Abstract
Background:
Femoroacetabular impingement (FAI) is a condition that is becoming increasingly recognized as a common etiology of hip pain in athletes, adolescents, and adults. However, history and clinical examination are often inconclusive in reaching a diagnosis, while imaging often detects asymptomatic abnormalities. Treatment has traditionally been limited to surgery, with the role of conservative management remaining unclear.
Purpose:
To evaluate the utility of the intra-articular hip injection in the diagnosis and management of FAI.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
MEDLINE, EMBASE, and PubMed databases were screened in duplicate for studies published between January 1946 and January 2014. Search terms included femoroacetabular impingement, hip impingement, and intra-articular injection. Quality assessment using the Methodological Index for Non-Randomized Studies (MINORS) scale was completed for all included studies. Data evaluated included study design, study objectives, number of hips, injected product, duration of pain relief, and outcomes measured.
Results:
Our search yielded 8 studies involving 281 hips. Studies were categorized into diagnostic (4 studies), therapeutic (3 studies), and prognostic (1 study) applications. Patients with FAI and its degenerative sequelae obtained greater relief from diagnostic intra-articular hip injection than those without (P < .05). The diagnostic intra-articular injection performed under ultrasound guidance was better tolerated than injections performed under fluoroscopic guidance (pain rating, 5.6 vs 3.0; P < .1). Intra-articular injection of hyaluronic acid was the most effective at providing pain relief (in 23 patients), with significant improvements of functional outcome measures (Harris Hip Score, visual analog scale) present at 12 months. Pooled results with corticosteroid injection resulted in improvement in only 15% (9/60) of patients at 6 weeks. A negative response to intra-articular hip injection was a strong predictor for poor surgical outcomes.
Conclusion:
The results of this review suggest that (1) pain relief obtained from an intra-articular hip injection supports a diagnosis of FAI, (2) therapeutic relief at 12 months may be achieved, particularly with hyaluronic acid, and (3) a negative response to preoperative injections may predict poor short-term surgical outcomes. Additional large studies are required to build on the small number of studies included in this review, and further delineate the role of intra-articular hip injection in the management of FAI.
Keywords: femoroacetabular impingement, hip impingement, intra-articular injection
Femoroacetabular impingement (FAI) is characterized by abnormal mechanical contact between the acetabular rim (pincer impingement) or proximal femur (cam impingement) and is increasingly recognized as a potential cause of early hip osteoarthritis and labral cartilage pathology.11,18 Intra-articular hip pain related to FAI often presents as groin pain, or less commonly, as pain in the buttocks or low back.15 However, being able to confidently attribute a patient’s symptoms to FAI remains a diagnostic challenge even after clinical evaluation and imaging.6,8,42 Physical examination maneuvers such as FABER (flexion, abduction, external rotation) and FADIR (flexion, adduction, internal rotation) are of low sensitivity and specificity.12,30 The sensitivities of radiographic evaluation often depend on the projection considered and can be quite low.16 Furthermore, the prevalence of asymptomatic FAI morphology on radiographs and magnetic resonance arthrography (MRA) has been found to be approximately 15% in the general population19,24 and even higher in athletes.25,30
Given that several recent studies have demonstrated a high prevalence of morphologic abnormalities associated with FAI in asymptomatic individuals, the use of diagnostic injection to localize the source of a patient’s pain is often beneficial.25,37 Fluoroscopic or ultrasound-guided anesthetic diagnostic intra-articular hip injections have been commonly utilized to improve accuracy of diagnosis, with the aim of differentiating intra-articular hip pain from extra-articular sources through the relief of symptoms.23,29,31 For example, Byrd and Jones12 reported 90% accuracy of a positive response to injection, which correlated with intraoperative findings on hip arthroscopy. The purpose of this systematic review is to evaluate the utility of hip injection in patients with FAI with regard to diagnostic, prognostic, and therapeutic uses.
Methods
Identification of Studies
Two reviewers independently and in duplicate searched MEDLINE, PubMed, and EMBASE for studies that utilized intra-articular hip injections prior to surgical intervention for FAI. The search strategy combined the following terms: femoral acetabular impingement, hip impingement, and intra-articular injection. Medical Subject Headings (MeSH) and EMTREE headings and subheadings were used in various combinations in OVID and supplemented with free text to increase sensitivity. The search strategy was adapted to PubMed to include electronic publications ahead of print. Articles published between January 1974 and January 2014 from EMBASE and between January 1946 and January 2014 from MEDLINE were searched. Consulting with experts, hand-searching the references of eligible full-text articles, and browsing the “related articles” feature in PubMed were all used to identify additional eligible studies.
Disagreement regarding data and study inclusion was resolved by discussion and consensus with the senior author (O.R.A.).
Assessment of Study Eligibility
Studies meeting the following inclusion criteria were included in the review: studies involving (1) more than 5 patients, (2) adult patients aged 16 to 50 years, (3) involving (arthroscopic) femoroacetabular impingement surgery, (4) intra-articular hip injections, (5) reporting of clinical or radiographic outcomes, (6) human studies, and (7) articles published in English.
The exclusion criteria were as follows: (1) commentaries, review articles, case reports, basic science studies (except review article references); (2) studies reporting on nonarthroscopic hip surgery; and (3) cadaveric/nonhuman studies.
Assessment of Methodological Quality
Two reviewers independently assessed the methodological quality of all included studies. Observational studies were evaluated with the Methodological Index for Non-Randomized Studies (MINORS), which was developed and validated by Slim et al.38 The ideal MINORS score for comparative studies is 24, and 16 for noncomparative studies. All studies were graded for the level of evidence according to the criteria of Wright and Swiontkowski.44
Data Abstraction
Data were collected and recorded independently by each of the reviewers in a piloted computer spreadsheet program (Microsoft Excel 2013). Abstracted data included the following: number of patients, study design, number of hips, imaging modality used, injected product, pain relief, duration of pain relief, article type, injection method, study objectives, outcome measured, and correlation between imaging and operative findings.
Data Analysis
All data abstracted from eligible studies were organized into a table. Descriptive statistics were calculated to reflect the frequency of outcome measures.
The kappa (κ) statistic was used to examine interobserver agreement for study eligibility. Based on the guidelines of Landis and Koch,28 a κ of 0-0.2 represented slight agreement; 0.21-0.40, fair agreement; 0.41-0.60, moderate agreement; and 0.61-0.80, substantial agreement. A value greater than 0.80 was considered almost perfect agreement. Interobserver agreement for methodological quality assessment was calculated using the intraclass correlation coefficient (ICC). Both the κ and ICC were calculated using SPSS statistical analysis software (SPSS Inc).
Results
Study Identification
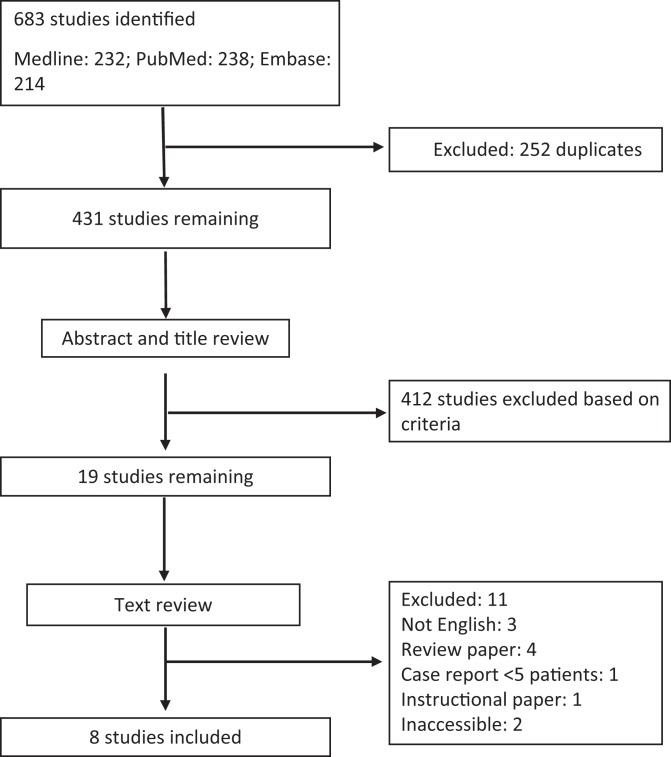
The initial search retrieved 683 studies, of which 19 initially met the inclusion criteria (Figure 1). However, 3 studies were not available in English, 4 were review articles, 1 was an instructional paper, 1 was a small case report, and 2 studies were inaccessible. Therefore, 8 studies were included in this review. For overall agreement between reviewers for the final eligibility decision, κ was 0.64 (95% CI, 0.58-0.69), indicating substantial agreement.
Figure 1.
Search method.
Study Characteristics
All of the included studies in this systematic review were conducted between 2010 and 2014. There were a total of 281 patients and 281 hips injected in these 8 studies. The studies were conducted in Italy (n = 2), the United States (n = 4), Canada (n = 1), and Taiwan (n = 1). The mean sample size per study was 35.1 (range, 6-72). Studies were divided into categories of diagnostic (n = 4), therapeutic (n = 3), or prognostic (n = 1). There were 6 cohort studies (level 2) and 2 case series (level 4). The quality of the included studies was assessed using the MINORS score. The mean score for noncomparative studies was 11 of 16 points (range, 11-13). Scores for noncomparative studies can be understood as: 0-4, very low quality; 5-8, low quality; 9-12, moderate quality; and 13-16, high quality. The mean score for comparative studies was 17.3 of 24 points (range, 16-18). Scores for comparative studies can be understood as: 0-6, very low quality; 7-12, low quality; 13-18, moderate quality; and 19-24, high quality. Agreement between reviewers in the assessment of study methodology was excellent (ICC, 0.94; 95% CI, 0.72-0.99).
In the studies reviewed, morphology consistent with FAI was confirmed by either radiograph alone (n = 1), magnetic resonance imaging (MRI) alone (n = 1), radiographs and MRA (n = 4), or MRA followed by arthroscopic confirmation (n = 2). In 2 articles, the definitive diagnostic method was not stated.
Hip injections were administered either freehand under ultrasound guidance (n = 5) or fluoroscopic guidance (n = 3) or with a fixed-hand ultrasound-guided technique (n = 1) (Table 1).
TABLE 1.
Study Characteristicsa
| Author (Year) | Study Design | MINORS Score | Study Objectives | No. of Hips | Imaging Modality for FAI Diagnosis | Injected Product | Injection Method | Pain Relief From Injection | Correlation Between Injection and Imaging | Conclusion |
|---|---|---|---|---|---|---|---|---|---|---|
| Diagnostic | ||||||||||
| Kivlan et al (2010)26 | Case series, comparative | 17 | To compare percentage relief from IAHI in patients with FAI | 72 | MRA and arthroscopically confirmed | 6 mL 1% lidocaine, 6 mL 0.25% bupivacaine, 80 mg triamcinolone | Fluoroscopic guidance | Mean pain relief for patients with FAI (85%) vs no FAI (64%) | NA | Patients with FAI and its degenerative sequelae obtained greater relief from diagnostic intra-articular hip injection than those without |
| Hsu et al (2012)21 | Cohort study, comparative | 18 | Identify factors influencing discomfort during US-guided hip injection | 44 | Not stated | Mixture of gadopentenate dimeglumine, iopromide, 2% lidocaine | Fixed guided US and freehand US | NA | NA | Procedure time is the most important factor in influencing hip discomfort |
| Martini et al (2012)30 | Cohort study, comparative | 18 | Compare diagnostic accuracy of MRA with contrast vs MRA with HA | 18 | Radiographs and MRA | 60 mg HA vs 12 mL paramagnetic contrast agent | Freehand US guidance | NA | IAHI of HA viscosupplementation had similar diagnostic value to conventional MRA | MRA with intra-articular injection of HA had similar diagnostic value to conventional MRA, allowing therapy to be combined with diagnosis |
| Byrd et al (2014)13 | Cohort study, comparative | 16 | Compare patient satisfaction between US- and fluoroscopically guided IAHI | 12 | Not stated | 40 mg methylprednisolone + 0.25% bupivacaine or 1% lidocaine | Freehand US guidance | NA | NA | US-guided IAHI was less painful for patients and more convenient than when fluoroscopically guided |
| Therapeutic | ||||||||||
| Hunt et al (2012)22 | Cohort study, noncomparative | 11 | Describe outcomes of conservative therapies for FAI | 6 | Radiographs and MRA | 40 mg triamcinolone + 1% lidocaine | Fluoroscopic guidance | 6/6 had relief at 1 y with activity modification | All patients with response to injection had diagnosis confirmed by MRA | Conservative management should be considered before surgery for FAI |
| Abate et al (2013)3 | Cohort study, noncomparative | 12 | Report on hip pain and function after US-guided injection of HA | 23 | Radiographs | 32 mg HA | Freehand US guidance | 23/23 had relief at 1 y | NA | HA provides good results of increased hip range of motion and function |
| Krych et al (2014)27 | Case series, noncomparative | 12 | Assess and compare the efficacy of therapeutic intra-articular steroid injections | 54 | MRI | 40 mg methylprednisolone or 40 mg/mL triamcinolone or 6 mg/mL betamethasone + local anesthetic | Freehand US or fluoroscopic guidance | 20/54 had significant pain relief at 14 d; 6/54 had relief at 6 wk | NA | IAHI of steroid injection has limited therapeutic benefit |
| Prognostic | ||||||||||
| Ayeni et al (2014)7 | Cohort study | 12 | Examine the predictive value of relief from IAHI on surgical outcomes for FAI | 52 | Radiographs, MRA, and arthroscopically confirmed | 0.25% bupivacaine + 40 mg of methylprednisolone acetate | Fluoroscopic guidance | 28/52 had pain relief from injection and improved HHS ratings at 6 mo postsurgery | NA | A negative response to IAHI may predict poor outcomes after FAI surgery |
aFAI, femoroacetabular impingement; HA, hyaluronic acid; HHS, Harris Hip Score; IAHI, intra-articular hip injection; MINORS, Methodological Index for Non-Randomized Studies; MRA, magnetic resonance arthrography; MRI, magnetic resonance imaging; NA, not applicable; US, ultrasound.
Diagnostic Studies
Four studies were identified evaluating the diagnostic application of intra-articular hip injection.13,21,26,30 In 3 of these studies, intra-articular hip injection was administered under ultrasound guidance, and fluoroscopically in 1 study.
In a diagnostic role, it was determined by Kivlan et al26 that patients with FAI obtained greater pain relief from intra-articular steroid injection (triamcinolone, 80 mg) than those without FAI (mean relief, 85% vs approximately 64%, respectively). Pain relief from the injection in this study was graded on a continuous scale from 0% to 100% and assessed during a 2-hour time window. It was also found that patients with degenerative sequelae of FAI, such as acetabular cartilage delamination, obtained significantly greater pain relief than patients who did not have chondral pathology (91% vs 76% relief; P < .05). Coexisting pathology from extra-articular sources (such as iliopsoas, bursae, or gluteal muscles) did not lessen the percent relief obtained from intra-articular injection, and accordingly, did not alter the diagnostic value of the intra-articular hip injection.
In the study by Byrd et al,13 patients who had undergone ultrasound and prior fluoroscopically guided intra-articular hip injection (of local anesthetic plus 1 mL of 40 mg/mL methylprednisolone) were asked to compare the procedures. Patients reported clinic-based ultrasound-guided injections to be significantly more convenient and less painful than hospital-based fluoroscopic injections, and this method was preferred by 98% of patients (P < .01). This study did not specify a postinjection time frame during which the pain relief obtained was assessed.13
Hsu et al21 sought to identify factors that cause discomfort during ultrasound-guided intra-articular injection. In their study (n = 44 hips), a contrast agent was injected using either a freehand or fixed-hand ultrasound-guided technique. It was found that discomfort was significantly (P < .001) related to the time required for needle manipulation (4.0 ± 0.9 vs 19.4 ± 17.6 seconds) and total procedure time, which were less when using a fixed-hand technique.21
The study by Martini et al30 (n = 18 hips) compared the diagnostic results of MRA performed using intra-articular hyaluronic acid to conventional MRA that was performed using gadolinium contrast. All images obtained using MRA with hyaluronic acid allowed for satisfactory assessment of the parameters for radiological diagnosis without statistical difference between the 2 types of MRA.30
Therapeutic
Three studies involving 83 hips evaluated the efficacy of therapeutic intra-articular steroids (60 patients; 54 patients in the study by Krych et al27 and 6 patients in the study by Hunt et al22) and hyaluronic acid (23 patients in the study by Abate et al3) in patients with FAI. Patients received a corticosteroid (ie, 40 mg triamcinolone, 40 mg methylprednisolone, 6 mg betamethasone) combined with a local anesthetic or hyaluronic acid alone (ie, 32 mg hyaluronic acid). Patients were followed up to 1 year3,22 and up to 6 weeks.27 Pooled results of these studies demonstrated intra-articular injection of hyaluronic acid provided clinically significant improvement in visual analog scale (VAS) and Harris Hip Score (HHS) outcomes for all patients (23/23), with relief sustained at 12 months (P < .05). In the study by Abate et al,3 hyaluronic acid therapy also contributed to decreased utilization of oral nonsteroidal anti-inflammatory medication by more than 50% in 10 of 23 patients.
Pooled results of 2 studies evaluating corticosteroid injections found that only 15% (9/60) of patients had significantly decreased pain and found improvement in their numeric pain score, HHS, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and numeric rating scale outcomes at 6 weeks.22,27 The study by Krych et al27 found the mean duration of significant pain relief to be 9.8 days, and only 6% (3/54) of patients had relief at 6 weeks. The type of corticosteroid used did not cause any significant difference in pain relief observed, and all patients in this study went on to have hip arthroscopy. In the study by Hunt et al,22 all 6 patients achieved significant pain relief that was still present 12 months after therapeutic injection. All 6 patients were satisfied with nonoperative treatment. The patients in the study by Krych et al27 were instructed to return to full activity, while patients in the study by Hunt et al22 were advised to avoid aggravating activities.
Prognostic
One study reported on the role of intra-articular injections in predicting functional outcomes and operative findings.7 Ayeni et al7 examined the predictive value of relief obtained from intra-articular injection (5 mL 0.25% bupivacaine with 40 mg methylprednisolone) and subsequent successful arthroscopic FAI management. In this study, a positive response to injection was defined as any degree of pain reduction achieved within 2 weeks after the injection. Forty-two of 52 (81%) patients experienced early pain relief from the intra-articular injection and scored >70 on the modified HHS. However, only 28 of those patients who responded positively to injection had scores >70 at 6 months postsurgery (28/52; 54%). Those patients who had a negative outcome postsurgery (modified HHS score <70) complained of pain in the perioperative sites (hip flexors and abductors). None of these patients underwent repeat surgery. A positive result from an intra-articular hip injection presurgery was determined to be a weak prognostic factor for successful arthroscopic FAI management (likelihood ratio 1.15 for positive test). The authors noted that a negative response from an intra-articular hip injection was a stronger predictor of a poorer surgical outcome (likelihood ratio, 0.57).7
Discussion
This systematic review is the first to evaluate the role of the intra-articular hip injection in the diagnosis, treatment, and prognosis of FAI. This condition has only recently become a recognized cause of hip pain. Accordingly, there is a paucity of high-quality studies pertaining to the accurate diagnosis and management of this condition. This is the case for our systematic review, in which we were able to find only a small number of studies for each role of the intra-articular hip injection.
With fewer studies, the quality of each included study becomes increasingly important. In our review, because of the lack of available data, some conclusions pertaining to the specific role of intra-articular hip injections were based on individual studies. The current state of the evidence is such that all studies included in our review were of moderate quality as assessed by the MINORS score. For this reason, conclusions drawn from these individual studies must be interpreted with caution.
Previous studies have examined the use of the intra-articular injection in identifying various intra-articular hip pathologies. Byrd and Jones12 demonstrated that fluoroscopically guided intra-articular hip joint injections are 90% accurate in the diagnosis of intra-articular hip pathology, including labral tears and ligamentum teres rupture. Pateder and Hungerford35 demonstrated 100% sensitivity and 81% specificity for injections to distinguish hip versus spine pain. Although it can reliably differentiate intra-articular pathology from extra-articular pathology, the clinician should bear in mind that the diagnosis of FAI is formulated on the basis of a patient’s history, physical examination, imaging, and other supporting tests, which include the intra-articular hip injection. Thus, the response to an injection on its own is not sufficient to diagnose FAI.
In their review, Kivlan et al26 found that pain relief obtained from an intra-articular hip injection supports a diagnosis of FAI and that the concurrent presence of extra-articular pathology did not significantly lessen the percent pain relief achieved from injection. The clinician may wonder how the diagnostic injection can differentiate between intra- and extra-articular pain sources if the percent relief obtained is comparable. It is possible that extra-articular hip pain may still be the primary source of pain, despite intra-articular findings. Alternatively, pain that is not relieved by intra-articular injection may indicate pain generating from extra-articular sources. Another explanation may be that extra-articular pathology is asymptomatic and incidental to intra-articular findings. Last, the diagnostic injection may help discriminate symptomatic from asymptomatic intra-articular pathology, especially in patients with suspicion of both intra- and extra-articular involvement.
Patients in the study by Kivlan et al26 had already been evaluated extensively through physical examination and imaging prior to receiving the diagnostic injection, and the pretest suspicion for FAI was already high.26 Therefore, the study sample did not represent a generalized population of patients with hip pain, and the value of an intra-articular hip injection may vary depending on when in the diagnostic algorithm the injection is utilized.
In this review concerning FAI, it was found that in a diagnostic role, consideration should be given to the use of ultrasound-guided technology. Previous studies have cited ultrasound-guided intra-articular hip injection as a viable and increasingly popular alternative to fluoroscopic guidance for several reasons, including accessibility, compact size, lack of ionizing radiation exposure, superior visualization of soft tissue structures, and greater accuracy of delivery.4,32,33,39–41 This trend toward its increased popularity in the general literature is something that was found in the search specific to FAI as well.39,40 Two studies in this review suggest that ultrasound-guided injections are less painful and less inconvenient for patients than fluoroscopically guided intra-articular hip injection.12,13 Care should be taken to minimize needle manipulation and procedure duration, as these factors play the largest role in patient discomfort. In the study by Byrd et al,13 patients were asked to compare ultrasound-guided injections to fluoroscopic injections they had previously undergone, introducing recall bias to the study’s findings. Last, MRA can be performed after intra-articular injection of a therapeutic agent (such as hyaluronic acid) rather than a contrast agent because both forms of MRA allow for proper assessment of imaging parameters. This allows diagnosis and therapy to be combined into a single session and possibly replaces the need for a contrast agent.13,21,30
It was found that intra-articular hyaluronic acid is a well-tolerated therapy for FAI and may provide significant pain relief and functional improvement at 12 months. In the study by Abate et al,3 none of the patients who received an intra-articular injection of hyaluronic acid underwent surgery at 12 months. This has particular clinical relevance as it may allow patients to delay the surgical option and also contributes to reduction in oral nonsteroidal anti-inflammatory drug consumption and their systemic effects. A control group was lacking from this study, and the effect of placebo cannot be excluded. Several studies have reported hyaluronic acid as efficacious in the therapy of hip osteoarthritis and rheumatoid arthritis.1,4,33 However, joints other than the knee have not yet been approved by the Food and Drug Administration (FDA) for intra-articular hyaluronic acid injection, and the management of FAI with hyaluronic acid requires further investigation.
The therapeutic benefit of corticosteroids in FAI, however, is less clear, as Kyrch et al27 noted that only 37% of patients had significantly diminished pain at 2 weeks post–corticosteroid injection, and only 6% of patients had sustained relief at 6 weeks. In the study by Hunt et al,22 all 6 patients avoided surgery, and at 1 year follow-up, were satisfied with nonoperative management that included physiotherapy, activity modification, and a therapeutic corticosteroid injection. This difference in activity restrictions may account for the contrasting findings of Krych et al27 and Hunt et al.22 Also, the retrospective study by Krych et al27 only included patients that eventually underwent hip arthroscopy and were unsatisfied with the therapeutic relief of injection. Given that all these patients had failed nonoperative management, this population may represent a subset of patients with more severe FAI, and the results cannot be applied to milder FAI or the entire spectrum of patients with FAI. A control group of patients that may have achieved satisfactory relief with the injection was not included. Multiple radiologists provided the intra-articular hip injection under both ultrasound and fluoroscopy, introducing technical variability into the study. The heterogeneity of patient groups, severity of pathology, and overall treatment strategies employed in these studies makes it challenging to draw firm conclusions regarding the benefit of corticosteroids.
A systematic review by Samora et al36 reported that full return to sports in patients with FAI is only possible after surgical management. However, recent studies included here were not part of that review and indicate that a trial of conservative management should be considered initially. This is especially the case if there are contraindications to surgery or a need for its delay. Wall et al43 examined nonoperative management strategies for FAI and the evidence for their support. They determined from their systematic review that physical therapy and activity modification offer some benefit to patients. Other treatment strategies such as nonsteroidal anti-inflammatory drugs have been mentioned and promoted in several discussion articles. However, there is a paucity of strong evidence-based advice and clinical trials evaluating nonoperative management, and it is likely that much of what is present in the available literature is based on expert opinion.43 Further studies will need to evaluate dosing of the therapeutic agent, activity modification postinjection, and its safety in pediatric populations prior to the intra-articular injection becoming standard of care.
Patients often inquire about the risks of masking symptoms with a therapeutic intra-articular hip injection rather than correcting the mechanical conflict of the hip. Retrospective studies of patients who had already developed hip osteoarthritis have shown an association between hip osteoarthritis and FAI morphology.5,14,17 However, these studies did not show an association between hip osteoarthritis and FAI symptoms such as groin pain or the severity of FAI morphology and the development of osteoarthritis. Prospective studies are now beginning to appear in the literature to address this common question. In a group of 43 hips with cam morphology who had already developed mild hip osteoarthritis, one-third of hips showed no progression of osteoarthritis after 10 years.9 In another study of 96 hips with asymptomatic FAI morphology on imaging, patients were followed for a mean 18.5 years. It was found that 82% of hips did not develop osteoarthritis or symptoms.20 With this in mind, the clinician should explain to the patient that for the time being, there is not enough supporting evidence to state that FAI morphology will certainly lead to the development of osteoarthritis, its severity, or when it may occur.
The response to an intra-articular hip injection provides valuable information in predicting intra-articular pathology, surgical findings, and functional outcomes, which can in turn aid the surgeon in decision making and patient education. The results of the study by Ayeni et al7 contradict assumptions by patients and surgeons that pain relief obtained from an intra-articular injection is indicative of satisfactory outcomes after surgery. On the contrary, a negative response from an intra-articular hip injection is a stronger predictor of a poorer surgical outcome. As such, patients should be clearly informed of the role of the intra-articular injection in supporting the diagnosis of FAI and in predicting and planning subsequent management. Patients and their surgeons should be cognizant that even with a positive response to injection, pain may remain postoperatively in cases of inadequate decompression, articular cartilage injury, inappropriate rehabilitation, or many other reasons. The findings of Ayeni et al7 and Kivlan et al26 support each other in that if pain persists after diagnostic intra-articular hip injection and hip arthroscopy, an extra-articular source should be considered.
Strengths and Limitations
There are multiple strengths to this systematic review. The literature search was extensive, and multiple reviewers were involved in article screening, assessment, and data abstraction. There was strong agreement for study inclusion. References of recent reviews and the included articles were also searched to be comprehensive. Furthermore, eligibility criteria were broad enough to capture the various uses of the intra-articular hip injection as it relates to FAI.
This review has limitations that must be acknowledged. This review was composed of a small number of observational studies, and many of these studies involved relatively small sample sizes and lacked a control population. Some conclusions were based on individual studies. The patient populations were diverse, and in some studies, for example, only patients with mild FAI were included. The heterogeneity of included studies made it difficult to pool data for a meta-analysis and for making of specific recommendations. For example, in pooled results of studies utilizing corticosteroids, heterogeneity of patient traits did not allow for definitive conclusions. Patients often receive therapeutic hip injections while being instructed to follow activity restrictions and limit hip-aggravating movements. This makes it difficult to attribute pain relief solely to the injection. However, patients have often already tried activity modification and physical therapy before an injection is considered, and so the therapeutic use of an injection should not be seen as diminished. Each study had different definitions of positive response to injection, which needed to be taken into account. In a small number of studies, patients had both FAI and intra-articular pathology such as labral tears. This was specified where it is the case. Finally, this systematic review was composed of observational studies, which are at risk of various types of bias, such as large numbers lost to follow-up or lack of blinding. Nevertheless, many studies included here enrolled consecutive patients to decrease the potential risk of selection bias.
Implications for Future Research
Based on the results of this review, future studies should focus on the efficacy of injections when diagnosing and treating FAI. There is also a need for additional large trials showing the long-term safety and efficacy of hyaluronic acid for intra-articular hip pathology. Joints other than the knee have not been approved by the FDA for intra-articular hyaluronic acid injection. This is a considerable obstacle given that hyaluronic acid is a potential treatment option for FAI and has been used in the treatment of osteoarthritis and rheumatoid arthritis.2,10,32,34 The further development of parameters for contrast-enhanced ultrasound imaging will also be helpful in reducing the need for more costly imaging such as MRA.
Conclusion
Intra-articular hip injections have a role in the diagnosis, therapy, and prognostication of FAI. The results of this review suggest that pain relief obtained from an injection supports a diagnosis of FAI. Ultrasound may be the preferred and increasingly popular method of performing and receiving an intra-articular injection. MRA can be performed after hyaluronic acid injection in the same session because it can be diagnostic and comparable with conventional MRA with MR contrast agent. Therapeutic relief up to 12 months can be achieved, particularly with hyaluronic acid. However, it is difficult to recommend other agents based on heterogeneity of pooled results. Finally, intra-articular hip injection is useful in providing prognostic information on short-term outcomes with regard to outcomes following FAI surgery.
Footnotes
Declaration of Conflicting Interests: The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Abate M, Pelotti P, De Amicis D, Di Iorio A, Galletti S, Salini V. Viscosupplementation with hyaluronic acid in hip osteoarthritis (a review). Ups J Med Sci. 2008;113:261–277. [DOI] [PubMed] [Google Scholar]
- 2. Abate M, Pulcini D, Di Iorio A, Schiavone C. Viscosupplementation with intra-articular hyaluronic acid for treatment of osteoarthritis in the elderly. Curr Pharm Des. 2010;16:631–640. [DOI] [PubMed] [Google Scholar]
- 3. Abate M, Scuccimarra T, Vanni D, Pantalone A, Salini V. Femoroacetabular impingement: is hyaluronic acid effective? Knee Surg Sports Traumatol Arthrosc. 2014;22:889–892. [DOI] [PubMed] [Google Scholar]
- 4. Atchia I, Kane D, Reed MR, Isaacs JD, Birrell F. Efficacy of a single ultrasound-guided injection for the treatment of hip osteoarthritis. Ann Rheum Dis. 2011;70:110–116. [DOI] [PubMed] [Google Scholar]
- 5. Audenaert EA, Peeters I, Van Onsem S, Pattyn C. Can we predict the natural course of femoroacetabular impingement? Acta Orthop Belg. 2011;77:188–196. [PubMed] [Google Scholar]
- 6. Ayeni OR, Belzile EL, Musahl V, et al. Results of the perception of femoroacetabular impingement by surgeons survey (PROCESS). Knee Surg Sports Traumatol Arthrosc. 2014;22:906–910. [DOI] [PubMed] [Google Scholar]
- 7. Ayeni OR, Farrokhyar F, Crouch S, Chan K, Sprague S, Bhandari M. Pre-operative intra-articular hip injection as a predictor of short-term outcome following arthroscopic management of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2014;22:801–805. [DOI] [PubMed] [Google Scholar]
- 8. Ayeni OR, Wong I, Chien T, Musahl V, Kelly BT, Bhandari M. Surgical indications for arthroscopic management of femoroacetabular impingement. Arthroscopy. 2012;28:1170–1179. [DOI] [PubMed] [Google Scholar]
- 9. Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br. 2009;91:162–169. [DOI] [PubMed] [Google Scholar]
- 10. Battaglia M, Guaraldi F, Vannini F, et al. Efficacy of ultrasound-guided intra-articular injections of platelet-rich plasma versus hyaluronic acid for hip osteoarthritis. Orthopedics. 2013;36:e1501–e1508. [DOI] [PubMed] [Google Scholar]
- 11. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. [DOI] [PubMed] [Google Scholar]
- 12. Byrd JW, Jones KS. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32:1668–1674. [DOI] [PubMed] [Google Scholar]
- 13. Byrd JW, Potts EA, Allison RK, Jones KS. Ultrasound-guided hip injections: a comparative study with fluoroscopy-guided injections. Arthroscopy. 2014;30:42–46. [DOI] [PubMed] [Google Scholar]
- 14. Clohisy JC, Dobson MA, Robison JF, et al. Radiographic structural abnormalities associated with premature, natural hip-joint failure. J Bone Joint Surg Am. 2011;93(suppl 2):3–9. [DOI] [PubMed] [Google Scholar]
- 15. Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467:638–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Domayer SE, Ziebarth K, Chan J, Bixby S, Mamisch TC, Kim YJ. Femoroacetabular cam-type impingement: diagnostic sensitivity and specificity of radiographic views compared to radial MRI. Eur J Radiol. 2011;80:805–810. [DOI] [PubMed] [Google Scholar]
- 17. Ecker TM, Tannast M, Puls M, Siebenrock KA, Murphy SB. Pathomorphologic alterations predict presence or absence of hip osteoarthrosis. Clin Orthop Relat Res. 2007;465:46–52. [DOI] [PubMed] [Google Scholar]
- 18. Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed] [Google Scholar]
- 19. Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg. 2010;92:2436–2444. [DOI] [PubMed] [Google Scholar]
- 20. Hartofilakidis G, Bardakos NV, Babis GC, Georgiades G. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J Bone Joint Surg Br. 2011;93:580–586. [DOI] [PubMed] [Google Scholar]
- 21. Hsu YC, Wu YC, Kao HL, Pan RY, Lee MS, Huang GS. Factors influencing discomfort during anterior ultrasound-guided injection for hip arthrography. J Chin Med Assoc. 2013;76:510–516. [DOI] [PubMed] [Google Scholar]
- 22. Hunt D, Prather H, Harris Hayes M, Clohisy JC. Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of prearthritic, intra-articular hip disorders. PM R. 2012;4:479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jacobson JA, Bedi A, Sekiya JK, Blankenbaker DG. Evaluation of the painful athletic hip: imaging options and imaging-guided injections. AJR Am J Roentgenol. 2012;199:516–524. [DOI] [PubMed] [Google Scholar]
- 24. Jung KA, Restrepo C, Hellman M, AbdelSalam H, Morrison W, Parvizi J. The prevalence of cam-type femoroacetabular deformity in asymptomatic adults. J Bone Joint Surg Br. 2011;93:1303–1307. [DOI] [PubMed] [Google Scholar]
- 25. Kapron AL, Anderson AE, Aoki SK, et al. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS exhibit selection. J Bone Joint Surg Am. 2011;93:e111(1-10). [DOI] [PubMed] [Google Scholar]
- 26. Kivlan BR, Martin RL, Sekiya JK. Response to diagnostic injection in patients with femoroacetabular impingement, labral tears, chondral lesions, and extra-articular pathology. Arthroscopy. 2011;27:619–627. [DOI] [PubMed] [Google Scholar]
- 27. Krych AJ, Griffith TB, Hudgens JL, Kuzma SA, Sierra RJ, Levy BA. Limited therapeutic benefits of intra-articular cortisone injection for patients with femoro-acetabular impingement and labral tear. Knee Surg Sports Traumatol Arthrosc. 2014;22:750–755. [DOI] [PubMed] [Google Scholar]
- 28. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 29. Martin RL, Irrgang JJ, Sekiya JK. The diagnostic accuracy of a clinical examination in determining intra-articular hip pain for potential hip arthroscopy candidates. Arthroscopy. 2008;24:1013–1018. [DOI] [PubMed] [Google Scholar]
- 30. Martini C, Sconfienza LM, Ferrero G, Fabbro E, Orlandi D, Serafini G. RM-arthrography of hip joint after intra-articular injection of hyaluronic acid (HA). Comparison with conventional RM-arthrography in a group of patients affected by femoro-acetabular impingement. Skeletal Radiol. 2012;41:875. [Google Scholar]
- 31. Maslowski E, Sullivan W, Forster Harwood J, et al. The diagnostic validity of hip provocation maneuvers to detect intra-articular hip pathology. PM R. 2010;2:174–181. [DOI] [PubMed] [Google Scholar]
- 32. Mei-Dan O, McConkey MO, Petersen B, McCarty E, Moreira B, Young DA. The anterior approach for a non-image-guided intra-articular hip injection. Arthroscopy. 2013;29:1025–1033. [DOI] [PubMed] [Google Scholar]
- 33. Micu MC, Bogdan GD, Fodor D. Steroid injection for hip osteoarthritis: efficacy under ultrasound guidance. Rheumatology (Oxford). 2010;49:1490–1494. [DOI] [PubMed] [Google Scholar]
- 34. Mulvaney SW. A review of viscosupplementation for osteoarthritis of the hip and a description of an ultrasound-guided hip injection technique. Curr Sports Med Rep. 2009;8:291–294. [DOI] [PubMed] [Google Scholar]
- 35. Pateder DB, Hungerford MW. Use of fluoroscopically guided intra-articular hip injection in differentiating the pain source in concomitant hip and lumbar spine arthritis. Am J Orthop (Belle Mead NJ). 2007;36:591–593. [PubMed] [Google Scholar]
- 36. Samora JB, Ng VY, Ellis TJ. Femoroacetabular impingement: a common cause of hip pain in young adults. Clin J Sport Med. 2011;21:51–56. [DOI] [PubMed] [Google Scholar]
- 37. Schmitz MR, Bittersohl B, Zaps D, Bomar JD, Pennock AT, Hosalkar HS. Spectrum of radiographic femoroacetabular impingement morphology in adolescents and young adults: an EOS-based double-cohort study. J Bone Joint Surg Am. 2013;95:e90. [DOI] [PubMed] [Google Scholar]
- 38. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. [DOI] [PubMed] [Google Scholar]
- 39. Smith J, Hurdle MF. Office-based ultrasound-guided intra-articular hip injection: technique for physiatric practice. Arch Phys Med Rehabil. 2006;87:296–298. [DOI] [PubMed] [Google Scholar]
- 40. Smith J, Hurdle MF, Weingarten TN. Accuracy of sonographically guided intra-articular injections in the native adult hip. J Ultrasound Med. 2009;28:329–335. [DOI] [PubMed] [Google Scholar]
- 41. Sofka CM, Saboeiro G, Adler RS. Ultrasound-guided adult hip injections. J Vasc Interv Radiol. 2005;16:1121–1123. [DOI] [PubMed] [Google Scholar]
- 42. Tijssen M, van Cingel R, Willemsen L, de Visser E. Diagnostics of femoroacetabular impingement and labral pathology of the hip: a systematic review of the accuracy and validity of physical tests. Arthroscopy. 2012;28:860–871. [DOI] [PubMed] [Google Scholar]
- 43. Wall PD, Fernandez M, Griffin DR, Foster NE. Nonoperative treatment for femoroacetabular impingement: a systematic review of the literature. PM R. 2013;5:418–426. [DOI] [PubMed] [Google Scholar]
- 44. Wright JG, Swiontkowski MF. Introducing a new journal section: evidence-based orthopaedics. J Bone Joint Surg. 2000;82:759–760. [Google Scholar]