Abstract
Background:
The anterior cruciate ligament (ACL) is commonly torn, and surgical reconstruction is often required to allow a patient to return to their prior level of activity. Avoiding range of motion (ROM) loss is a common goal, but little research has been done to identify when ROM loss becomes detrimental to a patient’s future function.
Purpose:
To determine whether there is a relationship between early knee side-to-side extension difference after ACL reconstruction and knee side-to-side extension difference at 12 weeks. The hypothesis was that early (within the first 8 weeks) knee side-to-side extension difference will be predictive of knee side-to-side extension difference seen at 12 weeks.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Knee side-to-side extension difference measures were taken on 74 patients undergoing ACL reconstruction rehabilitation at the initial visit and 4, 8, and 12 weeks postoperatively. Visual analog scores (VAS) and International Knee Documentation Committee (IKDC) scores were also recorded at these time frames.
Results:
There was a strong relationship between knee extension ROM at 4 and 12 weeks (r = 0.639, P < .001) and 8 and 12 weeks (r = 0.742, P < .001). When the variables of knee extension ROM at initial visit and 4 and 8 weeks were entered into a regression analysis, the predictor variable explained 61% (R2 = 0.611) of variance for knee extension ROM at 12 weeks, with 4 weeks (R2 = 0.259) explaining the majority of this variance.
Conclusion:
This study found that a patient’s knee extension at 4 weeks was strongly correlated with knee extension at 12 weeks.
Clinical Relevance:
This information may be useful for clinicians treating athletic patients who are anxious for return to sport by providing them an initial goal to work toward in hopes of ensuring successful rehabilitation of their knee.
Keywords: knee extension, ACL reconstruction, rehabilitation, range of motion
Rehabilitation of patients after anterior cruciate ligament (ACL) reconstruction plays a vital role in helping a patient return to their prior level of activity.4,8,15 A common goal of rehabilitation after ACL reconstruction includes avoiding complications such as loss of range of motion (ROM) and quadriceps femoris weakness, which is associated with loss of knee extension.8,15 Although impaired postoperative ROM remains one of the most frequent complications after ACL reconstruction,2,3,15 little research has been done to identify when loss of ROM becomes unrecoverable.
Loss of full knee extension is a potentially debilitating problem. It is thought that a lack of symmetrical knee extension after ACL reconstruction is more debilitating than preoperative instability and that a small loss of extension is particularly detrimental for the active population.16 Previous research has found that the 3 most common complications after ACL reconstruction were a loss of full extension, patellofemoral pain, and quadriceps weakness.22 Additionally, a loss of 5° of extension caused an abnormal or flexed-knee gait that led to increased joint loading, patellofemoral pain, and quadriceps weakness.14,22 Knee extension loss can reduce the amount of quadriceps extension torque,1,24 especially when the knee is close to full extension.1 Thus, these results suggest that if knee extension after ACL reconstruction is unable to be restored, the patient may have to function without the ability of the quadriceps femoris to fully activate and produce enough force required for such functional activities as squatting and ascending or descending stairs.
A lack of regaining full, symmetrical knee extension has also been found to have adverse long-term effects for the ACL-reconstructed patient population. In a 10-year minimum follow-up study, Shelbourne and Gray24 found the International Knee Documentation Committee (IKDC) and Noyes subjective scores to be significantly better in patients with normal extension when compared with patients who had less than normal extension. Interestingly, this study found that patients with meniscectomy but normal knee ROM had similar subjective scores as those with intact menisci and less than normal knee ROM (3°-5° of extension loss compared with the contralateral limb). Similarly, an additional long-term concern with knee extension ROM loss is the association with osteoarthritic (OA) knee changes. Shelbourne et al26 found that when factors of meniscal status or articular cartilage damage were controlled for, loss of normal knee ROM after ACL reconstruction at final follow-up (mean, 10.5 ± 4.5 years) was associated with a higher prevalence of OA on radiographs. With favorable patient outcomes scores and the expectation of improving the long-term health of the knee being common goals for ACL reconstruction,24,26 the proposed role knee extension plays should make this a focus of rehabilitation.
Postoperatively, a recent study supported the Knee Symmetry Model for avoiding extension loss after ACL reconstruction.5 This model emphasized the importance of symmetrical knee ROM, elimination of time frames as postoperative guidelines, unrestricted knee ROM immediately, strict bed rest for the first 5 days postoperatively, and specialized rehabilitation for the graft donor knee and the ACL-reconstructed knee. Results at a minimum of 1 year after surgery showed that 100% of patients had achieved full knee extension. Those patients who obtained knee symmetry sooner postoperatively had lower and less frequent complication rates after ACL reconstruction, but a specific time frame was not identified for when knee symmetry was achieved.5
Overall, there seems to be a lack of evidence in the literature with regard to postoperative time frames for regaining knee extension after ACL reconstruction. While it appears that a lack of full knee extension may play a role in functional deficits such as quadriceps femoris weakness,24 flexed-knee gait,14,18 and diminished hop test scores,22 it is unclear the point at which this becomes detrimental. Therefore, the intent of this study was to determine whether there was a relationship between early knee side-to-side extension difference after ACL reconstruction and knee side-to-side extension difference at 12 weeks. A second aim was to examine the relationships between knee side-to-side extension difference and patient-reported outcomes of the IKDC and visual analog scale (VAS). Finally, the third aim of the study was to use early knee extension ROM differences to predict knee extension ROM differences at 12 weeks. We hypothesized that early (within the first 8 weeks) knee side-to-side extension difference will be predictive of knee side-to-side extension difference at 12 weeks.
Methods
Design
A cross-sectional study design was used to assess the relationship between the following variables: knee side-to-side extension difference, VAS scores, and scores on the IKDC Subjective Knee Evaluation Form. Each of these variables were assessed at initial visit and 4, 8, and 12 weeks postoperatively.
Participants
Participant demographics are listed in Table 1. Patients were identified during regularly scheduled visits to participating physicians and/or physical therapists. Patients were undergoing treatment at 1 of 2 possible physical therapy clinics by a physical therapist following a standard ACL reconstruction protocol focusing on regaining symmetrical knee ROM. This protocol included passive and active ROM exercises to regain knee extension and was performed 3 times daily until symmetrical knee extension was obtained. Participating physicians included 3 orthopaedic surgeons who are within the Texas Health Ben Hogan Sports Medicine System (Fort Worth, Texas, USA). Patients were considered for study participation if it was their first ACL reconstruction (autograft hamstring, autograft patellar tendon, and allograft hamstring), were within 2 weeks of ACL reconstruction (mean initial physical therapy visit was 5 days after surgery), had not performed structured physical therapy since surgery, and were between 13 and 55 years old. All reconstruction techniques used in the ACL reconstruction were single bundle. Patients were excluded from the study for the following reasons: full-thickness chondral defect of 1.5 cm or greater7 (grade III or IV Outerbridge arthroscopic grading system), grade II or III medial collateral ligament (MCL) or lateral collateral ligament (LCL) tear, posterior cruciate ligament tear (grade I-III), simultaneous fracture with ACL tear, and meniscus repair required with ACL reconstruction (medial or lateral meniscus) due to prescribed ROM and weightbearing restrictions in the early stages (all patients included in the current study did not have weightbearing or ROM limitations). The surgeons in our study cleared patients for surgery if minimal swelling and ROM loss were present, and close communication was maintained with the treating surgeon to monitor enrollment of patients. Patients were enrolled into the study by an investigator in the outpatient sports medicine facility once they were confirmed to meet the inclusion and exclusion criteria. Participants averaged 2 times per week in physical therapy for 12 weeks. The institutional review board of Texas Health Resources approved the research procedures.
TABLE 1.
Participant Demographics After ACL Reconstructiona
| Age, y, mean ± SD | 17.7 ± 4.5 |
| Sex, n (%) | |
| Male | 35 (47.2) |
| Female | 39 (52.8) |
| Injury type, % | |
| Noncontact | 68.9 |
| Contact | 13.2 |
| Indirect contact | 17.9 |
| Involved limb, n (%) | |
| Right | 37 (50) |
| Left | 37 (50) |
| Graft, % | |
| Patellar tendon | 89.3 |
| Hamstring | 4.9 |
| Allograft | 5.8 |
| IKDC at baseline, mean ± SD | 22.2 ± 10.9 |
| VAS at baseline, mean ± SD | 5.6 ± 1.9 |
aACL, anterior cruciate ligament; IKDC, International Knee Documentation Committee; VAS, visual analog scale.
Patient-Reported Outcome Measurements
Once consent was obtained for the study, participants were asked to complete an IKDC, a VAS for pain at rest, and were measured for knee side-to-side extension difference (which included measuring into hyperextension) on the initial visit of physical therapy after ACL reconstruction. The IKDC is a knee-specific, patient-oriented outcome measure of symptoms, function, and sports activities in patients with a variety of knee impairments and conditions,13 with its validity, reliability, and responsiveness having been established in the adult and adolescent populations.11,13,23 Patients were asked to rate their pain intensity at rest by placing a mark on a 100-mm VAS with the extremes labeled “no pain” at 0 mm and “worst imaginable pain” at 100 mm. At this time, participants were also given a standard ACL reconstruction protocol that focused on regaining full, available knee extension as compared with the other limb. Patients were in a postoperative knee brace for 2 weeks that was opened to allow full available knee ROM and were on standard axillary crutches until able to demonstrate appropriate quadriceps activation for gait (single-leg stance on involved limb for 30 seconds). In addition, knee side-to-side extension difference, IKDC, and VAS were collected at time points of 4, 8, and then again at 12 weeks.
Range of Motion Measurements
Knee extension ROM measurements were taken with a goniometer with a bubble level attachment while the patient was in a supine position with both knees in extension (Figure 1). Using a goniometer to measure knee extension has been found to have an intraclass correlation coefficient (ICC) value of 0.98 for intratester reliability and 0.99 for intertester reliability.10,27 The patient was instructed to actively tighten their quadriceps and fully straighten the knee to the best of their ability, and knee ROM was measured as described by Norkin and White.17 Independent of the treating physical therapist, knee extension measurements were taken by 2 designated physical therapists. The 2 physical therapists were responsible for knee extension measurements at each time frame and had a combined experience of 20.5 years in orthopaedic rehabilitation. Prior to beginning the study, a pilot study was conducted with the 2 designated physical therapists measuring knee ROM on 25 subjects to establish interrater reliability. Reliability for knee extension was calculated and found to be good (ICC(2,1), 0.88; standard error of the mean [SEM], 0.10).
Figure 1.

Use of goniometer with bubble level to measure active knee extension.
Statistical Analysis
Pearson product moment correlation coefficients were used to determine the relationship between knee side-to-side extension difference and VAS and IKDC scores at different time points (initial visit and 4, 8, and 12 weeks). This ROM measurement was a side-to-side difference score between the involved and uninvolved limbs. In addition, a linear regression model was used to predict the effect of the knee extension variables on the outcome of knee extension ROM at 12 weeks, with an alpha level set at P < .05. A repeated-measures analysis of variance (ANOVA) was performed to examine within-subject differences of knee extension ROM. All analyses were calculated using SPSS version 19.0 (IBM). The ROM extension measures were also rated following the IKDC Knee Ligament Standard Evaluation Form (IKDC Knee Examination Form–2000), which compares extension side to side and provides the following categories: normal (within 2° of uninvolved side), nearly normal (within 3°-5°), abnormal (within 6°-10°), and severely abnormal (>10°).
Results
Correlations
Table 2 summarizes the findings of knee side-to-side extension difference across each time point (initial visit and 4, 8, and 12 weeks). A significant main effect was seen for knee extension across time (F 2,59 = 42.53, P < .001). There was a strong relationship between knee extension ROM at 4 and 12 weeks (r = 0.639, P < .001) and 8 and 12 weeks (r = 0.742, P < .001). A weak relationship was seen for knee extension ROM at initial visit and 12 weeks (r = 0.370, P = .003). For IKDC, there was a weak positive relationship between self-reported functional outcome and knee extension at 12 weeks (r = 0.343, P = .003). There was no significant relationship between VAS and knee extension at any of the time variables (P > .05).
TABLE 2.
Mean Knee Extension ROM After ACL Reconstructiona
| Time Frame | Side-to-Side Difference, deg | Involved Limb, deg | Uninvolved Limb, deg |
|---|---|---|---|
| Initial visit | 9.6 ± 5.7 | –5.2 ± 6.0 | 4.4 ± 3.5 |
| Week 4 | 4.7 ± 3.2 | –0.61 ± 3.2 | 3.9 ± 2.9 |
| Week 8 | 2.5 ± 2.5 | 1.2 ± 2.9 | 3.8 ± 2.9 |
| Week 12 | 2.0 ± 2.6 | 2.0 ± 3.1 | 4.0 ± 2.8 |
aValues are reported as mean ± SD. Mean range of motion (ROM) was calculated from active ROM measure of the involved side minus active ROM measure of the uninvolved extremity. For extension ROM, a positive number represents hyperextension past 0°. ACL, anterior cruciate ligament.
Linear Regression
When the variables of knee extension ROM at initial visit, 4, and 8 weeks were entered into a regression analysis, the predictor variables explained 61% (R 2 = 0.611) of the variance for knee extension ROM at 12 weeks, with an effect size of f 2 = 1.57. The observed post hoc power analysis was 1.0. Knee extension ROM at 4 and 8 weeks explained 46% (R 2 = 0.457) of this variance, with 4 weeks (R 2 = 0.259) explaining the majority (Figure 2). At 4 weeks, the mean involved knee extension was –0.61° ± 3.2°, mean uninvolved knee extension was 3.9° ± 2.9°, mean knee side-to-side extension difference was 4.7° ± 3.2°, IKDC was 50.2 ± 9.6, and VAS was 2.1 ± 1.7. At 12 weeks, the mean involved knee extension was 2.0° ± 3.1°, mean uninvolved knee extension was 4.0° ± 2.8°, mean knee side-to-side extension difference was 2.0° ± 2.6°, IKDC was 71.0 ± 9.2, and VAS was 0.9 ± 1.1. Table 3 provides the IKDC extension rating and the number of patients who fell into each category.
Figure 2.
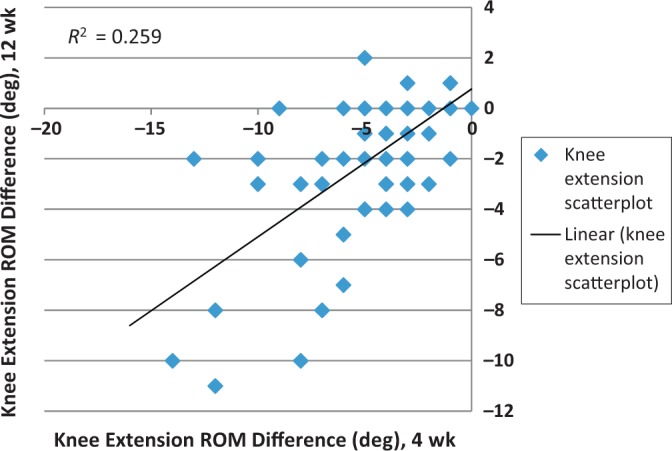
Relationship between knee extension range of motion (ROM) at 4 and 12 weeks.
TABLE 3.
Extension Ratings at 4 and 12 Weeks Using the IKDC Rating Systema
| Time Frame | Normal | Nearly Normal | Abnormal |
|---|---|---|---|
| 4 weeks | 18 (24.3) | 13 (17.6) | 4 (5.4) |
| 12 weeks | 54 (72.9) | 6 (8.1) | 1 (1.3) |
aValues are reported as n (%). IKDC, International Knee Documentation Committee.
Discussion
Regaining full ROM has been consistently found to improve long-term outcomes for ACL reconstruction patients, especially in the realm of knee extension restoration.5,20,21,24,26 Multiple studies have been conducted to determine factors that can limit a patient’s ability to regain full extension,5,12,14,19 but to our knowledge, none have determined in what time frame this extension needs to be achieved. Many studies concerning postoperative ACL rehabilitation and extension have had varying short- and long-term follow-up for assessing extension ROM. Our study found that a patient’s knee side-to-side extension difference at 4 weeks was strongly correlated with knee side-to-side extension difference at 12 weeks. Although a strong relationship was seen between the 8- and 12-week extension measure, the extension measures at 4 weeks had a stronger relationship when it came to predicting extension at 12 weeks.
Our results provide those involved with postoperative ACL rehabilitation an initial goal of obtaining nearly normal (within 3°-5° of uninvolved knee) knee extension at 4 weeks, which may be used clinically as a predictor of normal (within 2° of uninvolved knee) extension at 12 weeks, another specific time frame. The average knee extension ROM at 4 weeks for this study was 4.7° ± 3.2° side-to-side difference. Our purpose was to examine early outcomes of knee extension to provide reference guidelines for the postoperative ACL patient since, in the opinion of some clinical researchers, those who do not have extension by 6 months will likely not regain full ROM.6 From their extensive experience in ACL reconstruction rehabilitation and outcomes, Shelbourne and Klotz25 hypothesized that a reference guideline for gaining symmetrical ROM is helpful for athletic patients anxious to return to sport by providing them an initial goal to work toward. In addition, this information may provide a framework for those less active patients wanting to return to squatting, kneeling, and ascending and descending stairs.
An earlier study by Mauro et al14 had secondary findings similar to ours. While Mauro et al14 defined a loss of extension as greater than 5° side-to-side difference in knee extension at 4 weeks, our average side-to-side knee extension loss was 4.7° ± 3.2°. The primary intent of their study was to determine if stricter guidelines for determining extension loss after ACL reconstruction would find a higher rate of extension loss and different contributing factors. Retrospectively, the authors inadvertently determined that of 229 patients involved in their study, 58 lacked 5° or more of knee extension at 4 weeks, and 28 (48%) went on to have an arthroscopic debridement to achieve full extension.14 Although none of the patients in our study required secondary surgical intervention, knee extension ROM at 4 weeks seems to be a good indicator of whether restoration of knee extension is going to be an issue.
When studying long-term effects of knee extension ROM loss in ACL-reconstructed patients, Shelbourne and Gray24 found patients with normal knee ROM but meniscal removal had similar IKDC and Noyes subjective scores as those with less than normal knee ROM (3°-5° of extension loss compared with the contralateral limb) and intact menisci. This led Shelbourne and Gray24 to deduce that slight motion loss can have similar adverse effects on a patient’s subjective score as having joint damage. Additionally, based on their patient’s results at 10 to 20 years after ACL reconstruction, Shelbourne and Klotz25 published a clinical commentary stating that full, symmetrical knee ROM is the definitive factor of long-term patient satisfaction. When meniscal status and articular cartilage damage prior to surgery were normalized, Shelbourne et al26 found loss of normal knee ROM at 10-year follow-up after ACL reconstruction was associated with a higher prevalence of OA on radiographs. Patients with a >5° loss of knee extension had the highest prevalence of radiographic evidence of OA. When Shelbourne and Gray24 considered the increased rate of OA in their 10-year follow-up of patients lacking symmetrical extension after ACL reconstruction and the increased rate of OA found by Daniel et al9 in ACL-reconstructed knees with extension loss compared with ACL-deficient knees, Shelbourne and Gray24 deduced that performing an ACL reconstruction without also obtaining full knee ROM might be more detrimental than not performing a reconstruction. Our finding that knee side-to-side extension difference at 4 weeks is a good predictor of knee side-to-side extension difference at 12 weeks can provide clinicians with an initial ROM goal to avoid these adverse long-term effects.
Limitations
It is important to realize that our results are limited to a relationship between restoration of knee extension ROM at 4 and 12 weeks. Because of the relatively small sample size and the correlational approach to this study, we are unable to establish a direct cause and effect. Although our study identified the importance of restoring knee extension within 5° of the normal knee by 4 weeks, it did not detect which tissue or structures may be limiting a patient’s ability to regain extension. Future studies should include measures to identify what role these tissues are playing in extension loss and whether some are more problematic or easily managed than others.
All participants in this study averaged 2 times per week of structured physical therapy over a 12-week period; however, we cannot guarantee absolute compliance with the standardized protocol when they were not under the direct supervision of the physical therapists. We attempted to minimize noncompliance by providing education regarding the standard protocol to the participant and treating physical therapist and by having the principal investigator visit weekly with each participant during a scheduled physical therapy appointment.
Conclusion
Although impaired postoperative ROM remains one of the most frequent complications after ACL reconstruction,2,3,15 little research has been done to identify at what time frame ROM loss negatively affects outcomes. Knee side-to-side extension difference at 4 weeks was strongly correlated with knee side-to-side extension difference at 12 weeks. This information may be useful for clinicians treating an athletic patient anxious for return to sport as well as those less active patients wanting to return to traditional functional activities, such as normal gait or ascending and descending stairs, by providing them an initial goal to work toward in hopes of ensuring successful rehabilitation of their knee.
Acknowledgment
The authors thank the staff physical therapists at Texas Health Ben Hogan Sports Medicine for their help in recruitment of subjects and assistance in data collection.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Ahmad CS, Kwak SD, Ateshian GA, Warden WH, Steadman JR, Mow VC. Effects of patellar tendon adhesion to the anterior tibia on knee mechanics. Am J Sports Med. 1998;26:715–724. [DOI] [PubMed] [Google Scholar]
- 2. Allum R. Complications of arthroscopic reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2003;85:12–16. [DOI] [PubMed] [Google Scholar]
- 3. Almekinders L, Moore T, Freedman D, Taft T. Post-operative problems following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1995;3:78–82. [DOI] [PubMed] [Google Scholar]
- 4. Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries, part 2. Am J Sports Med. 2005;33:1751–1767. [DOI] [PubMed] [Google Scholar]
- 5. Biggs A, Jenkins WL, Urch SE, Shelbourne KD. Rehabilitation for patients following ACL reconstruction: a knee symmetry model. N Am J Sports Phys Ther. 2009;4:2–12. [PMC free article] [PubMed] [Google Scholar]
- 6. Bottoni CR, Liddell TR, Trainor TJ, Freccero DM, Lindell KK. Postoperative range of motion following anterior cruciate ligament reconstruction using autograft hamstrings: a prospective, randomized clinical trial of early versus delayed reconstructions. Am J Sports Med. 2008;36:656–662. [DOI] [PubMed] [Google Scholar]
- 7. Cameron ML, Briggs KK, Steadman JR. Reproducibility and reliability of the Outerbridge classification for grading chondral lesions of the knee arthroscopically. Am J Sports Med. 2003;31:83–86. [DOI] [PubMed] [Google Scholar]
- 8. Cosgarea AJ, Sebastianelli WJ, DeHaven KE. Prevention of arthrofibrosis after anterior cruciate ligament reconstruction using the central third patellar tendon autograft. Am J Sports Med. 1995;23:87–92. [DOI] [PubMed] [Google Scholar]
- 9. Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient a prospective outcome study. Am J Sports Med. 1994;22:632–644. [DOI] [PubMed] [Google Scholar]
- 10. Gogia PP, Braatz JH, Rose SJ, Norton BJ. Reliability and validity of goniometric measurements at the knee. Phys Ther. 1987;67:192–195. [DOI] [PubMed] [Google Scholar]
- 11. Higgins LD, Taylor MK, Park D, et al. Reliability and validity of the International Knee Documentation Committee (IKDC) subjective knee form. Joint Bone Spine. 2007;74:594–599. [DOI] [PubMed] [Google Scholar]
- 12. Irrgang J, Harner C. Loss of motion following knee ligament reconstruction. Sports Med. 1995;19:150–159. [DOI] [PubMed] [Google Scholar]
- 13. Irrgang JJ, Anderson AF, Boland AL, et al. Responsiveness of the international knee documentation committee subjective knee form. Am J Sports Med. 2006;34:1567–1573. [DOI] [PubMed] [Google Scholar]
- 14. Mauro CS, Irrgang JJ, Williams BA, Harner CD. Loss of extension following anterior cruciate ligament reconstruction: analysis of incidence and etiology using IKDC criteria. Arthroscopy. 2008;24:146–153. [DOI] [PubMed] [Google Scholar]
- 15. Mohtadi NG, Webster-Bogaert S, Fowler PJ. Limitation of motion following anterior cruciate ligament reconstruction. A case-control study. Am J Sports Med. 1991;19:620–624. [DOI] [PubMed] [Google Scholar]
- 16. Nabors ED, Richmond JC, Vannah WM, McConville OR. Anterior cruciate ligament graft tensioning in full extension. Am J Sports Med. 1995;23:488–492. [DOI] [PubMed] [Google Scholar]
- 17. Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry. 4th ed Philadelphia, PA: F.A. Davis; 2009. [Google Scholar]
- 18. Perry J, Antonelli D, Ford W. Analysis of knee-joint forces during flexed-knee stance. J Bone Joint Surg Am. 1975;57:961–967. [PubMed] [Google Scholar]
- 19. Petsche TS, Hutchinson MR. Loss of extension after reconstruction of the anterior cruiciate ligament. J Am Acad Orthop Surg. 1999;7:119–127. [DOI] [PubMed] [Google Scholar]
- 20. Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft a controlled, prospective trial. Am J Sports Med. 2007;35:564–574. [DOI] [PubMed] [Google Scholar]
- 21. Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction differences and similarities. Am J Sports Med. 2005;33:1337–1345. [DOI] [PubMed] [Google Scholar]
- 22. Sachs RA, Daniel DM, Stone ML, Garfein RF. Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med. 1989;17:760–765. [DOI] [PubMed] [Google Scholar]
- 23. Schmitt LC, Paterno MV, Huang S. Validity and internal consistency of the International Knee Documentation Committee subjective knee evaluation form in children and adolescents. Am J Sports Med. 2010;38:2443–2447. [DOI] [PubMed] [Google Scholar]
- 24. Shelbourne KD, Gray T. Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med. 2009;37:471–480. [DOI] [PubMed] [Google Scholar]
- 25. Shelbourne KD, Klotz C. What I have learned about the ACL: utilizing a progressive rehabilitation scheme to achieve total knee symmetry after anterior cruciate ligament reconstruction. J Orthop Sci. 2006;11:318–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shelbourne KD, Urch SE, Gray T, Freeman H. Loss of normal knee motion after anterior cruciate ligament reconstruction is associated with radiographic arthritic changes after surgery. Am J Sports Med. 2012;40:108–113. [DOI] [PubMed] [Google Scholar]
- 27. Watkins MA, Riddle DL, Lamb RL, Personius WJ. Reliability of goniometric measurements and visual estimates of knee range of motion obtained in a clinical setting. Phys Ther. 1991;71:90–96. [DOI] [PubMed] [Google Scholar]


