Abstract
Background:
Arthroscopic rotator cuff repair has traditionally been performed in the subacromial space from the bursal side of the tendon. The undersurface rotator cuff repair technique involves the arthroscope remaining in the glenohumeral joint, thus viewing the tendon from its undersurface during repair without a bursectomy or acromioplasty.
Purpose:
To compare the clinical and structural outcomes of undersurface rotator cuff repair with bursal-side repair.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A retrospective analysis of prospectively collected data was conducted on 2 cohorts of patients who had undergone arthroscopic rotator cuff repair with knotless suture anchors configured in a single-row formation using inverted mattress–style sutures from either the bursal side (n = 100) or undersurface (n = 165) of the supraspinatus tendon. Data were collected preoperatively, intraoperatively, and at 1 week, 6 weeks, 3 months, 6 months, and 2 years postoperatively. At each time point, patients completed a modified L’Insalata questionnaire to assess patient-ranked pain scores and were clinically examined using standardized tests. Ultrasound examination was performed at 6 months and 2 years to assess the integrity of the repair.
Results:
At 2 years postoperatively, patients in both cohorts had significantly less pain and less difficulty with overhead activities compared with preoperative levels (P < .001). The type of repair performed (bursal or undersurface) did not affect the ability to perform overhead activities at 2 years. At 2 years, both groups also had similar retear rates (21% for bursal side, 23% for undersurface). The mean operative time for the arthroscopic rotator cuff repair was 32 minutes when performed from the bursal side and 20 minutes when performed from the undersurface (P < .001).
Conclusion:
Arthroscopic rotator cuff repair, whether performed from the subacromial space or glenohumeral joint, resulted in decreased levels of pain and difficulty with overhead activities at 2 years. The major difference between the 2 techniques was operative time, with the undersurface technique being performed significantly faster than the bursal-side repair technique.
Keywords: shoulder, rotator cuff tear, arthroscopic rotator cuff repair, undersurface repair technique, bursal side repair, overhead activities
Rotator cuff tears are among the most common causes of pain and functional disability in the shoulder and commonly affect the supraspinatus tendon.5,7,9,18,20 Integrity of the supraspinatus is vital for overhead shoulder function.19 Full-thickness rotator cuff tears often do not heal without treatment.3 These tears are able to be repaired surgically using open surgery.10,21,23 With advances in technology and surgical skill, rotator cuff tears have increasingly been repaired arthroscopically.3,11–13,23,24,29 Arthroscopic repair was often technically demanding and has been associated with long operating times and retear rates of up to 90%.2,3,14–16
The undersurface arthroscopic rotator cuff repair technique involves keeping the arthroscope in the glenohumeral joint, allowing the supraspinatus tendon to be viewed from its undersurface while being repaired.24,29 A feature of this technique is that a subacromial bursectomy and acromioplasty are not performed.24,29 Several studies have shown that there is no benefit to performing an acromioplasty concurrently while performing a rotator cuff repair.6,13,21 Preliminary results suggest that this technique can be performed significantly more quickly than a bursal-side arthroscopic repair and has a retear rate of 20% at 6 months postoperatively.23,29
The primary aim of this study, therefore, was to determine whether the arthroscopic undersurface rotator cuff repair technique influenced patient-ranked pain and difficulty with overhead activities at 2 years postoperatively compared with a standard bursal-side repair technique. Secondary aims were to determine whether the surgical technique utilized influenced the frequency and severity of patient-ranked pain scores, patient functional outcomes, and postoperative rates of tendon retear and revision surgery.
Methods
Ethical approval was granted by our local ethics committee (HREC 06/53). This was a retrospective case-control cohort study of data gathered prospectively. Patients were included in the study if (1) they had an arthroscopic rotator cuff repair performed by a single surgeon (G.A.C.M.), with a minimum 2-year follow-up, and with a repair technique that utilized either a bursal-side or undersurface repair with knotless suture anchors (Opus Magnum; ArthroCare Corp) in a tension band configuration; (2) it was a primary surgery; and (3) the patient had a full-thickness or partial-thickness tear converted to a full-thickness tear prior to repair. Patients were excluded from the study if they had ipsilateral severe arthritis, humeral head fracture, an irreparable tear, a partial repair with a defect, a polytetrafluorethylene (PTFE) patch used during surgery, previous shoulder surgery, a combination of both bursal-side and undersurface repair techniques performed, if the operative report was not indicative of which technique had been used, or if 2-year postoperative follow-up could not be conducted.
Surgical Technique
Rotator cuff repairs utilizing both the bursal-side and undersurface repair techniques were performed with the patient positioned in the beach-chair position and under interscalene block.11,23,24,29 If there was a partial-thickness supraspinatus tear greater than 50% of the thickness of the supraspinatus, a scalpel was used to convert this tear into a full-thickness tear.24 In both types of repair, the torn tendon edge and landing site were prepared with a 4.0- or 5.5-mm shaver (Stryker Endoscopy) introduced through a lateral portal.23,24,29 Grasping of and passing sutures through the torn tendon edge was accomplished using an Opus Smart Stitch Suture Device (ArthroCare Corp), and anchor holes at the landing site were created using a T-handled punch.11,12,23,24,29 The specific surgical techniques required to perform both the bursal-side and undersurface repairs have been outlined elsewhere and are here described in brief.11,12,23,24,29
Bursal-Side Repair Technique
The bursal-side repair was traditionally performed using a 3-portal technique.11,12,23 However, the senior author (G.A.C.M.) adapted this technique to utilize 2 portals: located posteriorly for viewing the glenohumeral joint and subacromial space and laterally for both subacromial decompression and rotator cuff repair.11,12,23 After inspecting the glenohumeral joint, the arthroscope was placed in the subacromial bursa, and a bursectomy and an acromioplasty were performed.11,12,23 The edge of the torn rotator cuff tendon and footprint on the greater tuberosity were then debrided using an arthroscopic shaver.11,12,23 The torn tendon was grasped utilizing the Opus SmartStitch Suture Device.23 Polyester sutures were delivered using an inverted mattress configuration.23 A single-row configuration was used for the repair, with anchor holes being made at the landing site through the lateral portal.23 Once the anchor hole was prepared, the limbs of the suture were passed through the Opus Magnum Knotless Implant, which was then inserted and deployed into the bone.23 Prior to locking, the suture was wound through the anchor to facilitate reduction of the torn tendon.23
Undersurface Repair Technique
The undersurface technique involved the arthroscope being inserted into the glenohumeral joint through the posterior portal, which allowed undersurface visualization of the torn tendon (Figure 1).24,29 The arthroscope then remained in the glenohumeral joint throughout the repair of the tendon.24,29 The position of the lateral portal was determined using a spinal needle, with primary considerations being that the sutures should be able to be passed easily through the tendon edge and that the anchors were able to be placed at right angles to the tendon footprint on the greater tuberosity (Figure 1).24,29 Preparation of the tendon edge and landing site was as outlined above.23 The sutures were passed through the tendon, then through the anchor (Opus Magnum anchor).23 The anchor was inserted into the hole, wound in, and then deployed into the bone, reducing the torn tendon (Figure 1).23
Figure 1.
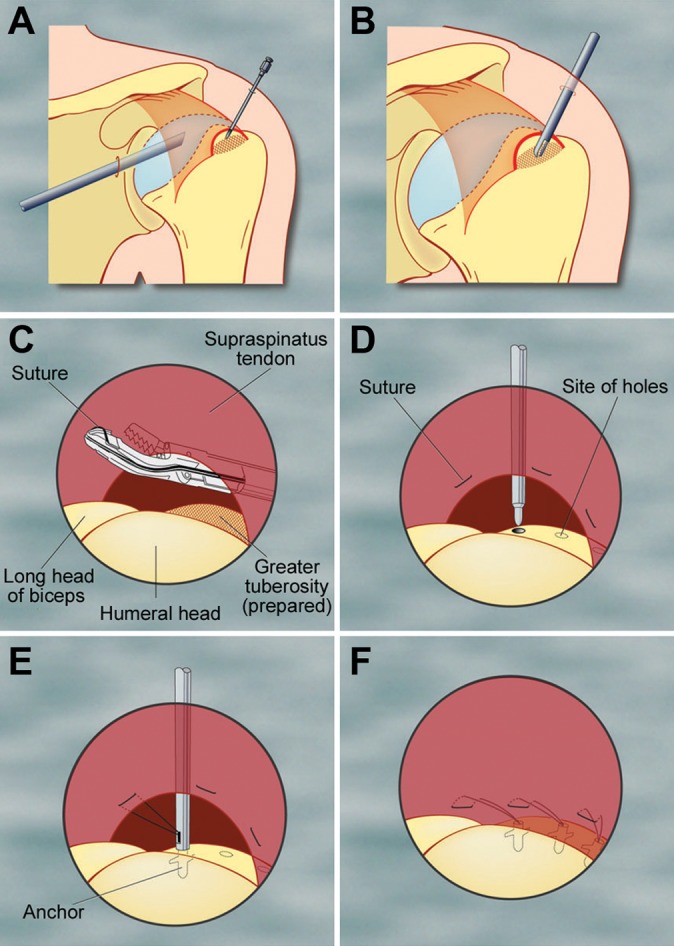
Surgical procedure for the undersurface approach to arthroscopic rotator cuff repair. (A) The torn tendon is inspected from its undersurface and the torn tendon edge is located using a spinal needle. (B) The landing site on the greater tuberosity of the humerus is prepared using a shaver. (C) While visualizing the torn tendon from its undersurface, the tendon is grasped and sutures are passed through the tendon using the Opus SmartStitch Suture Device. (D) The landing sites for the anchors are created on the greater tuberosity using a T-handle punch. (E) Both limbs of the suture are passed through the anchor, which together are inserted into the prepared holes and the anchor is deployed and secured into the bone. (F) The TensionLock winding mechanism reduces the tendon to bone, thereby completing the repair. Adapted and reproduced with permission from Wu et al.29
Surgical Technique Transition
Prior to March 2004, the senior author (G.A.C.M.) performed open rotator cuff repair surgery utilizing metallic suture anchors (Mitek RC QuickAnchor; DePuy Mitek).23 The surgeon then changed to arthroscopic rotator cuff repair, utilizing a knotted fixation technique performed on the bursal side of the tendon.23 From March 2005, a knotless suture anchor (Opus Magnum) utilizing a tension band suture configuration was used for tendon fixation, with repairs also occurring on the tendon’s bursal side.23 From December 2006, the surgeon devised and then began to use the undersurface repair technique utilizing a knotless anchor (Opus Magnum) with a tension band suture configuration. During this time, larger tears that required an extra suture to adequately repair were often performed with a combination of both techniques. The bursal-side repair cohort had repairs performed temporally earlier than the undersurface repair cohort, with a period of overlap when both bursal-side and undersurface repairs were performed.
Postoperative Rehabilitation Protocol
Patients from both cohorts underwent a previously outlined recovery protocol that involved 3 phases.24 Phase 1 consisted of immobilization of the operated shoulder in a sling with a small abduction pillow (UltraSling; DJO Australia). From day 1 postoperatively, mobilization exercises were commenced, which aimed to improve elbow range of motion (ROM), grip, periscapular strength, and internal and external rotation.24 From week 2 postoperatively, shoulder flexion and extension exercises were begun.24 Phase 2 exercises involved isometric strengthening and occurred from 6 weeks to 3 months postoperatively. Phase 3 exercise began at 3 months postsurgery and finished at 6 months postsurgery. Phase 3 exercises, performed twice a day, utilized a yellow Thera-Band (The Hygenic Corp) for strengthening exercises and allowed overhead lifting of up to 5 kg.24 Cold therapy (Durasoft; DJO Australia) commenced and continued every 2 hours for 20 minutes regularly for the first 48 hours after surgery, and then as needed.24
Outcome Measures
Patients completed the Shoulder Service Questionnaire at each visit to the clinic both pre- and postoperatively. This questionnaire was based on the L’Insalata questionnaire and utilized a Likert-type scale to rank frequency and severity of shoulder pain, level of shoulder stiffness, and the patient’s overall rating of their shoulder condition.17,26
Examiner-determined data regarding shoulder function was gathered through clinical testing performed by trained observers. Passive ROM and strength were assessed preoperatively and at 6 and 12 weeks, 6 months, and 2 years postoperatively. Passive ROM was assessed by visual estimation for forward flexion, external rotation, internal rotation, and abduction as previously outlined.26 Strength was measured using an HFG-45 Hand-Held Force Gauge (Transducer Techniques) in the planes of internal and external rotation at 0° of shoulder abduction, elevation in the scapular plane, adduction of the arm, and when performing the lift-off test.25,26
Ultrasound Examination
At 6 months and 2 years postoperatively, the integrity of the repair was assessed via ultrasound. Ultrasound was performed by 2 experienced ultrasonographers who used a GE Logiq E9 machine with a linear ML 6- to 15-MHz transducer using a previously outlined standard protocol.4,28
Statistical Analysis
Parametric data (shoulder strength and ROM) were compared using unpaired Student t tests. Nonparametric data (pain scores, internal rotation vertebral levels) were assessed using Mann-Whitney rank-sum tests. The chi-square test was utilized to assess dichotomous data. Correlations and regression (multiple linear and logistic) analyses were also performed. Where there were significant differences in patient-ranked pain scores or functional outcomes at 2 years, a 2-way analysis of variance (ANOVA) was carried out. For each set of tests, the significance level was set at 0.05, and Bonferroni corrections were used to correct for conducting multiple tests. Statistical analysis was carried out utilizing SigmaPlot v11 (Systat Software Inc), GraphPad Prism v6 (GraphPad Software Inc), and SPSS (IBM Corp).
Results
Patient Inclusion and Exclusion Criteria
Between March 2005 and September 2010, the senior author (G.A.C.M.) carried out 1418 arthroscopic rotator cuff repairs. Of these, 243 repairs were excluded due to either having a combination of bursal-side and undersurface repair techniques or not having the technique specified on the operative report. Of the remaining repairs, 56 were excluded due to prior ipsilateral shoulder surgery, 49 for an irreparable tear or a partial repair, 39 for severe ipsilateral osteoarthritis, 15 for an isolated subscapularis repair, 5 for fixation of an ipsilateral humeral head avulsion fracture, and 4 due to use of a PTFE patch during surgery. After these exclusions, 692 patients (742 shoulders) were deemed eligible for the study and were contacted. Of these, 257 patients (265 shoulders) had either a bursal-side or undersurface arthroscopic rotator cuff repair using a knotless tension band technique (Opus Magnum) and attended a minimum 2-year follow-up with ultrasound examination of the rotator cuff repair. These patients were included in the study. Of these, 100 surgeries were performed using a bursal-side repair technique and 165 were performed using the undersurface repair technique.
Patient Demographics
The bursal-side repair cohort consisted of 53 women and 46 men (100 shoulders), with a mean age of 58 years (range, 25-88 years) (Table 1). The undersurface cohort had 75 women and 86 men (165 shoulders) with a mean age of 60 years (range, 18-87 years). The mean duration of symptoms from injury to surgery was 19 months (range, 0-192 months) for the bursal repair group and 15 months (range, 0-156 months) for the undersurface group. Both groups were also well matched in terms of prevalence of osteoarthritis, diabetes, and injuries that were work related (Table 1). There were no differences in preoperative pain or functional scores between the 2 groups, but the undersurface cohort had slightly, but significantly, greater preoperative external rotation strength.
TABLE 1.
Demographic and Intraoperative Data of Bursal-Side and Undersurface Arthroscopic Rotator Cuff Repair Groupsa
| Variable | Bursal-Side Repair (n = 100) | Undersurface Repair (n = 165) | Bursal vs Undersurface | P Value |
|---|---|---|---|---|
| Sex, male:female, n | 47:53 | 88:77 | NS | .48b |
| Age at surgery, y, mean (range) | 58 (25-88) | 60 (18-87) | NS | .14b |
| Time from initial injury to repair, mo, mean ± SEM (range) | 19.03 ± 3.4 (0-192) | 15.25 ± 2.1 (0-152) | NS | .34c |
| Affected shoulder, left:right, n | 35:65 | 80:85 | NS | .08b |
| Diabetes, n | 7 | 15 | NS | .80b |
| Osteoarthritis, n | 9 | 35 | NS | .27b |
| Work-related injury, n | 26 | 43 | NS | >.99b |
| Tear size, mean ± SEM (range) | ||||
| Anterior-posterior, mm | 18 ± 1 (5-60) | 17 ± 1 (5-50) | NS | .23c |
| Medial-lateral, mm | 15 ± 1 (4-60) | 14 ± 1 (4-50) | NS | .91c |
| Area, mm2 | 339 ± 51 (25-3600) | 384 ± 22 (25-2000) | NS | .25c |
| Full-thickness tears, n | 54 | 104 | NS | .46b |
| Partial-thickness tears, n | 34 | 51 | NS | .46b |
| Anchors used, mean ± SEM (range) | 2.1 ± 0.1 (1-5) | 2.1 ± 0.1 (1-5) | NS | .36b |
| Operative time, min, mean ± SEM (range) | 32 ± 1.3 (6-60) | 20 ± 0.8 (4-50) | <.001 | <.001c |
aNS, not statistically significant; SEM, standard error of mean.
bChi-square test.
cUnpaired Student t test.
In terms of procedures carried out concurrently with the rotator cuff repair, in the bursal-side repair group, 40 patients had an acromioplasty, 8 had removal of calcium for calcific tendonitis, 1 had a labral repair, 1 a subscapularis repair, 1 an acromioclavicular (AC) joint injection, 1 a capsular release, 1 had removal of bony fragments, 1 had both the removal of calcium for calcific tendonitis and a capsular release, and 1 had a biceps tenodesis and subscapularis repair.
In the undersurface cohort, 13 patients had an acromioplasty in addition to the rotator cuff repair, 4 had labral repairs, 3 had a biceps tenodesis, 2 had a capsular release, 1 had a biceps tenodesis and acromioplasty, 1 had a biceps tenotomy, 1 had a distal clavicle excision, 1 had manipulation under anesthesia, 1 a subscapularis repair, and 1 an AC joint injection. Acromioplasty was performed only on patients with type III (hooked) acromion or with severe impingement.
Intraoperative Data
The mean tear area was 3.5 cm2 for the bursal group (range, 0.25-36 cm2) and 2.8 cm2 for the undersurface group (range, 0.25-20 cm2) (P = .25) (Table 1). On average, 2 anchors were used in the repairs for both groups. There was no significant difference between groups with respect to the number of partial-thickness or full-thickness tears. The bursal-side repair required significantly more operating time (32 minutes) compared with the time required to perform an undersurface repair (20 minutes) (P < .001) (Table 1).
Patient-Ranked Outcomes
Our primary aim was to determine whether the undersurface surgical repair technique influenced difficulty and pain with overhead activities at 2 years postoperatively. At 2 years, both cohorts had significantly less difficulty with overhead activities than before their surgery (P < .001). However, the type of repair performed (bursal side or undersurface) did not affect the ability to perform overhead activities at 2 years (Figure 2).
Figure 2.
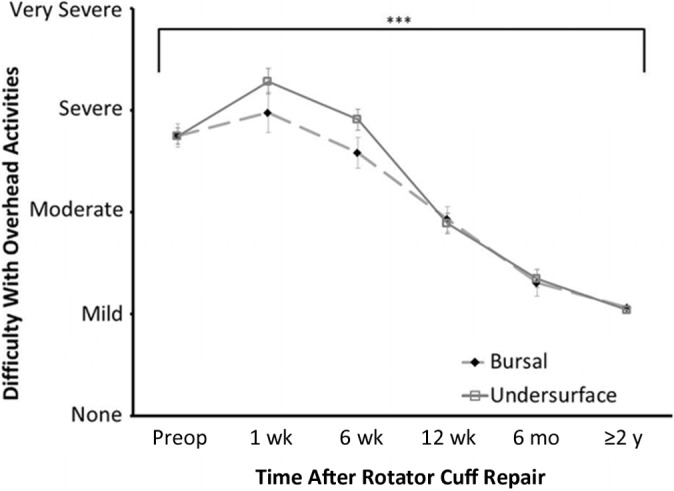
Effect of surgical technique on level of difficulty with overhead activities. Comparison between the bursal-side and undersurface repair cohorts using Mann-Whitney rank-sum test. ***P < .001 across both the bursal and undersurface cohorts.
At 2 years, both cohorts had significantly decreased levels of pain with overhead activities compared with preoperative results (P < .001), with there being no significant difference between cohorts (Figure 3).
Figure 3.
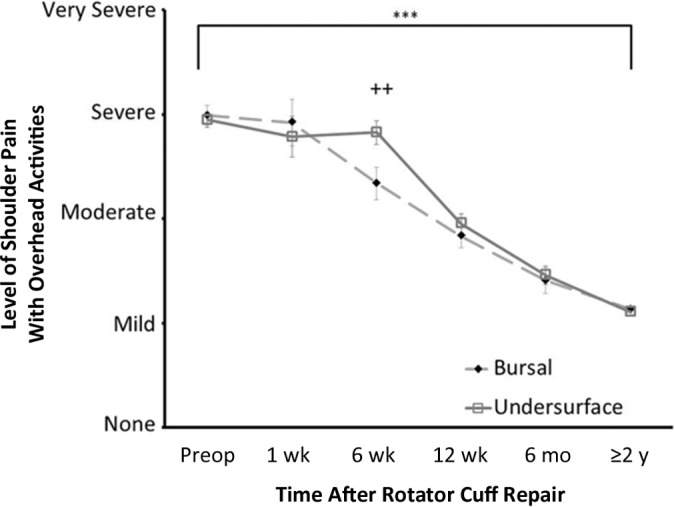
Effect of surgical technique on patient-ranked pain scores. Comparison between the bursal side (n = 100) and undersurface repair (n = 165) cohorts in terms of level of shoulder pain with overhead activities. ***P < .001 across both the bursal and undersurface cohorts; ++ P < .01 between the cohorts using the Mann-Whitney rank-sum test.
Both groups had a significantly decreased frequency of extreme shoulder pain, pain during activity, and pain during sleep at 2 years compared with before surgery (P < .001). The undersurface group had more frequent shoulder pain when sleeping at both 12 weeks and 2 years postoperatively when compared with the bursal group (P = .03) (Figure 4). There was no significant difference between the cohorts with respect to frequency of extreme and activity pain at 2 years (Table 2).
Figure 4.
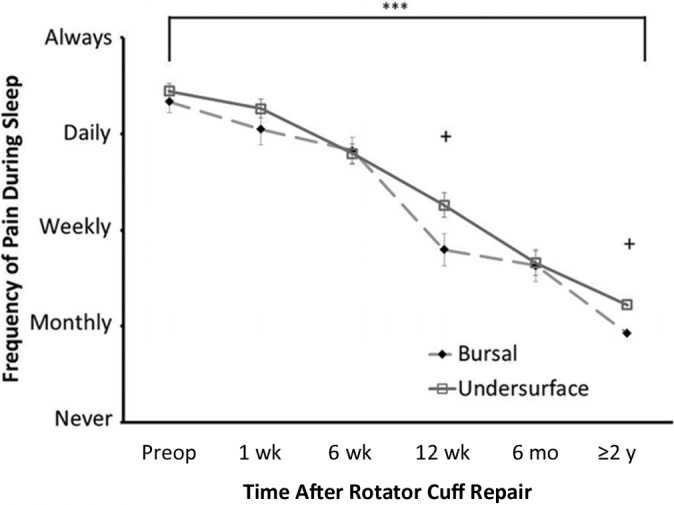
Effect of surgical technique on frequency of sleep pain. Comparison between the bursal-side and undersurface repair cohorts using the Mann-Whitney rank-sum test. ***P < .001 across both the bursal-side and undersurface cohorts; + P < .05 between the bursal and undersurface cohorts.
TABLE 2.
Patient-Ranked Pain Scoresa
| Outcomeb | Bursal-Side Repair | Undersurface Repair | Bursal vs Undersurface | P Value |
|---|---|---|---|---|
| Pain severity | ||||
| At rest | ||||
| Preoperatively | 1.77 | 1.78 | NS | .88 |
| 2 y | 0.65 | 0.65 | NS | .92 |
| When sleeping | ||||
| Preoperatively | 2.22 | 2.28 | NS | .74 |
| 2 y | 0.66 | 0.84 | NS | .06 |
| Pain frequency | ||||
| Extreme pain | ||||
| Preoperatively | 2.45 | 2.82 | NS | .20 |
| 2 y | 0.46 | 0.65 | NS | .23 |
| Activity pain | ||||
| Preoperatively | 3.51 | 3.64 | NS | .22 |
| 2 y | 1.41 | 1.48 | NS | .60 |
| When sleeping | ||||
| Preoperatively | 3.34 | 3.45 | NS | .52 |
| 2 y | 0.93 | 1.22 | <.05 | .03 |
| Level of difficulty with reaching behind the back | ||||
| Preoperatively | 2.71 | 2.59 | NS | .45 |
| 2 y | 0.97 | 0.90 | NS | .32 |
| Shoulder stiffness | ||||
| Preoperatively | 1.74 | 1.73 | NS | .93 |
| 2 y | 0.88 | 0.86 | NS | .97 |
| Highest level of work | ||||
| Preoperatively | 1.36 | 1.25 | NS | .38 |
| 2 y | 1.30 | 1.16 | NS | .30 |
| Highest level of sport | ||||
| Preoperatively | 0.36 | 0.47 | NS | .27 |
| 2 y | 0.49 | 0.61 | NS | .30 |
aComparison between the groups using the Mann-Whitney rank-sum test. Values are expressed as means. NS, not statistically significant.
bPain questionnaire numerical conversion for question “How often is your shoulder painful?”: 4, always; 3, daily; 2, weekly; 1, monthly; 0, never.
At the 2-year follow-up, patients in both groups experienced significantly less pain at rest, sleep, and during activity compared with preoperative levels (P < .001). At 2 years, there was no significant difference in pain severity between the groups (Table 2).
Both cohorts had significantly less difficulty when reaching behind the back at 2 years when compared with prior to surgery (P < .001). At 2 years, there was no significant difference in difficulty reaching behind the back between the 2 groups (Table 2).
At 2 years postoperatively, both groups reported significantly less shoulder stiffness compared with preoperative levels (P < .001), with no significant difference between the 2 groups at any time point (Table 2). Overall shoulder satisfaction improved for both groups, from an overall mean of poor preoperatively to good at the 2-year follow-up (P < .001). There was no significant difference in levels of shoulder satisfaction between the cohorts at any time point (Table 2).
Shoulder Strength
The groups were well matched in terms of supraspinatus and adduction strength prior to surgery. Both groups had significantly improved supraspinatus and adduction strength at 2 years postoperatively compared with preoperative strength (P < .001). However, at 2 years, there was no significant difference between the groups (Figure 5 and Table 3).
Figure 5.
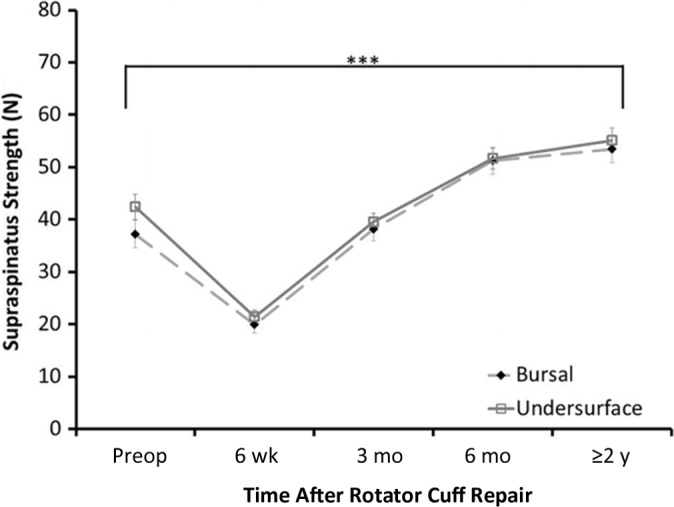
Effect of surgical technique on supraspinatus strength. ***P < .001. The black significance line equals improvement across both cohorts. Comparison completed using the Student t test.
TABLE 3.
Strength and Range of Motion Data of Bursal-Side and Undersurface Arthroscopic Rotator Cuff Repair Groups Taken Preoperatively and at 2 Years Postoperativelya
| Variable | Bursal-Side Repair | Undersurface Repair | Bursal vs Undersurface | P Value |
|---|---|---|---|---|
| Strength, N | ||||
| Supraspinatus | ||||
| Preoperative | 37.2 ± 2.7 (0-125) | 42.4 ± 2.4 (0-173) | NS | .15b |
| 2 y | 53.5 ± 2.6 (0-136) | 55.2 ± 2.4 (0-145) | NS | .63b |
| Adduction | ||||
| Preoperative | 66.9 ± 4.3 (0-246) | 76.4 ± 3.5 (0-224) | NS | .34b |
| 2 y | 104.8 ± 9.2 (0-380) | 87.3 ± 3.6 (0-243) | NS | .08b |
| Internal rotation | ||||
| Preoperative | 62.38 ± 3.1 (13-170) | 67.86 ± 2.7 (0-178) | NS | .19b |
| 2 y | 73.48 ± 3.2 (14-198) | 77.42 ± 2.5 (0-158) | NS | .33b |
| External rotation | ||||
| Preoperative | 47.7 ± 2.8 (9-162) | 55.7 ± 2.5 (0-167) | <.05 | .04b |
| 2 y | 63.8 ± 7.1 (10-204) | 60 ± 2.2 (0-154) | NS | .61b |
| Lift-off test | ||||
| Preoperative | 31.7 ± 3.1 (0-106) | 36.1 ± 2.1 (0-108) | NS | .25b |
| 2 y | 47.1 ± 2.6 (0-131) | 48.8 ± 2.3 (0-129) | NS | .63b |
| Range of motion, deg | ||||
| Abduction | ||||
| Preoperative | 127.1 ± 4.5 (30-180) | 125 ± 3.2 (30-180) | NS | .72b |
| 2 y | 147 ± 3.5 (40-180) | 149.3 ± 2.7 (40-180) | NS | .59b |
| Forward flexion | ||||
| Preoperative | 144.6 ± 3.7 (45-180) | 158.7 ± 10.3 (40-180) | NS | .20b |
| 2 y | 163.5 ± 10.3 (40-180) | 166.6 ± 2 (50-180) | NS | .34b |
| External rotation | ||||
| Preoperative | 55.8 ± 2.2 (10-90) | 54.7 ± 2.1 (20-100) | NS | .71b |
| 2 y | 56.1 ± 1.6 (0-95) | 59.4 ± 1.8 (0-100) | NS | .22b |
| Internal rotation (vertebral level) | ||||
| Preoperative | L1 ± 0.5 (S5-T7) | L1 ± 0.4 (S5-T7) | NS | .79c |
| 2 y | T9 ± 0.4 (S5-T7) | T10 ± 0.3 (S5-T7) | <.05 | .02c |
aValues are expressed as mean ± standard error of the mean, with range in parentheses. NS, not statistically significant.
bStudent t test.
cMann-Whitney rank-sum test.
At 2 years, both cohorts had significantly improved strength in both internal rotation and the lift-off test (P < .001), and there was no significant difference between the bursal-side and undersurface repair groups at any time point (Table 3).
The undersurface cohort had significantly greater external rotation strength preoperatively when compared with the bursal cohort (P = .04). At 2 years, there was no significant difference in external rotation strength between the bursal-side and undersurface repair groups. However, only the undersurface group had significant improvement in external rotation strength at 2 years compared with preoperative scores (P = .03) (Table 3).
Passive Range of Motion
At 2 years, both groups had significantly improved ROM in abduction and forward flexion (P < .001), with there being no significant difference between the groups (Table 3).
The undersurface cohort had significantly improved external rotation ROM at 2 years (P = .05), while the bursal cohort did not show significant improvement. At 2 years, there was no significant difference between the groups (Table 3).
At 2 years, both groups had significant improvement for internal rotation ROM compared with preoperative scores (P < .001). At 6 months, the undersurface cohort had significantly greater internal rotation ROM (P < .001). However, at 2 years postoperatively, the bursal cohort showed greater ROM in internal rotation (P = .02) (Table 3).
Retear Rates and Revision Surgery
Assessment of the tendon integrity was performed using ultrasound at both 6 months and 2 years postoperatively.
Bursal-Side Repair Group
The bursal-side repair group had 21 retears (21/100, 21%) at 6 months and 20 (20/100, 20%) retears at 2 years postoperatively. At 6 months, the mean retear size was found to be 2.7 ± 0.5 cm2, with the mean retear size at 2 years being 4.8 ± 0.7 cm2. During the study period, 9 of these retears required revision rotator cuff repair surgery (9/20, 45%) and 3 had repair of the tendon defect and a concurrent acromioplasty (3/20, 15%). There was also a revision surgery to remove a loose anchor (1/20, 5%), and 1 procedure that was not documented (1/20, 5%). The overall revision surgery rate was 14% (14/100).
Undersurface Repair Group
The undersurface repair group had 25 retears (25/165, 15%) at 6 months postoperatively and 38 retears (38/165, 23%) at 2 years. The mean retear size was 3.2 ± 0.7 cm2 at 6 months and 3.1 ± 0.4 cm2 at 2 years. During the study period, 14 of these retears came to revision rotator cuff repair surgery (14/38, 37%). Three further revision surgeries were required to remove loose anchors (3/38, 8%). One patient had their retear repaired with a PTFE patch (1/38, 3%), 1 had to repair a retorn tendon and have a concurrent acromioplasty (1/38, 3%), and 1 had to treat postoperative frozen shoulder (1/38, 3%). The overall revision surgery rate was 12% (20/165).
There was no significant difference between groups at 6 months (P = .24) or 2 years (P = .87) for either retear rate or rate of revision surgeries. At 6 months, there was no significant difference between the groups in terms of mean retear size. However, at 2 years, it was found that the bursal-side repair group had significantly larger retears (P = .04).
Positive Impingement Signs
At 2-year follow-up, both cohorts showed significant reductions in rates of internal and external rotation impingement signs compared with preoperative levels (P < .001), but there were no differences between cohorts at any postoperative time points.
Discussion
This study examined clinical outcomes of 2 cohorts of patients who had their rotator cuffs repaired either from the bursal side or the undersurface. There was no significant difference in level of pain or difficulty with overhead activities between the bursal-side and undersurface repair cohorts 2 years after surgery. However, the undersurface technique showed significantly shorter operative time and smaller retear size at 2 years postoperatively. At 2-year follow-up, the bursal-side cohort had less frequent pain at night and increased internal rotation ROM.
As outlined above, an undersurface rotator cuff repair was able to be carried out faster than a bursal-side repair, with a mean time of 20 minutes for an undersurface repair compared with 32 minutes for a bursal-side repair.24,29 Time was able to be saved during surgery as there was no need to perform either a bursectomy or an acromioplasty.29 Shorter operating times are associated with reducing the cost of surgery and the risk of complications.8,29 We also found that the time to perform a bursal-side repair was reduced compared with previous results.24,29 This difference is likely to be due to the increased experience of the surgeon when performing the repair.14
At 2 years postoperatively, the size of tendon retears present in the undersurface repair cohort was significantly smaller than those present in the bursal-side repair cohort. This difference was not present at 6 months. There was a correlation between the undersurface repair technique and decreased tendon retear size at 2 years (r = 0.28, P < .05). There was no correlation between performing an acromioplasty during surgery and retear size at 2 years. There was no difference between the prevalence of retears that required revision surgery between the undersurface and bursal-side repair groups.
At 2 years, the undersurface repair group was found to have more frequent pain at night compared with those who had a bursal-side repair. However, a 2-way ANOVA showed that frequency of sleep pain at 2 years was not influenced by the surgical technique utilized. Multiple linear regression analysis showed that preoperative tear size, surgical technique, performing an acromioplasty, operative time, and retear size did not influence either frequency or level of sleep pain at 2 years after surgery.
At 2 years, the bursal-side repair cohort also had significantly better internal rotation ROM compared with the undersurface repair cohort. Functionally, this difference equated to patients being able to achieve approximately half of a vertebral-level increased internal rotation ROM. This difference may not be clinically significant. A 2-way ANOVA confirmed that at 2 years postoperatively, the surgical technique utilized did not influence internal rotation. This difference was also not due to lack of an acromioplasty. Multiple linear regression analysis showed that performing an acromioplasty did not influence internal rotation ROM.
A major difference between the bursal-side and undersurface repair cohorts was that an undersurface repair did not involve performing an acromioplasty. To assess the impact this may have had on both patient-ranked pain scores and functional outcomes, multiple linear regression analyses were carried out. These analyses showed that at 2 years postoperatively, performing an acromioplasty did not influence pain or difficulty with overhead activities, difficulty with reaching behind the back, shoulder stiffness, ROM (in the planes of forward flexion, abduction, internal rotation, external rotation), or shoulder strength (supraspinatus, adduction, external rotation, lift-off). However, it was found that not performing an acromioplasty during rotator cuff repair strongly correlated with increased internal rotation strength at 2 years postoperatively (r = 0.21, P < .01). Several other studies have shown no additional value to performing an acromioplasty.1,13,22,27
A previous pilot study examined undersurface and bursal-side repair cohorts, following patients up to 6 months postoperatively.29 This prior study found the undersurface repair technique resulted in reduced frequency of pain during activity at both 6 weeks and 3 months postoperatively, as well as reduced difficulty with reaching behind the back at 6 months.29 These results were not mirrored when examining findings from the current study, as there was no significant difference between the cohorts at these time points. Multiple linear regression analyses showed that frequency of activity pain at 6 weeks and 3 months postoperatively was not influenced by the original tear size, performing an acromioplasty, operative time, or the surgical technique utilized. This was also true when examining difficulty reaching behind the back at 6 months.
The pilot study showed no significant differences between the cohorts regarding frequency of pain during sleep, level of pain (during rest, sleep, and overhead activities), level of shoulder stiffness, and level of difficulty (with overhead activities and when reaching behind the back) at all time points up to 6 months postoperatively.29
A limitation to the current study was that a large number of patients who were eligible for the study (439/696, 63%) had to be excluded, as the 2-year postoperative follow-up could not be conducted on them. Two-year follow-up appointments were not standard procedure for this clinic, so patients had to be contacted individually to present for examination. It was noted that patients were often not willing to attend the follow-up appointments if they felt that their shoulder was not causing them any problems.
Strengths of the study were that all surgeries were carried out by 1 experienced surgeon (G.A.C.M.), there were no significant differences in demographic data, and the sample size of both groups was large. At each follow-up appointment, the patients completed the same Shoulder Service Questionnaire and had the same physical examination. The inclusion criteria also eliminated major concurrent pathologies.
Conclusion
Our study showed that there were no significant differences in postoperative pain and difficulty with overhead activities between bursal-side repair and undersurface repair techniques. Both groups showed significant improvements in postoperative pain and difficulty with overhead activities compared with preoperative levels. The undersurface technique was able to be performed significantly faster.
Footnotes
Declaration of Conflicting Interests: One or more of the authors has declared the following potential conflict of interest or source of funding: G.A.C.M. is a consultant for and received research funding from ArthroCare.
References
- 1. Abrams GD, Gupta AK, Hussey KE, et al. Arthroscopic repair of full-thickness rotator cuff tears with and without acromioplasty: randomized prospective trial with 2-year follow-up. Am J Sports Med. 2014;42:1296–1303. [DOI] [PubMed] [Google Scholar]
- 2. Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15:290–299. [DOI] [PubMed] [Google Scholar]
- 3. Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–1240. [DOI] [PubMed] [Google Scholar]
- 4. Briggs L, Murrell GAC. Diagnostic ultrasound: examination of the shoulder. Tech Shoulder Elbow Surg. 2011;12:101–107. [Google Scholar]
- 5. Browning DG, Desai MM. Rotator cuff injuries and treatment. Prim Care. 2004;31:807–829. [DOI] [PubMed] [Google Scholar]
- 6. Budoff JE, Nirschl RP, Guidi EJ. Debridement of partial-thickness tears of the rotator cuff without acromioplasty. Long-term follow-up and review of the literature. J Bone Joint Surg Am. 1998;80:733–748. [DOI] [PubMed] [Google Scholar]
- 7. Chillemi C, Petrozza V, Garro L, et al. Rotator cuff re-tear or non-healing: histopathological aspects and predictive factors. Knee Surg Sports Traumatol Arthrosc. 2011;19:1588–1596. [DOI] [PubMed] [Google Scholar]
- 8. Churchill RS, Ghorai JK. Total cost and operating room time comparison of rotator cuff repair techniques at low, intermediate, and high volume centers: mini-open versus all-arthroscopic. J Shoulder Elbow Surg. 2010;19:716–721. [DOI] [PubMed] [Google Scholar]
- 9. Clark JM, Harryman DT., 2nd Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy. J Bone Joint Surg Am. 1992;74:713–725. [PubMed] [Google Scholar]
- 10. Galatz LM, Griggs S, Cameron BD, Iannotti JP. Prospective longitudinal analysis of postoperative shoulder function: a ten-year follow-up study of full-thickness rotator cuff tears. J Bone Joint Surg Am. 2001;83:1052–1056. [PubMed] [Google Scholar]
- 11. Gartsman GM, Hammerman SM. Full-thickness tears: arthroscopic repair. Orthop Clin North Am. 1997;28:83–98. [DOI] [PubMed] [Google Scholar]
- 12. Gartsman GM, Khan M, Hammerman SM. Arthroscopic repair of full-thickness tears of the rotator cuff. J Bone Joint Surg Am. 1998;80:832–840. [DOI] [PubMed] [Google Scholar]
- 13. Gartsman GM, O’Connor DP. Arthroscopic rotator cuff repair with and without arthroscopic subacromial decompression: a prospective, randomized study of one-year outcomes. J Shoulder Elbow Surg. 2004;13:424–426. [DOI] [PubMed] [Google Scholar]
- 14. Green LB, Pietrobon R, Paxton E, Higgins LD, Fithian D. Sources of variation in readmission rates, length of stay, and operative time associated with rotator cuff surgery. J Bone Joint Surg Am. 2003;85:1784–1789. [DOI] [PubMed] [Google Scholar]
- 15. Jost B, Pfirrmann CW, Gerber C, Switzerland Z. Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2000;82:304–314. [DOI] [PubMed] [Google Scholar]
- 16. Jost B, Zumstein M, Pfirrmann CW, Gerber C. Long-term outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2006;88:472–479. [DOI] [PubMed] [Google Scholar]
- 17. L’Insalata JC, Warren RF, Cohen SB, Altchek DW, Peterson MG. A self-administered questionnaire for assessment of symptoms and function of the shoulder. J Bone Joint Surg Am. 1997;79:738–748. [PubMed] [Google Scholar]
- 18. Lam P, Murrell G. Biomechanical considerations for rotator cuff repairs. Tech Shoulder Elbow Surg. 2011;12:108–115. [Google Scholar]
- 19. Liem D, Lichtenberg S, Magosch P, Habermeyer P. Arthroscopic rotator cuff repair in overhead-throwing athletes. Am J Sports Med. 2008;36:1317–1322. [DOI] [PubMed] [Google Scholar]
- 20. Lohr JF, Uhthoff HK. Epidemiology and pathophysiology of rotator cuff tears [in German]. Orthopade. 2007;36:788–795. [DOI] [PubMed] [Google Scholar]
- 21. McCallister WV, Parsons IM, Titelman RM, Matsen FA., 3rd Open rotator cuff repair without acromioplasty. J Bone Joint Surg Am. 2005;87:1278–1283. [DOI] [PubMed] [Google Scholar]
- 22. Milano G, Grasso A, Salvatore M, Zarelli D, Deriu L, Fabbriciani C. Arthroscopic rotator cuff repair with and without subacromial decompression: a prospective randomized study. Arthroscopy. 2007;23:81–88. [DOI] [PubMed] [Google Scholar]
- 23. Millar NL, Wu X, Tantau R, Silverstone E, Murrell GA. Open versus two forms of arthroscopic rotator cuff repair. Clin Orthop Relat Res. 2009;467:966–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Murrell G. Advances in rotator cuff repair—undersurface repair. Tech Shoulder Elbow Surg. 2012;13:28–31. [Google Scholar]
- 25. Osbahr DC, Murrell GA. The rotator cuff functional index. Am J Sports Med. 2006;34:956–960. [DOI] [PubMed] [Google Scholar]
- 26. Ronquillo J, Szomor Z, Murrell GA. Examination of the shoulder. Tech Shoulder Elbow Surg. 2011;12:116–125. [Google Scholar]
- 27. Shin SJ, Oh JH, Chung SW, Song MH. The efficacy of acromioplasty in the arthroscopic repair of small- to medium-sized rotator cuff tears without acromial spur: prospective comparative study. Arthroscopy. 2012;28:628–635. [DOI] [PubMed] [Google Scholar]
- 28. Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am. 2000;82:498–504. [PubMed] [Google Scholar]
- 29. Wu XL, Baldwick C, Briggs L, Murrell GAC. Arthroscopic undersurface rotator cuff repair. Tech Shoulder Elbow Surg. 2009;10:112–118. [Google Scholar]


