Abstract
Background:
Multiple meta-analyses have been published in efforts to determine whether operative or nonoperative treatment of Achilles tendon ruptures affords superior outcomes.
Purpose:
To perform a systematic review of overlapping meta-analyses comparing operative and nonoperative treatment of Achilles tendon ruptures to determine which meta-analyses provide the highest level of evidence for treatment recommendations.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
A systematic review of the literature was performed to identify meta-analyses that fit the study inclusion criteria. Data were extracted from these meta-analyses regarding patient outcomes and reruptures. Meta-analysis quality was assessed using the Oxman-Guyatt and QUOROM (Quality of Reporting of Meta-analyses) systems. The Jadad algorithm was applied to determine the meta-analyses with the highest level of evidence.
Results:
Nine meta-analyses met the eligibility criteria, with all but 1 study including level 1 evidence. A total of 5842 patients were included. Seven studies found a higher rate of rerupture in the nonoperative group but a higher rate of complications in the operative group. One study found no differences in rerupture or complication rates, and 1 study found surgery decreased rerupture rates only when compared with nonoperative treatment without a functional brace. Three studies also identified an earlier return to work in the operative group. Almost all (8 of 9) of the meta-analyses had Oxman-Guyatt scores >3, indicating no major flaws.
Conclusion:
Operative treatment of Achilles tendon ruptures decreases rerupture rates but increases the risk for minor complications when compared with nonoperative treatment. Additionally, surgical treatment may allow earlier return to work.
Keywords: Achilles tendon, rupture, complication, nonoperative meta-analysis
Achilles tendon ruptures are a common problem facing both elite and recreational athletes.11,12 Achilles tendon ruptures are more than 3 times more common in men, and often occur in recreational athletes in their third or fourth decades of life who lead mostly sedentary lifestyles except on the weekends (ie, “weekend warriors”).4,11 Over the past several years, there has been a decline in the number of Achilles ruptures that are treated operatively, with a resultant increase in nonoperative treatment.4 The evidence surrounding this shift in treatment of Achilles tendon injuries varies widely. Some studies have demonstrated no significant difference in strength or rerupture rates in operative versus nonoperative treatment of Achilles tendon ruptures when the nonoperative patients were treated with an accelerated rehabilitation protocol.7 Others, however, have shown a significant increase in the rerupture rates of nonoperatively treated Achilles tendon injuries compared with patients treated surgically.20
The purpose of this study was to conduct a systematic review of overlapping meta-analyses comparing operative with nonoperative treatment for Achilles tendon ruptures to determine the discrepancy between meta-analyses and to determine which literature offers the best available evidence. The aims of this study were to (1) conduct a systematic review of all meta-analyses comparing operative and nonoperative treatment of Achilles tendon ruptures, (2) provide an analytic framework for interpreting the presently discordant best available evidence to develop treatment recommendations, and (3) identify gaps in the literature that require continued investigation. We hypothesized that operative treatment of Achilles tendon ruptures would offer a lower rate of rerupture but a higher complication rate than would nonoperative treatment.
Methods
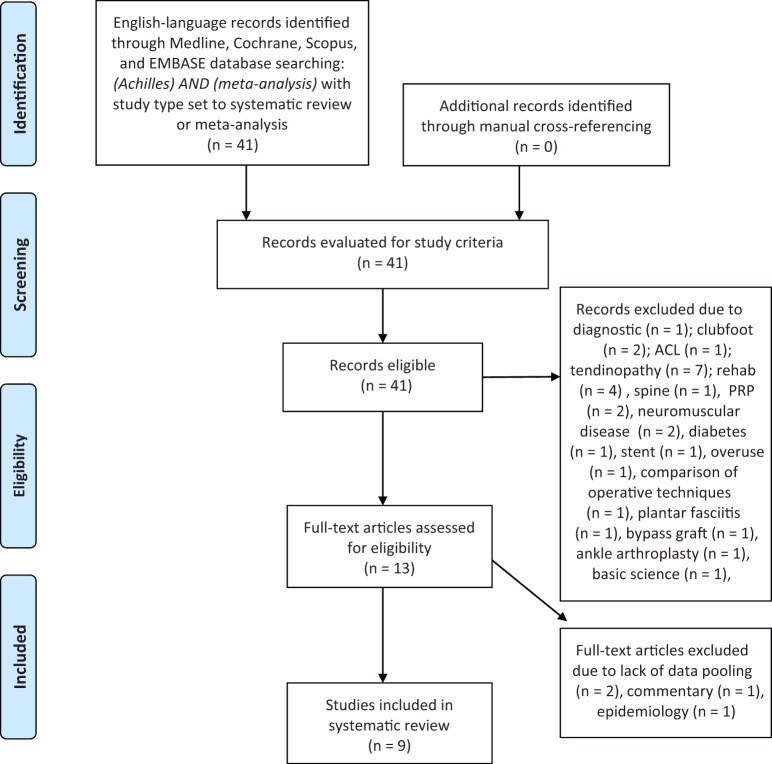
A systematic review of the literature was performed using MEDLINE, Cochrane Database of Systematic Reviews, SCOPUS, and EMBASE databases. The search methodology was limited to English-language articles, and the search strategy included search terms “[Achilles]” and “[meta-analysis]” to remain broad. All reviewed articles were then manually cross-referenced to ensure that all eligible studies were identified. All abstracts from this search were reviewed by 2 authors (B.J.E., B.M.S.) who applied the following inclusion criteria: (1) meta-analyses that compared operative and nonoperative treatment of Achilles tendon ruptures and (2) English language. The exclusion criteria were studies that were not clinical, that did not compare operative with nonoperative treatment, and that did not perform pooling of data. Full manuscripts were obtained for studies that met both the inclusion and exclusion criteria, and the references of these studies were manually reviewed to ensure no studies were overlooked. The tables of contents for the past 2 years of the Journal of Bone and Joint Surgery, The American Journal of Sports Medicine, Foot and Ankle International, Clinical Orthopaedics and Related Research, and Arthroscopy were manually searched as well for any additional studies. A PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) flow diagram shows our study selection algorithm (Figure 1).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) flow diagram for inclusion of studies. ACL, anterior cruciate ligament; PRP, platelet-rich plasma.
The following data were extracted from the included studies: primary author, journal of publication, year of publication, conflicts of interest, levels of evidence included, number and publication dates of primary studies included, inclusion and exclusion criteria, performance of heterogeneity analytics, sample size, patient demographics, follow-up period, blinding protocols, range of motion, return to previous sporting level, plantar flexion strength, calf circumference, and return to work. The following standardized outcome scores were extracted: Functional Index of the Lower Leg and Ankle (FIL), Musculoskeletal Functional Assessment Index (MFAI), Achilles Tendon Total Rupture Score (ATRS), and Physical Activity Scale (PAS). The incidence of complications was also recorded. The following methodological characteristics were recorded: the rationale for repeating the meta-analysis, the number of possible previous meta-analyses cited relative to the number actually cited, the databases utilized in the literature search, and the conclusions of the meta-analysis as to whether operative or nonoperative treatment resulted in fewer reruptures and overall complications.
The methodological quality of the meta-analyses was scored using the QUOROM (Quality of Reporting of Meta-analyses) system.15 The purpose of this scoring system is to provide a tool for evaluating meta-analyses based on the quality of their reporting and methodology in 18 categories. There are a total of 18 possible points, and each study was awarded 1 point in each category if they met over half of the criteria given in that category. Quality of the meta-analysis was graded using the Oxman-Guyatt quality appraisal tool.16 The Modified Coleman Methodology Score (MCMS) was extracted from individual studies when available. In addition, where known biases within the reviewed literature were reported by individual trials, these were recorded.
To interpret discordant meta-analyses, the Jadad decision algorithm5 was used. Sources of discordance include differences in the clinical question, inclusion and exclusion criteria, data extraction, quality assessment, data pooling, and statistical analysis.5 Scoring was performed based on assessment of randomization, randomization methodology, double blinding, withdrawals or dropouts, and allocation concealment. The 3 lead study authors (B.J.E., R.M., B.M.S.) independently scored each study, and their results were compared to determine which of the included meta-analyses provided the current best available evidence for treatment recommendations. All statistical analyses were performed using Excel X (Microsoft Corp).
Results
The initial search revealed 52 studies, which were reduced to 9 after implementation of the inclusion criteria (Figure 1).2,6,8–10,17,18,20,21 Studies were published between 1997 and 2013, and all 9 studies performed a meta-analysis, with only 2 failing to perform a heterogeneity analysis.10,20 No study reported a conflict of interest, but 4 studies failed to report whether a conflict of interest existed.2,8,10,21 The number of patients analyzed in these studies ranged from 448 (Bhandari et al2) to 990 (Lo et al10), with an average of 730 patients per study. Seven2,6,10,17,18,20,21 of the 9 studies separately listed the number of patients in the operative and nonoperative treatment groups, with a total of 2833 listed in the operative group and 2355 in the nonoperative group. Only 1 study10 reported on the median follow-up, and no study reported on the mean time from Achilles rupture to surgery or initiation of nonoperative treatment. Two18,20 of the 9 studies reported on the specific surgical techniques used, while 1 study9 reported on percutaneous versus open repair in the operative group.
Study Results
In the 9 meta-analyses that were included, there were some areas of heterogeneity and some of agreement. Seven2,6,8–10,20,21 of the studies concluded that surgery decreased rerupture rates compared with nonoperative treatment. One study18 found no difference between rerupture rates in the operative and nonoperative groups, while 1 study17 found that surgery decreased rerupture rates when compared with conservative treatment that did not include functional rehabilitation, but that the rerupture rates were not significantly different if the nonoperative treatment group underwent functional rehabilitation. All but 1 study18 found that patients in the surgery group had more complications than the nonoperative group. These complications included an increased rate of infection2,6,8–10,20 and adhesion formation6,8,9,20 among others. Khan et al9 also found that the percutaneous surgical approach resulted in a lower complication rate than open surgery, and that nonoperative patients who underwent functional bracing had a lower complication rate than those treated in a cast. Last, 3 studies found that patients in the surgery group went back to work sooner than the nonoperative group.6,17,21
Authors’ Assessment of the Prior Meta-analysis Literature
Authors generally tended to cite most of the previously published meta-analyses. Of the 8 studies that had prior meta-analyses available to cite, all reported their rationale for repeating the meta-analysis (Table 1). Multiple reasons were cited for repeating the meta-analysis, including the inclusion criteria6,17,20,21 and differing rehabilitation protocols18 among others.
TABLE 1.
Prior Systematic Reviews or Meta-analyses Actually Cited Compared With the Maximum Number That Could Possibly Have Been Cited, in Addition to the Authors’ Rationale for Repeating the Systematic Reviewa
| First Author | Date of Publication (mo/d/y) | Date of Last Literature Search (mo/d/y) | No. of Systematic Reviews or Meta-analyses on RCTs | Rationale for Repeating Meta-analysis on RCTsb | |
|---|---|---|---|---|---|
| Possible to Cite | Actually Cited | ||||
| Lo10 | –/–/1997 | –/–/1997 | 0 | 0 | N/A |
| Bhandari2 | 7/–/2002 | 8/–/2001 | 1 | 1 | “Previous reviews did not focus solely on randomized trials comparing conservative versus surgical therapy on rerupture rates. A previous metaanalysis combined results from observational studies and randomized trials…however, observational studies are more open to bias than randomized trials, and yield different results.” |
| Khan (2005)9 | 10/–/2005 | — | 2 | 2 | “Previous reviews have examined the relative advantages of operative and nonoperative treatment. However, to our knowledge, there has not been a systematic review of different methods of nonoperative treatment, operative treatment, and postoperative splinting.” |
| Khan (2010)8 | 9/–/2010 | 7/20/2009 | 3 | 3 | “There is a lack of consensus on the best management of the acute Achilles tendon rupture.… This review presents an update of the evidence for surgical intervention formerly presented in a Cochrane review that covered all interventions for these injuries.” |
| Zhao21 | –/–/2011 | 7/–/2011 | 4 | 3 | “A previous meta-analysis by Bhandari et al comparing complications of operative with nonoperative treatment of AATR did not provide a strong recommendation for surgery. Their meta-analysis included six studies, three of which were omitted from the present meta-analysis because of inadequate reporting of results or randomization.… In order to provide strong evidence, we used a strict methodological evaluation to include or exclude a relative study. To date, no high level meta-analysis compared these two methods directly.” |
| Jiang6 | 12/9/2011 | 9/1/2011 | 4 | 3 | “… However, these meta-analyses were based on a small sample size and insufficient analyses. The need remains for strong evidence based on the latest high-quality RCTs to test the [previous 3 meta-analyses] conclusions.” |
| Wilkins20 | 7/16/2012 | — | 5 | 3 | “… Additionally, previous meta-analyses have either included lower levels of evidence or have not included 2 of the largest and most recently published randomized controlled trials.” |
| Soroceanu17 | 12/5/2012 | 12/–/2011 | 6 | 2 | “… Since the latest of the two previously published meta-analyses, several additional randomized controlled clinical trials have sought to clarify the best treatment for acute Achilles tendon rupture. These trials, particularly those using functional bracing, have challenged the conclusions of the previous meta-analyses. Because of the conflicting results in the current body of literature, a reexamination of the evidence is needed to take into consideration the new trials … Our study includes foreign-language papers, contains a substantial number of new randomized trials that have been published since 2004, and includes a subgroup analysis of the rerupture rate.” |
| van der Eng18 | –/–/2013 | 12/31/2012 | 8 | 5 | “Previous reviews and trials that compared surgical and nonsurgical treatment did not specifically focus on the rehabilitation protocol. Therefore, the goal of the present meta-analysis was to compare the rerupture rate after surgical repair of the Achilles tendon followed by early weightbearing versus conservative treatment with early weightbearing. An additional analysis was performed of surgical versus conservative management with weightbearing after 4 weeks.” |
aAATR, acute Achilles tendon rupture; N/A, not available; RCT, randomized controlled trial; VAS, visual analog scale.
bAs abstracted from manuscript.
Search Methodology
Every study included in this review queried MEDLINE as part of the literature search. However, there was significant variability in the utilization of other databases, including EMBASE, OVID, the Cochrane Database of Systematic Reviews, the Cumulative Index to Nursing and Allied Health Literature, and others (Table 2). One study10 used 2 databases, 3 studies2,18,20 used 3 databases, 4 studies8,9,17,21 used 4 databases, and 1 study6 used 5 databases. There were 41 primary studies that were variably cited in the 9 meta-analyses included in this study (Table 3). The number of studies that were cited ranged from 6 (Bhandari et al2) to 19 (Lo et al10), with an average of 9 studies cited by each meta-analysis.
TABLE 2.
Search Methodology Used by Each of the Included Studiesa
| Search Database | ||||||||
|---|---|---|---|---|---|---|---|---|
| First Author | PubMed/MEDLINE | EMBASE | Cochrane Library Databaseb | CINAHL | OVID | Other | No. of Primary Studies | Primary Studies Included Only RCTs |
| Lo10 | + | − | − | − | − | + | 19 | − |
| Bhandari2 | + | − | + | − | − | + | 6 | + |
| Khan (2005)9 | + | + | + | + | − | − | 12 | + |
| Khan (2010)8 | + | + | + | + | − | − | 12 | + |
| Zhao21 | + | + | − | − | + | + | 8 | + |
| Jiang6 | + | + | + | − | + | + | 10 | + |
| Wilkins20 | + | − | + | − | − | + | 7 | + |
| Soroceanu17 | + | + | + | − | − | + | 10 | + |
| van der Eng18 | + | − | + | − | + | − | 7 | + |
aCINAHL, Cumulative Index to Nursing and Allied Health Literature; EMBASE, Excerpta Medica Database; MEDLINE, Medical Literature Analysis and Retrieval System Online; RCT, randomized controlled trial.
b“Cochrane Library Database” refers to any of the following: Cochrane database; Cochrane Musculoskeletal Injuries Group Specialized Register; Cochrane Bone, Joint, and Muscle Trauma Group Specialized Register; Cochrane Database of Systematic Reviews; Cochrane Central Register of Controlled Trials.
TABLE 3.
Primary Studies Included in Meta-analysis
| Meta-analysis | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Primary Study | Lo10 | Bhandari2 | Khan (2005)9 | Khan (2010)8 | Zhao21 | Jiang6 | Wilkins20 | Soroceanu17 | van der Eng18 |
| Aktas 2007 | − | − | − | + | − | − | − | − | − |
| Aktas 2009 | − | − | − | + | − | − | − | − | − |
| Andersen 1986 | + | − | − | − | − | − | − | − | − |
| Bomler 1989 | + | − | − | − | − | − | − | − | − |
| Cetti 1983 | + | − | − | − | − | − | − | − | − |
| Cetti 1993 | + | + | + | + | + | + | + | + | − |
| Cetti 1994 | + | − | + | − | − | − | − | − | − |
| Coombs 1981 | − | + | − | − | − | − | − | − | − |
| Costa 2006 | − | − | − | − | − | + | − | − | + |
| Fruensgaard 1992 | + | − | − | − | − | − | − | − | − |
| Gigante 2008 | − | − | − | + | − | − | − | − | − |
| Hogsan 1990 | + | − | − | − | − | − | − | − | − |
| Jessing 1975 | + | − | − | − | − | − | − | − | − |
| Kangas 2003 | − | − | + | − | − | − | − | − | − |
| Keating 2011 | − | − | − | − | + | + | − | − | + |
| Kellam 1985 | + | − | − | − | − | − | − | − | − |
| Keller 1984 | + | − | − | − | − | − | − | − | − |
| Kerkhoffs 2002 | − | − | + | − | − | − | − | − | − |
| Lildhodlt 1976 | + | − | − | − | − | − | − | − | − |
| Lim 2001 | − | − | + | + | − | − | − | − | − |
| Maffulli 2003 | − | − | + | − | − | − | − | − | − |
| Majewski 2000 | − | + | − | − | − | − | − | + | − |
| Massari 1994 | + | − | − | − | − | − | − | − | − |
| Metz 2008 | − | − | − | + | + | + | + | + | + |
| Moller 2001 | − | + | + | + | + | + | + | + | + |
| Mortensen 1992 | + | − | − | + | − | − | − | − | − |
| Mortensen 1999 | − | − | + | − | − | − | − | − | − |
| Nilsson-Helander 2010 | − | − | − | − | + | + | + | + | + |
| Nistor 1976 | + | − | − | − | − | − | − | − | − |
| Nistor 1981 | + | + | + | + | + | + | + | + | − |
| Pajala 2009 | − | − | − | + | − | − | − | − | − |
| Persson 1979 | + | − | − | − | − | − | − | − | − |
| Petersen 2002 | − | − | + | − | − | − | − | − | − |
| Ralston 1971 | + | − | − | − | − | − | − | − | − |
| Saleh 1992 | − | − | + | − | − | − | − | − | − |
| Schroeder 1997 | − | − | + | + | − | + | − | + | − |
| Sejberg 1990 | + | − | − | − | − | − | − | − | − |
| Solveborn 1994 | + | − | − | − | − | − | − | − | − |
| Thermann 1995 | − | + | − | − | − | − | − | + | − |
| Twaddle 2007 | − | − | − | + | + | + | + | + | + |
| Willits 2010 | − | − | − | − | + | + | + | + | + |
Study Quality and Validity
Oxman-Guyatt scores were assessed for each study and ranged from 3 (Lo et al10) to 7 (Khan and Carey Smith,8 Soroceanu et al,17 and Zhao et al21), with an average of 5.67 and median of 6 (Table 4). One study10 had a score of 3 or less, meaning this was the only study flagged as having major flaws in its methodology.16 The QUOROM score was also calculated for every study and ranged from 10 (Lo et al10) to 17 (Soroceanu et al17) out of a possible 18 points. The mean QUOROM score was 14.3 while the median score was 15. Three studies8,17,21 had higher Oxman-Guyatt scores than the others with a score of 7, indicating that these studies had minimal flaws. Two of these studies8,21 had QUOROM scores of 16, while 1 study had a score of 17,17 indicating these were the highest quality studies included in this review. The Jadad algorithm identified the same 3 studies as the highest level of evidence.8,17,21
TABLE 4.
Pooled Total Group Comparisons Performed by Each Meta-analysis and the Quality Scores for Each Meta-analysisa
| Meta-analysis | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Lo10 | Bhandari2 | Khan (2005)9 | Khan (2010)8 | Zhao21 | Jiang6 | Wilkins20 | Soroceanu17 | van der Eng18 | |
| Ankle range of motion | − | − | − | − | +b | − | − | +c | − |
| Return to previous level sporting rate, RR | − | − | − | − | + | + | − | − | − |
| Return to work time | − | − | − | − | +b | − | +d | +c | − |
| Mean time for sick leave, mean difference | − | − | − | − | − | + | − | − | − |
| Strength | − | − | − | − | − | − | − | + | − |
| Calf circumference | − | − | − | − | − | − | − | + | − |
| Return to normal function, RR | − | + | − | − | − | − | − | − | − |
| Spontaneous complaints, RR | − | + | − | − | − | − | − | − | − |
| Functional outcomes | − | − | − | − | − | − | − | + | − |
| Rerupture rate | − | +b | − | − | +b | +b | +e | +b | +b |
| Complications, RR | |||||||||
| Major | − | − | − | − | + | − | − | − | + |
| Moderate | − | − | − | − | + | − | − | − | − |
| Minor | − | − | − | − | + | − | − | − | + |
| Total (rerupture + other) | − | − | − | − | + | + | − | − | + |
| Complications (not rerupture) | − | − | − | − | − | − | − | + | − |
| Total infection, RR | − | + | − | − | − | − | − | − | − |
| Superficial infection, RR | − | − | − | − | − | + | − | − | − |
| Sensibility disturbance, RR | − | − | − | − | − | + | + | − | − |
| Deep infection, RR | − | − | − | − | − | + | + | − | − |
| Rate of scar adhesions, RR | − | − | − | − | − | + | + | − | − |
| Rate of DVT, RR | − | − | − | − | − | + | + | − | − |
| QUOROM score | 10 | 12 | 15 | 16 | 16 | 16 | 14 | 17 | 13 |
| Oxman-Guyatt score | 3 | 5 | 6 | 7 | 7 | 6 | 4 | 7 | 6 |
aDVT, deep vein thrombosis; QUOROM, Quality of Reporting of Meta-analyses; RR, risk ratio.
bRisk ratio.
cFixed-effect analysis.
dMean difference.
eOdds ratio.
Heterogeneity Assessment
Of the 9 meta-analyses included in this study, 2 did not perform a heterogeneity analysis (Table 5).10,20 Five6,8,9,17,18 of the 9 studies performed subgroup and/or sensitivity analyses to assess the influence of variables such as functional bracing, prolonged immobilization, sural nerve injury, deep venous thrombosis (DVT) rate, and others on outcomes (Table 5). These studies did not show any differences in their subgroup analyses. There were several other parameters that were descriptively reviewed without application of a formal subgroup or sensitivity analysis. These parameters included sporting activity, time off from work, calf circumference, plantar flexion strength, and others.
TABLE 5.
Heterogeneity or Subgroup Analyses of Primary Studiesa
| Meta-analysis | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Lo10 | Bhandari2 | Khan (2005)9 | Khan (2010)8 | Zhao21 | Jiang6 | Wilkins20 | Soroceanu17 | van der Eng18 | |
| Statistical heterogeneity analysis | − | + | + | + | + | + | − | + | + |
| Subgroup or sensitivity analysis | |||||||||
| Rerupture rate | |||||||||
| Open operative vs nonoperative | − | − | + | + | − | − | − | − | − |
| Open vs percutaneous | − | − | + | + | − | − | − | − | − |
| Cast immobilization alone vs cast immobilization then functional bracing in operative treatment | − | − | + | − | − | − | − | − | − |
| Cast immobilization vs functional bracing in nonoperative treatment | − | − | + | − | − | − | − | − | − |
| Augmented repair vs simple repair in operative treatment | − | − | − | + | − | − | − | − | − |
| Operative vs nonoperative | |||||||||
| Patients with weightbearing initiated ≤4 wk after treatment | − | − | − | − | − | − | − | − | + |
| Patients with weightbearing initiated >4 wk after treatment | − | − | − | − | − | − | − | − | + |
| Patients with early ROM functional rehabilitation | − | − | − | − | − | − | − | + | − |
| Patients with prolonged immobilization rehabilitation protocol | − | − | − | − | − | − | − | + | − |
| Patients in only high-Jadad-score (≥4) RCTs | − | − | − | − | − | + | − | − | − |
| Adhesion rate | |||||||||
| Open operative vs nonoperative | − | − | − | + | − | − | − | − | − |
| Open vs percutaneous | − | − | − | + | − | − | − | − | − |
| Operative vs nonoperative in patients in only high-Jadad-score (≥4) RCTs | − | − | − | − | − | + | − | − | − |
| DVT rate | |||||||||
| Open operative vs nonoperative | − | − | − | + | − | − | − | − | − |
| Open vs percutaneous | − | − | − | + | − | − | − | − | − |
| Skin-related complications (other than adhesions) rate: open operative vs nonoperative | − | − | − | + | − | − | − | − | − |
| Disturbing scar/wound puckering rate: open vs percutaneous | − | − | − | + | − | − | − | − | − |
| Sural nerve injury/sensibility disturbance rate: open operative vs nonoperative | − | − | − | + | − | − | − | − | − |
| Sensibility disturbance rate: operative vs nonoperative in patients in only high-Jadad- score (≥4) RCTs | − | − | − | − | − | + | − | − | − |
| Complications excluding rerupture rate | |||||||||
| Operative vs nonoperative | − | − | + | + | − | − | − | − | − |
| Open vs percutaneous | − | − | + | − | − | − | − | − | − |
| Cast immobilization alone vs cast immobilization then functional bracing in operative treatment | − | − | + | − | − | − | − | − | − |
| All complications rate: operative vs nonoperative in patients in only high-Jadad-score (≥4) RCTs | − | − | − | − | − | + | − | − | − |
| Major complications rate | |||||||||
| Operative vs nonoperative in patients with weightbearing initiated ≤4 wk after treatment | − | − | − | − | − | − | − | − | + |
| Operative vs nonoperative in patients with weightbearing initiated >4 wk after treatment | − | − | − | − | − | − | − | − | + |
| Minor complication rate | |||||||||
| Operative vs nonoperative in patients with weightbearing initiated ≤4 wk after treatment | − | − | − | − | − | − | − | − | + |
| Operative vs nonoperative in patients with weightbearing initiated >4 wk after treatment | − | − | − | − | − | − | − | − | + |
| Total infection rate | |||||||||
| Open operative vs nonoperative | − | − | + | + | − | − | − | − | − |
| Open vs percutaneous | − | − | + | + | − | − | − | − | − |
| Deep infection rate | |||||||||
| Open operative vs nonoperative | − | − | − | + | − | − | − | − | − |
| Open vs percutaneous | − | − | − | + | − | − | − | − | − |
| Augmented repair vs simple repair in operative treatment | − | − | − | + | − | − | − | − | − |
| Operative vs nonoperative in patients in only high-Jadad-score (≥4) RCTs | − | − | − | − | − | + | − | − | − |
| Superficial infection rate | |||||||||
| Open operative vs nonoperative | − | − | − | + | − | − | − | − | − |
| Open vs percutaneous | − | − | − | + | − | − | − | − | − |
| Return to former level of sporting: open operative vs nonoperative | − | − | − | + | − | − | − | − | − |
| Sporting activity postrupture: open operative vs nonoperative | − | − | − | 0 | − | − | − | − | − |
| Time off work: open vs percutaneous | − | − | − | 0 | − | − | − | − | − |
| Satisfaction: open operative vs nonoperative | − | − | − | 0 | − | − | − | − | − |
| Range of motion: open operative vs nonoperative | − | − | − | 0 | − | − | − | − | − |
| Calf circumference: open operative vs nonoperative | − | − | − | 0 | − | − | − | − | − |
| Power of plantar flexion: open operative vs nonoperative | − | − | − | 0 | − | − | − | − | − |
| Tendon width: open operative vs nonoperative | − | − | − | 0 | − | − | − | − | − |
| Duration of operation: open vs percutaneous | − | − | − | 0 | − | − | − | − | − |
a“+” indicates formal sensitivity or subgroup analysis was performed, “−” indicates formal sensitivity or subgroup analysis was not performed, and “0” indicates descriptive data were provided or discussed, but no analysis was performed. DVT, deep vein thrombosis; RCT, randomized controlled trial; ROM, range of motion.
Outcome Measures
There was a significant amount of variability in the functional outcome measures used by each meta-analysis (Table 6). The most frequently measured outcome measures were ankle range of motion,17,18,21 ankle strength,10,17,18,20,21 time to return to work,10,17,20,21 and rerupture rate.2,6,10,17,18,20,21 Only 1 study did not report on complications.8
TABLE 6.
General Group Outcomes (Pooled or Not Pooled) That Were Assessed for and Reported by Each of the Included Studiesa
| Meta-analysis | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Lo10 | Bhandari2 | Khan (2005)9 | Khan (2010)8 | Zhao21 | Jiang6 | Wilkins20 | Soroceanu17 | van der Eng18 | |
| Functional outcome measures | |||||||||
| Ankle range of motion | − | − | − | − | + | − | − | + | + |
| Ankle strength (ie, of plantar flexion, by different means, including dynamometry) | + | − | − | − | + | − | + | + | + |
| Return to previous level of sporting | + | − | − | − | + | + | − | − | − |
| Return to work time | + | − | − | − | + | − | + | + | − |
| Mean time for sick leave | − | − | − | − | − | + | − | − | − |
| Reduction of calf circumference/calf circumference | − | − | − | − | + | − | − | + | − |
| Period of hospitalization | − | − | − | − | + | − | − | − | − |
| Tendon width | − | − | − | − | + | − | − | − | − |
| Return to normal function | − | + | − | − | − | − | − | − | − |
| Spontaneous complaints | − | + | − | − | − | − | − | − | − |
| Functional outcomes/functional recovery (by different scales) | − | − | − | − | − | + | − | + | − |
| Functional scoring scales | |||||||||
| Visual analog scale | − | − | − | − | + | − | − | − | − |
| Musculoskeletal functional assessment index | − | − | − | − | + | − | − | − | − |
| Leppilahti ankle score | − | − | − | − | + | − | − | − | − |
| Achilles tendon total rupture score | − | − | − | − | + | − | − | − | − |
| Physical activity scale | − | − | − | − | + | − | − | − | − |
| Validated functional tests | − | − | − | − | + | − | − | − | − |
| Functional index for the lower leg and ankle | − | − | − | − | + | − | − | − | − |
| Complications | |||||||||
| Rerupture rate | + | + | − | − | + | + | + | + | + |
| “Major” complications | + | − | − | − | + | − | − | − | + |
| “Moderate” complications | + | − | − | − | + | − | − | − | − |
| “Minor” complications | + | − | − | − | + | − | − | − | + |
| Total complications (rerupture + other) | + | − | − | − | + | + | − | − | + |
| Total complications (excluding rerupture) | − | − | − | − | − | − | − | + | − |
| Total infection rate | − | + | − | − | − | − | − | − | − |
| Superficial infection rate | − | − | + | − | − | + | − | − | − |
| Deep infection rate | − | − | + | − | − | + | + | − | − |
| Incidence of sensibility disturbance/sural nerve sensory disturbance | + | − | + | − | − | + | + | − | − |
| Rate of scar adhesions | + | − | + | − | − | + | + | − | − |
| Rate of DVT | + | − | − | − | − | + | + | − | − |
| Rate of extreme tendon lengthening | + | − | − | − | − | + | − | − | − |
a“+” indicates that reference to the outcome variable was made and “−” indicates that reference to the outcome variable was not made. DVT, deep vein thrombosis.
Discussion
The purpose of this study was to conduct a systematic review of overlapping meta-analyses comparing operative with nonoperative treatment for Achilles tendon ruptures to determine which literature currently offers the best available evidence. We hypothesized that operative treatment of Achilles tendon ruptures would offer a lower rate of rerupture but higher complication rate than nonoperative treatment. This hypothesis was confirmed as 7 studies2,6,8–10,20,21 out of 9 concluded that surgery decreased rerupture rates compared with nonoperative treatment, while all but 1 study18 found that patients in the surgery group had more complications than the nonoperative group.
The American Academy of Orthopaedic Surgeons (AAOS) released their clinical practice guidelines (CPGs) regarding the treatment of acute Achilles tendon ruptures in 2010.3 In the guidelines, the AAOS makes weak recommendations for treating acute Achilles tendon rupture either operatively or nonoperatively, highlighting the lack of good evidence surrounding the topic. The CPGs also came to a consensus opinion to be cautious about pursuing surgical treatment of Achilles tendon ruptures in diabetics, smokers, patients with neuropathy, and others with poor wound healing potential given the higher likelihood of potential complications and wound issues. These recommendations are similar to the results of this study in that surgery is an option for decreasing rerupture rates after Achilles tendon rupture, but that complications are often significantly higher in the operatively treated patients and should therefore be carefully weighed against the benefits of operative fixation.
Differences in complication rates among the various surgical techniques for Achilles repair should be examined, as both the AAOS recommendations and the results of this study demonstrate that there is an overall higher rate of complications in patients undergoing surgical treatment of Achilles tendon ruptures. McMahon et al14 performed a meta-analysis to compare the outcomes of open versus percutaneous minimally invasive surgical repair of Achilles tendon ruptures. The results showed that while there were no differences in rerupture rate, tissue adhesion formation, and deep infection, the percutaneous technique had a significantly lower rate of superficial wound infections. Hence, as superficial infection is a common complication plaguing patients who undergo surgical treatment of Achilles tendon ruptures, thought should be given to using percutaneous techniques to minimize wound complications postoperatively. Similarly, the ability to bear weight in the nonoperative treatment group must be clarified. Barfod et al1 recently performed a blinded randomized controlled trial regarding immediate weightbearing in patients with Achilles ruptures and found no difference in functional outcomes between the group allowed to bear weight in their ankle orthosis immediately after their injury compared with the group who could not bear weight in their ankle orthosis for 6 weeks. Hence, early weightbearing appears to be an acceptable aspect of the algorithm for nonoperative treatment of Achilles ruptures.
Eight of the 9 studies included in this review had Oxman-Guyatt scores of ≥4, indicating they did not have major flaws with their methodology. However, 38,17,21 studies had higher scores than the others, with a score of 7, indicating the studies had minimal flaws. Furthermore, of the studies with Oxman-Guyatt scores of 7, 2 studies8,21 had QUOROM scores of 16, while 1 study had a score of 17.17 Hence, while only 1 of the studies included in this review showed major flaws, these 3 studies were thought to be the highest level of evidence available on the subject of operative versus nonoperative treatment of Achilles tendon ruptures as it related to rerupture rates and complications. Application of the Jadad algorithm also confirmed that these 3 studies provided the highest level of evidence. The first of these 3 studies, by Khan and Carey Smith,8 found a significantly lower rerupture rate in the operative group, but higher rates of infection, adhesion formation, and sural nerve injury/sensibility. This study did not pool data for functional outcomes. The second study, by Zhao et al,21 found that patients who underwent surgery had a lower rerupture rate and were able to return to work sooner but had a higher rate of minor and moderate complications. There was no difference in major complications or total complications between the 2 groups.21 Finally the third study, performed by Soroceanu et al,17 found that patients in the operative group had lower rerupture rates compared with the nonoperative group only when the nonoperative group was treated without functional rehabilitation. However, when the nonoperative group was treated with functional rehabilitation, they found no difference in rerupture rates. They also found no difference in strength or calf circumference, but did find that patients in the operative group returned to work sooner, but had a higher rate of complications.
The most recent study included in this review (van der Eng et al,18 2013) had a QUOROM score of 13 and Oxman-Guyatt score of 6, indicating that it was a good study but had more flaws than the 3 previously mentioned studies. This study found no difference in rerupture rates between the 2 groups. Interestingly, it also found no difference in complication rates between groups, whereas all of the other meta-analyses included in this review found a lower complication rate in the nonoperative group.
The discordance among these studies indicates that further investigation into the topic of nonoperative versus operative treatment of Achilles tendon ruptures is warranted. Over time, the rehabilitation protocol and weightbearing restrictions, as well as the surgical techniques, have evolved. Recent studies have shown that functional rehabilitation does not increase the rate of rerupture or other complications and may lead to a lower rerupture rate and an earlier return to work.13,19 However, as presented, most current evidence favors surgical treatment over nonsurgical treatment if the primary goal is to decrease the rerupture rate, but it favors nonoperative treatment if the goal is to prevent complications other than rerupture. Hence, the decision for treatment in patients with an Achilles tendon rupture should be individualized as patients with high activity levels or challenging jobs may accept the risk of a higher complication rate to reduce the rate of rerupture while less active patients or those with comorbidities may choose the nonoperative route to decrease the risk of infection, adhesions, and other complications. Furthermore, a significant gap in the literature exists as it relates to clinical outcome scores, as these varied widely by study. If investigators could standardize the outcome scores used to evaluate patients after operative or nonoperative treatment of their Achilles rupture, it would make for easier comparisons between studies and help guide treatment.
Limitations
As this is a review of prior meta-analyses, all of the limitations that were present in each of the 9 included studies are present in this study. These include potential heterogeneity and/or nonreporting of patients lost to follow-up, as well as time from injury to surgery or initiation of nonoperative treatment. Additionally, variability in rehabilitation protocols, surgical technique, and preoperative data may confound results. The strengths of this study include its use of multiple independent validated quality assessment tools, applied by 3 of the study authors with consensus agreement, as well as inclusion of the highest quality studies surrounding the subject of Achilles ruptures.15,16 These limitations were minimized as most of the studies included in this review were of level 1 evidence, but there were still limitations present.
Conclusion
Operative treatment of Achilles tendon ruptures decreases rerupture rates but increases minor complications compared with nonoperative treatment. Surgery may allow earlier return to work.
Footnotes
One or more of the authors declared the following potential conflict of interest or source of funding: S.L. receives royalties from SLACK Inc. B.J.C. receives royalties from Arthex, DJO, and Elsevier; is a consultant for Arthrex, Regentis, and Zimmer; owns stock in Carticept and Regentis; and receives research support from Arthex, Medipost, Musculoskeletal Transplant Foundation, National Institutes of Health (NIAMS and NICHD), Zimmer, Athletico, Ossur, Smith & Nephew, and Tournier. B.R.B. receives research support from Arthrex, Conmed Linvatec, DJO, Smith & Nephew, Ossur, and Tornier and receives royalties from SLACK Inc.
References
- 1. Barfod KW, Bencke J, Lauridsen HB, Ban I, Ebskov L, Troelsen A. Nonoperative dynamic treatment of acute Achilles tendon rupture: the influence of early weight-bearing on clinical outcome: a blinded, randomized controlled trial. J Bone Joint Surg Am. 2014;96:1497–1503. [DOI] [PubMed] [Google Scholar]
- 2. Bhandari M, Guyatt GH, Siddiqui F, et al. Treatment of acute Achilles tendon ruptures: a systematic overview and metaanalysis. Clin Orthop Relat Res. 2002;(400):190–200. [DOI] [PubMed] [Google Scholar]
- 3. Chiodo CP, Glazebrook M, Bluman EM, et al. Diagnosis and treatment of acute Achilles tendon rupture. J Am Acad Orthop Surg. 2010;18:503–510. [DOI] [PubMed] [Google Scholar]
- 4. Huttunen TT, Kannus P, Rolf C, Fellander-Tsai L, Mattila VM. Acute Achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med. 2014;42:2419–2423. [DOI] [PubMed] [Google Scholar]
- 5. Jadad AR, Cook DJ, Browman GP. A guide to interpreting discordant systematic reviews. CMAJ. 1997;156:1411–1416. [PMC free article] [PubMed] [Google Scholar]
- 6. Jiang N, Wang B, Chen A, Dong F, Yu B. Operative versus nonoperative treatment for acute Achilles tendon rupture: a meta-analysis based on current evidence. Int Orthop. 2012;36:765–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Keating JF, Will EM. Operative versus non-operative treatment of acute rupture of tendo Achillis: a prospective randomised evaluation of functional outcome. J Bone Joint Surg Br. 2011;93:1071–1078. [DOI] [PubMed] [Google Scholar]
- 8. Khan RJ, Carey Smith RL. Surgical interventions for treating acute Achilles tendon ruptures. Cochrane Database Syst Rev. 2010;(9):CD003674. [DOI] [PubMed] [Google Scholar]
- 9. Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, Parker M. Treatment of acute achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2005;87:2202–2210. [DOI] [PubMed] [Google Scholar]
- 10. Lo IK, Kirkley A, Nonweiler B, Kumbhare DA. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a quantitative review. Clin J Sport Med. 1997;7:207–211. [DOI] [PubMed] [Google Scholar]
- 11. Longo UG, Petrillo S, Maffulli N, Denaro V. Acute achilles tendon rupture in athletes. Foot Ankle Clin. 2013;18:319–338. [DOI] [PubMed] [Google Scholar]
- 12. Maffulli N, Longo UG, Maffulli GD, Khanna A, Denaro V. Achilles tendon ruptures in elite athletes. Foot Ankle Int. 2011;32:9–15. [DOI] [PubMed] [Google Scholar]
- 13. Mark-Christensen T, Troelsen A, Kallemose T, Barfod KW. Functional rehabilitation of patients with acute Achilles tendon rupture: a meta-analysis of current evidence [published online July 24, 2014]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3180-5 [DOI] [PubMed] [Google Scholar]
- 14. McMahon SE, Smith TO, Hing CB. A meta-analysis of randomised controlled trials comparing conventional to minimally invasive approaches for repair of an Achilles tendon rupture. Foot Ankle Surg. 2011;17:211–217. [DOI] [PubMed] [Google Scholar]
- 15. Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354:1896–1900. [DOI] [PubMed] [Google Scholar]
- 16. Oxman AD, Guyatt GH. Validation of an index of the quality of review articles. J Clin Epidemiol. 1991;44:1271–1278. [DOI] [PubMed] [Google Scholar]
- 17. Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials. J Bone Joint Surg Am. 2012;94:2136–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. van der Eng DM, Schepers T, Goslings JC, Schep NW. Rerupture rate after early weightbearing in operative versus conservative treatment of Achilles tendon ruptures: a meta-analysis. J Foot Ankle Surg. 2013;52:622–628. [DOI] [PubMed] [Google Scholar]
- 19. Wallace RG, Heyes GJ, Michael AL. The non-operative functional management of patients with a rupture of the tendo Achillis leads to low rates of rerupture. J Bone Joint Surg Br. 2011;93:1362–1366. [DOI] [PubMed] [Google Scholar]
- 20. Wilkins R, Bisson LJ. Operative versus nonoperative management of acute Achilles tendon ruptures: a quantitative systematic review of randomized controlled trials. Am J Sports Med. 2012;40:2154–2160. [DOI] [PubMed] [Google Scholar]
- 21. Zhao HM, Yu GR, Yang YF, Zhou JQ, Aubeeluck A. Outcomes and complications of operative versus non-operative treatment of acute Achilles tendon rupture: a meta-analysis. Chin Med J (Engl). 2011;124:4050–4055. [PubMed] [Google Scholar]