFSP). Pediatrics. 1999;104(1 pt 1):124–127 [DOI] [PubMed] [Google Scholar]
- 22.Lê Cook B, Barry CL, Busch SH. Racial/ethnic disparity trends in children’s mental health care access and expenditures from 2002 to 2007. Health Serv Res. 2013;48(1):129–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bishop TF, Press MJ, Keyhani S, Pincus HA. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Flores G, Tomany-Korman SC. The language spoken at home and disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(6). Available at: www.pediatrics.org/cgi/content/full/121/6/e1703 [DOI] [PubMed]
- 25.Hudson JL, Miller GE, Kirby JB. Explaining racial and ethnic differences in children’s use of stimulant medications. Med Care. 2007;45(11):1068–1075 [DOI] [PubMed] [Google Scholar]
- 26.Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics. 2010;125(1):75–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stein RE, Horwitz SM, Storfer-Isser A, et al. Attention-deficit/hyperactivity disorder: how much responsibility are pediatricians taking? Pediatrics. 2009;123(1):248–255 [DOI] [PubMed] [Google Scholar]
- 28.Williams J, Klinepeter K, Palmes G, Pulley A, Foy JM. Diagnosis and treatment of behavioral health disorders in pediatric practice. Pediatrics. 2004;114(3):601–606 [DOI] [PubMed] [Google Scholar]
- 29.Rushton JL, Fant KE, Clark SJ. Use of practice guidelines in the primary care of children with attention-deficit/hyperactivity disorder. Pediatrics. 2004;114(1). Available at: www.pediatrics.org/cgi/content/full/114/1/e23 [DOI] [PubMed] [Google Scholar]
- 30.Wolraich ML, Bard DE, Stein MT, Rushton JL, O’Connor KG. Pediatricians’ attitudes and practices on ADHD before and after the development of ADHD pediatric practice guidelines. J Atten Disord. 2010;13(6):563–572 [DOI] [PubMed] [Google Scholar]
- 31.Leslie LK, Weckerly J, Plemmons D, Landsverk J, Eastman S. Implementing the American Academy of Pediatrics attention-deficit/hyperactivity disorder diagnostic guidelines in primary care settings. Pediatrics. 2004;114(1):129–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kolko DJ, Campo J, Kilbourne AM, Hart J, Sakolsky D, Wisniewski S. Collaborative care outcomes for pediatric behavioral health problems: a cluster randomized trial. Pediatrics. 2014;133(4). Available at: www.pediatrics.org/cgi/content/full/133/4/e981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sarvet BD, Wegner L. Developing effective child psychiatry collaboration with primary care: leadership and management strategies. Child Adolesc Psychiatr Clin N Am. 2010;19(1):139–148 [DOI] [PubMed] [Google Scholar]
- 34.Sarvet B, Gold J, Bostic JQ, et al. Improving access to mental health care for children: the Massachusetts Child Psychiatry Access Project. Pediatrics. 2010;126(6):1191–1200 [DOI] [PubMed] [Google Scholar]
- 35.Hilt RJ, Romaire MA, McDonell MG, et al. The Partnership Access Line: evaluating a child psychiatry consult program in Washington State. JAMA Pediatr. 2013;167(2):162–168 [DOI] [PubMed] [Google Scholar]
- 36.Co JP, Johnson SA, Poon EG, et al. Electronic health record decision support and quality of care for children with ADHD. Pediatrics. 2010;126(2):239–246 [DOI] [PubMed] [Google Scholar]
- 37.Bell LM, Grundmeier R, Localio R, et al. Electronic health record-based decision support to improve asthma care: a cluster-randomized trial. Pediatrics. 2010;125(4). Available at: www.pediatrics.org/cgi/content/full/125/4/e770 [DOI] [PubMed] [Google Scholar]
- 38.Manseau M, Case BG. Racial-ethnic disparities in outpatient mental health visits to US physicians, 1993–2008. Psychiatr Serv. 2014;65(1):59–67 [DOI] [PubMed] [Google Scholar]
- 39.Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(2). Available at: www.pediatrics.org/cgi/content/full/121/2/e286 [DOI] [PubMed] [Google Scholar]
- 40.Broder-Fingert S, Shui A, Pulcini CD, Kurowski D, Perrin JM. Racial and ethnic differences in subspecialty service use by children with autism. Pediatrics. 2013;132(1):94–100 [DOI] [PubMed] [Google Scholar]
- 41.Zuvekas SH, Vitiello B. Stimulant medication use in children: a 12-year perspective. Am J Psychiatry. 2012;169(2):160–166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stevens J, Harman JS, Kelleher KJ. Race/ethnicity and insurance status as factors associated with ADHD treatment patterns. J Child Adolesc Psychopharmacol. 2005;15(1):88–96 [DOI] [PubMed] [Google Scholar]
- 43.Foster BA, Read D, Bethell C. An analysis of the association between parental acculturation and children’s medication use. Pediatrics. 2009;124(4):1152–1161 [DOI] [PubMed] [Google Scholar]
- 44.Chen AY, Chang RK. Factors associated with prescription drug expenditures among children: an analysis of the Medical Expenditure Panel survey. Pediatrics. 2002;109(5):728–732 [DOI] [PubMed] [Google Scholar]
- 45.Burns BJ, Costello EJ, Angold A, et al. Children’s mental health service use across service sectors. Health Aff (Millwood). 1995;14(3):147–159 [DOI] [PubMed] [Google Scholar]
- 46.Farmer EM, Burns BJ, Phillips SD, Angold A, Costello EJ. Pathways into and through mental health services for children and adolescents. Psychiatr Serv. 2003;54(1):60–66 [DOI] [PubMed] [Google Scholar]
- 47.Adair R, Perrin E, Hubbard C, Savageau JA. Practice parameters and financial factors impacting developmental-behavioral pediatrics. J Dev Behav Pediatr. 2010;31(6):477–484 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.