Abstract
Background:
Long-term results after anterior cruciate ligament (ACL) reconstruction are being reported with greater frequency, allowing a detailed analysis of long-term patient-reported outcomes and predictors.
Purpose:
To summarize expected patient-reported outcomes at a minimum 10 years following ACL reconstruction and to explore patient and surgical factors that affect these results.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
Prospective studies detailing patient-reported outcomes with a minimum follow-up of 10 years were identified. Average scores for each outcome measure were calculated. Factors identified in each paper as predictors of patient-reported outcomes were identified and described.
Results:
Thirteen studies met inclusion and exclusion criteria. Lysholm scores were reported in 317 of 406 patients (78.1%) in 6 studies, with a mean score of 91.7 ± 11.2. Subjective International Knee Documentation Committee scores were reported in 1726 of 2611 patients (66.1%) in 5 studies, with a mean score of 84.2 ± 15.5. Cincinnati knee scores were reported in 1323 of 1801 patients (73.5%) in 3 studies, with a mean score of 87.4 ± 14.4. Tegner activity scores were reported in 728 of 914 patients (79.6%) in 8 studies, with a mean score of 5.1. There was mixed evidence that meniscectomy and articular cartilage damage were associated with poorer patient-reported outcomes. Patient sex and graft choice did not affect patient-reported outcomes.
Conclusion:
Patient-reported outcomes are generally good at a minimum of 10 tears following ACL reconstruction. Further large prospective studies with regression modeling and consistent outcome reporting will clarify predictors of outcomes.
Keywords: anterior cruciate ligament reconstruction, long-term outcomes
Injury to the anterior cruciate ligament (ACL) is increasingly common, and ACL reconstruction is a frequently performed knee procedure. Current techniques typically result in a stable knee and successful restoration of function in the short term; however, long-term outcomes are more variable.
While recent systematic reviews have evaluated the long-term risk of ACL graft tear and contralateral ACL injury,5,24 as well as the risk of osteoarthritis following ACL injury and surgery,18 there has been less discussion of long-term patient-reported outcomes following ACL reconstruction. Patient-reported outcomes play an increasingly large role in the assessment of outcomes after treatment and are a recommended component of all clinical trials.3
Long-term patient-reported outcomes data following ACL reconstruction are crucial to share with patients who undergo ACL reconstruction as they provide outcome information from a patient perspective. The aim of this systematic review was to determine expected patient-reported outcomes with prospectively collected data at a minimum 10 years following ACL reconstruction and explore patient and surgical factors that affect these results.
Materials and Methods
Literature Review
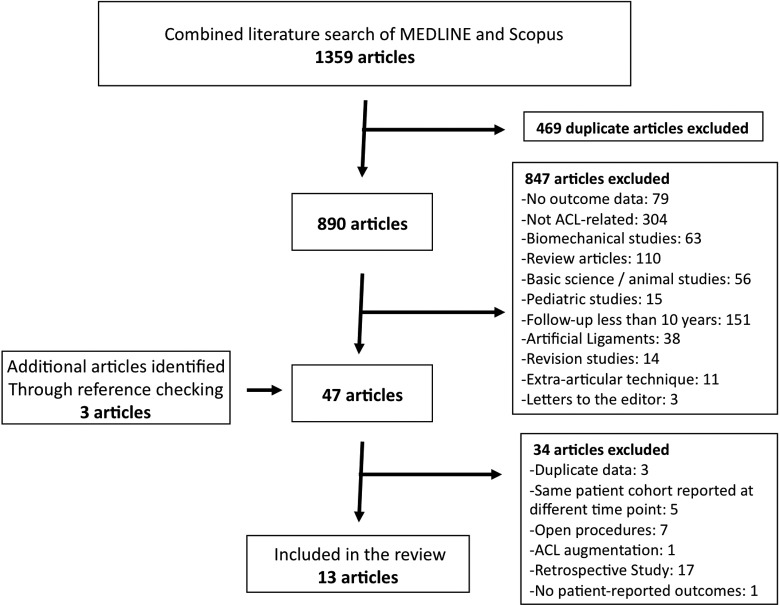
A search of MEDLINE and Scopus was performed to identify all publications from January 1, 1966 through June 6, 2014 reporting long-term outcomes of ACL reconstruction. Searches including the terms ACL or anterior cruciate, reconstruction, and long-term yielded 514 articles in MEDLINE and 845 articles in Scopus. After elimination of 469 duplicate citations, the titles and abstracts of 890 articles were reviewed. The 860 studies that failed to meet inclusion and exclusion criteria, outlined in Table 1, were eliminated. Review of the references of the remaining 44 studies yielded 3 other potential studies for inclusion. Full-text review of the 47 studies was undertaken, and 16 studies were removed that were duplicate publications (n = 3), shorter follow-up of patients reported elsewhere with longer follow-up (n = 5), ACL repair or augmentation procedures rather that reconstruction (n = 1), or open procedures (n = 7). Seventeen of the remaining 31 studies were excluded due to retrospective data collection, and 1 was excluded because it did not report patient-reported outcome data. The remaining 13 studies make up the data set for this review.‖ The literature search is summarized in Figure 1.
TABLE 1.
Inclusion and Exclusion Criteriaa
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Published prospective series describing outcomes of primary ACL reconstruction 10-year minimum follow-up Reconstruction with patellar tendon or hamstring tendon autograft Utilization of all-arthroscopic, arthroscopic-assisted, or mini-arthrotomy technique Reconstruction with an intra-articular graft, with or without extra-articular augmentation Provide data on patient-reported outcomes | Retrospective study design <10-year follow-up Utilization of graft tissue other than patellar tendon or hamstring tendon Open ACL reconstruction Reconstruction techniques without an intra-articular graft Multiligament knee injury other than low-grade MCL injuries Animal studies In vitro studies Reviews without original data Use of artificial ligaments Reconstruction techniques Revision ACL reconstructions Pediatric ACL reconstruction |
aACL, anterior cruciate ligament; MCL, medial collateral ligament.
Figure 1.
Search strategy used to identify papers for inclusion in the review.
Data Extraction
Extracted data included study characteristics, patient demographics, associated injuries, surgical technique, graft choice, details of rehabilitation, length of follow-up, patient-reported outcomes data, and factors evaluated by the authors as possibly affecting patient-reported outcomes. Data were extracted by 2 authors independently, and discrepancies were resolved by consensus.8,23
Statistics
Collected data were tabulated and summarized. Mean scores for patient-reported outcome measures were calculated as a weighted average of the mean scores from each study, weighted by the number of patients in each study. The standard deviation of the resulting overall mean was calculated based on the between-studies error as well as the precision (inverse variance) of the individual study means. When no measure of dispersion was reported, the mean standard deviation of the other studies reporting this outcome measure was utilized for this calculation.
Results
The 13 studies identified in the literature review include 4 randomized controlled trials (3 comparing patellar tendon with hamstring grafts1,11,21 and 1 evaluating the effect of bracing during rehabilitation17), 6 prospective cohort studies,9,10,12,19,22,25 and 3 case series with prospective data collection.2,6,13 Study design was reported as was initially assigned at the time of publication. All 13 studies include only prospectively collected data.
There were 3486 patients included in the 13 studies, with a mean age at the time of ACL reconstruction of 26.9 years. Mean patient age for the individual studies ranged from 23 to 38 years, and 66.8% of patients were male. The time from ACL injury to reconstruction varied greatly among the studies and ranged from all acute injuries to a mean of 5 years between injury and reconstruction. Exclusion criteria among the studies varied as well, but all excluded knees with multiple complete ligament injuries. Table 2 summarizes study demographic information.
TABLE 2.
Study Demographicsa
| Authors (Year) | Initial Cohort, n | Age, y, mean | Male Sex, % | Chronicity | Other Selection Criteria |
|---|---|---|---|---|---|
| Barenius et al1 (2014) | 164 | 25.7 | 57.1 | Median, 8 mo | Multiple ligament injuries excluded |
| Bourke et al2 (2012) | 755 | 29 | 64.0 | 38% were >12 wk | Prior contralateral ACL tears, those seeking injury compensation, and multiple ligament injuries excluded |
| Felmet6 (2010) | 189 | 38 | 61.4 | All but 4 were <12 mo | Those with subsequent major injury (tibial plateau fracture and multiple ligament injuries excluded) |
| Hanypsiak et al9 (2008) | 54 | 26.3 | 70.5 | All <3 mo | Chronic injuries (>3 mo) and multiple ligament injuries excluded |
| Hart et al10 (2005) | 50 | 29.1 | 67.7 | NR | Multiple ligament injuries and patients with chondral injuries excluded |
| Holm et al11 (2010) | 37 | 27 | 64.3 | Mean, 3.3 y | Multiple ligament injuries excluded |
| Janssen et al12 (2012) | 100 | 31.2 | 66.0 | Mean, 5 y | Multiple ligament injuries excluded |
| Lebel et al13 (2008) | 154 | 28.8 | 66.0 | Mean, 22 mo; 37 were >1 year | Multiple ligament injuries excluded |
| Moller et al17 (2009) | 62 | 27.5 | 48.4 | Mean, 6 mo | Multiple ligament injuries in either knee excluded |
| Oiestad et al19 (2010) | 219 | 27.1 | 57.0 | Mean, 28 mo | Multiple ligament injuries and other major trauma excluded |
| Sajovic et al21 (2011) | 64 | 26 | 57.8 | Mean, 24 mo; 85% were >12 wk | Patients with pre-existing osteoarthritis, prior meniscectomy, or multiple ligament injuries excluded |
| Shelbourne and Gray22 (2009) | 1545 | 22.6 | 72.0 | Mean, 2 mo | Prior contralateral ACL tears and multiple ligament injuries excluded |
| Wu et al25 (2002) | 103 | 24 | 57.0 | 73% were >4 mo | Multiple ligament injuries excluded |
aACL, anterior cruciate ligament; NR, not reported.
All reconstructions were performed via all arthroscopic, arthroscopic-assisted, or mini-arthrotomy techniques. Different femoral tunnel drilling techniques and fixation methods were used in the studies. Table 3 summarizes surgical technique. Details of the rehabilitation protocol were reported in 10 of the 13 studies. The majority allowed immediate full weightbearing, and only 4 studies utilized a postoperative brace, for time periods ranging from 3 to 8 weeks. Table 4 details the rehabilitation protocols for each study.
TABLE 3.
Surgical Techniquea
| Authors | Surgical Technique | Femoral Drilling Technique | Graft | Femoral Fixation | Tibial Fixation |
|---|---|---|---|---|---|
| Barenius et al1 | Arthroscopic | NR | BTB or hamstring autograft | Endobutton | Metal interference screw |
| Bourke et al2 | Arthroscopic | AM portal | BTB or hamstring autograft | Metal interference screw | Metal interference screw |
| Felmet6 | Arthroscopic | AM portal | BTB autograft | Press fit | Press fit |
| Hanypsiak et al9 | Arthroscopic-assisted | Outside-in | BTB or hamstring autograft | Metal interference screw | Metal interference screw |
| Hart et al10 | Arthroscopic | NR | BTB autograft | NR | NR |
| Holm et al11 | Arthroscopic | Transtibial | Hamstring autograft | Endobutton | Interference screw with staple backup |
| Janssen et al12 | Arthroscopic | Transtibial | Hamstring autograft | Bone mulch screw | Washerlock |
| Lebel et al13 | Arthroscopic | AM portal | BTB autograft | Metal interference screw | Metal interference screw |
| Moller et al17 | Arthroscopic/arthroscopic-assisted | Transtibial/outside-in | BTB autograft | Metal interference screw | Metal interference screw |
| Oiestad et al19 | Arthroscopic/mini-open | Transtibial/outside-in | BTB autograft | Metal interference screw | Metal interference screw |
| Sajovic et al21 | Arthroscopic | AM portal | BTB or hamstring autograft | Metal interference screw | Bioabsorbable interference screw |
| Shelbourne and Gray22 | Mini-open | Outside-in | BTB autograft | Button fixation | Button fixation |
| Wu et al25 | Arthroscopic | NR | BTB autograft | Metal interference screw | Metal interference screw |
aAM, anteromedial; BTB, bone-tendon-bone; NR, not reported.
TABLE 4.
Rehabilitationa
| Authors | CPM | Time to Partial Weightbearing | Time to Full Weightbearing | Brace Use | Time to Full Activity |
|---|---|---|---|---|---|
| Barenius et al1 | NR | Immediate | Immediate | Yes, 3 wk | 6 mo |
| Bourke et al2 | No | Immediate | Immediate | No | 6-9 mo |
| Felmet6 | No | Immediate | 1 wk | Yes, 7-8 wk | NR |
| Hanypsiak et al9 | NR | NR | NR | NR | NR |
| Hart et al10 | NR | NR | NR | NR | NR |
| Holm et al11 | No | Immediate | Immediate | No | 6 mo |
| Janssen et al12 | No | Immediate | Immediate | No | 6 mo |
| Lebel et al13 | NR | Immediate | Immediate | NR | NR |
| Moller et al17 | NR | NR | NR | NR | NR |
| Oiestad et al19 | No | Immediate | Immediate | No | 6 mo |
| Sajovic et al21 | No | Immediate | Immediate | Yes, 3 wk | 6 mo |
| Shelbourne and Gray22 | No | Immediate | Immediate | No | 4-6 mo |
| Wu et al25 | Yes | Immediate | Immediate | Yes, 4 wk | 6 mo |
aCPM, continuous passive motion device; NR, not reported.
Follow-up was available for 2636 of the 3486 patients (75.6%), with individual study follow-up ranging from 61.1% to 90.3%. Mean follow-up in all studies was at least 10 years (range, 10.3-16.9 years in the individual studies). Lysholm scores at final follow-up were reported in 317 of 406 patients (78.1%) in 6 studies.10–12,17,21,25 The mean overall Lysholm score was 91.7 ± 11.2. Subjective International Knee Documentation Committee (IKDC) scores at final follow-up were reported in 1726 of 2611 patients (66.1%) in 5 studies.2,9,13,22,25 The mean subjective IKDC score was 84.2 ± 15.5. Cincinnati knee scores at final follow-up were reported in 1323 of 1801 patients (73.5%) in 3 studies.11,19,22 The mean overall Cincinnati knee score was 87.4 ± 14.4. Knee injury and Osteoarthritis Outcome Score (KOOS) was reported in 190 of 226 patients (84.1%) in 2 studies,1,17 and is reported in Table 5. Tegner activity scores were reported in 728 of 914 patients (79.6%) in 8 studies.1,6,10–12,17,19,25 The mean overall Tegner score was 5.1.
TABLE 5.
Patient-Reported Outcomesa
| Authors | Patients Followed Up, n/Total (%) | Years to Follow-up, mean | Age at ACLR, y, mean | Outcomes Scoreb | ||||
|---|---|---|---|---|---|---|---|---|
| Lysholm | IKDC Subjective | Cincinnati | KOOS | Tegner | ||||
| Barenius et al1 | 134/164 (81.7) | 14 | 25.7 | Pain: 84 ± 17 Symptoms 76 ± 19 ADLs: 89 ± 17 Sport/Rec: 64 ± 28 Quality of Life: 62 ± 25 | 6 | |||
| Bourke et al2 | 598/755 (79.2)c | 16.9 | 29 | 85 ± 16 | ||||
| Felmet6 | 148/189 (78.3)c | 10.3 | 38 | A or B in 94.6% | 5 | |||
| Hanypsiak et al9 | 44/54 (81.5) | 12 | 26.3 | 70.3 ± 11.7 | ||||
| Hart et al10 | 31/40 (77.5)c | 10 | 29.1 | 93 | 6 | |||
| Holm et al11 | 29/37 (78.4) | 10.7 | 27 | 86.1 ± 15 | 87.8 ± 12.3 | 4.8 | ||
| Janssen et al12 | 86/100 (86.0) | 10 | 31.2 | 95 ± 8.2 | 6 | |||
| Lebel et al13 | 101/154 (66.6) | 11.6 | 28.8 | 90.5 ± 8.8 | ||||
| Moller et al17 | 56/62 (90.2) | 11.5 | 27.5 | 90 | Pain: 90 Symptoms: 86 ADLs: 94 Sport/Rec: 71 Quality of Life: 81 | 4 | ||
| Oiestad et al19 | 181/219 (82.6) | 12.4 | 27.1 | 83 ± 16 | 4 | |||
| Sajovic et al21 | 52/64 (81.2)c | 11 | 26 | 95 | ||||
| Shelbourne and Gray22 | 1113/1545 (72.0)c | 14 | 22.6 | 83.6 ± 15.5d | 88.1 ± 14.0 | |||
| Wu et al25 | 63/103 (61.2) | 10.3 | 24.0 | 88 ± 10 | 80 ± 18 | 6.4 | ||
| All | 91.7 ± 11.2 | 84.2 ± 15.5 | 87.4 ± 14.4 | Pain: 85.8 Symptoms: 78.9 ADLs: 90.5 Sport/Rec: 66.1 Quality of Life: 67.6 | 5.1 | |||
aACLR, anterior cruciate ligament reconstruction; ADLs, activities of daily living; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; Sport/Rec, sports and recreation.
bValues are reported as means or means ± SDs.
cPatients with graft failure or contralateral ACL tear excluded.
dn = 920 (59.5%) for the subjective IKDC score.
Meniscus and Articular Cartilage Status
The influence of meniscus status at the time of ACL reconstruction on patient-reported outcomes was analyzed in 4 studies.10,13,22,25 Hart et al10 noted no significant difference in Lysholm scores between patients with intact menisci (Lysholm, 96) and those who underwent partial meniscectomy (Lysholm, 95). Similarly, Lebel et al13 noted no significant differences in IKDC subjective scores based on whether partial meniscectomy was performed, although specific numbers were not reported. In contrast, Wu et al25 noted significantly lower Lysholm (3 ± 10 vs 94 ± 8) and IKDC subjective scores (76 ± 19 vs 80 ± 18) when partial or total meniscectomy was performed compared with patients with intact menisci. In multiple linear regression models, Shelbourne and Gray22 demonstrated that the performance of partial or total medial (P = .0071) or lateral (P = .022) meniscectomy predicted lower Cincinnati knee scores, while partial or total lateral meniscectomy predicted subjective IKDC scores (P = .030). Although statistically significant, the differences in Cincinnati score associated with partial or total medial (2.7 points) or lateral (3.3 points) meniscectomy did not reach clinical significance, nor did the difference in subjective IKDC score associated with partial or total lateral meniscectomy (4.3 points).
The influence of articular cartilage damage on outcomes was assessed in 3 studies.9,13,22 Hanypsiak et al9 reported no significant differences in subjective IKDC scores between patients with intact articular cartilage (IKDC, 69.0 ± 11.9) and those with articular cartilage lesions (IKDC, 72.8 ± 12.0).9 Similarly, Lebel et al13 noted no significant differences in IKDC subjective scores based on articular cartilage status, although specific numbers were not reported. In multiple linear regression models, Shelbourne and Gray22 demonstrated that articular cartilage injury was a significant predictor of lower Cincinnati (P = .039) and subjective IKDC scores (P = .002). Although statistically significant, the differences in Cincinnati score (3.1 points) and subjective IKDC score (6.5 points) associated with articular cartilage injury did not reach clinical significance.
Oiestad et al19 grouped patients with either meniscal or articular cartilage injury into a “combined injury group.” Comparison of this group with an isolated ACL injury group demonstrated similar Cincinnati knee scores (combined, 82; isolated, 85; P = .17).19
Patient Sex
The influence of patient sex on outcomes scores was analyzed in 3 studies.1,2,13 Barenius et al1 noted no significant differences in KOOS based on patient sex, while Bourke et al2 and Lebel et al13 noted no significant differences in subjective IKDC score based on patient sex.
Graft Choice
Four studies evaluated the impact of autograft choice (hamstring vs patellar tendon) on patient-reported outcomes following ACL reconstruction.1,2,11,21 In a randomized controlled trial, Barenius et al1 noted no significant difference in any KOOS subscales (all P > .05) based on graft choice. In a similar randomized trial, Holm et al11 noted no differences in Cincinnati (P = .20) or Lysholm scores (P = .64) based on graft type. Also in a randomized controlled trial, Sajovic et al21 noted no difference in Lysholm score (P = .31) based on graft choice. Finally, in a prospective cohort study, Bourke et al2 noted no significant differences in subjective IKDC score based on graft type.
Other Factors
One study by Lebel et al13 assessed the impact of body mass index (BMI) on patient-reported outcome scores, and no significant correlation was noted with subjective IKDC scores. Shelbourne and Gray22 noted that patients who failed to regain full extension or flexion relative to the contralateral side demonstrated poorer Cincinnati and subjective IKDC scores.
Discussion
This review demonstrates that generally good patient-reported outcome scores are noted at minimum 10 years following ACL reconstruction. Variable outcomes were noted across studies, likely representing differences in the individual patient populations. The lowest scores were noted in the KOOS sport/recreation function and knee-related quality of life subscales. These values point out the room for further improvement in the management of ACL injuries, and also likely represent good outcomes tools to assess the results of future reconstructions.
The influence of meniscal resection on outcomes scores was mixed. The 2 studies that included total and partial meniscectomy noted an effect,22,25 while those that assessed only partial meniscectomy noted no influence of partial meniscectomy on outcome scores.10,13 It should be noted that although these authors did not demonstrate differences in outcome scores, they did note increased radiographic evidence of osteoarthritis in the partial meniscectomy group. Similarly, the 1 study that evaluated the effect of BMI on patient-reported outcomes noted no correlation, but they did demonstrate a correlation between increased BMI and increased risk of radiographic evidence of osteoarthritis.13 Such findings are well known to be associated with partial meniscectomy, even at short time points,15 and likely precede the development of symptomatic osteoarthritis with lower patient-reported outcome scores.
No correlation between patient sex or graft choice and patient-reported outcomes was noted in this review. Ryan et al,20 in a 2014 systematic review of ACL reconstruction studies with shorter follow-up, also noted no clinically significant differences in patient-reported outcome score based on sex. Numerous systematic reviews have failed to demonstrate an effect of graft choice on patient-reported outcome scores following ACL reconstruction,7,14,16 which this study confirms at longer follow-up.
There are several limitations in the review. Primarily, there were a large variety of potential predictors of outcomes assessed in the studies along with a variety of outcomes measures to assess the results. This variability precluded the use of meta-analysis techniques that could combine data from multiple studies to more completely evaluate the potential effects of patient and surgical variables on outcome. Even variables with significant evidence in the literature to demonstrate their importance such as meniscus and articular cartilage status were inconsistently reported in the included studies with regard to their influence on outcomes.
Additional variability was created by the practice that was utilized in a number of the included studies of reporting patient-reported outcomes only for patients in whom no ACL graft failure or contralateral knee injury occurred. Reporting data in this manner gives a good assessment of the results in this limited portion of the population, but may result in overestimation of the outcome scores that can be expected for all patients who undergo the procedure. Furthermore, while the overall follow-up of 76.6% is reasonable given the minimum follow-up of 10 years, this follow-up does fall short of the desired 80%. Some individual studies had follow-up as low as 60% to 70%, potentially introducing bias in these studies.13,25 Finally, very few papers performed a regression analysis when assessing the impact of various patient and surgical factors on patient-reported outcome scores. Therefore, the majority of studies may be at risk for confounding, and it is not completely clear which factors are independent predictors of outcome. It has been calculated that a prospective longitudinal cohort of at least 2000 patients with 80% follow-up would be required to model interactions between meniscus and articular cartilage pathology while controlling for other variables that may influence outcomes following ACL reconstruction.4
Conclusion
Patient-reported outcomes are generally good at a minimum of 10 years following ACL reconstruction. There is some evidence that meniscectomy and articular cartilage damage are associated with poorer outcomes. Patient sex and graft choice do not affect patient-reported outcomes. Further large prospective cohort studies with good follow-up, consistent outcome reporting, and regression modeling are needed to clarify predictors of long-term patient-reported outcomes of ACL reconstruction.
One or more of the authors has declared the following potential conflict of interest or source of funding: Research support was provided by grant numbers K23AR063767 (to R.A.M.) and R01AR05557 (to K.P.S.) from the National Institutes of Health–National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIH-NIAMS) and aided by a grant from the Orthopaedic Research and Education Foundation (OREF). Funding for open access was provided by The Ohio State University Open Access Fund.
References
- 1. Barenius B, Ponzer S, Shalabi A, Bujak R, Norlen L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42:1049–1057. [DOI] [PubMed] [Google Scholar]
- 2. Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40:1985–1992. [DOI] [PubMed] [Google Scholar]
- 3. Calvert M, Blazeby J, Altman DG, Revicki DA, Moher D, Brundage MD. Reporting of patient-reported outcomes in randomized trials: the CONSORT PRO extension. JAMA. 2013;309:814–822. [DOI] [PubMed] [Google Scholar]
- 4. Cox CL, Huston LJ, Dunn WR, et al. Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? A 6-year multicenter cohort study. Am J Sports Med. 2014;42:1058–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Crawford SN, Waterman BR, Lubowitz JH. Long-term failure of anterior cruciate ligament reconstruction. Arthroscopy. 2013;29:1566–1571. [DOI] [PubMed] [Google Scholar]
- 6. Felmet G. Implant-free press-fit fixation for bone-patellar tendon-bone ACL reconstruction: 10-year results. Arch Orthop Trauma Surg. 2010;130:985–992. [DOI] [PubMed] [Google Scholar]
- 7. Forster MC, Forster IW. Patellar tendon or four-strand hamstring? A systematic review of autografts for anterior cruciate ligament reconstruction. Knee. 2005;12:225–230. [DOI] [PubMed] [Google Scholar]
- 8. Greenhalgh T. How to Read a Paper: The Basics of Evidence Based Medicine. 2nd ed London, UK: BMJ Publishing Group; 2001. [Google Scholar]
- 9. Hanypsiak BT, Spindler KP, Rothrock CR, et al. Twelve-year follow-up on anterior cruciate ligament reconstruction: long-term outcomes of prospectively studied osseous and articular injuries. Am J Sports Med. 2008;36:671–677. [DOI] [PubMed] [Google Scholar]
- 10. Hart AJ, Buscombe J, Malone A, Dowd GS. Assessment of osteoarthritis after reconstruction of the anterior cruciate ligament: a study using single-photon emission computed tomography at ten years. J Bone Joint Surg Br. 2005;87:1483–1487. [DOI] [PubMed] [Google Scholar]
- 11. Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med. 2010;38:448–454. [DOI] [PubMed] [Google Scholar]
- 12. Janssen RP, du Mée AW, van Valkenburg J, Sala HA, Tseng CM. Anterior cruciate ligament reconstruction with 4-strand hamstring autograft and accelerated rehabilitation: a 10-year prospective study on clinical results, knee osteoarthritis and its predictors. Knee Surg Sports Traumatol Arthrosc. 2013;21:1977–1988. [DOI] [PubMed] [Google Scholar]
- 13. Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C. Arthroscopic reconstruction of the anterior cruciate ligament using bone–patellar tendon–bone autograft: a minimum 10-year follow-up. Am J Sports Med. 2008;36:1275–1282. [DOI] [PubMed] [Google Scholar]
- 14. Magnussen RA, Carey JL, Spindler KP. Does autograft choice determine intermediate-term outcome of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2011;19:462–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Magnussen RA, Mansour AA, Carey JL, Spindler KP. Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg. 2009;22:347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;(9):CD005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Moller E, Weidenhielm L, Werner S. Outcome and knee-related quality of life after anterior cruciate ligament reconstruction: a long-term follow-up. Knee Surg Sports Traumatol Arthrosc. 2009;17:786–794. [DOI] [PubMed] [Google Scholar]
- 18. Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434–1443. [DOI] [PubMed] [Google Scholar]
- 19. Oiestad BE, Holm I, Aune AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38:2201–2210. [DOI] [PubMed] [Google Scholar]
- 20. Ryan J, Magnussen RA, Cox CL, Hurbanek JG, Flanigan DC, Kaeding CC. ACL reconstruction: do outcomes differ by sex? A systematic review. J Bone Joint Surg Am. 2014;96:507–512. [DOI] [PubMed] [Google Scholar]
- 21. Sajovic M, Strahovnik A, Dernovsek MZ, Skaza K. Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: an 11-year follow-up of a randomized controlled trial. Am J Sports Med. 2011;39:2161–2169. [DOI] [PubMed] [Google Scholar]
- 22. Shelbourne KD, Gray T. Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med. 2009;37:471–480. [DOI] [PubMed] [Google Scholar]
- 23. Spindler KP, Kuhn JE, Dunn W, Matthews CE, Harrell FE, Dittus RS. Reading and reviewing the orthopaedic literature: a systematic, evidence-based medicine approach. J Am Acad Orthop Surg. 2005;13:220–229. [DOI] [PubMed] [Google Scholar]
- 24. Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93:1159–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wu H, Hackett T, Richmond JC. Effects of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconstruction: a long-term prospective study. Am J Sports Med. 2002;30:845–850. [DOI] [PubMed] [Google Scholar]