Abstract
Background:
Rotator cuff tendinopathy is a frequent cause of shoulder pain that can lead to decreased strength and range of motion. Failures after using the single-row technique of rotator cuff repair have led to the development of the double-row technique, which is said to allow for more anatomical restoration of the footprint.
Purpose:
To compare 5 different types of suture patterns while maintaining equality in number of anchors. The hypothesis was that the Mason-Allen–crossed cruciform transosseous-equivalent technique is superior to other suture configurations while maintaining equality in suture limbs and anchors.
Study Design:
Controlled laboratory study.
Methods:
A total of 25 fresh-frozen cadaveric shoulders were randomized into 5 suture configuration groups: single-row repair with simple stitch technique; single-row repair with modified Mason-Allen technique; double-row Mason-Allen technique; double-row cross-bridge technique; and double-row suture bridge technique. Load and displacement were recorded at 100 Hz until failure. Stiffness and bone mineral density were also measured.
Results:
There was no significant difference in peak load at failure, stiffness, maximum displacement at failure, or mean bone mineral density among the 5 suture configuration groups (P < .05).
Conclusion:
According to study results, when choosing a repair technique, other factors such as number of sutures in the repair should be considered to judge the strength of the repair.
Clinical Relevance:
Previous in vitro studies have shown the double-row rotator cuff repair to be superior to the single-row repair; however, clinical research does not necessarily support this. This study found no difference when comparing 5 different repair methods, supporting research that suggests the number of sutures and not the pattern can affect biomechanical properties.
Keywords: rotator cuff, rotator cuff repair, biomechanics, shoulder, suture pattern, arthroscopic surgery
Rotator cuff tendinopathy is a frequent cause of shoulder pain and can cause a decrease in shoulder strength and range of motion. Tears of the rotator cuff tendon can be repaired open or arthroscopically. In general, arthroscopic rotator cuff repair (RCR) has been found to have similar clinical outcomes when compared with the open technique.4,14,16,30 Some studies have shown a higher rate of tear recurrence with an open surgical technique compared with arthroscopy when patients were examined by magnetic resonance imaging (MRI)4 or ultrasonography.11 Many different repair techniques for arthroscopic RCR have been described as the orthopaedic community strives to maximize tissue integrity and healing to optimize clinical strength and rehabilitation and to reduce tear recurrence.1,7,10,15,19,22,28
Historically, RCR has been performed using the single-row configuration that consists of suture anchors placed at the anatomic footprint of the rotator cuff.31 Failure rates of the standard single-row arthroscopic RCR have led surgeons to develop alternative fixation methods such as the double-row technique.4 This technique consists of the placement of medial row anchors at the lateral margin of the articular cartilage and placement of lateral row anchors in the lateral aspect of the footprint. Use of the double-row repair allows for a more anatomical restoration of the footprint,5,21,22 increased tendon-to-bone contact area,29 decreased gap formation after cyclic loading,27 and improved initial fixation strength.1,15,19 In a study by Ma et al,19 double-row fixation constructs had a significantly higher ultimate load than 3 types of single-row configurations: 287 N versus 191, 212, and 250 N.19 Ahmad et al1 reported that double-row repair had significantly less gapping than single-row repair. However, other biomechanical studies found that there was no difference in load to failure or gap formation between single- and double-row repairs.11,19 One such study showed that increasing strength was due to an increase in the number of sutures.13
Clinically, some studies have found no difference in outcomes between single- and double-row repair techniques.6,9 However, a systematic review of clinical arthroscopic rotator cuff repair studies (ranging from 1994 to 2009) found that, in general, the double-row repair techniques had a significantly lower retear rate compared with single-row repair techniques.8 Another clinical study showed that, for similarly sized tears, the double-row repair technique exhibited improved radiographic healing compared with the single-row technique.24
The purpose of this study was to compare 5 different types of suture patterns while maintaining equality in number of anchors. Using the suture bridge technique as a baseline guide, each configuration used 4 anchors. The 5 different techniques and suture configurations were as follows: (1) single-row repair with simple stitch, (2) single-row repair using a modified Mason-Allen technique, (3) double-row modified Mason-Allen technique, (4) double-row cross-bridge technique, and (5) double-row transosseous-equivalent technique with suture bridge. Our hypothesis was that the Mason-Allen–crossed cruciform transosseous-equivalent technique, configuration 3, is superior to other suture configurations while maintaining equality in suture limbs and anchors.
Methods
A total of 25 fresh-frozen cadaveric shoulders from 15 male and 10 female donors were used for this study. The mean age of the specimens was 71.7 years (range, 62-85 years). The specimens were randomized into 1 of 5 suture configuration groups (Figure 1): (1) single-row repair with simple stitch, (2) single-row repair with modified Mason-Allen, (3) double-row Mason-Allen, (4) double-row cross bridge, and (5) double-row suture bridge. All tissues were removed from the specimen. The supraspinatus tendon was completely resected using a scalpel blade. This was completed to test only the repair and not the strength of the surrounding tissue. The supraspinatus insertion site was identified (mean anteroposterior diameter, 25 mm; mean mediolateral diameter, 17 mm). For constructs 1 through 4, we utilized 4 anchors: two 4.5-mm PEEK (polyetheretherketone) anchors (Arthrex) and two 5.5-mm titanium anchors (Arthrex), as well as 6 sutures (No. 2 FiberWire; Arthrex). For the suture bridge technique (SutureBridge; Arthrex), we used its standard 2 medial row mattress sutures with a 5.5-mm anchor and a 4-strand cross-pattern configuration with the 4.5-mm pushlock anchors peripherally and 1 suture (No. 2 FiberWire; Arthrex).
Figure 1.
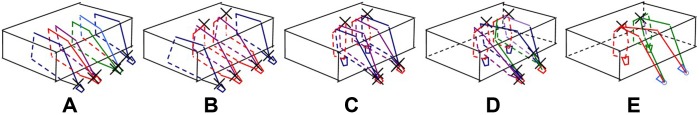
(A) Single lateral anchor row simple suture pattern; (B) lateral anchor row modified Mason-Allen and simple suture pattern; (C) double-row transosseous-equivalent anchors with modified Mason-Allen suture pattern; (D) double-row transosseous-equivalent anchors with cross-bridge suture pattern; (E) double-row transosseous-equivalent anchors with suture bridge suture pattern. X, knot; line, suture.
For the double-row repairs, the medial row was established along the junction of the articular surface of the humeral head and the medial footprint and the lateral row was established just lateral to the lateral aspect of the supraspinatus footprint. In the lateral to medial direction, the anchors were 17 mm apart, and in the anterior to posterior direction, the anchors were placed 15 mm apart. The anterior anchors were 5 mm from the anterior edge of the footprint, and the posterior anchors were 6.25 mm from the posterior aspect of the footprint. For the lateral row repairs, the anchors were placed just lateral to the lateral aspect of the supraspinatus footprint. They were placed equidistant from each other or approximately 5 mm apart. The anterior-most anchor was 5 mm from the anterior aspect of the supraspinatus footprint, and the posterior anchor was 5 mm from the posterior aspect of the footprint.
All sutures were tied with a single hole knot pusher. The knot consisted of a series of half hitches. First, 2 half hitches were placed in the same direction. The knot pusher was then switched to the other suture limb, the knot was tightened and locked, and then 3 alternating half hitches were tied. The horizontal suture pattern was tied with an anterior post on top of the tendon. The simple sutures from the lateral anchors were tied laterally on top of the anchor. All sutures were cut with an arthroscopic suture cutter.
Lateral Row With Simple Stitch Technique
This repair was composed of 4 lateral anchors (Figure 1A). The distance from the lateral anchor to the position where the suture penetrated the tendon medially was approximately 17 mm. The 2 middle anchors that had 2 sutures each were 3 mm apart. The 2 outside anchors had 1 suture each. The sutures were tied laterally at the anchors.
Lateral Anchor Row Modified Mason-Allen and Simple Suture Pattern
This repair was composed of 4 lateral anchors (Figure 1B). The 2 middle anchors had 2 sutures (4 suture limbs). The 2 suture limbs making up the horizontal mattress from the middle 2 anchors penetrated the tendon approximately 16 mm medially from the lateral anchor and were 5 mm apart. The simple suture pattern suture limb penetrated the medial tendon approximately 17 mm from the lateral anchor.
Double-Row Transosseous-Equivalent Anchors With Modified Mason-Allen Suture Pattern
The 2 medial anchors that had 1 suture each made up the horizontal mattress pattern (Figure 1C). The sutures were approximately 5 mm apart and approximately 16 mm from the lateral anchor to the medial penetration on the tendon for the horizontal mattress sutures. The lateral row that had 2 sutures each were placed in a simple pattern and inserted into the rotator cuff medially approximately 17 mm from the lateral anchor and crossed over the medial row horizontal sutures. One suture from each lateral anchor crossed over the medial row and 1 did not.
Double-Row Transosseous-Equivalent Anchors With Cross-Bridge Suture Pattern
The 2 medial anchors that had 1 suture each were 5 mm apart and 16 mm from the lateral anchor to the medial penetration on the tendon for the horizontal mattress sutures (Figure 1D). The lateral row that had 2 sutures each was placed in a simple pattern and pierced the rotator cuff medially 17 mm from the lateral anchor and crossed over the medial row horizontal sutures. The 1 suture from each lateral row was tied laterally on top of the anchor. The other suture that crossed was tied to its matching suture on the other lateral anchor in a way that each anchor had a lateral simple suture and a lateral crossing suture.
Double-Row Transosseous-Equivalent Anchors With Suture Bridge Suture Pattern
The 2 medial suture anchors each had 1 suture (Figure 1E). That suture was placed in a horizontal suture pattern that inserted into the medial aspect of the tendon 16 mm from the lateral edge of the tendon and the suture limbs were 5 mm apart. One limb of each suture that was associated with a medial anchor was crossed and matched with a suture from the other medial anchor that was not crossed, and the sutures were secured laterally to the lateral aspect of the supraspinatus footprint with a push-in knotless anchor. The 2 pushlock anchors were 15 mm apart.
Biomechanical Testing
The humerus was secured in an aluminum pot using polyester resin material (Bondo; 3M) and 4 set screws, then rigidly fixed to the base of a materials testing machine (Instron 1321; Instron Corp). It was positioned at an incline of 135° to the long axis of the tendon to model the physiological pull of the supraspinatus tendon, as described in a previous study.7 The proximal portion of the supraspinatus tendon was sewn using a Krackow suture technique into a piece of Dacron webbing material. The material used had a stiffness of 255 N/mm,23 and this minimized any effect of the material on the values reported. A custom-made clamp was used to grip the tendon/webbing complex during repair and was mounted to the crosshead of a servohydraulic materials testing machine.
Specimens were kept moist with a saline spray. A 2-N preload was applied for 10 seconds, and the specimens were loaded to failure under displacement control at a rate of 1 mm/s. Load in newtons and displacement in millimeters were recorded at 100 Hz until failure. Stiffness was calculated by determining the slope of the linear portion of the load displacement curve. Gap formation was determined using the values of displacement from the Instron testing machine.
Bone Mineral Density
Bone mineral density was measured for each specimen. A sample was taken from the greater tuberosity and the glenoid. The samples were scanned with the micro–computed tomography (µCT) system (Scanco VivaCT 40; Scanco Medical AG) using a voltage of 70 kVp and a current of 114 µA at 10-µm resolution. A cylindrical volume of interest was selected, and the bone mineral density was determined using software from the manufacturer.
Statistics
An a priori power analysis (alpha, 0.05; power, 0.80; effect size f, 0.90) revealed that 5 shoulders per group were necessary to conduct this study. Data were analyzed by analysis of variance (ANOVA) using SPSS statistical software, version 17.0 (SPSS Inc). Data were considered significant if P < .05. Results were graphed as mean ± standard error.
Results
There was no significant difference in peak load at failure for any of the groups (P > .05). The mean (±SE) peak load was 378.4 ± 154.4 N for the single-row Mason-Allen fixation, 361.0 ± 56.8 N for the double-row Mason-Allen fixation, 350.7 ± 126.0 N for the double-row suture bridge, 333.0 ± 114.4 N in the double-row cross bridge, and 309.5 ± 129.8 N for the single-row simple stitch (Figure 2).
Figure 2.
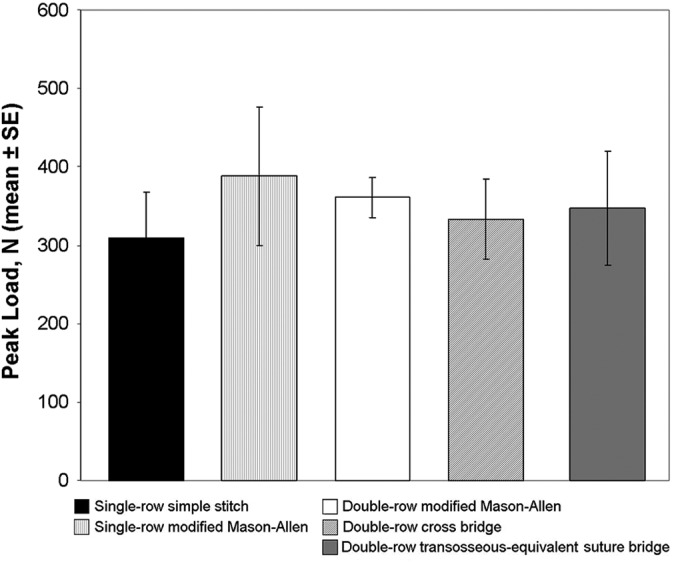
Mean peak load at failure for each suture pattern.
There was no significant difference in stiffness for any of the groups (P > .05). The double-row cross-bridge technique was the stiffest construct (20.5 ± 6.9 N/mm). The mean stiffness was 18.5 ± 6.3 N/mm for the double-row suture bridge, 17.9 ± 10.7 N/mm for the single-row Mason-Allen, 15.1 ± 4.4 N/mm for the double-row Mason-Allen, and 13.6 ± 9.0 N/mm for the single-row simple stitch (Figure 3).
Figure 3.
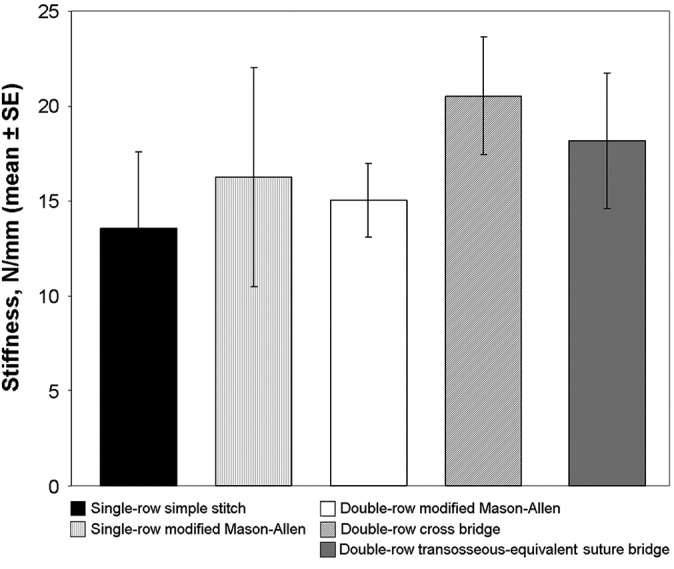
Mean stiffness for each suture pattern.
There was no significant difference in maximum displacement at failure (P > .05). The single-row Mason-Allen technique lengthened the most at failure (30.3 ± 8.3 mm). The mean maximum displacement at failure was 28.0 ± 4.9 mm for the single-row simple, 25.9 ± 10.9 mm for the double-row suture bridge, 26.8 ± 3.0 mm for the double-row Mason-Allen, and 24.6 ± 5.6 mm for the double-row cross-bridge technique (Figure 4).
Figure 4.
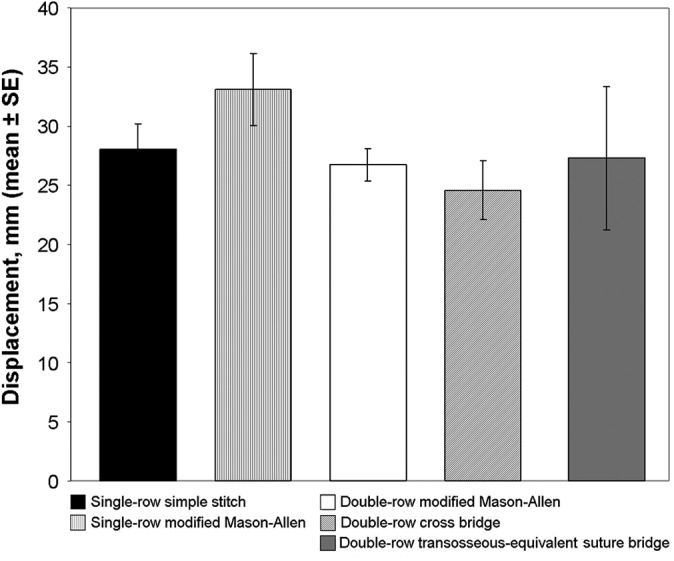
Mean displacement for each suture pattern.
For the single-row simple stitch, 3 of the repairs failed when the suture tore through the tissue, 1 failed at the anchor, and 1 failed when the tissue tore through the anchors. For the double-row Mason-Allen technique, all failures occurred when the suture tore through the tissue. For the single-row Mason-Allen technique, the majority of the failures were again at the tissue. However, 1 failure occurred at the anchor and in 1 case the suture itself broke. In the double-row cross-bridge group, again, 4 of the specimens failed when the tissue tore and 1 failed at the anchor. In the double-row suture bridge group, 2 failed when the suture tore through the tissue, 2 failed at the anchor, and 1 failed when the suture broke.
The mean bone mineral density for each group was (1) 767.8 ± 39.3 mgHa/cm3, (2) 763.7 ± 25.5 mgHa/cm3, (3) 764.9 ± 37.5 mgHa/cm3, (4) 737.8 ± 51.8 mgHa/cm3, and (5) 763.0 ± 34.7 mgHa/cm3. There was no significant difference between the groups (P > .05).
Discussion
The purpose of this study was to examine the load to failure, stiffness, and maximum displacement at failure of 5 different suture patterns commonly used for rotator cuff repair at time zero. The number of anchors was consistent between the groups to examine suture pattern only. These results did not confirm our original hypothesis that the Mason-Allen–crossed cruciform transosseous-equivalent technique, configuration 3, is superior to other suture configurations while maintaining equality in suture limbs and anchors. We found no significant difference in the biomechanical properties of these patterns. All had very similar load to failure and stiffness values.
Previous in vitro studies have shown the double-row repair to be superior to the single-row repair.1,5,15,18–22,26,27,29 Ma et al19 compared the double-row technique with 3 single-row techniques and found that the double-row technique had a higher load at failure than the other repair techniques. Smith et al27 compared a single-row repair with a single anchor and 2 sutures to a double-row repair with 2 anchors and 2 sutures. In this study, they found that the single-row repair had significant higher gap formation.27 There was also a trend indicating that the single row had a lower load to failure value.27 Kim et al15 also found that the double-row repair method improved strength and stiffness and more adequately restored the footprint. A recent biomechanical study examining single-row, double-row, and transosseous-equivalent techniques in an in vivo rabbit model found that the transosseous-equivalent technique was the strongest, followed by the double row and then single row.25
Other in vitro studies have found no biomechanical difference.3,17 Behrens et al3 examined the difference in gap formation between the transosseous-equivalent and transosseous-equivalent with suture bridge. In this study, they used 4 sutures in each group.3 They did not find a significant difference between the RCR techniques.3 This study examined cyclic loading only, not load to failure.3 Lorbach et al17 examined the biomechanical properties and footprint coverage of single- and double-row repairs in medium to large rotator cuff repairs. They found similar values for cyclic displacement and load to failure.17 They also found that while the double-row technique had a larger footprint, both techniques achieved complete footprint coverage.17
A recent study examined the strength of single-row repair using 2, 4, and 6 sutures and a 4-suture double-row repair.13 This study showed increasing strength as the number of sutures was increased.13 The 4-suture double-row repair was similar to the simple 4-suture repair.13 Our results somewhat support the research that suggests that the number of sutures and not the pattern can affect biomechanical properties, although the constructs with 4 sutures did not have higher load to failure than the suture bridge technique, which consisted of 2 sutures.
Clinical studies have generally reported no difference in clinical outcomes between single- and double-row repairs,2,6,7,12,28 although radiological differences28 and improvement in footprint coverage has been noted.5 A prospective study examining the difference in outcomes for patients with a supraspinatus tear repaired with a modified single-row Masson-Allen technique or a modified suture bridge double-row technique found no significant difference between the 2.12 Another study prospectively compared single- versus double-row configurations for rotator cuff repair and found no difference with regard to functional shoulder scores; however, tendon healing was better with the double-row repair at 6 months using computed tomography arthrography.7 A similar study conducted by Sugaya et al28 reported no clinical difference when comparing single- with double-row repairs for rotator cuff. However, better rotator cuff integrity was shown in MRI evaluation at follow-up.28 More recently, the “transosseous-equivalent” or suture bridge configuration has been developed as an advancement of the double-row concept. A case series evaluating this technique with MRI studies concluded that 88% of the 25 patients had an intact rotator cuff repair after at least 1 year of follow-up. This indicates excellent rotator cuff healing compared with most standard arthroscopic RCR studies.10
Limitations of this study are similar to those reported for any cadaveric study, including the age of the specimens utilized. In addition, we did not examine cyclic testing because we were looking to compare the initial strength of each repair at time zero.
Conclusion
In our study, there was no significant difference in peak load or stiffness when comparing 5 different rotator cuff repair methods. These data provide information about the initial strength of the repair at time zero only and do not account for healing. According to our results, other factors should be considered when choosing a repair technique such as number of sutures in the repair to judge the strength of the repair.
Acknowledgment
The authors thank Dr Xin Jin for his assistance with biomechanical testing.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: Sutures and anchors were provided by Arthrex, and unrestricted educational grants were provided by DePuy, Smith & Nephew, and Arthrex to the Detroit Sports Medicine Foundation.
References
- 1. Ahmad CS, Kleweno C, Jacir AM, et al. Biomechanical performance of rotator cuff repairs with humeral rotation: a new rotator cuff repair failure model. Am J Sports Med. 2008;36:888–892. [DOI] [PubMed] [Google Scholar]
- 2. Aydin N, Kocaoglu B, Guven O. Single-row versus double-row arthroscopic rotator cuff repair in small- to medium-sized tears. J Shoulder Elbow Surg. 2010;19:722–725. [DOI] [PubMed] [Google Scholar]
- 3. Behrens SB, Bruce B, Zonno AJ, Paller D, Green A. Initial fixation strength of transosseous-equivalent suture bridge rotator cuff repair is comparable with transosseous repair. Am J Sports Med. 2012;40:133–140. [DOI] [PubMed] [Google Scholar]
- 4. Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15:290–299. [DOI] [PubMed] [Google Scholar]
- 5. Brady PC, Arrigoni P, Burkhart SS. Evaluation of residual rotator cuff defects after in vivo single- versus double-row rotator cuff repairs. Arthroscopy. 2006;22:1070–1075. [DOI] [PubMed] [Google Scholar]
- 6. Burks RT, Crim J, Brown N, Fink B, Greis PE. A prospective randomized clinical trial comparing arthroscopic single- and double-row rotator cuff repair: magnetic resonance imaging and early clinical evaluation. Am J Sports Med. 2009;37:674–682. [DOI] [PubMed] [Google Scholar]
- 7. Charousset C, Grimberg J, Duranthon LD, Bellaiche L, Petrover D. Can a double-row anchorage technique improve tendon healing in arthroscopic rotator cuff repair? A prospective, nonrandomized, comparative study of double-row and single-row anchorage techniques with computed tomographic arthrography tendon healing assessment. Am J Sports Med. 2007;35:1247–1253. [DOI] [PubMed] [Google Scholar]
- 8. Duquin TR, Buyea C, Bisson LJ. Which method of rotator cuff repair leads to the highest rate of structural healing? A systematic review. Am J Sports Med. 2010;38:835–841. [DOI] [PubMed] [Google Scholar]
- 9. Franceschi F, Ruzzini L, Longo UG, et al. Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: a randomized controlled trial. Am J Sports Med. 2007;35:1254–1260. [DOI] [PubMed] [Google Scholar]
- 10. Frank JB, ElAttrache NS, Dines JS, Blackburn A, Crues J, Tibone JE. Repair site integrity after arthroscopic transosseous-equivalent suture-bridge rotator cuff repair. Am J Sports Med. 2008;36:1496–1503. [DOI] [PubMed] [Google Scholar]
- 11. Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-A:219–224. [DOI] [PubMed] [Google Scholar]
- 12. Gerhardt C, Hug K, Pauly S, Marnitz T, Scheibel M. Arthroscopic single-row modified Mason-Allen repair versus double-row suture bridge reconstruction for supraspinatus tendon tears: a matched-pair analysis. Am J Sports Med. 2012;40:2777–2785. [DOI] [PubMed] [Google Scholar]
- 13. Jost PW, Khair MM, Chen DX, Wright TM, Kelly AM, Rodeo SA. Suture number determines strength of rotator cuff repair. J Bone Joint Surg Am. 2012;94:e100. [DOI] [PubMed] [Google Scholar]
- 14. Kang L, Henn RF, Tashjian RZ, Green A. Early outcome of arthroscopic rotator cuff repair: a matched comparison with mini-open rotator cuff repair. Arthroscopy. 2007;23:573–582. [DOI] [PubMed] [Google Scholar]
- 15. Kim DH, Elattrache NS, Tibone JE, et al. Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med. 2006;34:407–414. [DOI] [PubMed] [Google Scholar]
- 16. Liem D, Bartl C, Lichtenberg S, Magosch P, Habermeyer P. Clinical outcome and tendon integrity of arthroscopic versus mini-open supraspinatus tendon repair: a magnetic resonance imaging-controlled matched-pair analysis. Arthroscopy. 2007;23:514–521. [DOI] [PubMed] [Google Scholar]
- 17. Lorbach O, Kieb M, Raber F, Busch LC, Kohn D, Pape D. Comparable biomechanical results for a modified single-row rotator cuff reconstruction using triple-loaded suture anchors versus a suture-bridging double-row repair. Arthroscopy. 2012;28:178–187. [DOI] [PubMed] [Google Scholar]
- 18. Lorbach O, Pape D, Raber F, Busch LC, Kohn D, Kieb M. Influence of the initial rupture size and tendon subregion on three-dimensional biomechanical properties of single-row and double-row rotator cuff reconstructions. Knee Surg Sports Traumatol Arthrosc. 2012;20:2139–2147. [DOI] [PubMed] [Google Scholar]
- 19. Ma CB, Comerford L, Wilson J, Puttlitz CM. Biomechanical evaluation of arthroscopic rotator cuff repairs: double-row compared with single-row fixation. J Bone Joint Surg Am. 2006;88:403–410. [DOI] [PubMed] [Google Scholar]
- 20. Ma CB, MacGillivray JD, Clabeaux J, Lee S, Otis JC. Biomechanical evaluation of arthroscopic rotator cuff stitches. J Bone Joint Surg Am. 2004;86-A:1211–1216. [DOI] [PubMed] [Google Scholar]
- 21. Mazzocca AD, Millett PJ, Guanche CA, Santangelo SA, Arciero RA. Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med. 2005;33:1861–1868. [DOI] [PubMed] [Google Scholar]
- 22. Meier SW, Meier JD. The effect of double-row fixation on initial repair strength in rotator cuff repair: a biomechanical study. Arthroscopy. 2006;22:1168–1173. [DOI] [PubMed] [Google Scholar]
- 23. Pandhi NG, Esquivel AO, Hanna JD, Lemos DW, Staron JS, Lemos SE. The biomechanical stability of distal clavicle excision versus symmetric acromioclavicular joint resection. Am J Sports Med. 2013;41:291–295. [DOI] [PubMed] [Google Scholar]
- 24. Pennington WT, Gibbons DJ, Bartz BA, et al. Comparative analysis of single-row versus double-row repair of rotator cuff tears. Arthroscopy. 2010;26:1419–1426. [DOI] [PubMed] [Google Scholar]
- 25. Quigley RJ, Gupta A, Oh JH, et al. Biomechanical comparison of single-row, double-row, and transosseous-equivalent repair techniques after healing in an animal rotator cuff tear model. J Orthop Res. 2013;31:1254–1260. [DOI] [PubMed] [Google Scholar]
- 26. Salata MJ, Sherman SL, Lin EC, et al. Biomechanical evaluation of transosseous rotator cuff repair: do anchors really matter? Am J Sports Med. 2013;41:283–290. [DOI] [PubMed] [Google Scholar]
- 27. Smith CD, Alexander S, Hill AM, et al. A biomechanical comparison of single and double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2006;88:2425–2431. [DOI] [PubMed] [Google Scholar]
- 28. Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005;21:1307–1316. [DOI] [PubMed] [Google Scholar]
- 29. Tuoheti Y, Itoi E, Yamamoto N, et al. Contact area, contact pressure, and pressure patterns of the tendon-bone interface after rotator cuff repair. Am J Sports Med. 2005;33:1869–1874. [DOI] [PubMed] [Google Scholar]
- 30. Verma NN, Dunn W, Adler RS, et al. All-arthroscopic versus mini-open rotator cuff repair: a retrospective review with minimum 2-year follow-up. Arthroscopy. 2006;22:587–594. [DOI] [PubMed] [Google Scholar]
- 31. Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19:116–120. [DOI] [PubMed] [Google Scholar]


