Abstract
Background:
Intra-articular (IA) corticosteroid therapy has been used for the treatment of inflammation and pain in the knee since the 1950s.
Purpose:
To review the current literature on the effects of IA corticosteroids on articular cartilage.
Study Design:
Systematic review.
Methods:
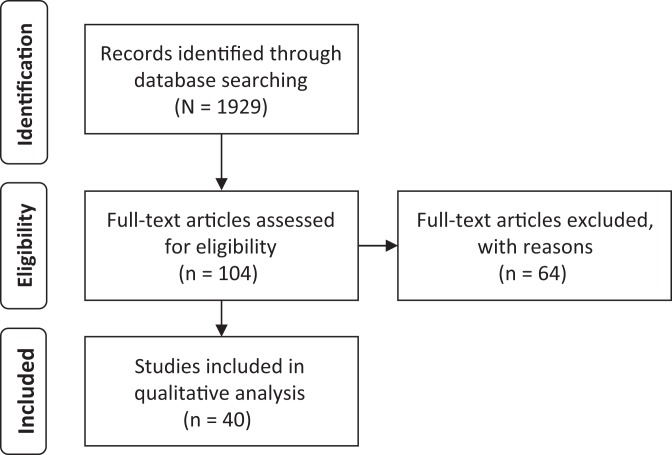
A MEDLINE and SCOPUS database search was performed, and studies were selected for basic science and clinical trial research on corticosteroids with direct outcome measures of cartilage health. Preliminary searches yielded 1929 articles, and final analysis includes 40 studies.
Results:
Methylprednisolone, dexamethasone, hydrocortisone, betamethasone, prednisolone, and triamcinolone were reported to display dose-dependent deleterious effects on cartilage morphology, histology, and viability in both in vitro and in vivo models. The beneficial animal in vivo effects of methylprednisolone, hydrocortisone, and triamcinolone occurred at low doses (usually <2-3 mg/dose or 8-12 mg/cumulative total dose in vivo), at which increased cell growth and recovery from damage was observed; the single human clinical trial indicated a beneficial effect of triamcinolone. However, at higher doses (>3 mg/dose or 18-24 mg/cumulative total dose in vivo), corticosteroids were associated with significant gross cartilage damage and chondrocyte toxicity. Dose and time dependency of corticosteroid chondrotoxicity was supported in the in vitro results, however, without clear dose thresholds.
Conclusion:
Corticosteroids have a time- and dose-dependent effect on articular cartilage, with beneficial effects occurring at low doses and durations and detrimental effects at high doses and durations. Clinically, beneficial effects are supported for IA administration, but the lowest efficacious dose should be used.
Keywords: corticosteroid, articular cartilage, chondrocytes, betamethasone, triamcinolone, methylprednisolone, prednisolone, dexamethasone, hydrocortisone
Intra-articular (IA) corticosteroid therapy has been used for the treatment of inflammation and pain in the knee since the 1950s.5 Corticosteroid therapy has been shown to be effective at temporarily alleviating joint symptoms associated with osteoarthritis and other inflammatory disorders.15 However, the long-term negative effects of these medications on articular cartilage has remained a concern.
The most commonly used corticosteroids for IA treatment are hydrocortisone, methylprednisolone, dexamethasone, betamethasone, prednisolone, and triamcinolone. They are often classified by their chemical and pharmacologic properties, including solubility and average duration. The average IA durations of action for the most common preparations are available in Table 1.
TABLE 1.
Corticosteroid Preparationsa
| Corticosteroid | Preparation | Solubility (in water) | Intra-articular Action Duration, d | Clinical Dose, mg |
|---|---|---|---|---|
| Hydrocortisone | Hydrocortisone acetate (HCA) | Insoluble | 6 | 25 |
| Methylprednisolone | Methylprednisolone acetate (MPA) | Insoluble | 7 | 10-30 |
| Dexamethasone | Dexamethasone sodium phosphate (DSP) | Soluble | 6 | 4 |
| Dexamethasone (DEX) | Insoluble | 8 | 8 | |
| Betamethasone | Betamethasone acetate (BMA) | Insoluble | 9 | 6 |
| Prednisolone | Prednisolone | Soluble | 10 | 10-30 |
| Triamcinolone | Triamcinolone acetonide (TA) | Insoluble | 14 | 10-40 |
| Triamcinolone hexacetonide (THA) | Insoluble | 21 | 20 |
This review will focus on the known effects of IA corticosteroids on articular cartilage. Existing basic science (human in vitro and animal in vivo studies) and human clinical data will be summarized and discussed individually by medication type, as generalizations about the effects of corticosteroids as a group would not be instructive.
Methods
This review article has been designed and reported in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for reporting systematic reviews.21 A MEDLINE and SCOPUS database search of studies published in English was performed in July 2014 using the following keywords: corticosteroid, articular cartilage, chondrocytes, betamethasone, triamcinolone, methylprednisolone, prednisolone, dexamethasone, and hydrocortisone. Preliminary searches yielded 1929 articles. Studies were excluded from analysis if they were duplicate articles, used genetically or chemically altered cell cultures, examined cartilage from an extra-articular source, or employed chemical cartilage damage. In vitro studies examining both healthy and osteoarthritic human cartilage were included (osteoarthritis studies are noted). All animal in vitro studies were excluded, and in vivo studies were excluded if the drug was not administered intra-articularly. Studies were also excluded if objective assessments of the articular cartilage were not implemented or if the medication dose was not recorded. Review articles were examined and used for background information. References from the included studies were reviewed for any additional relevant sources.
The final analysis included 40 articles (Figure 1). Of these, 1 was a clinically based study and 39 were basic science investigations. Data, including the dosage, duration, and method of administration; type of tissue used; animal or human model; and effect of the drug, were reviewed.
Figure 1.
PRISMA flow diagram.
Results
Hydrocortisone
The effects of hydrocortisone on articular cartilage have been investigated for both in vitro and in vivo models. These studies have utilized 3 different formulations of hydrocortisone: acetate (HCA), tert-butylacetate (HCTBA), and sodium succinate (HCSS). All compositions have a recommended dose in humans of 25 mg and an average IA duration of action of 6 days, but differ in solubility—HCA and HCTBA are insoluble in water, while HCSS is freely soluble in water.6,9,30,33
Human In Vitro Studies
A series of 2 studies by J. Wang et al39 and L. Wang et al40 studied the effect of HCSS doses in a 1-week culture. A dose of 0.2 μg/mL administered to chondrocytes was associated with the accumulation of cell-associated matrix macromolecules (especially aggrecan), increased hyaluronan levels, and inhibition of deleterious intracellular protease matrix metalloproteinase–1 (MMP-1).40 In a follow-up study, cultures treated with a range of doses (0.05, 0.2, 1.0 μg/mL) all demonstrated upregulation of cell-associated matrix aggrecan, type II collagen, and fibronectin as compared with control cultures.39 These findings indicate a beneficial effect of hydrocortisone on human chondrocyte metabolism due to stimulation of cartilage macromolecule synthesis and inhibition of degenerative enzymes.
Animal In Vivo Studies
All 5 studies examined the administration of IA hydrocortisone injections using healthy rabbit models. A single administration of 0.25 or 2.5 mg HCA (19% human weight) was examined, and an initial sharp fall in protein synthesis followed by a dose-dependent recovery to levels matching controls was found. Furthermore, at the high dose, the contralateral (uninjected) knee experienced a significant fall in protein synthesis, which may support a systemic effect of hydrocortisone.24 Another study, using 1 to 3 weekly HCA injections (0.167 and 1.67 mg/mL for 5% human weight), found no gross or microscopic disruption of the cartilage, even at superpharmacologic doses, as compared with baseline or control.3
A study of 2 to 10 weekly 25-mg injections of HCTBA (33% human weight) reported dose-dependent morphological lesions in the articular cartilage.32 Similarly, another study noted a dose-dependent response to the administration of 2 to 12 weekly 25-mg HCA injections (5% human weight), with an increasing number of cartilage fissures and cysts, a reduction in collagen production and PG content, and deleterious cellular changes including a progressive loss of mitochondria. Gross cartilage changes were only significantly different from controls at more than 8 injections (200 mg total dose) and were indistinguishable from controls at 4 injections (100 mg total dose).4 Eight weekly 25-mg HCSS injections (4% human weight) into both knees were also studied and led to significantly reduced proteoglycan synthesis.27
Summary
The basic science investigations on hydrocortisone support a dose-dependent effect on cartilage. At low doses (<6 mg), cartilage ultrastructure is maintained and gross cartilage recovery achieved. This is also seen in the in vitro studies, for which 0.05 to 1.0 μg/mL in 1-week culture demonstrated beneficial changes. However, at higher doses (>100 mg total dose), hydrocortisone administration results in gross cartilage damage and a loss of cartilage macromolecules.
Methylprednisolone
The basic science research on the effects of methylprednisolone has focused on 1 formulation of the drug, methylpredisolone acetate (MPA), which is water insoluble, has an average duration of action of 7 days, and has a recommended clinical dose of 10 to 30 mg.6,10,12,16,30
Human In Vitro Studies
In a continuous infusion pump model (to mimic joint fluid metabolism), Dragoo et al10 demonstrated that a single dose of 5-mg MPA resulted in a nonsignificant decrease in chondrocyte viability at 7 days, but in a separate 14-day culture, resulted in marked loss of viability (though not statistically significant). A study on chondrocytes from patients with primary osteoarthritis, however, found a beneficial effect of 0.01 mg/mL MPA in a range of 3- to 96-hour cultures. MPA alleviated cartilage damage through suppression of enzymes responsible for cartilage degradation, such as MMPs (types 2 and 9) and urokinase plasminogen activator.7 These chondrocyte investigations suggest that methylpredisolone has a time-dependent effect on human chondrocytes in vitro, with higher doses correlating with compromised viability but lower doses demonstrating a beneficial effect.
Animal In Vivo Studies
Murray et al26 examined 4 injections of 100 mg MPA at 2-week intervals in an equine knee model and discovered significant signs of degeneration, including decreased thickness and permeability.
Three articles examined the effect of MPA over a 12-week time course. One rabbit model (5% human weight) studied 2 doses (1.4 and 7 mg) given weekly and found dose-dependent cystic lesions, fissuring, and cell death and decreased proteoglycan levels.19 Another rabbit model (4% human weight) used 7 mg MPA administered in twice-weekly injections and similarly found increased cartilage erosions, decreased GAG content, and narrowing of joint spaces associated with MPA.2 A primate knee model (9% human weight) was used to examine 1, 2, or 6 injections of 20 mg MPA over 12 weeks and found only minor, nonsignificant, dose-dependent deleterious effects of MPA on histochemical properties of cartilage in comparison with controls.14
Two studies used a surgical injury model to examine MPA. Kopta and Blosser20 assessed the effect of 1 to 6 monthly 4-mg injections in rabbits (4% human weight) and observed a negative, dose-dependent correlation with recovery time, including decreased elasticity and thickness, and increased compressibility by the fourth injection (16 mg total dose).20 A canine model (33% human weight) with 2 injections of 20 mg MPA in 8 weeks reported positive results, including reduced incidence and size of lesions and increased chondrocyte density.29
Short-term daily methylprednisolone administration (0.1 mg/kg/d) for a range of 3 to 21 days resulted in a dose-dependent increase in articular surface fibrillation and inhibition of cell maturation after 4 daily injections in horses.38 Together, these in vivo studies of MPA have shown largely negative effects on articular cartilage morphology and protein content in both the short and long terms.
Summary
Collectively, the basic science literature on methylprednisolone reveals a large dose-dependent deleterious effect on cartilage. At high doses (>0.01 mg/mL or 7 mg), methylprednisolone appears to have catabolic effects on protein levels, chondrocyte viability, and gross cartilage morphology. At low doses (<0.01 mg/mL), positive effects may be observed, including reduction of lesions and increased chondrocyte density. Long-term methylprednisolone in vivo overwhelmingly supports deleterious effects on gross markers of cartilage health. The state of the joint (healthy, osteoarthritic, or surgically injured) and source of tissue may play a role in the tissue’s response to methylprednisolone.
Dexamethasone
Basic science investigations on the effects of dexamethasone on articular cartilage have utilized 2 preparations: dexamethasone (DEX) and dexamethasone sodium phosphate (DSP). DEX is insoluble in water, has an average IA duration of action of 8 days, and has a clinical dose of 8 mg, while DSP is soluble in water, has an action of 6 days, and a recommended dose of 4 mg.6,30
Human In Vitro Studies
There have been 5 in vitro studies on human chondrocytes, 4 of which suggest a detrimental effect of dexamethasone on cell viability and cartilage extracellular matrix. Su et al35 studied human osteoarthritic chondrocytes cultured for 1 day in 2.5, 25, 76, and 153 μM DEX and observed a significant down-regulation of the beneficial glycoprotein TIMP-3 in all cultures.35 Three DEX dosages (50, 100, and 150 μM) were studied in 1-, 2-, 3-, or 7-day cultures, and a time- and dose-dependent depression of transcription of Sox9, Col-II, and aggrecan, as well as a time- and dose-inhibition of chondrocyte growth, was reported after 3 days at the 2 highest doses.34 Another study examined human osteoarthritic chondrocytes at 25 μg/mL DEX for 24 and 48 hours. A time-dependent detrimental effect was observed, including significantly reduced cell viability and proteins responsible for proliferation and significant upregulation of proteins responsible for apoptosis for both culture durations.37 The time dependence of dexamethasone’s deleterious effects is also supported in a study on healthy human chondrocytes. Chondrocytes cultured with 100 μM/L DEX for 6, 12, and 24 hours had increased autophagy (beneficial cartilage protein turnover) but the same 100 μM/L DEX for 48 and 72 hours displayed significant chondrotoxicity, apoptosis, detrimental morphological changes, and a reduction of autophagy.22 Interestingly, in a separate investigation conducted by Dragoo et al,10 a single, clinically applicable dose of 1.17 mg DSP cultured for 7 days did not have a significant effect on healthy human chondrocyte viability. A separate 14-day trial also resulted in no significant loss of viability versus control culture. This study used a continuous infusion pump to mimic joint fluid metabolism for the cultured chondrocytes and may explain the discrepancy in results from other in vitro models.10
Animal In Vivo Studies
The only in vivo animal investigation with dexamethasone used a surgically induced cartilage damage model and intra-articularly administered 0.5 mg/kg DEX every 3 days for 3 weeks in rabbits. A beneficial effect was reported with protection of chondrocytes and gross morphology (osteophytes, cartilage lesions, discoloration, fibrillation), decreased synovial expression of MMP-3 and interleukin-1β, and decreased joint inflammation and joint tissue degradation, but also decreased synovial expression of collagen I.17
Summary
These basic science investigations demonstrate the dose and time dependence of dexamethasone toxicity. Low doses (2.5-50 μM) and short exposure times (<1 day) correlated with maintenance of cell viability and protection of cartilage morphology. At high doses (>100 μM) and longer culture times (3 days), dexamethasone may have detrimental effects on cartilage, such as decreased type II collagen levels, chondrotoxicity, and extracellular matrix breakdown. The single in vivo investigation supported a beneficial effect of repeated dexamethasone injections, perhaps due to dosage or cartilage interactions with the joint in vivo.
Betamethasone
The basic science research on the effects of betamethasone on articular cartilage has investigated 3 formulations of betamethasone, which are often used in combination. Betamethasone acetate (BMA), betamethasone sodium phosphate (BMSP), and betamethasone dipropionate (BMDPI) all have recommended human dosages of 6 mg and an average duration of action of 9 days. The formulations differ in solubility: BMA and BMDPI are insoluble in water, while BMSP is freely soluble in water.6,30
Human In Vitro Studies
Studies investigating the use of betamethasone have yielded mixed results. Farkas et al11 conducted investigations with 3.5 mg betamethasone (1 mL of 2 mg/mL BMSP with 5 mg/mL BMDPI) cultured for 2, 6, and 24 hours and found betamethasone was significantly chondrotoxic at 24 hours. Chondrocytes were also administered a single dose of BMSP and BMA at 1 mg in a culture using a continuous infusion pump to mimic joint fluid metabolism. This study demonstrated a significant decrease in chondrocyte viability at 9 and 14 days postinjection.10 However, Davis et al8 studied chondrocytes treated for 30 minutes in 0.2, 0.6, 1, 3, and 6 mg/mL BMSP and BMA combination, without benzalkonium chloride (a preservative used in clinical betamethasone combination formulations), and found no significant cell death at any dose up to 7 days after treatment. The study also compared betamethasone corticosteroids versus benzalkonium chloride and found significant cell death at even the lowest dose (0.01 mg/mL) benzalkonium chloride, which could explain discrepancies with in vivo findings.8 These studies suggest betamethasone has a deleterious effect on human chondrocytes, which may be mediated by shorter culture times and use of preparations without the preservative benzalkonium chloride.
Animal In Vivo Studies
Albano et al1 administered weekly injections for 1 to 8 weeks (0.25 mg BMDPI and 0.1 mg BMSP combination) intra-articularly to rabbits (46% human weight) and reported that 1, 2, and 4 injections (1.4 mg total dose) showed no significant differences from controls, while 6 (2.1 mg total dose) and 8 injections resulted in a significant decrease in cartilage proteoglycan content. Rabbits (46% human weight) were also administered 10 injections (3 mg BMSP and 3 mg BMA with 0.2 mg benzalkonium) over 20 weeks, and progressive articular cartilage lesions were found at both weeks 10 and 20.23 These results support dose-dependent betamethasone toxicity.
Summary
Collectively, the basic science literature on betamethasone demonstrates time- and dose-dependent deleterious effects on articular cartilage and chondrocytes. At low doses (<2.1 mg), betamethasone administration did not cause significant cartilage damage or cell death, but at higher doses (>2.1 mg), chondrotoxicity, loss of cartilage proteins, and progressive gross damage was observed. Caution should be exercised with the clinical use of betamethasone preparations containing benzalkonium chloride, as this preservative has exhibited significant chondrotoxicity.
Prednisolone
The formulations of prednisolone used in previous studies include prednisolone sodium succinate (PSS) and prednisolone acetate (PA), which have recommended clinical dose ranges of 10 to 30 mg and average IA durations of action of 10 days. PSS is slightly soluble in water while PA is insoluble in water.6,12,30
Human In Vitro Studies
Farkas et al11 treated samples of human chondrocytes as well as osteochondral explants with 25 mg PSS in 2-, 6-, and 24-hour cultures and demonstrated significant chondrotoxicity in both culture systems at 24 hours.11
Animal In Vivo Studies
Using an in vivo rabbit knee model (6% human weight), Ishikawa administered 0.58 mg/kg PA once a week for 8 weeks and found detrimental effects on gross cartilage markers, including loss of normal luster, fine fissures, thinning of cartilage, matrix fibrillation, chondrocyte distribution, and hypocellularity at 8 weeks postinjection.18
Summary
These 2 basic science studies demonstrate the prednisolone toxicity. At low culture times (6 hours), the cartilage does not exhibit significant damage, but above a time threshold (24 hours), chondrotoxicity and gross cartilage damage is found.
Triamcinolone
Basic science studies have evaluated the effect of triamcinolone acetonide (TA) and hexacetonide (THA) using chondrocyte and in vivo animal models. TA and THA are both insoluble in water, but THA is slightly more potent (recommended clinical dose of 20 mg for THA, 10-40 mg for TA) and longer acting (21 days for THA, 14 days for TA) than TA.6,10,30
Human In Vitro Studies
Monolayer chondrocytes treated for 15 minutes and cultured for 24 hours with 10 mg/mL TA were correlated with significant chondrotoxicity.36 In a culture using a continuous infusion pump to mimic joint fluid metabolism, a single dose (5 mg) of TA was studied, and a significant decrease in chondrocyte viability was observed at 14 days postinjection.10
Animal In Vivo Studies
In vivo studies evaluating triamcinolone have yielded conflicting results. Frisbie et al13 administered 2 IA injections of TA (12 mg at 13 and 27 days after surgical damage) in an equine knee model and demonstrated significantly better histomorphological parameters (cartilage fibrillation, chondrocyte necrosis, chondrone formation, and focal cell loss). A rabbit model (35% human weight) was used to examine the effect of 2 to 6 weekly (3 mg) TA injections and found dose-dependent degenerative changes in the cartilage (cyst formation and nuclear degeneration) and gross crystalline deposits.25 In a canine model (33% human weight) with 2 IA THA injections (1 month apart, 5 mg), a significant reduction in tibial plateau cartilage injury was found in the surgically induced damage group. No cartilage erosions, cell degradation, or death were noted for either the surgically damaged or THA control group compared with nontreated controls.28 Williams and Brandt41 examined a single dose of IA THA (0.4 mg/kg) in guinea pigs (8% human weight) and found no histochemical effect alone, but did find a significant protective effect on fibrillation, osteophytes, and cell viability after chemically induced cartilage damage.
Human Clinical Trial
One clinical trial by Raynauld et al31 examined the effect of 40 mg TA in osteoarthritis patients by administering injections every 3 months for 2 years. Long-term TA administration prevented narrowing of the radiographically measured joint space over a 2-year study period.31
Summary
The basic science studies on triamcinolone support disparate conclusions. Two in vitro chondrocyte investigations conclude that triamcinolone is chondrotoxic at all examined doses. However, in vivo animal and human clinical studies support triamcinolone’s possible chondral protection from injury or osteoarthritis. These effects were shown to be dose dependent, with deleterious effects on cartilage appearing after an 18-mg cumulative dose. The discrepancy in observed results may be due to heterogeneous factors such as type of animal model, dosage, or treatment time.
Conclusion
The time- and dose-dependent deleterious effects of the reviewed corticosteroids on articular cartilage are extensively supported by the basic science literature. The beneficial effects of corticosteroids occurred at low doses and short culture durations (usually <2-3 mg/dose or 8-12 mg/cumulative total dose in vivo) (Tables 2 and 3), at which increased cell growth and recovery from damage was observed. However, at higher doses and longer culture durations (>3 mg/dose or 18-24 mg/cumulative total dose in vivo), corticosteroids were associated with gross cartilage damage and chondrotoxicity. The literature demonstrates the complex effect methylpredisolone, dexamethasone, betamethasone, and hydrocortisone have on cartilage proteins (especially proteoglycan, type II collagen, aggrecan) through simultaneous mediation of the processes of protein production and breakdown. Methylprednisolone, dexamethasone, and hydrocortisone have demonstrated simultaneous mediation of both beneficial and detrimental upstream regulators of cartilage protein synthesis and breakdown, most notably the MMPs and tissue inhibitors of MMPs depending on dose and duration. The in vivo studies of methylprednisolone, hydrocortisone, and triamcinolone also support significant cartilage protection at low doses. Discrepancies in results between in vitro (support chondrotoxicity) and in vivo studies (support a protective effect) of triamcinolone, hydrocortisone, and betamethasone suggest that these corticosteroids have complex interactions within the joint. The single clinical trial examined in this review indicated a beneficial effect of IA administration of triamcinolone in osteoarthritis patients.
TABLE 2.
Human Chondrocyte In Vitro Studiesa
| Drug | Culture Duration, d | Dose, mg | Effect on Cartilage (+, ±, −) |
|---|---|---|---|
| MPA10 | 7 | 5 | ± |
| DSP10 | 7 | 1.17 | ± |
| BMSP/BMA10 | 9, 14 | 1 | − |
| BMSP with BMDPI11 | 0.83, 0.25 | 3.5 | ± |
| 1 | 3.5 | − | |
| PSS11 | 0.83, 0.25 | 25 | ± |
| 1 | 25 | − | |
| TA10 | 14 | 5 | − |
| TA36 | 0.01, 1 | 40 | − |
aBMA, betamethasone acetate; BMDPI, betamethasone dipropionate; BMSP, betamethasone sodium phosphate; DEX, dexamethasone; DSP, dexamethasone sodium phosphate; HCSS, hydrocortisone sodium succinate; MPA, methylprednisolone acetate; PSS, prednisolone sodium succinate; TA, triamcinolone acetonide.
TABLE 3.
Animal In Vivo Studiesa
| Drug | Animal | Total Dose, mg | No. of Injections | Injection Interval, d | Effect on Cartilage (+, 0, −) |
|---|---|---|---|---|---|
| Methylprednisolone acetate | Rabbit19 | 16.8 | 12 | 7 | − |
| Rabbit20 | 4-16 | 1-4 | 30 | 0 | |
| Rabbit20 | 20-24 | 5-6 | 30 | − | |
| Rabbit19 | 84 | 12 | 7 | − | |
| Rabbit2 | 168 | 24 | 3.5 | − | |
| Primate14 | 20-120 | 1, 2, or 6 | 14, 42 | 0 | |
| Canine29 | 40 | 2 | 30 | + | |
| Equine26 | 400 | 4 | 14 | − | |
| Hydrocortisone acetate | Rabbit24 | 0.25 | 1 | 0 | 0 |
| Rabbit24 | 2.5 | 1 | 0 | − | |
| Rabbit4 | 50-200 | 2-8 | 7 | 0 | |
| Rabbit4 | 200-300 | 8-12 | 7 | − | |
| Hydrocortisone sodium succinate | Rabbit27 | 200 bilaterally | 8 | 7 | − |
| Betamethasone dipropionate/sodium phosphate | Rabbit1 | 0.35-1.4 | 1, 2, or 4 | 7 | 0 |
| Rabbit1 | 2.1-2.8 | 6, 8 | 7 | − | |
| Betamethasone acetate/sodium phosphate | Rabbit23 | 60 | 10 | 14 | − |
| Triamcinolone hexacetonide | Canine28 | 10 | 2 | 30 | + |
| Triamcinolone acetonide | Equine13 | 24 | 2 | 15 | + |
aArticles were excluded from table if total dose (mg) was not available to facilitate comparison.
Footnotes
The authors reported that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Albano MB, Skroch GP, Ioshii SO, Grahels XS, de Alencar PG, Matias JE. Computerized photocolorimetric analysis of the effects of intraarticular betamethasone on the proteoglycan concentration of leporine knee cartilage matrix: influence of the number of intraarticular injections. Rev Col Bras Cir. 2009;36:256–260. [PubMed] [Google Scholar]
- 2. Badurski JE, Schwamm W, Popko J, Zimnoch L, Rogowski F, Pawlica J. Chondroprotective action of salmon calcitonin in experimental arthropathies. Calcif Tissue Int. 1991;49:27–34. [DOI] [PubMed] [Google Scholar]
- 3. Barker WD, Martinek J. An ultrastructural evaluation of the effect of hydrocortisone on rabbit cartilage. Clin Orthop Relat Res. 1976;(115):286–290. [PubMed] [Google Scholar]
- 4. Behrens F, Shepard N, Mitchell N. Alterations of rabbit articular cartilage by intra-articular injections of glucocorticoids. J Bone Joint Surg Am. 1975;57:70–76. [PubMed] [Google Scholar]
- 5. Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G. Intraarticular corticosteroid for treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. 2006;(2):CD005328. [DOI] [PubMed] [Google Scholar]
- 6. Caldwell JR. Intra-articular corticosteroids. Guide to selection and indications for use. Drugs. 1996;52:507–514. [DOI] [PubMed] [Google Scholar]
- 7. Chu SC, Yang SF, Lue KH, Hsieh YS, Li TJ, Lu KH. Naproxen, meloxicam and methylprednisolone inhibit urokinase plasminogen activator and inhibitor and gelatinases expression during the early stage of osteoarthritis. Clin Chim Acta. 2008;387:90–96. [DOI] [PubMed] [Google Scholar]
- 8. Davis D, Cyriac M, Ge D, You Z, Savoie FH. In vitro cytotoxic effects of benzalkonium chloride in corticosteroid injection suspension. J Bone Joint Surg Am. 2010;92:129–137. [DOI] [PubMed] [Google Scholar]
- 9. Douglas RJ. Corticosteroid injection into the osteoarthritic knee: drug selection, dose, and injection frequency. Int J Clin Pract. 2012;66:699–704. [DOI] [PubMed] [Google Scholar]
- 10. Dragoo JL, Danial CM, Braun HJ, Pouliot MA, Kim HJ. The chondrotoxicity of single-dose corticosteroids. Knee Surg Sports Traumatol Arthrosc. 2012;20:1809–1814. [DOI] [PubMed] [Google Scholar]
- 11. Farkas B, Kvell K, Czompoly T, Illes T, Bardos T. Increased chondrocyte death after steroid and local anesthetic combination. Clin Orthop Relat Res. 2010;468:3112–3120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Food and Drug Administration. FDA professional drug information. http://www.drugs.com/pro. Accessed April 2014.
- 13. Frisbie DD, Kawcak CE, Trotter GW, Powers BE, Walton RM, McIlwraith CW. Effects of triamcinolone acetonide on an in vivo equine osteochondral fragment exercise model. Equine Vet J. 1997;29:349–359. [DOI] [PubMed] [Google Scholar]
- 14. Gibson T, Burry HC, Poswillo D, Glass J. Effect of intra-articular corticosteroid injections on primate cartilage. Ann Rheum Dis. 1977;36:74–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Godwin M, Dawes M. Intra-articular steroid injections for painful knees. Systematic review with meta-analysis. Can Fam Physician. 2004;50:241–248. [PMC free article] [PubMed] [Google Scholar]
- 16. Hameed F, Ihm J. Injectable medications for osteoarthritis. P M R. 2012;4(suppl):S75–S81. [DOI] [PubMed] [Google Scholar]
- 17. Huebner KD, Shrive NG, Frank CB. Dexamethasone inhibits inflammation and cartilage damage in a new model of post-traumatic osteoarthritis. J Orthop Res. 2014;32:566–572. [DOI] [PubMed] [Google Scholar]
- 18. Ishikawa K. Effect of intra-articular corticosteroid on the meniscus. A histological and histochemical study in rabbit knees. J Bone Joint Surg Am. 1981;63:120–130. [PubMed] [Google Scholar]
- 19. Ishikawa K, Ohira T, Sakata H. Effects of intraarticular injection of halopredone diacetate on the articular cartilage of rabbit knees: a comparison with methylprednisolone acetate. Toxicol Appl Pharmacol. 1984;75:423–436. [DOI] [PubMed] [Google Scholar]
- 20. Kopta JA, Blosser JA. Elasticity of articular cartilage. Effects of intra-articular steroid administration and medial meniscectomy. Clin Orthop Relat Res. 1969;64:21–32. [PubMed] [Google Scholar]
- 21. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liu N, Wang W, Zhao Z, Zhang T, Song Y. Autophagy in human articular chondrocytes is cytoprotective following glucocorticoid stimulation. Mol Med Rep. 2014;9:2166–2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lutfi AM, Kosel K. Effects of intra-articularly administered corticosteroids and salicylates on the surface structure of articular cartilage. J Anat. 1978;127:393–402. [PMC free article] [PubMed] [Google Scholar]
- 24. Mankin HJ, Conger KA. The acute effects of intra-articular hydrocortisone on articular cartilage in rabbits. J Bone Joint Surg Am. 1966;48:1383–1388. [PubMed] [Google Scholar]
- 25. Moskowitz RW, Davis W, Sammarco J, Mast W, Chase SW. Experimentally induced corticosteroid arthropathy. Arthritis Rheum. 1970;13:236–243. [DOI] [PubMed] [Google Scholar]
- 26. Murray RC, DeBowes RM, Gaughan EM, Zhu CF, Athanasiou KA. The effects of intra-articular methylprednisolone and exercise on the mechanical properties of articular cartilage in the horse. Osteoarthritis Cartilage. 1998;6:106–114. [DOI] [PubMed] [Google Scholar]
- 27. Oegema TR, Jr, Behrens F. Proteoglycan aggregate synthesis in normal and chronically hydrocortisone-suppressed rabbit articular cartilage. Arch Biochem Biophys. 1981;206:277–284. [DOI] [PubMed] [Google Scholar]
- 28. Pelletier JP, Martel-Pelletier J. Protective effects of corticosteroids on cartilage lesions and osteophyte formation in the Pond-Nuki dog model of osteoarthritis. Arthritis Rheum. 1989;32:181–193. [DOI] [PubMed] [Google Scholar]
- 29. Pelletier JP, Mineau F, Raynauld JP, Woessner JF, Jr, Gunja-Smith Z, Martel-Pelletier J. Intraarticular injections with methylprednisolone acetate reduce osteoarthritic lesions in parallel with chondrocyte stromelysin synthesis in experimental osteoarthritis. Arthritis Rheum. 1994;37:414–423. [DOI] [PubMed] [Google Scholar]
- 30. Pharmacopeia.cn. United States pharmacopeia reference tables. http://www.pharmacopeia.cn/usp.asp. Accessed April 2014.
- 31. Raynauld JP, Buckland-Wright C, Ward R, et al. Safety and efficacy of long-term intraarticular steroid injections in osteoarthritis of the knee: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2003;48:370–377. [DOI] [PubMed] [Google Scholar]
- 32. Salter RB, Gross A, Hall JH. Hydrocortisone arthropathy—an experimental investigation. Can Med Assoc J. 1967;97:374–377. [PMC free article] [PubMed] [Google Scholar]
- 33. Snibbe JC, Gambardella RA. Use of injections for osteoarthritis in joints and sports activity. Clin Sports Med. 2005;24:83–91. [DOI] [PubMed] [Google Scholar]
- 34. Song YW, Zhang T, Wang WB. Gluococorticoid could influence extracellular matrix synthesis through Sox9 via p38 MAPK pathway. Rheumatol Int. 2012;32:3669–3673. [DOI] [PubMed] [Google Scholar]
- 35. Su S, Dehnade F, Zafarullah M. Regulation of tissue inhibitor of metalloproteinases-3 gene expression by transforming growth factor-β and dexamethasone in bovine and human articular chondrocytes. DNA Cell Biol. 1996;15:1039–1048. [DOI] [PubMed] [Google Scholar]
- 36. Syed HM, Green L, Bianski B, Jobe CM, Wongworawat MD. Bupivacaine and triamcinolone may be toxic to human chondrocytes: a pilot study. Clin Orthop Relat Res. 2011;469:2941–2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tu Y, Xue H, Francis W, et al. Lactoferrin inhibits dexamethasone-induced chondrocyte impairment from osteoarthritic cartilage through up-regulation of extracellular signal-regulated kinase 1/2 and suppression of FASL, FAS, and Caspase 3. Biochem Biophys Res Commun. 2013;441:249–255. [DOI] [PubMed] [Google Scholar]
- 38. Tung JT, Venta PJ, Caron JP. Inducible nitric oxide expression in equine articular chondrocytes: effects of antiinflammatory compounds. Osteoarthritis Cartilage. 2002;10:5–12. [DOI] [PubMed] [Google Scholar]
- 39. Wang J, Elewaut D, Hoffman I, Veys EM, Verbruggen G. Physiological levels of hydrocortisone maintain an optimal chondrocyte extracellular matrix metabolism. Ann Rheum Dis. 2004;63:61–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wang L, Wang J, Almqvist KF, Veys EM, Verbruggen G. Influence of polysulphated polysaccharides and hydrocortisone on the extracellular matrix metabolism of human articular chondrocytes in vitro. Clin Exp Rheumatol. 2002;20:669–676. [PubMed] [Google Scholar]
- 41. Williams JM, Brandt KD. Triamcinolone hexacetonide protects against fibrillation and osteophyte formation following chemically induced articular cartilage damage. Arthritis Rheum. 1985;28:1267–1274. [DOI] [PubMed] [Google Scholar]