Abstract
Background:
The pathogenesis of fifth metatarsal stress fractures remains uncertain.
Hypothesis:
Physical characteristics and environmental factors, which have received limited attention in the literature thus far, might be involved in the development of fifth metatarsal stress fractures.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
To test the study hypothesis, a medical examination and survey of the living environment of collegiate soccer players was conducted and correlated with the existence of fifth metatarsal stress fractures. The survey and measurements were conducted in 273 male athletes from the same college soccer team between 2005 and 2013. A medical examination comprising assessment of stature, body weight, body mass index, foot–arch height ratio, toe-grip strength, quadriceps angle, leg-heel angle, functional reach test, single-leg standing time with eyes closed, straight-leg raise angle, finger-floor distance, heel-buttock distance, ankle joint range of motion, and a general joint laxity test were performed once a year, along with a questionnaire survey. The survey was also repeated when a fifth metatarsal stress fracture was diagnosed. The study participants were separated into a fifth metatarsal stress fracture injury group and a noninjury group. The measurement items and survey items were compared, and the association between the factors and the presence or absence of injuries was analyzed.
Results:
Toe-grip strength was significantly weaker in the injury group compared with the noninjury group, suggesting that weak toe-grip is associated with fifth metatarsal stress fracture (P < .05). In addition, fifth metatarsal stress fractures were more common in the nondominant leg (P < .05). Between-group comparisons of the other items showed no statistically significant differences.
Conclusion:
The association between weak toe-grip strength and fifth metatarsal fracture suggests that weak toe-grip may lead to an increase in the load applied onto the lateral side of the foot, resulting in stress fracture. The finding of stress fracture being more common in the nondominant leg needs further study.
Keywords: fifth metatarsal bone, stress fracture, soccer, medical checkup
Fifth metatarsal stress fractures occurring during soccer games are a relatively frequent injury because soccer is a sport that involves many cutting and side-step movements.3,6,11,20 Fifth metatarsal stress fractures often lead to delayed healing3,21 or pseudarthrosis,11,25,30,31 and occasionally, refracture after treatment.8,28 For this reason, in the management of fifth metatarsal stress fractures in highly active individuals such as sports players and athletes, insufficient treatment and rehabilitation have been reported to lead to nonunion, which makes it impossible for the athlete to return to sports.1,2,11 Therefore, it is important that the factors involved in the occurrence of fifth metatarsal stress fractures be examined to design an effective program of prevention, treatment, and rehabilitation.
In terms of the factors contributing to the occurrence of fifth metatarsal stress fractures, previous reports from anatomic research studies have shown that the base of the fifth metatarsal bone is strongly attached to the cuboid and the fourth metatarsal bones by ligaments.10 This may explain why fractures often occur at the base of the fifth metatarsal.10 Epidemiological studies have shown that, in professional soccer players, such fractures are more likely to occur in younger athletes and that excessive exercise is a risk factor.6 Biomechanical studies have shown that the causes of fifth metatarsal stress fractures include vertical and mediolateral stress11 as well as the traction force23 of the peroneus brevis muscle. Previous reports based on the physical factors associated with fifth metatarsal stress fractures indicated hindfoot varus12 and a high arch.22,27 However, as far as we know, there have been no previous reports of studies examining the association between the occurrence of fifth metatarsal stress fractures and the patient’s physical characteristics prior to occurrence or the association of such fractures with environmental factors (eg, ground surface, type of spiked cleats).
Therefore, in this prospective study, data were obtained from a medical examination (physical characteristics) and environmental assessment of college soccer players. Subjects who developed fifth metatarsal stress fractures during the follow-up period (injury group) were compared with those who did not (noninjury group). In addition, comparisons were performed based on the playing surface at the time of the injury and the presence or absence of a history of ankle sprain or foot injury. The environment factors associated with occurrence of fifth metatarsal stress fractures were evaluated.
Methods
Study Participants
This study was conducted in 273 soccer players (excluding goalkeepers) who were affiliated with a male soccer team at a single college during a 9-year period between 2005 and 2013. At the time of entrance to the college, subjects were a mean (±SD) age of 18.0 ± 0.2 years, with a mean height of 171.4 ± 14.0 cm, mean body weight of 64.7 ± 6.3 kg, mean body mass index (BMI) of 23.5 ± 16.2 kg/m2, and had played soccer as an athlete for a mean of 10.0 ± 2.1 years. In this study, the team coaches did not change during the study period, and the athletes affiliated with the team had been separated into categories by ability as they participated in practice sessions and matches. Approval for the study was obtained from the university’s ethics committee. Detailed explanations of the study protocol were provided to the staff and athletes, and the athletes gave consent to participate in the study.
Survey Items
In the month of April of every fiscal year, a survey was distributed to the players during a medical examination. The following items were assessed:
History of sports injuries to the foot or ankle sprain. Each athlete was questioned regarding a history of injuries to the foot prior to entering college (from the time the athlete started playing soccer until the time they graduated from high school) that resulted in an inability to play soccer for ≥1 week. For those who had a history of injuries to the foot or ankle, the following were recorded: site of injury, diagnosis, timing of the injury, frequency of the injury, duration of the period of inability to play soccer, and information on whether surgery was performed. For those whose answers were unclear, further questioning was conducted individually.
Dominant leg. During the study, the leg that each athlete preferred to use when kicking a ball was considered the dominant leg.
Footwear. The number and shape of studs in the spiked cleats used by the athletes for everyday practice were examined.
Survey of Patients With Fifth Metatarsal Stress Fracture Injuries
For those players who incurred a fifth metatarsal stress fracture, the following were additionally assessed:
Results of orthopaedic physical examination. In all cases, any fifth metatarsal stress fracture that occurred during the students’ years of enrollment at the college was examined.
Footwear. The number of studs, as well as the shape of the studs in the spiked cleats worn at the time of injury, were recorded.
Playing surface. The ground surface at the time of the injury was recorded. The primary environment used by the study participants’ soccer teams during practice was natural turf from fiscal year 2003 to fiscal year 2006 and artificial turf from fiscal year 2007 onward.
Athlete-Exposures and the Incidence of Fifth Metatarsal Stress Fracture
Athlete-exposures (AEs) from each season were calculated. In addition, AEs corresponding to the following periods were calculated: while practicing on natural turf (fiscal years 2004-2006), while practicing on artificial turf (fiscal years 2007-2012), when the participants were juniors (first and second years of college), and when the participants were seniors (third and fourth years of college). The incidence of fifth metatarsal stress fractures was calculated per 1000 AEs for each of these periods.
Measurement Items
The following items were examined in April of each fiscal year during a medical examination by the team physical therapist. Checkup items were selected from recommended items by the Japan Football Association.
Body Demographics
Height, body weight, and BMI were all recorded.
Foot–Arch Height Ratio
The foot length and the height of the navicular bone were measured using an electronic caliper while the participant was in a natural standing position. The foot–arch height ratio was calculated by dividing the height of the navicular bone by the foot length.
Toe-Grip Strength
With reference to measurement devices used in a previous study,19 a measuring instrument that incorporated a digital dynamometer (Takei Scientific Instruments Co Ltd) was created. This instrument has high reliability; there were no significant differences among 3 measurements in 115 healthy volunteers, and the intraclass correlation coefficient was 0.973. The digital dynamometer was fixed to a wooden foundation plate, and a 4-mm–diameter stainless wire was attached to the dynamometer (Figure 1). This served as a bar to be gripped with the toes. The participants sat upright on a chair without leaning on the backrest (both knees and hips were flexed approximately 90°) to obtain the toe-grip strength measurement.26 Measurements were conducted while the ankles and feet were in a neutral position. The position of the toes was checked to ensure that the toes (from the first to the fifth toe) were applied against the toe-grasping bar, and the measurements were carried out while the lower leg was attached to a fixing board at the anterior surface of the leg. However, some participants were not able to grip the bar with their fifth toe. In this case, the first toe was used as a benchmark to set up the measurement position. Measurements were conducted while the examiner immobilized the heel to ensure that no compensatory motion of the ankle joint occurred. The measurements were conducted 3 times, allowing the participants sufficient rest between measurements. The maximum value was considered the representative value.
Figure 1.
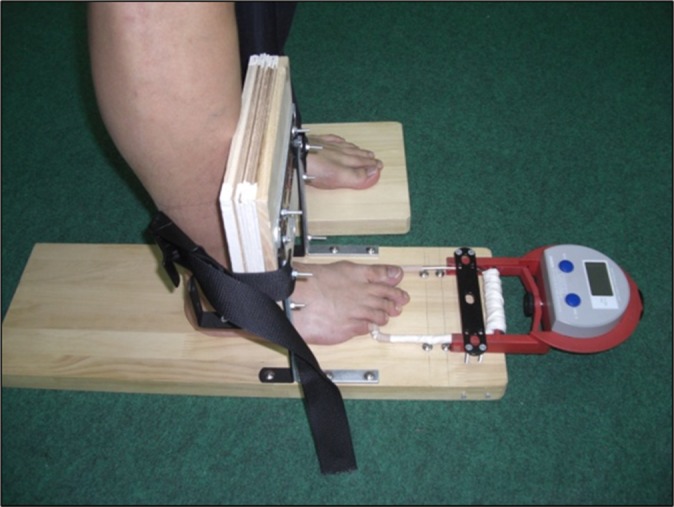
Toe-grip strength. The digital dynamometer was fixed to a wooden foundation plate, and a 4-mm–diameter stainless wire was attached to the area of the dynamometer, to which force would be applied. This served as a bar to be gripped with the toes. Measurements were conducted while both the ankles and feet were in a neutral position. The position of the toes was checked to ensure that the toes (from the first to the fifth toe) were applied against the toe-grasping bar, and the measurements were carried out while the lower leg was attached to a fixing board at the anterior surface of the leg.
Quadriceps Angle
The quadriceps angle (Q-angle) is formed by the connecting line from the anterior superior iliac spine to the center of the patella,13 with the connecting line from the center of the patella to the tibial tubercle. The Q-angle was measured in a neutral standing position using a goniometer.
Leg-Heel Angle
The angle formed by the long axis of the lower leg and the long axis of the calcaneus was measured in a neutral standing position using a goniometer.
Functional Reach Test
As a previous study reported,4 measurements were conducted to assess the ability to achieve dynamic postural control through toe-grip strength. Participants were instructed to stretch their hands forward in a standing posture and to press on a bar with their fingertips, allowing the bar to return to its original position, without letting their heel rise. The distance traveled by a bar placed vertically on a wall was measured.
Single-Leg Standing Time With Eyes Closed
Measurements were conducted for a maximum duration of 2 minutes as the participant joined both upper extremities in front of his chest while adopting a single-leg standing posture, keeping the eyes closed. Standing time was measured until the elevated part of the foot touched the ground or until a large compensatory motion was observed in both upper extremities as well as the trunk.
Straight-Leg Raising (SLR) Angle
To evaluate the flexibility of thigh flexor muscles, the angle of the hip joint in passive flexion was measured using a goniometer (Muranaka Medical Instruments Co Ltd) while the knee joint was left in extension.
Finger-Floor Distance (FFD)
To evaluate the flexibility of the spinal muscle groups, the lumbar region was placed in maximum flexion while both knee joints were in extension, and the distance between the fingertips and the floor was measured.
Heel-Buttock Distance (HBD)
To evaluate the flexibility of the quadriceps muscles, the knees were passively placed in flexion while the participant was in a prone position; the distance between the heels and the buttocks was measured when the buttocks started to rise from the floor.
Ankle Joint Range of Motion
The range of dorsiflexion of the ankle and the range of plantar flexion of the ankle were measured in a supine position using a goniometer (Tokyo University).
General Joint Laxity Test
Laxity testing was conducted on 6 joints, considered to be representative of the entire body (wrist, elbow, shoulder, hip, knee, and ankle) as well as the spinal column.29 These 7 items included thumb to forearm position, elbow hyperextension >15°, shoulder hyperrotation, hyperexternal rotation of the hip >90° in standing position, knee hyperextension >10°, ankle hyperdorsiflexion >45° in knee flexion, and anteflexion of the trunk. Positive shoulder hyperrotation was defined when participants could grasp their hands from both the cranial and caudal sides on their back. Positive hyperexternal rotation of the hip was defined when participants could maintain their toes at 180° of external rotation with the lower legs in an extended position. Positive forward flexion of the trunk was defined when participants could touch the floor with the bilateral palms of their hands while maintaining the lower leg in an extended position. For each item, a score of 1 point was given when the range of motion reached or exceeded baseline. The wrist, elbow, shoulder, knee, and ankle were 0.5 points on each side. Total scores were calculated. The maximum total score was 7.
Comparison
Study participants were divided into 2 groups. Participants who suffered from stress fracture of the fifth metatarsal were included in the injury group, and others were included in the noninjury group. One participant who had previous surgery for a stress fracture of the fifth metatarsal was included in the injury group. The foot of the injured participants in the injury groups was observed in either the dominant or nondominant leg. Furthermore, the occurrence of ankle sprain and foot disorder was also observed in the dominant or nondominant leg. For that reason, study participants were further divided into an injury foot group and noninjury foot group. The injury group and injury foot group were defined as injured players or the injured side of the foot, respectively. The noninjury group was defined as the nondominant leg of the noninjured players or players who were not injured. The noninjury foot group was defined as the sum of both feet in players who were not injured, as well as the noninjury side of the foot of the injured players.
The following comparisons were carried out between the injury and the noninjury foot groups and between the injury and the noninjury groups. In the between-group comparison of foot injury, comparisons were carried out between the dominant and nondominant legs and the presence of a history of sports injuries to the foot or of ankle sprain. Between the injury and the noninjury group, comparisons were carried out in terms of the number of studs in the spiked cleats, as well as the morphology of the studs. In the injury group, the spiked cleats used in the comparison were those worn at the time of the injury. In the noninjury group, the spiked cleats used in the comparison were those that the subject reported using most frequently during their years of enrollment at the college, or those that they used during their final year.
The incidence of fifth metatarsal stress fractures was calculated for the groups, and comparisons were conducted between the incidence for senior students versus juniors and for athletes playing on natural versus artificial turf. Statistical analyses were conducted using the chi-square test or Fisher exact test.
Statistical Analysis
In the injury and noninjury groups, all variables measured at the time of the participants’ admission to college were compared. Statistical analyses were conducted using the Mann-Whitney U test. In addition, the presence or absence of a fifth metatarsal stress fracture was used as a dependent variable; height, body weight, foot–arch height ratio, toe-grip strength, Q-angle, leg-heel angle, functional reach test, single-leg standing time with eyes closed, SLR angle, FFD, HBD, ankle dorsiflexion angle, ankle plantar flexion angle, and general joint laxity results were used as independent variables. The association between these variables was examined using logistic regression analysis. All statistical analyses were conducted using SPSS version 11.0 (SPSS Japan Inc), and the significance level was set at P < .05.
Results
The injury group comprised 16 soccer players; the noninjury group comprised the remaining 257 soccer players. In addition, the foot injury group comprised 16 feet, while the foot noninjury group accounted for 530 feet. The results of the comparison between the foot injury and noninjury groups are shown in Figure 2. No significant difference was found in terms of the presence or absence of history of injuries to the foot or ankle. Comparison between the dominant and nondominant leg showed that injuries were significantly more frequent in the nondominant leg (χ2 = 5.22, P = .02). The results of the comparison between the injury and noninjury groups are shown in Figure 3. No significant difference was found in the incidence of fifth metatarsal stress fractures in seniors compared with juniors. There was also no significant difference in the incidence of fifth metatarsal stress fractures on natural turf compared with artificial turf (Table 1).
Figure 2.
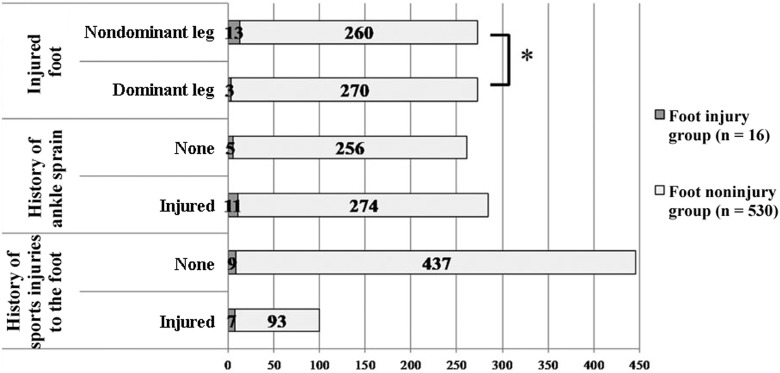
In the between-group comparison of foot injury, comparisons were carried out between the dominant and nondominant leg and the presence or absence of a history of sports injuries to the foot or ankle sprain (χ2 test, P < .05). *Comparison between the dominant leg and nondominant leg showed that injuries were significantly more frequent in the nondominant leg (χ2 = 5.22, P < .05).
Figure 3.
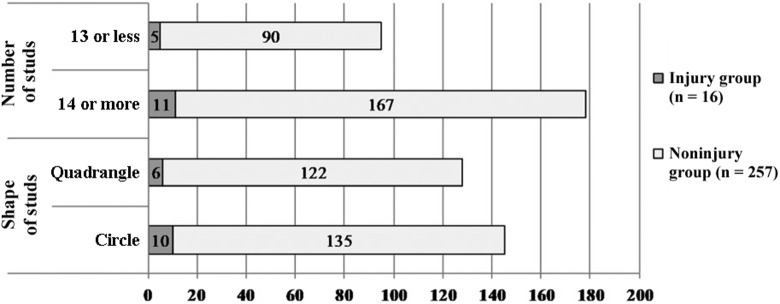
Comparison of the injured and the noninjured person group regarding stud shape and the number of studs on spiked cleats (χ2 test). There were no statistically significant differences between the groups for stud shape and the number of studs.
Table 1.
Incidence of Fifth Metatarsal Stress Fracture by University Year and Playing Surfacea
| No. of Injuries | IR per 1000 AEs (95% CI) | RR (95% CI) | P Valueb | |
|---|---|---|---|---|
| Injury during university year | 1.20 (0.51-1.89) | .72 | ||
| Juniors | 11 | 0.12 (0.00-2.20) | ||
| Seniors | 5 | 0.10 (0.00-2.18) | ||
| Playing surface | 0.53 (0.00-1.22) | .30 | ||
| Natural turf | 3 | 0.09 (0.00-1.90) | ||
| Artificial turf | 13 | 0.17 (0.00-1.98) |
aJuniors were first- and second-year students; seniors were third- and fourth-year students. AE, athete-exposure; IR, injury rate; RR, rate ratio.
bThere were no statistically significant differences for university year or ground environment.
Comparison between the injury and noninjury groups showed that toe-grip strength was significantly lower in those who had sustained a fracture (injury group, 16.7 ± 1.8 kg; noninjury group, 18.0 ± 2.4 kg; P = .01). The Q-angle also tended to be lower in those who had sustained a fracture (injury group, 13.9° ± 2.0°; noninjury group, 15.1° ± 2.3°; P = .07). There were no statistically significant differences between the groups for any other items assessed (Table 2). The results of the logistic regression analysis are shown in Table 3. In terms of the association with fifth metatarsal stress fracture injury, the odds ratio for toe-grip strength was 1.21 (95% CI, 1.01-1.45; P = .04), and the odds ratio for the Q-angle was 1.27 (95% CI, 0.99-1.62; P = .06).
Table 2.
Comparison of Measurement Items in the Injury and Noninjury Groupsa
| Injury Group (n = 16) | Noninjury Group (n = 257) | P Valueb | |
|---|---|---|---|
| Height, cm | 172.2 ± 4.9 | 171.7 ± 11.3 | .83 |
| Body weight, kg | 66.1 ± 4.1 | 64.7 ± 6.4 | .24 |
| BMI, kg/m2 | 22.3 ± 1.8 | 22.8 ± 12.6 | .18 |
| Foot–arch height ratio, % | 17.4 ± 2.0 | 17.7 ± 2.1 | .53 |
| Toe-grip strength, kg | 16.7 ± 1.8 | 18.0 ± 2.4 | .01 |
| Q-angle, deg | 13.9 ± 2.0 | 15.1 ± 2.3 | .07 |
| Leg-heel angle, deg | 6.4 ± 2.2 | 7.1 ± 1.9 | .28 |
| Functional reach test, cm | 45.9 ± 2.5 | 44.7 ± 5.0 | .18 |
| Single-leg standing time with eyes closed, s | 90.5 ± 22.6 | 97.0 ± 18.7 | .28 |
| SLR angle, deg | 90.3 ± 6.4 | 88.8 ± 7.7 | .54 |
| FFD, cm | 7.1 ± 8.0 | 8.4 ± 6.6 | .64 |
| HBD, cm | 0.2 ± 0.8 | 0.1 ± 0.6 | .87 |
| Ankle dorsiflexion, deg | 19.1 ± 3.8 | 19.5 ± 4.2 | .80 |
| Ankle plantar flexion, deg | 39.1 ± 4.6 | 39.7 ± 4.2 | .44 |
| Generalized joint laxity test, score | 0.6 ± 1.1 | 0.5 ± 1.0 | .97 |
aResults are reported as mean ± SD. BMI, body mass index; FFD, finger-floor distance; HBD, heel-buttock distance; Q-angle, quadriceps angle; SLR angle, straight-leg raising angle.
bMann-Whitney U test. Comparison between the injury and noninjury groups showed that the toe-grip strength was significantly lower in participants who sustained a fracture (P < .05). The Q-angle also tended to be lower in those who had sustained a fracture (P < .07). There were no statistically significant differences between the groups for any other items assessed.
Table 3.
Logistic Regression Analysis of the Physical Factors of Fifth Metatarsal Stress Fracturea
| Item | P Value | Odds Ratio (95% CI) |
|---|---|---|
| Height | .76 | 1.01 (0.96-1.06) |
| Body weight | .47 | 0.97 (0.89-1.06) |
| Foot–arch height ratio | .61 | 1.07 (0.83-1.37) |
| Toe-grip strength | .04 | 1.21 (1.01-1.45) |
| Q-angle | .06 | 1.27 (0.99-1.62) |
| Leg-heel angle | .44 | 1.12 (0.84-1.48) |
| Functional reach test | .34 | 0.94 (0.84-1.06) |
| Single-leg standing time with eyes closed | .32 | 1.01 (0.99-1.04) |
| SLR angle | .38 | 0.97 (0.90-1.04) |
| FFD | .51 | 1.03 (0.95-1.10) |
| HBD | .58 | 0.80 (0.36-1.78) |
| Ankle dorsiflexion range | .84 | 1.01 (0.88-1.16) |
| Ankle plantar flexion range | .35 | 1.07 (0.93-1.23) |
| Generalized joint laxity test | .66 | 0.89 (0.52-1.51) |
aFFD, finger-floor distance; HBD, heel-buttock distance; Q-angle, quadriceps angle; SLR angle; straight-leg raising angle.
Discussion
Comparison between the dominant and nondominant leg in those participants who had sustained a fifth metatarsal stress fracture injury showed that injury to the nondominant leg occurred significantly more frequently. The injury group and the noninjury group were compared, and the results showed that toe-grip strength was significantly lower in the injury group; the Q-angle also tended to be lower. There were no statistically significant differences between the groups regarding the other items. In addition, findings from the logistic regression analysis showed that toe-grip strength and Q-angle were contributing factors associated with fifth metatarsal stress fractures.
A number of research studies have previously examined factors contributing to the occurrence of fifth metatarsal stress fractures, including a research study on biomechanics,11 anatomic studies,10,22 and an epidemiological study.6 However, as far as we know, no study has yet examined the association between the occurrence of fifth metatarsal stress fractures, preexisting physical characteristics, and environmental factors.
In this study, toe-grip strength was significantly weaker in the fifth metatarsal stress fracture injury group than the noninjury group. With the base of support of the plantar region (ball of the large toe, ball of the small toe, heel), toe-grip strength may be involved in the grasping of the functional support surface during postural control. A number of previous studies have indicated an association between toe-grip strength and the ability to maintain balance and have shown that toe-grip strength decreases with age.7,16,24 Weak toe-grip strength has also been reported to be a risk factor for falls.14,15,17 In other words, weak toe-grip strength may decrease dynamic balance ability and may lead to an increase in the frequency of situations associated with increased load on the lateral part of the foot. Such an increase in the load applied on the lateral side of the foot may cause increased mechanical stress on the fifth metatarsal bone.
In addition, the injury group in this study tended to have a lower Q-angle compared with the noninjury group. The Q-angle expresses the action axis of the quadriceps femoris muscle and is believed to be closely associated with the mechanism of extension of the knee in the lower extremity (quadriceps femoris muscle, patella, patellar tendon, tibial tubercle). The Q-angle in the injury group tended to be smaller than that in the noninjury group. Although the Q-angle was within the normal limits described by previous studies,9,18 the angle was small. This could affect the knee extension mechanism and reduce the ability of the lower extremity to absorb shock, which suggests that the foot would sustain an increased shock load, particularly during running and jumping.
Fifth metatarsal stress fractures were significantly more frequent in the nondominant leg. Situations in which the nondominant leg acts as the pivot leg during dribbling movements and kicking motions may occur frequently during a soccer game. When situations involving the use of the nondominant leg as the pivot leg occur frequently, the load applied to the fifth metatarsal bone may act as a mechanical stressor, potentially leading to a fatigue fracture. No previous study has investigated the occurrence of fifth metatarsal stress fractures associated with soccer using a longitudinal study design. While our investigation was conducted on a single collegiate soccer team, the results show a possible impact of competitive soccer on fifth metatarsal stress fractures.
The comparisons between natural and artificial turf grounds showed no significant differences. There were also no differences between those with a history of sports injuries to the foot or of ankle sprains and those without, or between class levels (senior and junior years). However, environmental factors during soccer games are reported to be potential contributors to the occurrence of injuries that may cause disabilities.5 Based on this, we believe that such factors may need to be studied further.
Decreased shock-absorbing ability due to a small ankle dorsiflexion angle, varus position of the ankle in standing posture,22 and increased load on the lateral part of the foot due to a high arch may all predispose to fifth metatarsal stress fractures. However, the ankle dorsiflexion angle, leg-heel angle, and foot–arch height ratio showed no significant association with the occurrence of fifth metatarsal stress fractures in the present study. Many of the study participants from both the injury and noninjury groups had a history of ankle or foot injuries during their youth. Such sports injuries are believed to affect the functional morphology of the ankle and the foot, and they may have affected the results of our study.
A problematic issue with our study is the fact that the Q-angle was within the normal range proposed by previous studies18; this requires further investigation. The Q-angle is associated with the knee extension mechanism, and as such, the impact of the knee extension mechanism on plantar pressure will also need to be examined. In addition, the alignment of the entire body should also be taken into consideration. The measurement of toe-grip strength and Q-angle in this study involved an evaluation in a static environment; additional studies in dynamic environments and with a larger number of participants may be needed. Finally, an objective analysis of the dominant leg and nondominant leg during soccer games will need to be carried out. The impact of the frequency of use of the dominant and nondominant leg during soccer games, the types of motions performed, as well as their influence on the load conferred to the fifth metatarsal bone will need to be further examined.
The limitations of this study include the lack vitamin D, bone mineral density, or dietary calcium intake examination, as this study was based on medical examinations for the screening of physical characteristics. While this study was conducted over a long period, the number of cases of fifth metatarsal stress fracture was small, and any further studies might benefit from a larger number of participants.
Conclusion
A longitudinal study was conducted to examine the physical characteristics and environmental factors associated with college soccer players who sustained a fifth metatarsal stress fracture. In the injury group, toe-grip strength was significantly weaker than that in the noninjury group. In addition, the logistic regression analysis suggested that toe-grip strength may be associated with fifth metatarsal stress fracture injuries. There was a significantly higher frequency of fifth metatarsal stress fracture injuries affecting the nondominant leg compared with the dominant leg.
Acknowledgment
The authors thank all the research assistants, study therapists, physicians, coaches, and players who participated in this study.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Carp L. Fracture of the fifth metatarsal bone: with special reference to delayed union. Ann Surg. 1927;86:308–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dameron TB., Jr Fractures and anatomical variations of the proximal portion of the fifth metatarsal. J Bone Joint Surg. 1975;57:788–792. [PubMed] [Google Scholar]
- 3. Delee JC, Evans JP, Julian J. Stress fracture of the fifth metatarsal. Am J Sports Med. 1983;11:349–353. [DOI] [PubMed] [Google Scholar]
- 4. Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45:M192–M197. [DOI] [PubMed] [Google Scholar]
- 5. Ekstrand J, Nigg BM. Surface-related injuries in soccer. Sports Med. 1989;8:56–62. [DOI] [PubMed] [Google Scholar]
- 6. Ekstrand J, Torstveit MK. Stress fractures in elite male football players. Scand J Med Sci Sports. 2012;22:341–346. [DOI] [PubMed] [Google Scholar]
- 7. Endo M, Ashton-Miller JA, Alexander NB. Effect of age and gender on toe flexor muscle strength. J Gerontol A Biol Sci Med Sci. 2002;57:M392–M397. [DOI] [PubMed] [Google Scholar]
- 8. Glasgow MT, Naranja RJ, Jr, Glasgow SG, Torg JS. Analysis of failed surgical management of fractures of the base of the fifth metatarsal distal to the tuberosity: the Jones fracture. Foot Ankle Int. 1996;17:449–457. [DOI] [PubMed] [Google Scholar]
- 9. Hvid I, Andersen LI, Schmidt H. Chondromalacia patellae: the relation to abnormal patellofemoral joint mechanics. Acta Orthop Scand. 1981;52:661–666. [DOI] [PubMed] [Google Scholar]
- 10. Jones R. Fracture of the base of the fifth metatarsal bone by indirect violence. Ann Surg. 1902;35:697–700.2. [PMC free article] [PubMed] [Google Scholar]
- 11. Kavanaugh JH, Brower TD, Mann RV. The Jones fracture revisited. J Bone Joint Surg Am. 1978;60:776–782. [PubMed] [Google Scholar]
- 12. Lee KT, Kim KC, Park YU, Kim TW, Lee YK. Radiographic evaluation of foot structure following fifth metatarsal stress fracture. Foot Ankle Int. 2011;32:796–801. [DOI] [PubMed] [Google Scholar]
- 13. Livingston LA. The quadriceps angle: a review of the literature. J Orthop Sports Phys Ther. 1998;28:105–109. [DOI] [PubMed] [Google Scholar]
- 14. Menz HB, Morris ME, Lord SR. Foot and ankle characteristics associated with impaired balance and functional ability in older people. J Gerontol A Biol Sci Med Sci. 2005;60:1546–1552. [DOI] [PubMed] [Google Scholar]
- 15. Menz HB, Morris ME, Lord SR. Foot and ankle risk factors for falls in older people: a prospective study. J Gerontol A Biol Sci Med Sci. 2006;61:866–870. [DOI] [PubMed] [Google Scholar]
- 16. Menz HB, Zammit GV, Munteanu SE, Scott G. Plantarflexion strength of the toe: age and gender differences and evaluation of a clinical screening test. Foot Ankle Int. 2006;27:1103–1108. [DOI] [PubMed] [Google Scholar]
- 17. Mickle KJ, Munro BJ, Lord SR, Menz HB, Steele JR. ISB Clinical Biomechanics Award 2009: toe weakness and deformity increase the risk of falls in older people. Clin Biomech (Bristol, Avon). 2009;24:787–791. [DOI] [PubMed] [Google Scholar]
- 18. Mo J. Manual of Orthopedic Surgery. Park Ridge, IL: American Orthopaedic Association; 1972. [Google Scholar]
- 19. Murata S, Kutsuna T. The trial of measurement of foot grasp power—development of a new apparatus and the reproducibility of measurement values [in Japanese]. Rigakuryoho Kagaku. 2002;17:243–247. [Google Scholar]
- 20. Porter DA, Duncan M, Meyer SJ. Fifth metatarsal Jones fracture fixation with a 4.5-mm cannulated stainless steel screw in the competitive and recreational athlete: a clinical and radiographic evaluation. Am J Sports Med. 2005;33:726–733. [DOI] [PubMed] [Google Scholar]
- 21. Portland G, Kelikian A, Kodros S. Acute surgical management of Jones fractures. Foot Ankle Int. 2003;24:829–833. [DOI] [PubMed] [Google Scholar]
- 22. Raikin SM, Slenker N, Ratigan B. The association of a varus hindfoot and fracture of the fifth metatarsal metaphyseal-diaphyseal junction: the Jones fracture. Am J Sports Med. 2008;36:1367–1372. [DOI] [PubMed] [Google Scholar]
- 23. Roca J, Roure F, Fernandez Fairen M, Yunta A. Stress fractures of the fifth metatarsal. Acta Orthop Belg. 1980;46:630–636. [PubMed] [Google Scholar]
- 24. Scott G, Menz HB, Newcombe L. Age-related differences in foot structure and function. Gait Posture. 2007;26:68–75. [DOI] [PubMed] [Google Scholar]
- 25. Torg JS, Balduini FC, Zelko RR, Pavlov H, Peff TC, Das M. Fractures of the base of the fifth metatarsal distal to the tuberosity: classification and guidelines for non-surgical management. J Bone Joint Surg Am. 1984;66:209–214. [PubMed] [Google Scholar]
- 26. Uritani D, Fukumoto T, Matsumoto D, Shima M. Reference values for toe grip strength among Japanese adults aged 20 to 79 years: a cross-sectional study. J Foot Ankle Res. 2014;7:28 doi:10.1186/1757-1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Williams DS, 3rd, McClay IS, Hamil J. Arch structure and injury patterns in runners. Clin Biomech (Bristol, Avon). 2001;16:341–347. [DOI] [PubMed] [Google Scholar]
- 28. Wright RW, Fischer DA, Shively RA, Heidt RS, Jr, Nuber GW. Refracture of proximal fifth metatarsal (Jones) fracture after intramedullary screw fixation in athletes. Am J Sports Med. 2000;28:732–736. [DOI] [PubMed] [Google Scholar]
- 29. Yamazaki J, Muneta T, Ju YJ, Morito T, Okuwaki T, Sekiya I. Hip acetabular dysplasia and joint laxity of female anterior cruciate ligament injured patients. Am J Sports Med. 2011;39:410–414. [DOI] [PubMed] [Google Scholar]
- 30. Zelko RR, Torg JS, Rachun A. Proximal diaphyseal fractures of the fifth metatarsal—treatment of the fractures and their complications in athletes. Am J Sports Med. 1979;7:95–101. [DOI] [PubMed] [Google Scholar]
- 31. Zogby RG, Baker BE. A review of nonoperative treatment of Jones fracture. Am J Sports Med. 1987;15:304–307. [DOI] [PubMed] [Google Scholar]


