Abstract
Objectives
This study examined life stage differences in the provision of care to spouses with functional impairment.
Methods
We examined 1218 married adults aged 52 and older from the 2000 wave of the Health and Retirement Study (HRS) who received impairment-related help with at least one activity of daily living. We examined the differential likelihood that spouses serve as primary caregiver and the hours of care provided by spousal primary caregivers by life stage.
Results
We found that late middle-aged care recipients were more likely than their older counterparts to receive the majority of their care from their spouse, but received fewer hours of spousal care, mostly when spouses worked full time. Competing demands of caring for children or parents did not affect the amount of care provided by a spouse.
Discussion
Late middle-aged adults with functional limitations are more likely than older groups to be married and cared for primarily by spouses; however they may be particularly vulnerable to unmet need for care. As the baby boom generation ages, retirement ages increase, and federal safety nets weaken, people with health problems at older ages may soon find themselves in the same caregiving predicament as those in late middle age.
In 2000, approximately 20% of Americans aged 55 to 64 had activity limitations that were caused by chronic conditions (Pastor, Makuc, Reuben, & Xia, 2002). Five percent of this age group, approximately 1.4 millions Americans, reported needing assistance with daily activities as a result of a severe disability (Steinmetz, 2006). The aging of the Baby Boom generation along with recent trends in morbid obesity and resultant chronic conditions ensure an increase in disability among people in late middle age in the near future (McTigue et al., 2006), and recent studies suggest that morbidity and disability prevalence are on the rise among younger groups as well (O'Rand, 2005). Yet despite these trends, there is little information on care arrangements for this growing population of adults—specifically, people who require assistance during the period of late middle age, the ‘transition’ phase between middle age and the elder years, when activity limitations associated with a chronic condition escalate sharply (Pastor et al., 2002).
Despite substantial need, there are reasons to expect that there may be less help available to people in late middle age (i.e, those 50 to 64) who are ‘prematurely’ in need of help compared to their elderly counterparts (young-old (65 to 74) and older-old adults (75 and older)). What little we do know about the care networks of non-elderly persons is that they rely less on formal (i.e., paid or subsidized) care, than older persons (Laplante, Harrington, & Kang, 2002). Their access to Medicare, Medicaid and the safety net of federal and state services established to provide home care, nutrition and transportation services to those in need is limited to those in extreme poverty via Medicaid and to the severely disabled who, if they pass strict eligibility criteria regarding severity, still have a waiting period of two years (Centers for Medicare and Medicaid Services, n.d.; Moon, 1996). Similarly, Medicaid, a government-funded insurance program for the poor and disabled and the primary provider of institutional and community-based long term care services, is only available to individuals in late middle age who meet both strict financial and disability criteria, and benefits vary considerably by state (Iezzoni, 2003). Most middle-aged persons with chronic disease and disabilities do not meet these conditions.
Consequently, persons who require care prior to age 65 rely predominantly on informal care, that is, care provided by family members and friends, most of whom are also working-aged and juggling multiple work and family obligations. More specifically, spouses to adults with care needs in late mid-life are likely to bear the majority of caregiving responsibility since nearly 70% of the general population aged 55 to 64 are married (U.S. Census Bureau, n.d).
Competing obligations may jeopardize the amount of care that spouses can provide to their partners in late mid-life. They are more likely than older spousal caregivers to be dependent on continued employment to finance future retirement, access health insurance, cover living expenses, and fund their children's college education. Further, many spousal caregivers in late middle age may find themselves the sole financial provider of the family since health problems and disability may limit their partners' ability to work. Unlike older spousal caregivers, those in late mid-life are also part of the ‘sandwich generation’, that is, individuals aged 45-64 who have children under 25 living at home and who are also caring for elderly parents (Williams, 2004).
Using data from the 2000 wave of the Health and Retirement Study (HRS), we aimed to investigate life stage differences between the late middle-aged and older populations with functional limitations in both care arrangements and amount of help received by caregiving spouses. To our knowledge it is the first to focus specifically on the particular challenges that couples in late mid-life face when one member requires care.
Who Provides Care
An extensive body of research affirms that families provide the bulk of care to frail elderly persons, with spouses serving as the primary caregiver when available (e.g. Jette, Tennstedt, & Branch, 1992; Kemper, 1988; Stone, Cafferata, & Sangl, 1987; Wolff & Kasper, 2006). Primary caregivers are those caregivers who provide the most care to an individual in need. While specific operationalization varies from study to study, persons are most often designated the primary caregiver either by asking the care recipient directly who helps most, or by comparing the amount of time spent caregiving across all caregivers in a network. Like the more general caregiving literature, most of what we know about spousal caregiving in particular comes from studies on the elder population. A recent study by Wolff and Kasper (2006) using the National Long-term Care Survey and Informal Caregiver Survey provides a comprehensive view of spousal care for individuals 65 and older who received care. The authors found that when present, spouses served as the primary caregivers to their partners, and provided more hours of care on average in a given time period than any other primary caregiver type. Two thirds of spousal primary caregivers to elderly adults were sole caregivers. However, competing demands such as care for dependent children and work obligations were minimal among these spousal caregivers. Less than 5% of spousal primary caregivers to elderly adults had children younger than 15 in the household, and only 8% of these spousal primary caregivers worked for pay. This seems unlikely to be the case for the spousal caregivers for non-elderly adults.
Social support theory would suggest that late middle-aged adults in need of help would rely on family members and friends in a similar order of preference, obligation and/or availability as older adults (Messeri, Silverstein, & Litwak, 1993). In general, the strongest tie between two individuals is the tie between a married couple, followed by the tie between parents and children, siblings, other relatives, and finally non-relatives (Rossi & Rossi, 1991). Though it might be expected that couples in late middle age would be more likely to have children at home to provide for a sick parent while the other parent worked, children and young adults assume caregiving roles only under very specific circumstances and represent only a very small proportion of caregivers overall (Aldridge & Becker, 1999; Fruhauf, Jarrott, & Allen, 2006).
Spouses, therefore, are likely to be the primary caregivers to late middle-aged adults in need, whether they are employed or not. The findings of Wolff and Kasper (2006) paint a positive view of spousal caregiving for elderly adults, with limited obligations interfering with the provision of care. This depiction, as we discuss later, is clearly not representative of the experience of spousal caregivers to care recipients younger than 65.
Competing Family Obligations
Life stage affects spousal availability to provide care in terms of the likelihood of having dependent children or elderly parents to care for in addition to the ailing spouse. As Wolff and Kasper (2006) demonstrated, there were few spousal caregivers to adults aged 65 and older who had children under 15 living in the household. It is estimated that 17% of caregivers (not necessarily spousal caregivers) aged 55 to 64 have children under the age of 18 compared to only 2% of those 65 and older (National Alliance for Caregiving and AARP, 2004). Additionally, younger groups are more likely than older groups to have living parents. According to a recent study, approximately 38% of women aged 55 to 63 have a living parent (Henretta, Grundy, & Harris, 2001). Thus, many women in late middle age are potentially caring for both children and parents simultaneously (Grundy & Henretta, 2006). Whether these additional family obligations have a negative impact on the provision of care to a spouse is unknown.
Employment and Caregiving
There is a large literature that examines the relationship between employment and caregiving (E.g., Dentinger & Clarkberg, 2002; Ettner, 1995a; Henz, 2006; Pavalko & Henderson, 2006). Much of it focuses on the employment status of working-aged adults (primarily women) providing care to elder parents, and when non-elderly disabled persons are included as care recipients the relationship between the caregiver and care recipient is not generally emphasized (Ettner, 1995a, 1995b; Henz, 2006; Pavalko & Artis, 1997; See Dentinger & Clarkberg, 2002 for an exception). The literature indicates that both employment and caregiving suffer from competing demands. The struggle to balance caregiving and work obligations costs families billions of dollars in lost wages each year (Harrington Meyer, 2005; Wakabayashi & Donato, 2005). Conversely, although employment does not necessarily lessen the likelihood of becoming a caregiver to an elderly parent (Pavalko & Artis, 1997), it reduces the amount of care provided compared to those who do not work (Doty, Jackson, & Crown, 1998).
Although some women who provide care to their parents reduce work hours or leave the labor force altogether, spousal caregivers in late middle age may be less likely to consider those options. Private health insurance is the dominant form of health insurance for those younger than 65, and is largely tied to the continued employment (often full time) of a family member, since unsubsidized coverage is prohibitively expensive (Harrington Meyer, 2005). If one spouse is unable to work or to work full time, the other may have no choice but to continue to work full time to secure health insurance for the family. Even if the spouse who requires care does qualify for public insurance, neither Medicare nor Medicaid extends that coverage to the partner or dependents.
Premature exits from the labor force also have a significant negative impact on income security (Harrington Meyer, 1996; Pavalko & Henderson, 2006; Wakabayaski & Donato, 2005). Not only does leaving a job because of illness or caregiving responsibilities reduce the immediate flow of income to meet day-to-day expenses, but the election of early receipt of Social Security benefits prior to the full retirement age permanently reduces the amount an individual is eligible to receive by as much as 30% (Social Security Administration, n.d.). Those younger than 65 must certainly weigh the pros and cons of caregiving against the short and long-term consequences of premature exits from the labor force. With large increases in life expectancy over the latter half of the 20th century, even those 65 to 74 must consider the possibility of living another 15 to 30 years. Finding a balance between provision of adequate amounts of care and present and future household financial security is particularly salient for spousal caregivers in midlife.
In no other caregiver-care recipient dyad is the financial wellbeing and health insurance status of both members so intimately connected as when the caregiver is the spouse. As such, the commitment to and need for employment may differ substantially for a spouse compared to another type of caregiver. Since the option to reduce work hours or leave the work force altogether may not be feasible, and in some instances may be completely untenable, a shortfall in the amount of care provided to a disabled spouse is a likely consequence. To our knowledge, however, no study has specifically addressed the association between employment and hours of care provided to a spouse who requires care prior to eligibility for Medicare and Social Security.
Although we expected that the vast majority of spouses would assume the role of primary caregiver to their partner regardless of life stage, we hypothesized that there would be significant life stage differences among individuals with similar levels of disability and associated need for care in the amount of care provided such that younger care recipients would receive less care from their spouses than older care recipients. We hypothesized that these differences would be explained in large part by life stage differences in labor force participation, and to a lesser extent, by family obligations to other generations. We tested these hypotheses using three life stages: 52 to 64, considered here to be late middle aged; 65 to 74, young old; and 75 and older, older-old. Though late middle-aged adults were of most immediate concern, the young-old adults were considered to be a transitional group, eligible for Medicare, aging services and Social Security benefits, yet still more likely to be working and have other dependents than older-old adults.
Method
Data Source
The HRS is a longitudinal study that began in 1992. In 1998, the HRS was merged with the Assets and Health Dynamics of the Oldest Old (AHEAD) and two new cohorts were added to create a sample representative of the population aged 50 and older (Health and Retirement Study, 2000). We used the 2000 wave in which extensive caregiving information for spousal caregivers was available. Because of this, our youngest group started at 52, not 50.
Samples
Of the 18,149 individuals representative of the civilian non-institutionalized U.S population aged 52 and older in the 2000 HRS, 2259 respondents reported difficulty performing and as a result received assistance with at least one activity of daily living (ADL) or instrumental activity of daily living (IADL). ADLs included walking, dressing, eating, bathing, toileting and getting in and out of bed, and IADLs included managing money, preparing meals, getting groceries, using the telephone, and taking medications. Questions were worded in such a way as to limit any inherent gender bias in responses to IADL questions (see Walker, Pratt, & Eddy, 1995). Of the 2259 who received assistance with one or more ADL or IADL because of their difficulty, 1218 were married at the time of the survey and comprised the analytic sample for this research. All reported statistics were weighted to be representative of the non-institutionalized population aged 52 and older, though reported numbers of cases refer to the unweighted sample.
Measures
Outcomes
We examined two main outcomes. Among the 1218 married respondents who received at least a minimum of care, the first outcome was whether or not their spouse served as their primary caregiver. The second outcome was the number of hours of care those spousal primary caregivers (n=1001) provided in the past month.
Respondents could name multiple caregivers. Six percent of all caregivers were missing a measure of hours of care. This was because the respondent did not provide the number of days per month that the caregiver helped out or did not provide the number of hours per day. To retain cases, we used multiple hot-deck imputation stratifying by life stage and the relationship of the caregiver to the care recipient to impute missing values (Kalton & Kasprqyk, 1986). We then assigned primary caregiver status to the person who provided the most hours of care in the month prior to the survey.
Care recipient characteristics
Life stage, measured here as age groups, was the key characteristic of interest. Though we used age as a proxy for life stage, the two are not entirely interchangeable. Life stage is tied not only to chronological age, but also to societal trends, and so the timing of our data (2000) is important to remember as well. As was previously mentioned, we divided life stage into three groups: those 52 to 64 (38%, SE = 1.9%), 65 to 74 (27%, SE = 1.6%), and 75 and older (36%, SE = 1.5%). They are referred to as late middle age, young old, and older old throughout.
We included as controls a number of care recipient characteristics that differ by age and are also associated with the receipt of care and thus potential confounders of the relationship of life stage and community based care. They were gender (Allen, 1994; Katz, Kabeto, & Langa, 2000), race/ethnicity (Stommel, Given, & Given, 1998; Wallace, Levy-Storms, Kington, & Andersen, 1998), education (Desai, Lentzner, & Weeks, 2001), enrollment in Medicaid, current work status, income, and several measures of disease and morbidity.
Similar to the technique used in Katz, Kabeto, and Langa (2000), total household income was used as a five-category variable that divided the total household income for the entire HRS sample into quintiles. Functional impairment was measured by counts of the number of ADLs (range 0-6) and IADLs (range 0-5) the care recipient reported difficulty performing, and cognitive impairment was a dichotomous indicator defined by a rating given by the interviewer as the reason for a proxied interview.
Use of a wheelchair was controlled, because the use of more complex assistive devices such as wheelchairs (compared to canes) is a function of disability severity (Allen, Foster & Berg, 2001). Other measures to further control for severity were: the number of nights a respondent spent in the hospital in the two years prior to the survey, and the number of times in the month prior to the interview that the respondent spent more than half of the day in bed because of a health problem. Finally, we controlled the number of medical conditions, including heart condition, diabetes, stroke, lung disease, cancer, arthritis, high blood pressure, and psychiatric disorder, a measure which served as a further measure of comorbidity (Wallace & Herzog, 1995).
Spousal characteristics
The HRS is unique because in households with a married or partnered couple, detailed information was collected from both individuals. This allowed us to control for a number of spousal characteristics that may make it easier or more difficult for a spouse to provide care. We included measures of ADL and IADL difficulties, current work status (not working, fewer than 20 hours, 20-39 hours, 40 or more hours per week), whether or not the spouse was currently caring for dependent children or elderly parents, and whether or not the spouse was the sole caregiver.
Analytic Plan
We conducted bivariate analyses comparing care recipient and spousal characteristics by life stage. The likelihood of a person serving as the primary caregiver to his or her spouse was modeled using multivariate logistic regression. Ordinary least squares regression was used to model logged hours of care from the primary caregiver for the subset of 1001 care recipients whose spouse served as primary caregiver in the month prior to the survey. Variables were entered in blocks to determine whether age differences in care were explained by particular care recipient and spousal characteristics. Model 1 included life stage and controlled for care recipient sociodemographic and indicators of disease and morbidity. Model 2 added spousal gender and functional status characteristics. Model 3 added in addition spousal competing demands. All descriptive statistics and multivariate analyses were conducted using survey procedures within Stata to adjust for the complex sampling design (Statacorp, 2003, 2005).
Results
care Recipient Characteristics by Life Stage
Table 1 presents care recipient characteristics stratified by life stage. Respondents in late middle age consisted of fewer men and more minorities than the younger-old and older-old groups. Compared to the older groups, they were also better educated, had higher household incomes, and were somewhat more likely to be currently working than older persons receiving care.
Table 1. Characteristics by Life Stage for Married Care Recipients Who Receive Care for at Least 1 ADL/IADL.
| Late Middle-Aged | Young-Old | Older-Old | |
|---|---|---|---|
| (52 to 64) | (65 to 74) | (75 and older) | |
| % | % | % | |
| N | 418 | 355 | 445 |
| Male | 48.70 | 52.42 | 55.68 |
| Race/Ethnicity | |||
| non-Hispanic White | 75.11 | 75.91 | 83.40 |
| non-Hispanic Black | 12.43 | 13.20 | 9.49 |
| Hispanic | 10.86 | 8.28 | 6.42 |
| Other race/ethnicity | 1.60 | 2.61 | 0.69 |
| Education | |||
| Less than high school | 33.52 | 42.67 | 44.93 |
| High school | 34.70 | 30.59 | 31.36 |
| More than high school | 31.78 | 26.75 | 23.71 |
| Receives Medicaid | 12.07 | 16.42 | 8.85 |
| Currently works for pay | 17.91 | 4.66 | 3.17 |
| Household Income | |||
| Bottom quintile | 19.33 | 17.98 | 44.93 |
| 2nd quintile | 16.44 | 37.88 | 31.36 |
| 3rd quintile | 20.02 | 20.20 | 23.71 |
| 4th quintile | 23.55 | 14.83 | 8.85 |
| 5th quintile | 20.67 | 9.11 | 3.17 |
| ADL difficulties, m (se) | 1.82 (.09) | 1.91 (.10) | 1.68 (.12) |
| IADL difficulties, m (se) | 1.45 (.06) | 1.69 (.10) | 2.02 (.09) |
| Hospitalizations in past 2 years, m (se) | 5.74 (.74) | 7.30 (.83) | 6.84 (1.57) |
| Bed days in past month, m (se) | 4.24 (.46) | 4.33 (.52) | 3.25 (.46) |
| Medical conditions, m (se) | 2.72 (.08) | 2.92 (.10) | 2.85 (.08) |
| Uses a wheelchair | 8.68 | 12.93 | 12.31 |
| Has cognitive impairment | 8.20 | 16.18 | 22.66 |
They did not appear to be healthier, however. Respondents in all life stages had similar levels of ADL difficulties, days spent in the hospital in the two years prior to the survey, medical conditions, and wheelchair use. Late middle-aged adults actually spent more days in bed because of health problems compared to their older counterparts, but reported fewer IADL difficulties and less cognitive impairment.
Spouse Characteristics by Care Recipient Life Stage
Spouse characteristics are presented in Table 2. By and large and regardless of life stage, when a spouse provided care, he or she served as the primary caregiver to the individual in need. However, a substantial minority of spouses did not provide any care to their loved one; 12.6% of late middle-aged adults, 16.0% of young-old adults and 18.7% of older-old adults received most of their care from someone other than their spouse. The remainder of Table 2 highlights life stage differences in select characteristics that may influence the amount of care that a spouse provides.
Table 2. Characteristics of Spouses and Care Network by Care Recipient Life Stage.
| Late Middle-Aged | Young-Old | Older-Old | |
|---|---|---|---|
| (52 to 64) | (65 to 74) | (75 and older) | |
| % | % | % | |
| N | 418 | 355 | 445 |
| Caregiving Status | |||
| Primary caregiver to spouse | 87.40 | 84.04 | 81.18 |
| Caregiver, but not primary | 3.31 | 4.37 | 4.64 |
| Does not help | 9.28 | 11.59 | 14.18 |
| Male | 51.36 | 47.58 | 41.32 |
| ADL difficulties, m (se) | .34 (.04) | .56 (.08) | .67 (.08) |
| IADL difficulties, m (se) | .21 (.03) | .40 (.06) | .61 (.10) |
| Receives help for own limitations | 8.36 | 18.08 | 23.47 |
| Cares for children or parents | 37.28 | 10.64 | 1.75 |
| Work status | |||
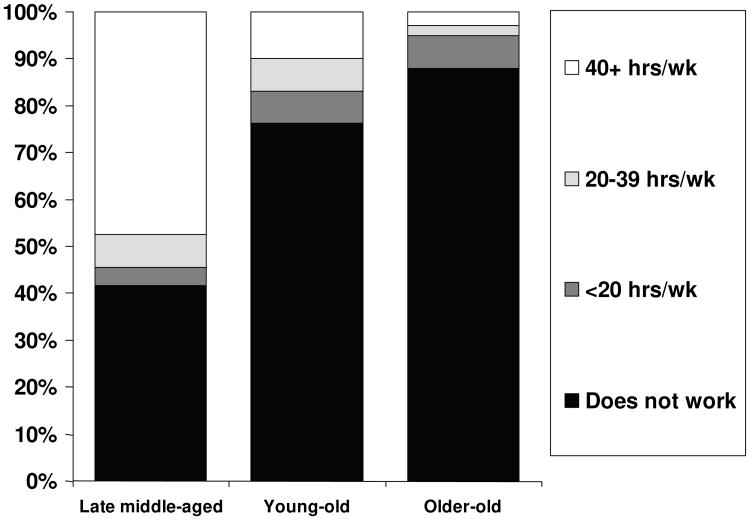
| Does not work | 43.83 | 80.18 | 89.76 |
| Less than 20 hours per week | 4.16 | 6.03 | 6.06 |
| 20 to 39 hours per week | 6.84 | 5.50 | 1.94 |
| 40 or more hours per week | 45.18 | 8.29 | 2.24 |
| More than one helper in network | 23.89 | 25.21 | 25.37 |
| Among spousal primary caregiver | |||
| Hours of help in past month | 97.47 | 149.70 | 182.50 |
The percentage of spouses who were male decreased with life stage. Functional limitations (ADL and IADL difficulties) among spouses increased significantly with life stage, as did the percent of spouses who received help for their own functional limitations. Younger spouses were more likely to have caregiving responsibilities for dependent children or elderly parents, and they were much more likely to be working at least 40 hours per week at the time of the survey than their older counterparts. Finally, among those who served as primary caregivers, spouses of those in late middle age provided many fewer hours of care to their partner compared to the young-old and older-old groups (about 3 hours per day, assuming a 30 day month, compared with 6 hours for the oldest-old group).
Multivariate Analyses
Likelihood of Spouse as Primary Caregiver
There were 1218 eligible married care recipients who received help with at least one ADL/IADL in the month prior to the survey. Results of the logistic regression analyses examining the likelihood of a spouse becoming the primary caregiver to a husband or wife are presented in Table 3.
Table 3. Logistic Regression of Likelihood of Spouse Serving as Primary Caregiver to Those Who Report Receiving Help with at Least 1 ADL/IADL in Month Prior to the Surveya.
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| B | SE B | B | SE B | B | SE B | |
| Age (ref: 75+) | ||||||
| 52 to 64 | .58* | .22 | .17 | .24 | .11 | .28 |
| 65 to 74 | .34 | .26 | .03 | .27 | .02 | .27 |
| Spousal Characteristics | ||||||
| Male | -1.07*** | .21 | -1.06*** | .21 | ||
| # ADL difficulties | -.10 | .08 | -.10 | .08 | ||
| # IADL difficulties | -.71*** | .12 | -0.71*** | .12 | ||
| Receives help for own limitations | -.57 | .33 | -.57 | .33 | ||
| Cares for children or parents | .17 | .31 | ||||
| Work Status (ref: Not working) | ||||||
| Less than 20 hours per week | .33 | .49 | ||||
| 20 to 39 hours per week | .20 | .65 | ||||
| 40 or more hours per week | .03 | .43 | ||||
| Constant | 2.23 | 3.62 | 2.53*** | |||
| F | 5.77 | 10.02 | 8.96 | |||
| d.f. | 20,34 | 24,29 | 26,27 | |||
N= 1173. Models also controlled for care recipient disease and morbidity (# ADL difficulties, # IADL difficulties, use of wheelchair, bed days in past month, hospitalizations in past two years, # medical conditions, cognitive impairment) and sociodemographic characteristics (education, income, race and ethnicity, currently working, receipt of Medicaid). Models are weighted.
p < = .05.
p < = .01.
p < = .001.
As Model 1 indicates, when care recipient sociodemographic, disease, and morbidity characteristics were controlled, spouses of late middle-aged adults were actually more likely to assume the role of primary caregiver than spouses of older-old adults. Model 2 additionally controlled for the spouse's gender and functional status. Both men and individuals with greater IADL difficulties were less likely to serve as primary caregivers to their spouses. The life stage difference in likelihood of a spouse being primary caregiver to the care recipient shown in Model 1 was explained by these variables. Model 3 included competing demands on the spouse's time including caring for other dependents or elderly parents and current work status. Neither of these significantly affected the likelihood of acting as primary caregiver to a spouse.
Hours of Care Provided by Spousal Primary Caregiver
Among those whose spouse served as primary caregiver, the next set of analyses examined hours of care provided by the spouse in the month prior to the survey. There were 1001 eligible individuals whose spouse served as primary caregiver. Model 1 in Table 4 presents multivariate results of the log hours of care that spouses provide as primary caregivers controlling for care recipient sociodemographic, disease, and morbidity characteristics. We can interpret coefficients derived from a log-transformed dependent variable as 100*(beta) = percent change in Y given a unit increase in X. With this in mind, spousal primary caregivers to late middle-aged adults provided 23% fewer hours of care to their partners than did spousal primary caregivers to older-old adults, but spousal primary caregivers to young-old adults did not differ from those to older-old adults in the amount of care they provided. The difference between the late middle-aged and the young-old groups was also significant (not shown).
Table 4. OLS Regression of Log Hours of Care Provided in Past Month by the Spousal Primary Caregivera.
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| B | SE B | B | SE B | B | SE B | |
| Age (ref: 75+) | ||||||
| 52 to 64 | -.23* | .11 | -.30* | .12 | -.08 | .12 |
| 65 to 74 | .00 | .14 | -.01 | .13 | .04 | .13 |
| Spouse Characteristics | ||||||
| Male | .25* | .09 | .20* | .09 | ||
| Has secondary caregivers | .47 *** | .14 | .48 *** | .14 | ||
| # ADL difficulties | .13 * | .05 | .11 * | .05 | ||
| # IADL difficulties | -.31* | .12 | -.32* | .13 | ||
| Receives help for own limitations | .02 | .21 | .00 | .22 | ||
| Cares for children or parents | -.05 | .13 | ||||
| Work Status (ref: Not working) | ||||||
| Less than 20 hours per week | -.14 | .16 | ||||
| 20 to 39 hours per week | -.20 | .18 | ||||
| 40 or more hours per week | -.51*** | .15 | ||||
| Constant | 2.62*** | .23 | 2.84*** | .23 | 2.81*** | .23 |
| R2 | .30 | .34 | .35 | |||
| F | 24.65 | 27.23 | 26.53 | |||
| d.f. | 20,34 | 25,29 | 26,27 | |||
N=969. Models also controlled for care recipient disease and morbidity (# ADL difficulties, # IADL difficulties, use of wheelchair, bed days in past month, hospitalizations in past two years, # medical conditions, cognitive impairment) and sociodemographic characteristics (education, income, race and ethnicity, currently working, receipt of Medicaid). Models are weighted.
p < = .05.
p < = .01.
p < = .001.
Models 2 and 3 in Table 4 examined changes in the life stage effect upon adding spousal characteristics. Controlling for caregiver gender, functional status, the presence of secondary helpers, and the receipt of help for the spouse's own functional limitations, the life stage difference in hours of care provided by spouses of late middle-aged adults compared to older-old adults increased from 23% to 30%.
In addition to modifying the life stage effect, all but one of the spouse characteristics also directly affected the outcome. Men who served as primary caregivers to their spouses provided 25% more hours of care to their wives than women who served as primary caregivers to their husbands. Primary caregivers with secondary helpers provided 47% more help to their spouses than those without secondary helpers. Finally spousal primary caregivers with IADL limitations provided fewer hours of care to their significant others compared to those without IADL limitations, but those with ADL limitations provided more hours of care compared to those without.
When the competing demands of caring for children or parents and employment were added to the model, all life stage differences in hours of care provided were eliminated (see Model 3). Current work status drove the findings. Those who were working at least full time provided 51% fewer hours of care to their spouses than those who were not currently working. Among spousal primary caregivers to late middle-aged adults, nearly 50% worked full time or greater (47%), compared to only 9% of spousal primary caregivers to young-old adults and only 3% of spousal primary caregivers to older-old adults (see Figure 1). Caring for dependent children or parents did not affect the hours of care provided by spousal caregivers.
Figure 1. Work Status of Spousal Primary Caregivers by Respondent Life Stage.
Discussion
Life Stage Differences in Spousal Caregiving
The purpose of this study was to examine life stage differences in spousal caregiving for married persons aged 50 and older who received help with daily living activities. We found that more than 80% of spouses in each age group served as primary caregivers to their husbands or wives and the majority did so without any additional help. However, spouses who served as primary caregivers to late middle-aged adults provided significantly fewer hours of care compared to their older counterparts after controlling for care recipient needs and select caregiver characteristics. These life stage differences disappeared after controlling for the caregiver's work status. Although part-time work status was not associated with fewer hours of care, those who worked full time provide fully 50% fewer hours of care to their spouses than those who did not work.
Close to half of spousal primary caregivers to late middle-aged adults in our study worked 40 hours or more per week. This is in stark contrast to the 9% of spousal primary caregivers to young-old adults and 3% of spousal primary caregivers to older-old adults who did so. Although no other study has examined the effect of work status on care hours provided by spouses specifically, our findings are consistent with Doty and colleagues (1998) who examined women of working age. Further, they indicate that the problem of balancing work and caregiving responsibilities is particularly salient for spousal caregivers in late mid-life who may be struggling to maintain health insurance and financial stability amidst caring adequately for their partner.
Some have speculated that a caregiver may work full time or more hours in order to earn enough money to pay for formal care for their relatives in need (Soldo & Hill, 1995). At least for spouses of late middle-aged adults in our study, this does not appear to be the case, as fewer than 2% of respondents with spousal primary caregivers who worked full time received any formal care at all in this study (results not shown).
More likely, spousal caregivers to late middle-aged adults at least partly work out of necessity. They are younger than the traditional retirement age, and if they have health insurance, it is likely to be employee-based health insurance (Weissman & Epstein, 1994). They are too young to qualify for Medicare, and even if their spouse requiring care meets the strict healthcare cost and income criteria for Medicaid eligibility, insurance coverage does not extend to themselves and dependent children (Ho et al., 2005).
The deficit in care provided by spouses who worked full time is disturbing since prior research had demonstrated an association between reduced hours of care and increased risk for unmet need (Laplante et al, 2004). Unmet need for care in the community is associated with a number of negative consequences including burns and falls (Laplante et al., 2004; Allen & Mor, 1997). While further research is needed to determine whether fewer hours of care result in unmet need for late middle-aged adults or whether these caregivers are simply more efficient at providing care, prior to these analyses the vulnerability of this particular group may have easily been overlooked given the presence of a spouse in their network.
Other family obligations to children and elderly parents did not affect the amount of care given to a spouse. It is likely that the time obligations to other family members are more flexible than the time obligations of employment. Perhaps it is the time given to children or parents that is reduced when care is provided to a spouse rather than the reverse. Or perhaps spousal caregivers reduce time spent in other activities in order to care for all family in need. The explanation of our present finding is beyond the scope of this study, but deserves further attention.
Caregiver Gender
In addition to the results focusing on life stage difference in care hours, we also found other results that deserve more research. Life stage differences in the likelihood of receiving any spousal care are explained largely by the gender and functional status of the spouse. Specifically, men of all life stages are less likely to serve as primary caregivers to their wives and they make up a greater proportion of caregivers to late middle-aged adults than older groups. The finding that men are less likely to serve as primary caregiver than women is widely supported in the literature (e.g., Allen, Goldscheider, & Ciambrone, 1999; Stone et al., 1987; Walker, Pratt, & Eddy, 1995).
We also found that men who serve as primary caregivers to their spouses provide more hours of care than female primary caregivers, which is in contrast to a recent meta-analysis reporting that women typically provide more care than men (Pinquart and Sorensen, 2006). However, the current study is confined to care recipients' spousal caregivers only, not men as a whole, limiting the comparability of the two findings. The husbands in this study may be the exception to the rule among husbands in general by serving as primary caregivers in the first place. An alternative explanation is suggested by the recent work of Calasanti and King (2007), who stress the importance of considering gendered roles and social context when discussing differences in caregiving by gender. From this perspective, it may be that typical household work is considered to be “caregiving” when performed by husbands whose wives have performed these activities prior to their impairment, while only those “new” tasks specifically related to husbands' impairment are considered in time estimates when wives provide care (Dwyer & Seccombe, 1991). Thus, the context or frame of reference in which care recipients estimate hours of spousal care may be quite different by caregiver gender.
Other Influences on Spousal Care
Additionally, we found that primary caregivers with secondary helpers provide 47% more help to their spouses than those without secondary helpers, suggesting that secondary helpers do not act as a substitute for the primary caregiver to ease their burden, but serve to supplement their support because the needs of the care recipient are so great. Finally, we found that spousal primary caregivers with IADL limitations provide fewer hours of care to their significant others compared to those without IADL limitations, but those with ADL limitations provide more hours of care compared to those without. This is likely because when all else is held equal, a caregiver with an ADL limitation may take longer to perform a caregiving task than a person who does not have an ADL limitation or may be homebound and less likely to engage in non-caregiving activities.
Limitations and Future Research
Because this study is cross-sectional, we cannot make causal inferences about the relationship between work status, caregiving, and health insurance status. Longitudinal studies would provide better evidence of causality. Further research is also warranted to determine whether reduced hours of care to late middle-aged adults is associated with increases in unmet need compared to older groups. It is conceivable that although our study controls for rich measures of disease and morbidity, we fail to capture real differences in frailty between the younger groups and the older groups. Perhaps late middle-aged adults with self care needs are more able to assist in their own care (e.g., balance more of their own weight in transferring from bed to chair) and in doing so reduce the actual amount of time it takes to help care for them effectively compared to their elderly counterparts. This has yet to be determined.
Despite these limitations and the need for further research, this study makes important contributions to the literature. To date, no study has focused on the specific dynamics of caregiving and competing responsibilities for spousal caregivers, particularly in mid-life. Because of their life stage, late middle-aged adults with functional limitations are more likely than older groups to be married and cared for primarily by a spouse and this study showed that they may be particularly vulnerable to unmet need for care.
A Look Toward the Future
As the baby boom generation continues to move into late middle age and the elder years, it is likely to become increasingly difficult for family members to successfully combine the responsibilities of caregiving and labor force participation. Trends in obesity and morbidity, caregiving network characteristics, and labor force participation suggest that this concern will only intensify and carry over into older life stages. Persons in late middle age are increasingly obese and likely to suffer functional limitations as a result (Sturm, Ringel, & Andreyeva, 2006). At the same time, informal caregivers are increasingly taking on the full burden of caregiving responsibilities and receiving little help from others (Wolff & Kasper, 2006). Labor force participation is projected to increase among those in late middle age in the coming decade, and potentially double among those 65 and older (Toossi, 2005).
To complicate matters, both Social Security and the Medicare program face financial challenges that threaten their staying power without substantial reforms (Hudson, 2005). Both increased life expectancies and the size of the Baby Boom generation will put an unprecedented strain on the Social Security system in the coming decades. Potential reforms include increasing taxes to pay for benefits, decreasing benefits, increasing the age at which a person is eligible to receive benefits, and partial privatization (Herd & Kingson, 2005). Similarly, skyrocketing costs of the Medicare program, similar to health care costs in general, have also led to discussions about reforms (Moon, 2005). Like those for Social Security, potential reforms under discussion include age increases in eligibility, reductions in benefits, and higher cost sharing with the beneficiary. Any of these reforms will likely have an effect on one's flexibility to juggle work responsibilities and caregiving at any age. Respondents in our study aged 65-74 (“young-old”) did not show the same reduction in care hours because of work status as caregivers of respondents in late middle-age since the majority of those who still worked did so on a part-time basis. As retirement ages continue to climb and federal safety nets weaken, people with care needs who are “young-old” may soon find themselves in the same caregiving predicament as those who are in late middle age.
Conclusions
Clearly, chronological age is not a good predictor of vulnerability to illness and disability (O'Rand, 2005). Though it has taken a backseat to other strategies in recent years, universal health insurance that recognizes vulnerability at all stages of life must seriously be considered. So too must caregiver support services for family members with competing obligations in mid-life, as well as for older caregivers whose own health may be compromised by the demands of providing care to a disabled spouse (Ho et al., 2005). Otherwise, the benefits of medical advances that have reduced mortality from chronic diseases and injury may be diminished by poorer quality of life among people with disability and their families, at least among those without sufficient resources to purchase the care they need.
Acknowledgments
This study was funded in part by a Demography Fellowship from the National Institute for Child Health and Human Development (NICHD). Portions of these analyses were previously presented at the 2006 Gerontological Society of America Annual Meeting. We thank the anonymous reviewers whose suggestions both strengthened this manuscript and provided us with new ideas for future work.
Footnotes
Author Contributions: J.C. Lima planned the study, conducted the statistical analyses, and wrote the manuscript. S. M. Allen supervised and helped frame the study, oversaw the analyses, and contributed substantially to the writing of the manuscript. F. Goldscheider provided guidance with the conceptualization of the study, and edited this and earlier versions of the manuscript. O. Intrator provided guidance with the statistical analyses, suggesting imputation techniques and sensitivity analyses to strengthen the methods and confirm the results.
References
- Aldridge J, Becker S. Children as carers: The impact of parental illness and disability on children's caring roles. Journal of Family Therapy. 1999;21:303–320. [Google Scholar]
- Allen SM, Mor V. The prevalence and consequences of unmet need: Contrasts between older and younger adults with disability. Medical Care. 1997;35:1132–1148. doi: 10.1097/00005650-199711000-00005. [DOI] [PubMed] [Google Scholar]
- Allen SM, Goldscheider F, Ciambrone DA. Gender roles, marital intimacy, and nomination of spouse as primary caregiver. The Gerontologist. 1999;39:150–158. doi: 10.1093/geront/39.2.150. [DOI] [PubMed] [Google Scholar]
- Allen SM, Foster A, Berg K. Receiving help at home: The interplay of human and technological assistance. Journal of Gerontology: Social Sciences. 2001;56B:S374–S382. doi: 10.1093/geronb/56.6.s374. [DOI] [PubMed] [Google Scholar]
- Allen SM. Gender differences in spousal caregiving and unmet need for care. Journal of Gerontology: Social Sciences. 1994;49:S187–S195. doi: 10.1093/geronj/49.4.s187. [DOI] [PubMed] [Google Scholar]
- Calasanti T, King N. Taking ‘women's work’ ‘like a man’: Husbands' experiences of care work. The Gerontologist. 2007;47:516–527. doi: 10.1093/geront/47.4.516. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services (n.d.) Medicare Eligibility Criteria. Retrieved January 15, 2004 from www.medicare.gov/MedicareEligibility/Home.asp?dest=NAV|Home|GeneralEnrollment#TabTop.
- Dentinger E, Clarkberg M. Informal caregiving and retirement timing among men and women: Gender and caregiving relationships. Journal of Family Issues. 2002;23:857–879. [Google Scholar]
- Desai MM, Lentzner H, Weeks JD. Unmet need for personal assistance with activities of daily living among older adults. Gerontologist. 2001;41:82–88. doi: 10.1093/geront/41.1.82. [DOI] [PubMed] [Google Scholar]
- Doty P, Jackson ME, Crown W. The impact of female caregivers' employment status on patterns of formal and informal eldercare. Gerontologist. 1998;38:331–341. doi: 10.1093/geront/38.3.331. [DOI] [PubMed] [Google Scholar]
- Dwyer JW, Seccombe K. Elder care as family labor: the influence of gender and family position. Journal of Family Issues. 1991;12:229–247. [Google Scholar]
- Ettner SL. The opportunity costs of elder care. Journal of Human Resources. 1995a;31:189–205. [Google Scholar]
- Ettner SL. The impact of parent care on female labor supply decisions. Demography. 1995b;32:63–80. [PubMed] [Google Scholar]
- Fruhauf CA, Jarrott SE, Allen KR. Grandchildren's perceptions of caring for grandparents. Journal of Family Issues. 2006;27:887–911. [Google Scholar]
- Grundy E, Henretta J. Between elderly parents and adult children: A new look at the intergenerational care provided by the ‘sandwich generation’. Ageing and Society. 2006;26:707–722. [Google Scholar]
- Harrington Meyer M. Making claims as workers or wives: The distribution of social security benefits. American Sociological Review. 1996;61:449–465. [Google Scholar]
- Harrington Meyer M. Decreasing welfare, increasing old age inequality: Whose responsibility is it? In: Hudson RB, editor. The New Politics of Old Age Policy. Baltimore: Johns Hopkins University Press; 2005. pp. 65–89. [Google Scholar]
- Health and Retirement Study. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740) Ann Arbor, MI: 2000. public use dataset. Core. [Google Scholar]
- Henretta JC, Grundy E, Harris S. Socioeconomic differences in having living parents and children: A U.S.-British Comparison of Middle-Aged Women. Journal of Marriage and Family. 2001;63:852–867. [Google Scholar]
- Henz U. Informal caregiving at working age: Effects of job characteristics and family configuration. Journal of Marriage and Family. 2006;68:411–429. [Google Scholar]
- Herd P, Kingson ER. Reframing Social Security: Cures worse than the disease. In: Hudson RB, editor. The New Politics of Old Age Policy. Baltimore: Johns Hopkins University Press; 2005. pp. 183–204. [Google Scholar]
- Ho A, Collins SR, Davis K, Doty MM. A Look at Working-Age Caregivers' Roles, Health Concerns, and Need for Support. The Commonwealth Fund; 2005. Aug, [PubMed] [Google Scholar]
- Hudson RB. Contemporary challenges to age-based public policy. In: Hudson RB, editor. The New Politics of Old Age Policy. Baltimore: Johns Hopkins University Press; 2005. pp. 1–19. [Google Scholar]
- Iezzoni L. When Walking Fails. New York: University of California Press; 2003. [Google Scholar]
- Jette A, Tennstedt S, Branch L. Stability of informal long-term care. Journal of Aging and Health. 1992;4:193–211. doi: 10.1177/089826439200400203. [DOI] [PubMed] [Google Scholar]
- Kalton G, Kasprzyk D. The treatment of missing survey data. Statistics Canada. 1986;12:1–16. [Google Scholar]
- Katz SJ, Kabeto M, Langa KM. Gender disparities in the receipt of home care for elderly people with disability in the United States. Journal of the American Medical Association. 2000;284:3022–3027. doi: 10.1001/jama.284.23.3022. [DOI] [PubMed] [Google Scholar]
- Kemper P. The evaluation of the National Long Term Care Demonstration: Overview of the findings. Health Services Research. 1988;23:161–174. [PMC free article] [PubMed] [Google Scholar]
- Laplante M, Harrington C, Kang T. Estimating paid and unpaid hours of personal assistance services in activities of daily living provided to adults living at home. Health Services Research. 2002;37:397–415. doi: 10.1111/1475-6773.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laplante M, Kaye HS, Kang T, Harrington C. Unmet need for personal assistance services: Estimating the shortfall in hours of help and adverse consequences. Journal of Gerontology: Social Sciences. 2004;59B:S98–S108. doi: 10.1093/geronb/59.2.s98. [DOI] [PubMed] [Google Scholar]
- McTigue K, Larson JC, Valoski A, Burke G, Kotchen J, Lewis CE, Stefanick ML, Van Horn L, Kuller L. Mortality and cardiac and vascular outcomes in extremely obese women. Journal of the American Medical Association. 2006;296:79–86. doi: 10.1001/jama.296.1.79. [DOI] [PubMed] [Google Scholar]
- Messeri P, Silverstein M, Litwak E. Choosing optimal support groups: A review and reformulation. Journal of Health and Social Behavior. 1993;24:122–137. [PubMed] [Google Scholar]
- Moon M. Medicare Now and in the Future. 2nd. Washington, D.C.: The Urban Institute; 1996. [Google Scholar]
- Moon M. Sustaining Medicare as an age-related program. In: Hudson RB, editor. The New Politics of Old Age Policy. Baltimore: Johns Hopkins University Press; 2005. pp. 205–218. [Google Scholar]
- National Alliance for Caregiving & AARP. Caregiving in the U.S. 2004 Retrieved July, 6 2007, from http://www.aarp.org/research/reference/publicopinions/aresearch-import-853.html.
- O'Rand AM. When old age begins: Implications for health, work, and retirement. In: Hudson Robert B., editor. The New Politics of Old Age Policy. Baltimore: Johns Hopkins University Press; 2005. [Google Scholar]
- Pastor PN, Makuc DM, Reuben C, Xia H. Chartbook on trends in the health of Americans Health, United States. Vol. 2002. National Center for Health Statistics; Hyattsville, MD: 2002. [Google Scholar]
- Pavalko EK, Artis JE. Women's caregiving and paid work: Causal relationships in late midlife. Journal of Gerontology: Social Sciences. 1997;52:S170–S179. doi: 10.1093/geronb/52b.4.s170. [DOI] [PubMed] [Google Scholar]
- Pavalko E, Henderson K. Combining care work and paid work: Do workplace policies make a difference? Research on Aging. 2006;28:359–374. [Google Scholar]
- Pinquart M, Sorensen S. Gender differences in caregiver stressors, social resources, and health: An updated meta-analysis. Journal of Gerontology: Psychological Sciences. 2006;61:33–45. doi: 10.1093/geronb/61.1.p33. [DOI] [PubMed] [Google Scholar]
- Rossi A, Rossi P. Of Human Bonding – Parent-Child Relations Across the Life Course. New York: Aldine De Gruyter; 1990. [Google Scholar]
- Social Security Administration. (n.d.) Information retrieved October 26, 10 2006 from www.ssa.gov.
- Soldo B, Hill MS. Family structure and transfer measures in the HRS: Background and overview. Journal of Human Resources. 1995;30:S108–S117. [Google Scholar]
- Statacorp. Stata Statistical Software: Releases 8.0 and 9.1. College Station, TX: Stata Corporation; 2003, 2005. [Google Scholar]
- Steinmetz E. American With Disabilities: 2002. Washington, D.C.: U.S. Census Bureau; 2006. pp. 70–107. Current Population Reports. [Google Scholar]
- Stommel M, Given C, Given B. Racial differences in the division of labor between primary and secondary caregivers. Research on Aging. 1998;20:199–217. [Google Scholar]
- Stone R, Cafferata G, Sangl J. Caregivers of the frail elderly: A national profile. Gerontologist. 1987;27:616–626. doi: 10.1093/geront/27.5.616. [DOI] [PubMed] [Google Scholar]
- Sturm R, Ringel JS, Andreyeva T. Trends – Increasing obesity rates and disability trends. Health Affairs. 2006;23:199–205. doi: 10.1377/hlthaff.23.2.199. [DOI] [PubMed] [Google Scholar]
- Toossi M. Labor force projections to 2014: Retiring boomers. Monthly Labor Review. 2005 Nov;:25–44. [Google Scholar]
- U.S. Census Bureau (n.d.), Current Population Survey. Annual Social and Economic Supplement Table A1. Marital Status of People 15 Years and Over, by Age, Sex, Personal Earnings, Race, and Hispanic Origin Internet Release Date: March 27, 2007. 2006 Retrieved July 6, 2007 from http://www.census.gov/population/socdemo/hh-fam/cps2006/tabA1-all.xls.
- Wakabayashi C, Donato K. The consequences of caregiving: Effects on women's employment and earnings. Population Research and Policy Review. 2005;24:467–488. [Google Scholar]
- Walker AJ, Pratt CC, Eddy L. Informal caregiving to aging family members: A critical review. Family Relations. 1995;44:402–411. [Google Scholar]
- Wallace R, Herzog A. Overview of the health measures in the Health and Retirement Study. The Journal of Human Resources. 1995;30:S84–S107. [Google Scholar]
- Wallace SP, Levy-Storms L, Kington RS, Andersen RM. The persistence of race and ethnicity in the use of long-term care. Journal of Gerontology: Social Sciences. 1998;53B:S104–S112. doi: 10.1093/geronb/53b.2.s104. [DOI] [PubMed] [Google Scholar]
- Weissman JS, Epstein AM. Falling Through the Safety Net: Insurance Status and Access to Health Care. Baltimore and London: The Johns Hopkins University Press; 1994. [Google Scholar]
- Williams C. Perspectives on Labour and Income. September. Vol. 5. Ottowa: Statistics Canada; 2004. The sandwich generation [Electronic version] [Google Scholar]
- Wolff JL, Kasper JD. Caregivers of frail elders: Updating a national profile. Gerontologist. 2006;46:344–356. doi: 10.1093/geront/46.3.344. [DOI] [PubMed] [Google Scholar]