Abstract
Background
Lack of insurance has been shown to lead to delays in seeking care as well as fewer preventive medicine visits and poorer overall health status.
Purpose
To investigate the effects of insurance status on the timing and treatment of patients with bucket-handle meniscus tears.
Study Design
Cohort study; Level of evidence, 3.
Methods
Charts from 2004 to 2013 were retrospectively reviewed for patients diagnosed with bucket-handle meniscus tears. Patients were divided into 2 groups: insured or underinsured. The insured group included patients with commercial insurance or Medicare. The underinsured group included patients with Medicaid or Charity Care. Time intervals were categorized as <6 weeks or ≥6 weeks.
Results
A total of 52 patients were included in this study: 15 (29%) insured and 37 (71%) underinsured. Underinsured patients experienced delays in initial presentation to an orthopaedic surgeon (P = .004), time from magnetic resonance imaging to surgery (P = .01), and time from injury to surgery (P = .007). Repair rates were 40% and 38% (P > .999) for the insured and underinsured, respectively. Repair rates for <6 weeks from injury to surgery were 75% for insured (P = .007) and 100% for underinsured patients (P = .001). Repair rates for ≥6 weeks from injury to surgery were 0% for insured and 30% for underinsured patients. Overall, patients with an injury-to-surgery time of <6 weeks had a significantly higher repair rate (87%) than those managed >6 weeks (19%) (P < .001).
Conclusion
Underinsured patients experience significant delays in time to presentation and overall time to surgery. However, the overall repair rate between the insured and underinsured is similar. Regardless of insurance status, patients undergoing arthroscopy within 6 weeks of injury have a significantly higher repair rate than those after 6 weeks.
Clinical Relevance
Patients undergoing arthroscopy within 6 weeks of injury have a significantly higher repair rate than those after 6 weeks.
Keywords: insurance, meniscus, bucket handle, timing
Displaced bucket-handle tears of the meniscus can lead to significant knee disability. The displaced fragment may block knee motion and, if left untreated, tears may extend, rendering an avulsed, irrepairable fragment, particularly if the tear extends into the avascular zone of the meniscus.9,13,17,18 The meniscus plays an important role in both load bearing and load distribution across the knee joint.10 Partial meniscectomy has been shown to lead to decreased contact area, increased contact pressure, and compressive strains across the joint contributing to early degenerative wear.4,5,7,11,26 Repair and stabilization of tears enhances outcomes and decreases the risk of radiographically detectable knee arthritis.1,10,24 Prompt management of these tears prior to the onset of degeneration appears to increase the likelihood of a successful repair.21
Lack of insurance has been shown to lead to delays in seeking care as well as fewer preventive medicine visits and poorer overall health status.8 Currently, a significant portion of the United States population remains either uninsured or underinsured. In 2008, The United States Census Bureau reported that 15.4% (46.3 million people) of the population was uninsured and 14.1% (42.6 million people) had Medicaid as their primary insurance. Several studies using both pediatric and adult patient populations have shown that for similar types of injuries, underinsured patients may have delayed management and may be treated in different locations, such as level I trauma centers, compared with insured patients.2,14,15,19,22,23,27
In our experience within a university hospital setting where a significant underinsured patient population exists, we have noticed that these patients often present in a delayed fashion after a knee injury, while their insured counterparts present more promptly. The purpose of our study was to investigate the correlation between health insurance status of an urban population within a university hospital setting and the timing and type of treatment for displaced bucket-handle meniscus tears. We had 2 hypotheses: (1) after a bucket-handle meniscus injury, underinsured patients would have a delayed presentation and (2) this delay would result in a greater likelihood of tear irrepairability at the time of arthroscopy.
Methods
Once institutional review board approval was obtained, charts dating to 2004 were retrospectively reviewed for all patients presenting to our orthopaedic surgery sports clinic and office who were diagnosed with a bucket-handle meniscus tear. All patients were treated by 1 of 2 sports fellowship–trained orthopaedic surgeons at our institution. Inclusion criteria included diagnosis of a bucket-handle meniscal tear based on magnetic resonance imaging (MRI) and confirmed with arthroscopy. Exclusion criteria included multiligamentous knee injuries (except for concomitant isolated anterior cruciate ligament [ACL] injuries) and severe arthritis (grade IV chondromalacia). Patients with concomitant ACL injuries were included in this study since these injuries commonly occur simultaneously. Patients were divided into 1 of 2 groups (insured and underinsured) based on their health insurance status. The insured group consisted of patients with either private/commercial insurance or Medicare. The underinsured group consisted of patients with Medicaid or Charity Care. Charity Care is free or reduced-charge care within the state of New Jersey provided for low-income patients who have no health care coverage.
In addition to demographic information, the dates of injury, initial visit to an orthopaedic surgeon, MRI, and surgery were recorded, and temporal relationships were analyzed. Specifically, we compared time from injury to initial presentation to an orthopaedic surgeon, time from presentation to surgery, time from injury to surgery, time from presentation to MRI, and time from MRI to surgery. The time intervals for all categories were categorized as <6 weeks or ≥6 weeks. The side of meniscal injury (medial or lateral) and whether the tear was repairable or nonrepairable intraoperatively was also recorded for each patient. Criteria for “repairability” included tears <3 mm from the periphery (up to the red-white zone), noncomplex tears (vertical), and reducible fragments that did not have an avulsed free end or significant degeneration that prevented tension-free reduction. Associated injuries were noted, including those to the ACL and posterior cruciate ligament (PCL) as well as patients with bicompartmental (medial and lateral) meniscal injuries within the same knee.
Statistical Analysis
Minitab 15.1.30.0 software was used to analyze repair rates and compare the insured and underinsured groups with respect to the temporal relationships. Both the chi-square test and 2-sample test for proportion were used for this analysis, and a significant difference was defined as P ≤ .05. The primary endpoint for all patients was the date of surgery, and primary outcome was either meniscal repair or meniscectomy.
Results
A total of 59 patients were included in this study. Nineteen (32%) patients were categorized as insured and 40 (68%) as uninsured. There were a total of 49 males and 10 females. In the insured group, there were 74% (n = 14) males and 26% (n = 5) females. In the uninsured group, there were 88% (n = 35) males and 12% (n = 5) females. The average age of the entire population was 27 years (range, 11-59 years). The insured group had an average age of 31 years (range, 13-59 years), and the uninsured group 26 years (range, 11-49 years). There were no significant differences between the demographics of the insured and uninsured groups (Table 1). The insured group had 14 medial and 5 lateral bucket-handle tears. The underinsured had 27 medial and 13 lateral bucket-handle tears. Table 2 provides a summary of the <6 week temporal relationships for the insured and underinsured study population from the following analyses.
TABLE 1.
Characteristics of the Insured and Underinsured Study Population
| Insured (n = 19) | Underinsured (n = 40) | P Value | |
|---|---|---|---|
| Age, y | .21 | ||
| <18 | 5 | 13 | |
| 19-36 | 8 | 22 | |
| ≥37 | 6 | 5 | |
| Sex, male:female, n | 14:5 | 35:5 | .19 |
| Bucket-handle tear, medial:lateral meniscus, n | 14:5 | 27:13 | .63 |
| Type of injury | .14 | ||
| Isolated | 10 | 13 | |
| Associated injury | 9 | 27 |
TABLE 2.
Summary of Temporal Relationships Between the Insured and Underinsured (in Percentages)a
| Insured (n = 19) | Underinsured (n = 40) | P Value | |
|---|---|---|---|
| Injury to presentation <6 wk | 79 | 30 | <.001 |
| Presentation to surgery <6 wk | 89 | 58 | .010 |
| Presentation to MRIb <6 wk | 100 | 75 | .100 |
| MRI to surgery <6 wk | 79 | 35 | .002 |
| Injury to surgery <6 wk | 68 | 20 | <.001 |
aMRI, magnetic resonance imaging.
bExcludes patients who had an MRI prior to initial presentation.
Injury to Initial Presentation to an Orthopaedic Surgeon
Fifteen of 19 (79%) insured patients presented <6 weeks compared with 12 of 40 (30%) underinsured patients (P < .001).
Presentation to Surgery
Seventeen of 19 (89%) insured patients had a <6 week presentation to surgery compared with 23 of 40 (58%) underinsured patients (P = .01).
Presentation to MRI
All insured patients had an MRI performed within 6 weeks of presentation to an orthopaedic surgeon; 10 of 19 (53%) insured patients had an MRI performed prior to presentation. Nineteen of 39 (49%) uninsured patients had an MRI performed prior to presentation to an orthopaedic surgeon. Of the patients with an MRI performed prior to presentation, 14 of 19 (74%) still had delays (>6 weeks from the time of injury) in presenting to our clinic. Of the remaining 20 patients without an MRI prior to presentation, 15 of 20 (75%) had an MRI performed within 6 weeks of presentation (P = .1) and 5 of 20 (25%) after 6 weeks. Twelve (60%) of these patients with an MRI performed after visiting our clinic had delays (>6 weeks from the time of injury) in presenting to our clinic. The date of MRI for 1 patient was unable to be obtained, and thus this patient was not included within the analysis for time from presentation to MRI.
MRI to Surgery
Fifteen of 19 (79%) insured patients had an MRI to surgery time of <6 weeks, compared with 14 of 40 (35%) underinsured (P = .002).
Injury to Surgery
Thirteen of 19 (68%) insured patients had a <6 week injury-to-surgery time, compared with 8 of 40 (20%) underinsured (P < .001).
Repairability
Seven of 19 (37%) insured patients had repairable meniscal tears compared with 16 of 40 (40%) underinsured patients (P > .999). Of the insured patients who had repairable tears, 7 of 7 (100%) had a <6 week injury-to-presentation time (mean, 10 days; range, 2-26 days), 7 of 7 (100%) had a <6 week presentation-to-surgery time (mean, 15 days; range, 5-26 days), and 7 of 7 (100%) had a <6 week injury-to-surgery time (mean, 25 days; range, 11-40 days). Of the insured patients with nonrepairable meniscal tears, the average time from injury to presentation was 63 days (range, 2-298 days), the average time from presentation to surgery was 32 days (range, 5-108 days), and the average time from injury to surgery was 93 days (range, 7-411 days). Eight of 12 (67%) nonrepairable meniscal tears had a <6 week injury-to-presentation time (mean, 12 days; range, 2-30 days), 10 of 12 (83%) had a <6 week presentation-to-surgery time (mean, 19 days; range, 5-41 days), and 5 of 12 (42%) had a <6 week injury-to-surgery time (mean, 21 days; range, 7-39 days).
Of the underinsured patients with repairable tears, 10 of 16 (63%) had a <6 week injury-to-presentation time (mean, 13 days; range, 3-29 days), 12 of 16 (63%) had a <6 week presentation-to-surgery time (mean, 13 days; range, 2-22 days), and 8 of 16 (50%) had a <6 week injury-to-surgery time (mean, 22 days; range, 5-42 days). Of the 24 underinsured patients with nonrepairable meniscal tears, the mean time from injury to presentation was 338 days (range, 28-1045 days), the mean time from presentation to surgery was 80 days (range, 6-554 days), and the mean time from injury to surgery was 393 days (range, 48-1246 days). Two of 24 (8%) nonrepairable meniscal tears had a <6 week injury-to-presentation time (mean, 32 days; range, 28-37 days), 11 of 24 (46%) had a <6 week presentation-to-surgery time (mean, 16 days; range, 6-36 days), and 0 of 24 (0%) had a <6 week injury-to-surgery time.
Medial Versus Lateral Meniscus
The insured group had 6 of 14 (43%) medial and 1 of 5 (20%) lateral bucket-handle meniscus tears repaired. The underinsured had 7 of 27 (26%) medial and 9 of 13 (69%) lateral bucket-handle meniscus tears repaired. Overall, the medial meniscus repair rate was 32%, and the lateral meniscus repair rate was 56% (P = .3).
Age and Sex Versus Repairability
There was no association between age and repairability rates when we divided the patients into 3 age groups: ≤18, 19-36, and ≥37 years (P = .21). There was also no significant association between sex and repairability, with a 43% repair rate for all males included in this study and a 30% repair rate for all females (P = .6).
Time From Injury to Surgery Versus Repairability
When all patients were included, the repair rates were 75% (15/20) in the <6 week group compared with 21% (8/39) for those undergoing surgery >6 weeks (P < .001).
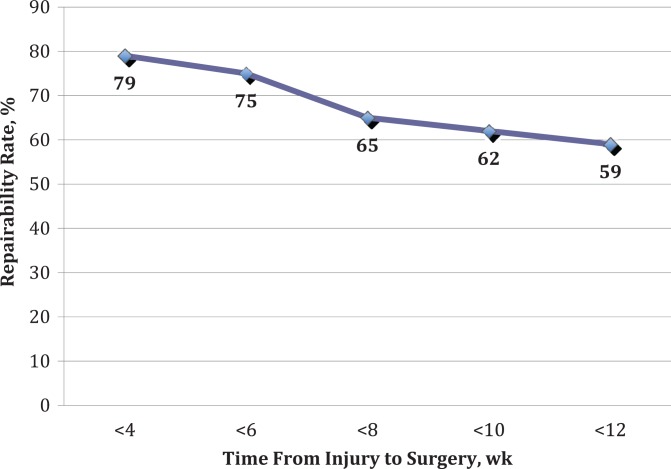
Repairability was also stratified by injury-to-surgery times of <4, <6, <8, <10, and <12 weeks. The repairability rates at these time points were 79%, 75%, 65%, 62%, and 59%, respectively (Figure 1).
Figure 1.
Rates of repairability for time from injury to surgery at <4, <6, <8, <10, and <12 weeks.
Associated Injuries
Insured Group
The insured group consisted of 14 medial meniscus and 5 lateral meniscus bucket-handle tears. Of the 14 medial meniscus bucket-handle tears, 5 (36%) were isolated, 1 (7%) had an associated non–bucket-handle lateral meniscus tear, 4 (29%) had complete ACL tears, 2 (14%) had a torn ACL graft, and 1 (7%) had a chronic ACL-deficient knee.
Of the 5 lateral meniscus bucket-handle tears, 3 (60%) were isolated, 1 (20%) had a grade 2 PCL injury treated nonoperatively, and 1 (20%) had a complete ACL tear with a non–bucket-handle medial meniscus tear. All ACL tears were reconstructed at the time of surgery.
Underinsured Group
The underinsured group consisted of 27 patients with medial meniscus bucket-handle tears and 13 patients with lateral meniscus bucket-handle tears. Of the 27 patients with medial meniscus bucket-handle tears, 3 (11%) were isolated, 1 (4%) had a non–bucket-handle lateral meniscus tear, 1 (4%) had a partial ACL tear, 15 (56%) had complete ACL tears, and 7 (26%) had complete ACL tears with a non–bucket-handle lateral meniscus tear.
Of the 13 patients with lateral meniscus bucket-handle tears, 10 (77%) presented as isolated injuries, 2 (15%) had complete ACL tears, and 1 (8%) had a complete ACL tear with a non–bucket-handle medial meniscus tear.
Discussion
Bucket-handle meniscus tears result in significant patient disability, and prompt management is ideal. In our study, we found that the insurance status of patients influenced several of the time points from injury that we measured, but did not ultimately change the result of whether a bucket-handle tear was repairable. We found that underinsured patients experienced significant delays in initial presentation to an orthopaedic surgeon, time from initial presentation to surgery, time from MRI to surgery, and overall time from injury to surgery.
Prior studies have also documented disparities between the management of insured and underinsured patients within the health care system. Underinsured patients, for example, are often referred to large hospitals for treatment, even if that treatment could be procured in an ambulatory facility. Wolinsky et al27 suggested that nonmedical reasons play a role in determining where ambulatory patients requiring surgery for definitive treatment are treated. They found that ambulatory patients who could have been treated at an ambulatory care facility but who ultimately received definitive care at a level I trauma center were significantly more likely to be underinsured. Archdeacon et al2 reported that uninsured patients were more likely than insured patients to be transferred to a level I trauma center for definitive care of femoral fractures. In our study, 49% of underinsured patients had already undergone an MRI prior to presentation to our clinic. Despite care already having been initiated, because of the additional referral step to our hospital, this group still had significant delays in presentation and time to surgery.
A study by Sabharwal et al19 performed at our institution found that 52% of children with private insurance received care, including evaluation with cast application, within 24 hours compared with 22% of those who were underinsured. They also found that the underinsured were more likely to have visited another health facility besides the initial emergency department before presenting to a university hospital emergency department. Several other studies have confirmed a delay in treatment or unmet needs of pediatric patients with orthopaedic injuries covered by Medicaid and other forms of public health insurance.6,14,15,22,23
In the adult arthroscopic literature, a recent study by Gundle et al12 looking at over 1000 patients found similar rates of arthroscopy performed within 6 months from the initial office visit between insured and uninsured groups. However, subgroup analysis revealed that those with private insurance had a higher rate of surgery than those without insurance. This study, however, did not examine whether a repair or meniscectomy was performed at the time of arthroscopy and its relation to type of insurance status or chronicity of injury.12
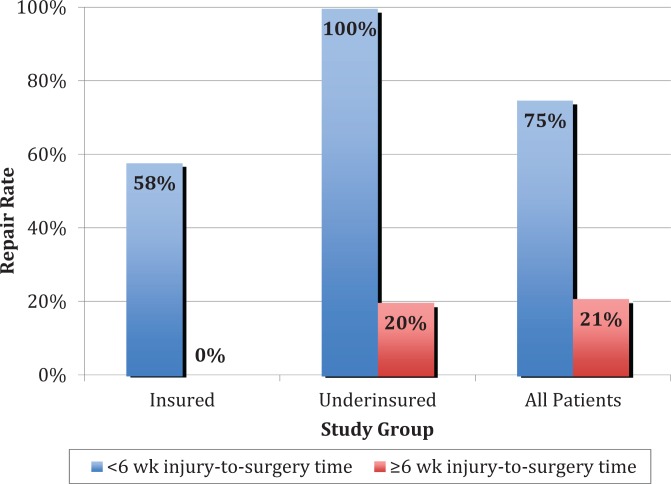
We hypothesized that the delays experienced by our underinsured patients would result in a greater rate of irrepairable tears at the time of surgery. This was not borne out by our results, which showed overall similar rates of repairability between insured (37%) and uninsured (40%) patients. The discrepancy may lie in the repair rates of those patients who were managed within 6 weeks. While insured patients with <6 week injury-to-presentation and injury-to-surgery times had repair rates of 47% and 58%, respectively, underinsured patients with <6 week times had higher repair rates of 83% and 100%. Additionally, while no insured patients with ≥6 week injury-to-presentation or injury-to-surgery times had repairable menisci, underinsured patients with ≥6 week times had repair rates of 21% and 25%, respectively. The larger percentage of underinsured patients presenting chronically and still amenable to repair may be due to the disparate cohort sizes of insured and underinsured patients within our study. Furthermore, a larger percentage of underinsured patients had associated ACL tears and were <36 years old. Concomitant ACL reconstruction and young age are relative indications for meniscus repair.16,25 A study with a larger patient population where these subgroup demographic differences are eliminated may potentially be able to more clearly correlate delays with a decreased rate of repair.
Our study shows that tears managed within 6 weeks of injury have a high repair rate of 75% (Figure 2). To our knowledge, there are no studies that correlate time from injury to surgery with repairability of bucket-handle tears. Previous studies have shown that prompt management of bucket-handle tears prior to the onset of degeneration may lead to more successful outcomes. Shelbourne and Carr21 found degenerative meniscal tears to have a higher retear rate after repair, with 80% of their unsuccessful repairs occurring from degenerative bucket-handle tears. They found that although degenerative tears have the potential to heal, repair appears to provide no advantage over partial meniscectomy, with subjective scores lower than patients undergoing meniscectomy at a mean 7.8 years after surgery in the meniscectomy group and 8.9 years after surgery in the repair group. Contrastingly, repair of nondegenerative bucket-handle tears provided subjective results equal to patients with intact menisci.
Figure 2.
Repair rates for insured, underinsured, and all patients combined with respect to <6 weeks and ≥6 weeks injury-to-surgery time intervals.
Scott et al20 found no significant difference in healing rates of menisci repaired within 3 weeks of injury versus after 3 weeks. However, they included all meniscal tear types and did not isolate bucket-handle repairs with respect to the time intervals evaluated. They found no significant difference in healing rates between the displaced bucket-handle repairs compared with the remainder of menisci repaired. In contrast, another study found bucket-handle tears to demonstrate poor healing potential.3 This study, however, failed to mention the timing from injury to surgery.
Our study shows that the rate of repairability of a bucket-handle meniscus tear goes down with time, as expected. Within 6 weeks, the feasibility of reducing and repairing the meniscus is quite high. After the 12-week postinjury mark, however, repairability rates appear to drop to around 59%. Although repairability is a subjective decision made by the surgeon at the time of arthroscopy, we feel that the criteria we used are commonly accepted and easily recognized. The change in repairability rates with time may reflect the natural history of microscopic and macroscopic changes occurring in the bucket-handle fragment while it remains displaced.
Our study was limited by its retrospective nature and a possible selection bias inherent to data collection at a single academic institution. We felt, however, that limiting the groups to a single hospital would allow us to compare insured and underinsured patients while mitigating the effect that management at a heterogeneous group of centers might entail. The overall sample size may have been too low to draw significance in some of our analyses. Nevertheless, we were able to find significant differences in many of our outcome measures. A power analysis showed that we would need over 2000 patients to draw significant conclusions regarding repairability rates with respect to insurance status and time to surgery. Because bucket-handle tears do not occur as frequently as other types of meniscus tears, collecting a large number of patients is logistically more challenging. Finally, we did not follow clinical outcomes in our patients. Although, ultimately, clinical outcomes validate or refute the judgment made at the time of repair, the goals of this study were not to evaluate patient outcomes. Instead, we sought to identify a possible discrepancy between 2 subgroups in the management of this time-sensitive orthopaedic injury and to evaluate the first step in its surgical management, namely the reducibility and repairability of the bucket-handle fragment. In other words, did the time from injury to surgery affect the ability of the bucket-handle fragment to be reduced and repaired in the first place? We continue to collect data on these patients. Future studies will attempt to correlate clinical outcomes with the initial surgical management.
Conclusion
In the management of displaced bucket-handle meniscus tears, underinsured patients experience delays in presentation and overall time to surgery when compared with insured patients. Regardless of insurance status, we found that patients undergoing arthroscopic management for a bucket-handle meniscus tear within 6 weeks of injury have a significantly greater repair rate than those who have surgery performed in a delayed fashion and that the repair rate decreases as time elapses. Our study supports prompt management of these injuries, ideally within 6 weeks, to maximize the chances of meniscus reduction and repair. Future studies are needed to bear out the longer term clinical ramifications of successfully reduced repairs.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Aglietti P, Zaccherotti G, De Biase P, Taddei I. A comparison between medial meniscus repair, partial meniscectomy, and normal meniscus in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1994;(307):165–173. [PubMed] [Google Scholar]
- 2. Archdeacon MT, Simon PM, Wyrick JD. The influence of insurance status on the transfer of femoral fracture patients to a level-I trauma center. J Bone Joint Surg Am. 2007;89:2625–2631. [DOI] [PubMed] [Google Scholar]
- 3. Asahina S, Muneta T, Yamamoto H. Arthroscopic meniscal repair in conjunction with anterior cruciate ligament reconstruction: factors affecting the healing rate. Arthroscopy. 1996;12:541–545. [DOI] [PubMed] [Google Scholar]
- 4. Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14:270–275. [DOI] [PubMed] [Google Scholar]
- 5. Bedi A, Kelly NH, Baad M, et al. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am. 2010;92:1398–1408. [DOI] [PubMed] [Google Scholar]
- 6. Berman S, Dolins J, Tang SF, Yudkowsky B. Factors that influence the willingness of private primary care pediatricians to accept more Medicaid patients. Pediatrics. 2002;110:239–248. [DOI] [PubMed] [Google Scholar]
- 7. Bourne RB, Finlay JB, Papadopoulos P, Andraea P. The effect of medial meniscectomy on strain distribution in the proximal part of the tibia. J Bone Joint Surg Am. 1984;66:1431–1437. [PubMed] [Google Scholar]
- 8. Chou CF, Johnson PJ, Ward A, Blewett LA. Health care coverage and the health care industry. Am J Public Health. 2009;99:2282–2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cooper DE, Arnoczky SP, Warren RF. Meniscal repair. Clin Sports Med. 1991;10:529–548. [PubMed] [Google Scholar]
- 10. Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30B:664–670. [PubMed] [Google Scholar]
- 11. Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthrotic knee joints. Acta Orthop Scand. 1980;51:871–879. [DOI] [PubMed] [Google Scholar]
- 12. Gundle KR, McGlaston TJ, Ramappa AJ. Effect of insurance status on the rate of surgery following a meniscal tear. J Bone Joint Surg Am. 2010;92:2452–2456. [DOI] [PubMed] [Google Scholar]
- 13. Henning CE, Lynch MA, Clark JR. Vascularity for healing of meniscus repairs. Arthroscopy. 1987;3:13–18. [DOI] [PubMed] [Google Scholar]
- 14. Iobst C, King W, Baitner A, Tidwell M, Swirsky S, Skaggs DL. Access to care for children with fractures. J Pediatr Orthop. 2010;30:244–247. [DOI] [PubMed] [Google Scholar]
- 15. Newacheck PW, Stoddard JJ, Hughes DC, Pearl M. Health insurance and access to primary care for children. N Engl J Med. 1998;338:513–519. [DOI] [PubMed] [Google Scholar]
- 16. O’Shea JJ, Shelbourne KD. Repair of locked bucket-handle meniscal tears in knees with chronic anterior cruciate ligament deficiency. Am J Sports Med. 2003;31:216–220. [DOI] [PubMed] [Google Scholar]
- 17. Pujol N, Panarella L, Selmi TA, Neyret P, Fithian D, Beaufils P. Meniscal healing after meniscal repair: a CT arthrography assessment. Am J Sports Med. 2008;36:1489–1495. [DOI] [PubMed] [Google Scholar]
- 18. Rosenberg TD, Scott SM, Coward DB, et al. Arthroscopic meniscal repair evaluated with repeat arthroscopy. Arthroscopy. 1986;2:14–20. [DOI] [PubMed] [Google Scholar]
- 19. Sabharwal S, Zhao C, McClemens E, Kaufmann A. Pediatric orthopaedic patients presenting to a university emergency department after visiting another emergency department: demographics and health insurance status. J Pediatr Orthop. 2007;27:690–694. [DOI] [PubMed] [Google Scholar]
- 20. Scott GA, Jolly BL, Henning CE. Combined posterior incision and arthroscopic intra-articular repair of the meniscus. An examination of factors affecting healing. J Bone Joint Surg Am. 1986;68:847–861. [PubMed] [Google Scholar]
- 21. Shelbourne KD, Carr DR. Meniscal repair compared with meniscectomy for bucket-handle medial meniscal tears in anterior cruciate ligament-reconstructed knees. Am J Sports Med. 2003;31:718–723. [DOI] [PubMed] [Google Scholar]
- 22. Skaggs DL, Clemens SM, Vitale MG, Femino JD, Kay RM. Access to orthopedic care for children with medicaid versus private insurance in California. Pediatrics. 2001;107:1405–1408. [DOI] [PubMed] [Google Scholar]
- 23. Skaggs DL, Lehmann CL, Rice C, et al. Access to orthopaedic care for children with Medicaid versus private insurance: results of a national survey. J Pediatr Orthop. 2006;26:400–404. [DOI] [PubMed] [Google Scholar]
- 24. Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jager A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med. 2010;38:1542–1548. [DOI] [PubMed] [Google Scholar]
- 25. Toman CV, Dunn WR, Spindler KP, et al. Success of meniscal repair at anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37:1111–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975;(109):184–192. [DOI] [PubMed] [Google Scholar]
- 27. Wolinsky P, Kim S, Quackenbush M. Does insurance status affect continuity of care for ambulatory patients with operative fractures? J Bone Joint Surg Am. 2011;93:680–685. [DOI] [PubMed] [Google Scholar]