Abstract
Background
The factors associated with anterior cruciate ligament (ACL) tears are not completely clear. Some studies have shown that patients with a narrow intercondylar notch have a predisposition for ACL tears.
Purpose
To determine the relationship between the α angle and intercondylar notch width measurements and ACL tears.
Study Design
Case-control study; Level of evidence, 3.
Methods
A total of 530 patients (308 with ACL rupture, 222 with healthy ACLs) were included in this study. The α angle and intercondylar width were measured from magnetic resonance images (MRIs). Binary logistic regression analysis was performed to determine the influence of the variables on ACL status (normal or torn). Odds ratios (ORs) and their respective 95% CIs were also calculated.
Results
No significant differences in patient age and the affected knee were found between patients with normal or torn ACLs. The mean α angle was higher in patients with a torn ACL than in those with an intact one (57.5° ± 5.5° vs 56.2° ± 4.5°; P = .009). Intercondylar width was significantly lower in patients with a torn ACL than in those with an intact one (18.2 ± 3.1 vs 19.5 ± 3.6 mm; P < .001). A highly significant difference between men and women was found for mean intercondylar notch width (19.3 ± 3.3 vs 17.4 ± 3.1 mm; P < .001). In a logistic regression model, sex, intercondylar width, and α angle were statistically significant when adjusted for age.
Conclusion
Study results suggest that the ACL tears are associated with a narrow intercondylar notch and a high α angle, and that tears occur more frequently in men than in women.
Clinical Relevance
The model proposed in this study could be used by the physician in the medical office as a tool to identify the risk factors that may predispose a patient for a potential ACL tear.
Keywords: anterior cruciate ligament, intercondylar notch, alpha angle, anthropometric measures
An anterior cruciate ligament (ACL) tear is a serious knee injury. Currently, the most common treatment is surgery. The etiology of ACL tears is not completely clear; the cause was primarily thought to be a traumatic mechanism with rotation, hyperextension, or by contraction of the quadriceps muscle.5,14 However, some studies show a morphological predisposition and, as a consequence, some authors have measured intercondylar notch dimensions and have shown that when the intercondylar notch was narrow, patients have a high predisposition for ACL tear.8,11 In fact, the clinical relevance of the intercondylar notch was recognized by Fu and Musahl,11 who developed a mathematical model to quantitatively characterize impingement of the ACL against the intercondylar notch in 3-dimensional (3D) space. Stijak et al18 stated that the most important anatomic risk factors in ACL tears are the morphometric parameters of the intercondylar notch. In morphometric studies, the index of notch width and the index of notch shape (NWI and NSI, respectively) are commonly used.8 In addition to the impingement of the ACL at the anterior and posterior roof of the notch, a smaller, weaker ACL in the small intercondylar notch may be the reason for disposition for an ACL rupture.8
In some patients with a torn ACL, the angle between the longitudinal femoral axis and Blummensaat line (BL) increases compared with that of patients with a normal ACL (personal observation). However, the implication of the BL angle or the degree of inclination of BL observed by magnetic resonance imaging (MRI) has not been reported. Consequently, this study was performed to measure this angle and determine whether this measure was associated with ACL tears. Measuring the angle between the BL and tibial plateau surface line was initially considered, but this angle would result in erroneous measurements because of the relative tibial position with respect to the femur. Consequently, the distance between the main longitudinal femoral axis with respect to the BL was measured. This measure is independent of tibial and femoral position.
The purpose of this study was to determine the relationships between the alpha (α) angle and intercondylar notch width measures and ACL tears. To accomplish this objective, selected MRIs from 530 patients with or without ACL tears were retrospectively evaluated.
Methods
Patients
A total of 530 patients (364 male, 166 female) with a mean age of 33.4 ± 11.5 years agreed to participate in this study. The study was approved by the Universidad de Murcia Ethics Committee. All patients presented to the Orthopaedics Unit at Clínica CEMTRO for knee problems, including ACL tears. To be included in this study, patients had to be older than 18 years, evaluated with the same MRI study protocol, and had not had any previous intervention in the same knee. Thus, among the patients included in the study, 308 had an ACL tear while the remaining 222 had a normal ACL and came to our unit for other knee problems.
MRI Measurements of α Angle and Intercondylar Space
Images of the knee were obtained by MRI (Optima MR450w 1.5T; General Electric) using a multielement quadrature 8-channel antenna (HD TRKnee PA; General Electric). The patients were positioned supine, with the knee in the center of the coil. This position was varied, if necessary, to see other pathologies. The knee was slightly flexed (15°) and the foot in its natural flexion of 4° to 5° of external rotation, favoring the ACL study. The antenna was positioned in the isocenter of the magnet or closest to it.
Fat-saturated proton density sagittal and axial sequences were obtained. The sagittal plane was programmed geometrically over the transverse plane, orthogonal with respect to the posterior intercondylar line by passing a cut by the ACL. We used a field of view of approximately 15 cm, a 3-mm slice thickness every 0.3-mm advance, and a high-resolution matrix. The axial plane was determined according to the sagittal plane marking of the lower edge of both condyles. Scanning started at the level of the patella tendon attachment to the tibia and extended to the quadriceps insertion into the upper pole of the patella.
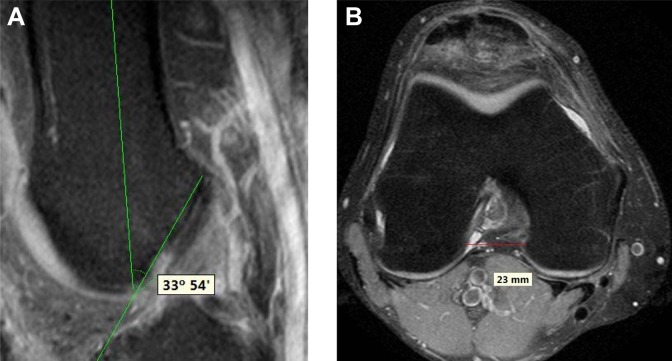
The α angle and the intercondylar width were measured using MRIs downloaded in the Common ECH version 2.0.0 program (Common Management Solutions) and the measuring tools of the application. The α angle measurement was performed as follows: in a sagittal section where the entire BL is seen, the α angle is that formed by the BL and the long axis of the femur (Figure 1A). In an axial section, the intercondylar notch width was considered as the lowest distance between both condyles (most narrow site of the intercondylar notch) (Figure 1B).
Figure 1.
Representative example of (A) α angle and (B) intercondylar notch distance measures on magnetic resonance images (MRIs).
Statistical Analysis
Statistical analysis was performed using SPSS Statistics v. 22 for Windows software (IBM). Continuous variables were expressed as the mean ± SD, and normality was checked using the Kolmogorov-Smirnov test. The means were compared using the Student t test (normal variables) or with Mann-Whitney U test (nonparametric comparisons). Categorical variables were expressed as a percentage with the minimum and maximum values as a dispersion measure. Comparison of counts and percentages was carried out using the χ2 test.
Binary logistic regression analysis was performed to determine the influence of the different variables on the ACL status (normal or torn). Thus, the dependent variable was defined as “ACL status” (0, normal; 1, torn). Overall significance was assessed by the log of likelihood ratio with the χ2 test, and goodness of fit was studied by the Hosmer-Lemeshow test. Statistical significance of the coefficients in the regression equation was contrasted with the Wald test. Odds ratios (ORs) and their respective 95% CIs were also estimated. To study the ability of the definitive model in the discrimination between the 2 values of the dependent variable, a receiver operating characteristic (ROC) curve was constructed using the predicted probability values estimated with this model as the test variable and “ACL status: pathologic = 1” as the value of the state variable.25 Cutoff probability values to discriminate between “ACL status: healthy” and “ACL status: pathologic” were estimated by examining the ROC curve coordinates.
In all comparisons and parameter estimations, a value of P < .05 (2 sides) was considered statistically significant.
Results
Table 1 shows the comparison of sex, age, knee, α angle, and intercondylar space among patients with a normal or torn ACL. No significant differences in patient age and the affected knee were found between patients with normal or torn ACLs. The α angle and intercondylar width were significantly different between patients with normal or torn ACLs. The α angle (Figure 2A) was greater in patients with a torn ACL than those with an intact one (57.5° ± 5.5° vs 56.2° ± 4.5°; P = .009) (Table 1). On the contrary, the intercondylar width (Figure 2B) was significantly lower in patients with a torn ACL than in those with an intact one (18.2 ± 3.1 vs 19.5 ± 3.6 mm; P < .001) (Table 1). A highly significant difference between men and women was found for mean intercondylar notch width (19.3 ± 3.3 vs 17.4 ± 3.1 mm; P < .001, Mann-Whitney U test). On the contrary, the α angle was statistically similar for both sexes (56.7° ± 5.2° in men vs 57.5° ± 5.0° in women; P = .098, Mann-Whitney U test).
Table 1.
Comparison of Epidemiological Factors Between Patients With Intact or Torn Anterior Cruciate Ligaments
| Intact (n = 222) | Torn (n = 308) | P | |
|---|---|---|---|
| Sex, n | |||
| Male | 140 | 224 | .018a |
| Female | 82 | 84 | |
| Age, y, mean ± SD | 33.3 ± 11.1 | 33.8 ± 12.5 | .954b |
| Knee, n | |||
| Left | 96 | 147 | .307a |
| Right | 126 | 161 | |
| α angle, deg, mean ± SD | 56.2 ± 4.5 | 57.5 ± 5.5 | .009b |
| Intercondylar notch distance, mm, mean ± SD | 19.5 ± 3.6 | 18.2 ± 3.1 | <.001b |
aχ2 test.
bMann-Whitney U test.
Figure 2.
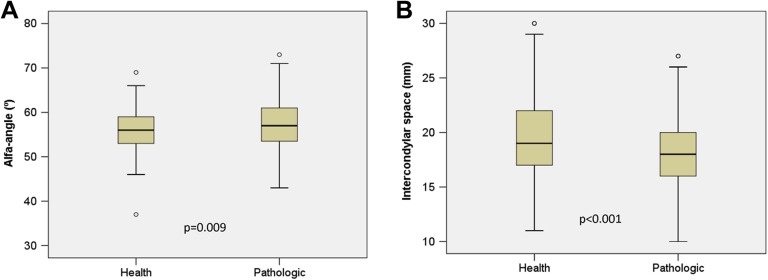
Box plots of anthropometric measures (A, α angle; B, intercondylar space) in healthy and pathologic anterior cruciate ligaments.
The distribution of normal and torn ACLs was significantly different for women and men (P = .018).
A global binary logistic regression analysis model was constructed to study the effect of all variables included in the present study on ACL status as a dependent variable (0, normal; 1, torn). After the exclusion of nonsignificant variables (1 by 1), the best-fit model obtained (model that includes significant variables and those variables that make the model fit well to data) is shown in Table 2. Log of likelihood ratio contrasted by the χ2 test demonstrated that the model was highly significant (χ2 = 40.18; degrees of freedom [df] =4; P < .001). The Hosmer-Lemeshow test that evaluates the differences between the probabilities predicted by the model and those observed showed that the goodness of fit for the model was acceptable (χ2 = 5.8; df = 8; P = .671). As shown in Table 2, sex, intercondylar space measurement, and α angle were statistically significant, when adjusting by age. Age was included in the model only for mathematical reasons. The ORs estimated for the variables included in the model are shown in Table 2. There is an inverse relationship between the intercondylar space width and ACL rupture, so it is more likely to have a pathological ACL when there is a narrow intercondylar space. Finally, from this model we can deduce that there is scarce influence of the α angle in the ACL status (OR, 1.049; 95% CI, 1.011-1.014). The probability values estimated with the above-described model were used to construct an ROC curve taking “ACL status, pathologic” as the state variable (Figure 3). Area under the ROC curve (AUC) was 0.645 (95% CI, 0.597-0.693; P < .001), indicating that the probabilities predicted by the model were very similar to those observed. According to the estimated parameters of the model, the probability of having a torn ACL for a given patient could be predicted by substituting the value of the factors into the following equation:
Table 2.
Binary Logistic Regression Analysis to Elucidate the Factors Affecting Anterior Cruciate Ligament Status (Healthy/Pathologic)
| Factor | Coefficient (B) | P | Odds Ratio | 95% CI |
|---|---|---|---|---|
| Sex (male) | 0.796 | <.001 | 2.217 | 1.474-3.333 |
| Intercondylar notch width | −0.142 | <.001 | 0.868 | 0.819-0.920 |
| α angle | 0.048 | .011 | 1.049 | 1.011-1.088 |
| Age | -0.001 | .857 | 0.999 | 0.983-1.014 |
| Constant | -0.211 | .861 |
Figure 3.
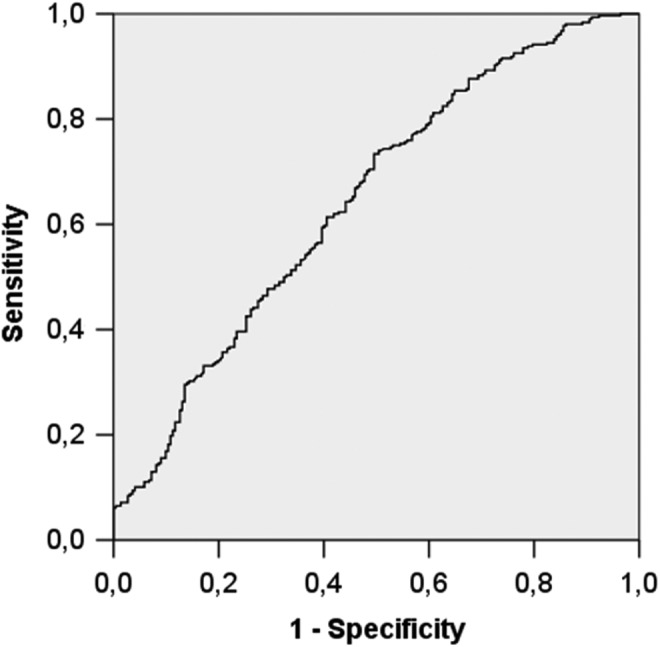
Receiver operating characteristic curve constructed with the probability values predicted with the logistic regression model, using “ACL status, pathologic” as the state variable. Area under the curve (AUC), 0.645; 95% CI of AUC, 0.597 to 0.693 (P < .001). ACL, anterior cruciate ligament.
Table 3 shows the number of patients correctly and incorrectly classified by the model, taking a predicted probability value of 0.50 as a cutoff, which means that patients with a calculated probability <0.50 are classified as having a normal ACL and patients with a value ≥0.50 are classified as having a torn ACL. Taking the data depicted in Table 3 into account, the model had a 38.3% specificity and 80.5% sensitivity for detecting patients with pathologic ACL. False-positive and false-negative rates were 61.7% and 19.5%, respectively. Predictive positive value was 64.4%, and predictive negative value was 58.6%. Finally, the overall accuracy or diagnostic efficiency of the model was 62.8% in the identification of patients with pathologic ACL.
Table 3.
Number of Patients Correctly and Incorrectly Classified by the Binary Logistic Regression Modela
| Observed (N = 530) | Predicted | Percentage of Patients Correctly Classified | |
|---|---|---|---|
| Intact ACL (n = 145) | Torn ACL (n = 385) | ||
| Intact ACL (n = 222) | 85 | 137 | 38.3 |
| Torn ACL (n = 308) | 60 | 248 | 80.5 |
| Overall percentage of correctly classified patients | 62.8 | ||
aPatients with a predicted probability value ≥0.50 were considered as having a pathologic ACL. ACL, anterior cruciate ligament.
Discussion
The number of ACL tears is increasing because there is a greater number of people participating in sports. Consequently, identification of the factors associated with an increased risk of having an ACL tear is important.16 Some studies have shown that morphology of the intercondylar notch is one of the parameters that predisposes athletes to an ACL tear.1,16 In most of our patients with ACL tears, the α angle increases when compared with that of intact ones. This study was performed to establish the importance of the degree of inclination of BL and as a cause of ACL tears.
In the univariate analysis, the α angle and intercondylar notch distance were significantly different between patients with or without ACL tear. Thus, a greater α angle was associated with patients with a torn ACL. In addition, as has been published previously by many authors, the intercondylar notch width was narrowest in patients with pathologic ACL.3,7,8,10,12 Cha et al3 measured the intercondylar notch width, notch index, sagittal notch angle, and notch angle. They found that patients with mucoid ACL hypertrophy showed a narrower notch, a more pronounced notch angle, and a smaller notch area than controls, highlighting the importance of the intercondylar notch in the development of an ACL tear. They constructed a mathematical model that evaluated the role of the intercondylar notch in impingement of the ACL.3 This fact is supported by the findings of Fu and Musahl,11 who postulated in 2013 that the impingement of the ACL against the intercondylar notch is a main factor for ACL tears. A notch narrower than 12 mm wide may be associated with the absence of the ACL.12
A logistic regression model was constructed to study the risk factors for ACL tears. As expected, after evaluating the results of the univariate analysis, sex and intercondylar notch width were the most relevant factors, followed by the α angle. Our model has a relative high sensitivity but its specificity is low, which means that it is able to accurately predict patients with a torn ACL but it is not accurate enough to identify patients with an intact ACL. The reason for this is that there are probably other factors, not evaluated in this study, that may contribute to ACL tears. Apart from neuromuscular and anatomic factors,15,16 Smith et al17 identified several other factors such as hormonal, genetic, cognitive function, previous injury, and extrinsic factors that are associated with an ACL tear. All publications indicate that the risk for having a torn ACL is multifactorial. Understanding these factors and the complex interactions among them is important to clearly establish predisposition to ACL tears. There are many studies that evaluated different anthropometric measures, the index of the intercondylar notch,1,6,9,13,20,22 and lateral condyle morphology.23,24 The goal of the present study was to identify patients who are predisposed to ACL tears using 2 morphological features, which can be measured with MRI.3,4,21 The α angle and intercondylar notch width measurements may be useful in daily medical practice to evaluate the knee prior to ACL reconstruction.
One limitation of the present study is measuring 3D structures in 2D projections in which the ACL has an oblique arrangement and the intercondylar notch measurements may vary depending on the morphology of the lateral condyle. This may cause measurement variations depending on the resonance protocol and on the orientation of the image slices in their spatial arrangement. The advantage of this protocol is that objective measurements were made of bony structures with MRI.
Conclusion
ACL tears are associated with a small intercondylar notch width and a high α angle. In our opinion, when the α angle increases, the ACL is in a relative horizontal position, which causes more frequent ACL rupture in extension due to impingement against the anterior intercondylar notch. However, there is less impingement when the α angle is decreased because the ACL adopts a more vertical position and can turn on itself. In this case, ACL rupture could be more related to the narrowness of the intercondylar notch than impingement. All of the opinions related to the morphology of the intercondylar notch explain the noncontact mechanism of ACL rupture, but 1 important factor that may predispose a patient to an ACL tear is the relative angular position of the tibia with respect to the femur.2 The difference between men and women in the predisposition of ACL tears may be explained by the morphological differences between sexes, and the risk for ACL tears is multifactorial.19 For this reason, 1 factor of femoral morphology will not be the sole cause of ACL tears.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by the Fundacion Pedro Guillen.
References
- 1. Anderson AF, Dome DC, Gautam S, Awh MH, Rennirt GW. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29:58–66. [DOI] [PubMed] [Google Scholar]
- 2. Beynnon BD, Hall JS, Sturnick DR, et al. Increased slope of the lateral tibial plateau subchondral bone is associated with greater risk of noncontact ACL injury in females but not in males: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med. 2014;42:1039–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cha JH, Lee SH, Shin MJ, Choi BK, Bin SI. Relationship between mucoid hypertrophy of the anterior cruciate ligament (ACL) and morphologic change of the intercondylar notch: MRI and arthroscopy correlation. Skeletal Radiol. 2008;37:821–826. [DOI] [PubMed] [Google Scholar]
- 4. Chambat P. ACL tear. Orthop Traumatol Surg Res. 2013;99(suppl):S43–S52. [DOI] [PubMed] [Google Scholar]
- 5. Chambat P, Guier C, Sonnery-Cottet B, Fayard JM, Thaunat M. The evolution of ACL reconstruction over the last fifty years. Int Orthop. 2013;37:181–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Charlton WP, St John TA, Ciccotti MG, Harrison N, Schweitzer M. Differences in femoral notch anatomy between men and women: a magnetic resonance imaging study. Am J Sports Med. 2002;30:329–333. [DOI] [PubMed] [Google Scholar]
- 7. Dahlstedt L, Dalén N, Dahlborn M, Nilsson T. Value of intercondylar notch plasty. CT studies and peroperative measurements of 127 knees. Acta Orthop Scand. 1990;61:558–561. [DOI] [PubMed] [Google Scholar]
- 8. Dienst M, Schneider G, Altmeyer K, et al. Correlation of intercondylar notch cross sections to the ACL size: a high resolution MR tomographic in vivo analysis. Arch Orthop Trauma Surg. 2007;127:253–260. [DOI] [PubMed] [Google Scholar]
- 9. Domzalski M, Grzelak P, Gabos P. Risk factors for anterior cruciate ligament injury in skeletally immature patients: analysis of intercondylar notch width using magnetic resonance imaging. Int Orthop. 2010;34:703–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Everhart JS, Flanigan DC, Chaudhari AM. Anteromedial ridging of the femoral intercondylar notch: an anatomic study of 170 archival skeletal specimens. Knee Surg Sports Traumatol Arthrosc. 2014;22:80–87. [DOI] [PubMed] [Google Scholar]
- 11. Fu FH, Musahl V. Anatomic ACL reconstruction. Preface. Clin Sports Med. 2013;32:xv–xvi. [DOI] [PubMed] [Google Scholar]
- 12. Hernigou P, Garabedian JM. Intercondylar notch width and the risk for anterior cruciate ligament rupture in the osteoarthritic knee: evaluation by plain radiography and CT scan. Knee. 2002;9:313–316. [DOI] [PubMed] [Google Scholar]
- 13. LaPrade RF, Burnett QM., 2nd Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1994;22:198–202. [DOI] [PubMed] [Google Scholar]
- 14. Pappas E, Zampeli F, Xergia SA, Georgoulis AD. Lessons learned from the last 20 years of ACL-related in vivo-biomechanics research of the knee joint. Knee Surg Sports Traumatol Arthrosc. 2013;21:755–766. [DOI] [PubMed] [Google Scholar]
- 15. Shelbourne KD, Kerr B. The relationship of femoral intercondylar notch width to height, weight, and sex in patients with intact anterior cruciate ligaments. Am J Knee Surg. 2001;14:92–96. [PubMed] [Google Scholar]
- 16. Smith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: a review of the literature—part 1: neuromuscular and anatomic risk. Sports Health. 2012;4:69–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Smith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: a review of the literature—part 2: hormonal, genetic, cognitive function, previous injury, and extrinsic risk factors. Sports Health. 2012;4:155–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stijak L, Nikolić V, Blagojević Z, et al. Influence of morphometric intercondylar notch parameters in ACL ruptures [in Serbian]. Acta Chir Iugosl. 2006;53(4):79–83. [DOI] [PubMed] [Google Scholar]
- 19. Sturnick DR, Vacek PM, DeSarno MJ, et al. Combined anatomic factors predicting risk of anterior cruciate ligament injury for males and females. Am J Sports Med. 2015;43:839–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sutton KM, Bullock JM. Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg. 2013;21:41–50. [DOI] [PubMed] [Google Scholar]
- 21. Tanzer M, Lenczner E. The relationship of intercondylar notch size and content to notchplasty requirement in anterior cruciate ligament surgery. Arthroscopy. 1990;6:89–93. [DOI] [PubMed] [Google Scholar]
- 22. Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31:831–842. [DOI] [PubMed] [Google Scholar]
- 23. van Diek FM, Wolf MR, Murawski CD, van Eck CF, Fu FH. Knee morphology and risk factors for developing an anterior cruciate ligament rupture: an MRI comparison between ACL-ruptured and non-injured knees. Knee Surg Sports Traumatol Arthrosc. 2014;22:987–994. [DOI] [PubMed] [Google Scholar]
- 24. Vrooijink SH, Wolters F, Van Eck CF, Fu FH. Measurements of knee morphometrics using MRI and arthroscopy: a comparative study between ACL-injured and non-injured subjects. Knee Surg Sports Traumatol Arthrosc. 2011;19(suppl 1):S12–S16. [DOI] [PubMed] [Google Scholar]
- 25. Zweig MH, Campbell G. Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem. 1993;39:561–577. [PubMed] [Google Scholar]