Abstract
Background:
Calcified rotator cuff tendinitis is a common cause of chronic shoulder pain that leads to significant pain and functional limitations. Although most patients respond well to conservative treatment, some eventually require surgical treatment.
Purpose:
To evaluate the clinical outcome with arthroscopic removal of calcific deposit and rotator cuff repair without acromioplasty for the treatment of calcific tendinitis of the supraspinatus tendon.
Study Design:
Case series; Level of evidence, 4.
Methods:
This study retrospectively evaluated 30 consecutive patients with a mean age of 49.2 years. The mean follow-up was 35 months (range, 24-88 months). Pre- and postoperative functional assessment was performed using the Constant score, University of California Los Angeles (UCLA) score, and Quick Disabilities of the Arm, Shoulder, and Hand (DASH). Pain was assessed by visual analog scale (VAS). Radiographs and magnetic resonance imaging (MRI) were performed to evaluate the recurrence of calcifications and the indemnity of the supraspinatus tendon repair.
Results:
Significant improvement was obtained for pain (mean VAS, 8.7 before surgery to 0.8 after; P < .001). The mean Constant score increased from 23.9 preoperatively to 85.3 postoperatively (P < .001), the mean Quick DASH score decreased from 47.3 preoperatively to 8.97 postoperatively (P < .001), and the UCLA score increased from 15.8 preoperatively to 32.2 postoperatively (P < .001). MRI examination at last follow-up (70% of patients) showed no tendon tears, and 96.2% of patients were satisfied with their results.
Conclusion:
Arthroscopic removal and rotator cuff repair without acromioplasty can lead to good results in patients with symptomatic calcifying tendonitis of the supraspinatus tendon.
Keywords: calcifying tendinitis, rotator cuff, arthroscopy
Calcific tendinopathy of the rotator cuff is a common condition, with a reported prevalence varying from 2.7% to 22%, mostly affecting women aged between 30 and 50 years.4,25 The supraspinatus tendon is the most commonly involved.25
Nonoperative treatment is usually successful in up to 90% of patients.17 Several conservative treatments showed favorable results in the management of calcific tendinopathy of the rotator cuff: physical therapy, oral anti-inflammatory medication, subacromial corticosteroid injections, lavage and aspiration, and high-energy extracorporeal shockwave therapy.1,5,6,9,13,22,26
Surgical treatment is reserved for patients in which prolonged conservative therapy has failed and the deposits do not show signs of spontaneous resolution on radiographs.12,17,19
There are some controversial issues concerning arthroscopic treatment of these lesions. First, the significance of removing all calcium deposits is largely debated in the literature, with studies showing favorable results with both subtraction of all deposits10,19,20 and partial eradication of the calcifications.2,8,14 Second, the removal of the calcific material usually leaves a hole in the tendon. Some surgeons recommend primary repair of the lesion,23,27 while others do not routinely suture the residual defect.11,14,20 Finally, the last controversial topic is the need of a subacromial decompression in addition to the removal of the calcific deposit. Some investigators stated that successful outcome seemed to be independent of subacromial decompression.14,15 Nonetheless, others prefer to associate a subacromial decompression principally in those patients with signs of impingement on the coracohumeral ligament or those with an acromion type III.2,11
The purpose of this study was to evaluate the clinical outcomes and complications of complete arthroscopic removal of intratendinous calcific deposits and repair of the tendon lesion without acromioplasty.
Methods
Between June 2005 and June 2012, 30 patients with calcifying rotator cuff tendinitis were treated with arthroscopic excision of the calcium deposits and tendon defect repair without acromioplasty.
Our institutional review board (IRB 00003580) approved the study protocol.
Inclusion criteria were shoulder pain persistence for more than 4 months (mean, 5.8 months) with visible calcification on conventional radiographs and failure of intensive nonoperative treatment, including physical therapy, nonsteroidal anti-inflammatory drugs, and steroid injections, for at least 3 months. The deposits were located in the supraspinatus tendon in all cases.
Patients with concomitant pathologies such as instability, rotator cuff tears, or acromioclavicular joint pathology were excluded from this study.
Demographic and clinical characteristics of patients regarding age, sex, shoulder dominance, injured side, and duration of symptoms before surgery were documented. A summary of demographic and clinical characteristics of patients is shown in Table 1.
TABLE 1.
Demographic and Clinical Characteristics of Patients and Lesions
| Sex, n | |
| Male | 5 |
| Female | 21 |
| Age, y, mean (range) | 49.2 (32-72) |
| Dominant hand, % | 61.5 |
| Involved shoulder, n | |
| Right | 16 |
| Left | 10 |
| Mean follow-up, mo, mean (range) | 35 (24-88) |
| Symptom duration, mo, mean ± SD | 5.5 ± 1.6 |
| Calcific deposit type, na | |
| A | 18 |
| B | 8 |
aAccording to the French Arthroscopic Society radiographic classification: type A, homogeneous calcification, well-defined limits; type B, heterogeneous and fragmented calcification, well-defined limits.
Twenty-six patients were available for the final analysis (21 women and 5 men). Four patients were lost to follow-up: 1 was excluded because he had a concomitant calcification of the subscapular tendon, 2 were not available for analysis because they moved outside the country, and 1 patient died. There were 16 right shoulders and 10 left shoulders. Dominant side was involved in 61.5% of patients. The mean age was 49.2 years (range, 32-72 years).
The French Arthroscopic Society radiographic classification16 was used to assess calcific deposits preoperatively: type A, homogeneous calcification with well-defined limits; type B, heterogeneous and fragmented calcification with well-defined limits; type C, heterogeneous calcification with poorly defined limits and sometimes with a punctate appearance; and type D, dystrophic calcifications at the tendon insertion. The preoperative evaluation showed 18 type A lesions (69.3%) and 8 type B lesions (30.7%).
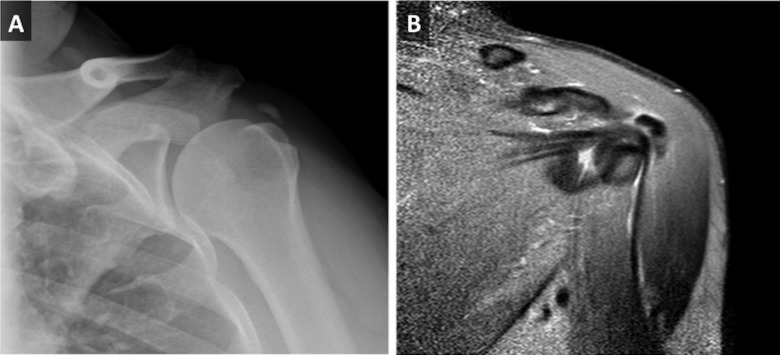
All patients were evaluated with preoperative anterioposterior radiographs: axillary lateral and supraspinatus outlet view. Each patient underwent magnetic resonance imaging (MRI) to rule out possible concomitant pathologies such as rotator cuff lesions (Figure 1).
Figure 1.
(A) Plain radiographs showing type A calcific deposit (homogeneous calcification with well-defined limits). (B) Magnetic resonance image showing the calcific deposit in the supraspinatus tendon before surgery.
Preoperative and postoperative clinical assessment was performed with Constant score, University of California Los Angeles shoulder scale (UCLA score), and Quick Disabilities of the Arm, Shoulder, and Hand (DASH) score. Pain evaluation was carried out using a visual analog scale (VAS). Furthermore, all patients were asked to describe the subjective result of the intervention as excellent, good, fair, or poor.
Throughout follow-up, all patients were evaluated with radiographs and MRI to evaluate the recurrence of calcifications and the indemnity of the supraspinatus tendon repair. Oblique coronal, oblique sagittal, and transverse views of T2-weighted images on MRI were used to classify postoperative cuff integrity into 5 categories according to Sugaya et al24: type I, repaired cuff appeared to have sufficient thickness compared with normal cuff with homogeneously low intensity on each image; type II, sufficient thickness compared with normal cuff associated with partial high intensity area; type III, insufficient thickness with less than half the thickness when compared with normal cuff, but without discontinuity, suggesting a partial-thickness delaminated tear; type IV, presence of a minor discontinuity in only 1 or 2 slices on both oblique coronal and sagittal images, suggesting a small, full-thickness tear; and type V, presence of a major discontinuity observed in more than 2 slices on both oblique coronal and sagittal images, suggesting a medium or large full-thickness tear.
Intraoperative and postoperative complications were documented.
Surgical Technique
All patients were operated on in a beach-chair position. Patients received combined anesthesia (regional blockade + general anesthesia). First, diagnostic arthroscopy was performed in a standardized manner. The arthroscope was inserted through a posterior portal, and the glenohumeral joint was evaluated first. Associated intra-articular abnormalities were documented. Then, the scope was relocated to the subacromial space, and a lateral portal was established.
After bursal debridement, the calcium deposits were located by percutaneous needling and excised with a motorized shaver or a small curette; extensive washing followed. An attempt to remove all calcium was made with the aid of intraoperative fluoroscopy if necessary. The tendon tears created with the shaver were repaired completely.
Suture anchor repair was undertaken in the case of a relatively large full-thickness defect and partial-thickness tear of greater than Ellman grade III after removal of calcific material, and side-to-side repair was performed in partial tear of Ellman grade II to avoid propagation of rotator cuff tear. No subacromial decompression was accomplished in any patient.
Postoperative Rehabilitation
Postoperative protocol consisted of sling immobilization for 3 to 4 weeks depending on the type of repair performed. A standardized rehabilitation protocol for rotator cuff repairs was used with progressive range of motion exercises as tolerated.
Statistical Analysis
Pre- and postoperative scores were compared using the Student t test for independent samples. Continuous variables are presented as means ± standard deviations, whereas categorical variables as absolute and relative frequencies. The statistical analysis was performed using the software STATA version 12 (Stata Corp). A P value <.05 was considered statistically significant.
Results
The mean follow-up period was 36 months (range, 12-84 months). A summary of clinical results is shown in Table 2. The pain scores improved significantly from a mean of 8.7 before surgery to 0.8 after the operation (P < .001). All functional scores improved significantly after surgery. The mean Constant score increased from 23.9 preoperatively to 85.3 postoperatively (P < .001), the mean DASH score decreased from 47.3 preoperatively to 8.97 postoperatively (P < .001), and the UCLA score increased from 15.8 preoperatively to 32.2 postoperatively (P < .001). With subjective evaluation, 96.2% of patients reported having a good or excellent result (10 excellent, 15 good) and 3.8 % (n = 1) reported fair results. No patient scored his result as poor.
TABLE 2.
Summary of Clinical Results (Pre- and Postoperative VAS Pain, Constant, Quick DASH, and UCLA Scores)a
| Preoperative | Postoperative | P Value | |
|---|---|---|---|
| VAS | 8.7 ± 1.8 | 0.8 ± 0.3 | <.001 |
| Quick DASH | 47.3 ± 15.9 | 8.97 ± 8.4 | <.001 |
| Constant | 23.9 ± 14.2 | 85.3 ± 12.8 | <.001 |
| UCLA | 15.8 ± 13 | 32.2 ± 9.2 | <.001 |
| Subjective results | |||
| Excellent | 10 | ||
| Good | 15 | ||
| Fair | 1 | ||
| Poor | 0 |
aDASH, Disabilities of the Arm, Shoulder, and Hand; UCLA, University of California Los Angeles; VAS, visual analog scale.
No residual calcifications were observed in postoperative radiographs. Postoperative tendon integrity evaluation with MRI was possible in 70% of patients. All these patients showed integrity of the rotator cuff tendons. The postoperative MRI Sugaya classification results showed 10 patients corresponding to type I category and 16 patients corresponding to type II category.
Repair using a suture anchor was performed in 22 patients (84.6%), and side-to-side repair in 4 patients (15.4%). In the suture anchor group, there were 18 complete tears and 4 partial tears grade III after total calcium removal according to Ellman classification. In the side-to-side repair group, all the repaired defects were grade II according to Ellman classification.
In the postoperative period, a frozen shoulder was observed in 2 patients (7.6%). Both patients were treated satisfactorily with physical therapy.
Discussion
Arthroscopic treatment of calcifying tendinitis of the rotator cuff has been described with favorable results.7,11,18,21,27 However, due to the heterogeneity of the techniques used in different publications and the paucity of comparative studies, there is no consensus regarding the optimal operative treatment. This study shows that in patients with calcifying tendinitis who do not respond favorably to nonoperative treatment, complete removal of calcific deposits and tendon repair without acromioplasty results in significant pain relief and improvement in functional outcomes.
The importance of removing all of the calcium is largely debated in the literature. On the one hand, some investigators suggest that complete eradication of the calcium deposits is not necessary.2,11,14,21 The rationale for this assumption is that a cell-mediated resorption can be initiated by the surgical incision of the affected tendon. Ark et al2 were the first to report no difference in functional outcomes in patients with residual calcium deposits compared with those without residual calcium deposits in postoperative control radiographs. These results were confirmed later by other authors.11,14,21 On the other hand, many authors stated that successful outcomes seemed to be strongly related to the absence of calcium deposits in the tendon. Porcellini et al19 evaluated 63 patients with arthroscopic removal of calcifying tendinitis at a mean follow-up of 36 months. In the study, the authors showed that improved Constant scores were inversely related to the number and size of residual calcifications in the tendon. The strength of this study compared with previous publications is that ultrasound was used to determine the presence of residual calcifications, which is especially useful to detect microcalcifications. Other authors also report better results when complete removal of the calcifications was achieved.10,12,20
In our patients, we attempted to remove all possible calcium and degenerative tissue surrounding the lesion because we believe this could accelerate recovery and facilitate healing. As well, it is still a matter for debate whether the lesions left after the calcium removal should be repaired. While most studies focus on the evaluation of calcification residue with radiographs, little attention has been given to tendon healing. Some investigators do not routinely perform the repair of the residual tendon as they believe in the natural self-healing of the tendon.10 However, Seil et al21 evaluated patients treated with removal of calcium deposits without repair of the tendon defect, and 31% of patients showed a rotator cuff defect with ultrasound evaluation at 24-month follow-up. Moreover, in a recent retrospective study, Balke et al3 reviewed 48 patients who were available for ultrasound examination after arthroscopic removal of calcium deposits without tendon repair, showing a partial tendon tear of the supraspinatus in 11 patients (23%). On the other hand, Porcellini et al19 showed no cuff tears with ultrasound examination after the complete removal of calcific deposits at 5 years of follow-up. It is important to note that in their study, all patients with large partial tears or complete tears after calcium removal (62% of patients) were treated with tendon repair. These results were consistent with our findings. We examined 70% of our patients (21 of 30) with MRI at a mean follow-up of 36 months and no cuff tears were found. Undoubtedly, further research is needed in this field, but our study and the available evidence suggest that the repair of the defect after calcium removal has a favorable effect on tendon healing—especially in large partial tears and complete lesions.
The last controversial issue regarding operative treatment of calcifying tendinitis of the shoulder is whether it is necessary to perform acromioplasty. Some studies favor arthroscopic acromioplasty as a routine treatment for calcifications in the rotator cuff.5,23 However, numerous studies failed to prove a benefit for additional subacromial decompression.7,11,12,14,19 Marder et al15 compared 25 patients treated by debridement, with 25 patients treated by debridement and concomitant subacromial decompression, and found that the addition of acromioplasty did not add benefit and retarded return to unrestricted activity without pain. We did not perform any subacromial decompression. Acromioplasty is not supported by published clinical and basic science studies focused on the etiology and pathogenesis of calcific tendonitis.18,25 Therefore, enlarging the subacromial space does not treat the causative pathologic process.
Our study has limitations. First, this is a retrospective study and we have no control group with alternate approaches. Second, the group presents heterogeneity in terms of previous conservative treatments.
Conclusion
Arthroscopic removal of calcific deposits and tendon repair without acromioplasty yielded excellent functional outcomes with high (93%) levels of patient satisfaction with the procedure. The absence of rotator cuff tears in patients available for MRI control suggests that supraspinatus defect repair at surgery may benefit tendon healing.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Albert JD, Meadeb J, Guggenbuhl P, et al. High-energy extracorporeal shock-wave therapy for calcifying tendinitis of the rotator cuff: a randomised trial. J Bone Joint Surg Br. 2007;89:335–341. [DOI] [PubMed] [Google Scholar]
- 2. Ark JW, Flock TJ, Flatow EL, Bigliani LU. Arthroscopic treatment of calcific tendinitis of the shoulder. Arthroscopy. 1992;8:183–188. [DOI] [PubMed] [Google Scholar]
- 3. Balke M, Bielefeld R, Schmidt C, Dedy N, Liem D. Calcifying tendinitis of the shoulder: midterm results after arthroscopic treatment. Am J Sports Med. 2012;40:657–661. [DOI] [PubMed] [Google Scholar]
- 4. Bosworth B. Calcium deposits in the shoulder and subacromial bursitis; a survey of 12122 shoulders. JAMA. 1941;116:2477–2482. [Google Scholar]
- 5. de Witte PB, Selten JW, Navas A, et al. Calcific tendinitis of the rotator cuff: a randomized controlled trial of ultrasound-guided needling and lavage versus subacromial corticosteroids. Am J Sports Med. 2013;41:1665–1673. [DOI] [PubMed] [Google Scholar]
- 6. Ebenbichler GR, Erdogmus CB, Resch KL, et al. Ultrasound therapy for calcific tendinitis of the shoulder. N Engl J Med. 1999;340:1533–1538. [DOI] [PubMed] [Google Scholar]
- 7. El Shewy MT. Arthroscopic removal of calcium deposits of the rotator cuff: a 7-year follow-up. Am J Sports Med. 2011;39:1302–1305. [DOI] [PubMed] [Google Scholar]
- 8. Hofstee D-J, Gosens T, Bonnet M, De Waal Malefijt J. Calcifications in the cuff: take it or leave it? Br J Sports Med. 2007;41:832–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hsu C-J, Wang D-Y, Tseng K-F, Fong Y-C, Hsu H-C, Jim Y-F. Extracorporeal shock wave therapy for calcifying tendinitis of the shoulder. J Shoulder Elbow Surg. 2008;17:55–59. [DOI] [PubMed] [Google Scholar]
- 10. Hurt G, Baker CL. Calcific tendinitis of the shoulder. Orthop Clin North Am. 2003;34:567–575. [DOI] [PubMed] [Google Scholar]
- 11. Jacobs R, Debeer P. Calcifying tendinitis of the rotator cuff: functional outcome after arthroscopic treatment. Acta Orthop Belg. 2006;72:276–281. [PubMed] [Google Scholar]
- 12. Jerosch J, Strauss JM, Schmiel S. Arthroscopic treatment of calcific tendinitis of the shoulder. J Shoulder Elbow Surg. 1998;7:30–37. [DOI] [PubMed] [Google Scholar]
- 13. Lee S-Y, Cheng B, Grimmer-Somers K. The midterm effectiveness of extracorporeal shockwave therapy in the management of chronic calcific shoulder tendinitis. J Shoulder Elbow Surg. 2011;20:845–854. [DOI] [PubMed] [Google Scholar]
- 14. Maier D, Jaeger M, Izadpanah K, Bornebusch L, Suedkamp NP, Ogon P. Rotator cuff preservation in arthroscopic treatment of calcific tendinitis. Arthroscopy. 2013;29:824–831. [DOI] [PubMed] [Google Scholar]
- 15. Marder RA, Heiden EA, Kim S. Calcific tendonitis of the shoulder: is subacromial decompression in combination with removal of the calcific deposit beneficial? J Shoulder Elbow Surg. 2011;20:955–960. [DOI] [PubMed] [Google Scholar]
- 16. Molé D, Kempf JF, Gleyze P, Rio B, Bonnomet F, Walch G. Results of endoscopic treatment of non-broken tendinopathies of the rotator cuff. 2. Calcifications of the rotator cuff [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1993;79:532–541. [PubMed] [Google Scholar]
- 17. Oliva F, Via AG, Maffulli N. Calcific tendinopathy of the rotator cuff tendons. Sports Med Arthrosc. 2011;19:237–243. [DOI] [PubMed] [Google Scholar]
- 18. Oliva F, Via AG, Maffulli N. Physiopathology of intratendinous calcific deposition. BMC Med. 2012;10:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Porcellini G, Paladini P, Campi F, Paganelli M. Arthroscopic treatment of calcifying tendinitis of the shoulder: clinical and ultrasonographic follow-up findings at two to five years. J Shoulder Elbow Surg. 2004;13:503–508. [DOI] [PubMed] [Google Scholar]
- 20. Rizzello G, Franceschi F, Longo UG, et al. Arthroscopic management of calcific tendinopathy of the shoulder—do we need to remove all the deposit? Bull NYU Hosp Joint Dis. 2009;67:330–333. [PubMed] [Google Scholar]
- 21. Seil R, Litzenburger H, Kohn D, Rupp S. Arthroscopic treatment of chronically painful calcifying tendinitis of the supraspinatus tendon. Arthroscopy. 2006;22:521–527. [DOI] [PubMed] [Google Scholar]
- 22. Serafini G, Sconfienza LM, Lacelli F, Silvestri E, Aliprandi A, Sardanelli F. Rotator cuff calcific tendonitis: short-term and 10-year outcomes after two-needle US-guided percutaneous treatment—nonrandomized controlled trial. Radiology. 2009;252:157–164. [DOI] [PubMed] [Google Scholar]
- 23. Seyahi A, Demirhan M. Arthroscopic removal of intraosseous and intratendinous deposits in calcifying tendinitis of the rotator cuff. Arthroscopy. 2009;25:590–596. [DOI] [PubMed] [Google Scholar]
- 24. Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21:1307–1316. [DOI] [PubMed] [Google Scholar]
- 25. Uhthoff H, Loehr J. Calcific tendinopathy of the rotator cuff: pathogenesis, diagnosis, and management. J Am Acad Orthop Surg. 1997;5:183–191. [DOI] [PubMed] [Google Scholar]
- 26. Yoo JC, Koh KH, Park WH, Park JC, Kim SM, Yoon YC. The outcome of ultrasound-guided needle decompression and steroid injection in calcific tendinitis. J Shoulder Elbow Surg. 2010;19:596–600. [DOI] [PubMed] [Google Scholar]
- 27. Yoo JC, Park WH, Koh KH, Kim SM. Arthroscopic treatment of chronic calcific tendinitis with complete removal and rotator cuff tendon repair. Knee Surg Sports Traumatol Arthrosc. 2010;18:1694–1699. [DOI] [PubMed] [Google Scholar]