Abstract
Background:
Procedures performed by surgeons with higher provider volumes offer advantages both to the individual patient and the health system, with studies documenting fewer adverse events, shorter surgical times, and decreased reoperation rates. With workforce requirements for surgeons growing, it is increasingly necessary to establish the most efficient structure of this workforce.
Hypothesis:
Substantial economic savings are realized when procedures are performed by high-volume providers as compared with low-volume providers in the areas of readmission, prolonged admission, and subsequent surgery.
Study Design:
Economic and decision analysis; Level of evidence, 2.
Methods:
This study utilized decision modeling to estimate the cost savings to high-volume providers in sports medicine. Simple decision models were constructed for 3 common procedures: anterior cruciate ligament (ACL) reconstruction, rotator cuff repair, and total shoulder arthroplasty. Outcome probabilities for adverse events (readmission, prolonged admission, and subsequent surgery) and costs were taken from the literature. A Monte Carlo simulation reflecting the incidence of these procedures in the United States was performed to estimate the total nationwide cost of these procedures, and the impact of both negative and positive policies on this cost were examined using sensitivity analysis.
Results:
The costs per case attributable to adverse outcomes for ACL reconstruction (in 2010 US$) were $496, $781, and $868 for high-, medium-, and low-volume providers, respectively. For rotator cuff repair, these numbers were $523, $640, and $872, and for total shoulder arthroplasty, $1692, $1876, and $2021, respectively. Sensitivity analysis revealed that a 50% increase in the number of these 3 procedures performed by high-volume surgeons could save the health system $23.1 million. If all procedures were performed by high-volume surgeons, the health system could save $72 million.
Conclusion:
The hypothesis was accepted; higher provider volumes for surgeons do convey substantial societal economic benefits. Policies to incentivize and facilitate a greater portion of procedures being performed by high-volume surgeons may increase the efficiency of resource utilization in health care delivery.
Keywords: high-volume providers, economic impact, sports medicine, provider volume
Several authors have documented fewer adverse events and improved outcomes when procedures are performed by high-volume surgeons and in high-volume hospitals.7,9,10,12,19,20,22 Additionally, high-volume providers appear to be more efficient, producing superior outcomes at a lower cost.8,21
Optimal societal health care delivery is often discussed as having 3 primary components: effectiveness, equity, and efficiency. Historically, health in the United States focused on maximizing effectiveness, and the recent Patient Protection and Affordable Care Act attempted to remedy the inequities within the US health care system. To provide these 2 components, we must now focus significant effort on investigating and implementing efficient clinical practice. Because workforce requirements for surgeons are growing, it is increasingly necessary to establish the most efficient structure of this workforce.15
Our hypothesis was that high-volume surgeons provide substantial economic savings as compared with low-volume surgeons in the areas of readmission, prolonged admission, and subsequent surgery. In this article, we utilize the power of decision modeling to estimate the financial impact of high-volume providers using the example of sports medicine.
Methods
General Model Overview
To illustrate potential cost savings, the analysis focused on one area of surgical specialization: orthopaedic sports medicine. Reasons for this example are as follows: (1) the primary procedures performed are increasing in prevalence, (2) the procedures require sufficient technical skill for high volume to be important, and (3) provider volume has been well studied.16 A simple decision model was created to compare specific adverse outcomes for 3 major procedures germane to orthopaedic sports medicine–trained physicians: anterior cruciate ligament (ACL) reconstruction, rotator cuff repair, and total shoulder arthroplasty. These are 3 procedures for which fellowship-trained sports medicine surgeons are expected to attain expertise, and they account for a large portion of sports medicine surgical procedures.
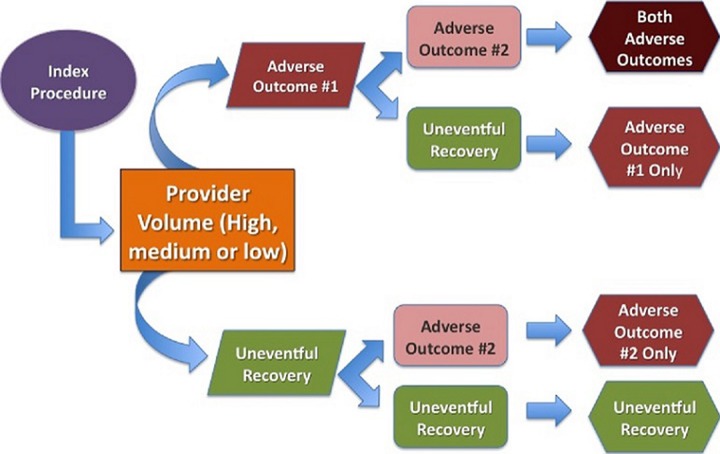
The model begins with a patient being treated by a high-, medium-, or low-volume provider. The patient will transition to adverse outcome #1 or uneventful outcome and then to adverse outcome #2 or uneventful recovery based on published rates of these adverse outcomes. At the end of the model, patients can experience 1 of 4 outcomes: 2 adverse events, 1 of either, or uneventful recovery. Figure 1 shows a schematic of the model.
Figure 1.
Decision model schematic.
Adverse Outcomes
The model focuses only on specific adverse outcomes studied from large state and national databases.11,13,17 Three distinct adverse outcomes were examined for each procedure. These outcomes were (1) additional knee surgery within 1 year and readmission within 30 days for ACL reconstruction, (2) nonroutine discharge and increased length of stay for rotator cuff repair, and (3) complications and nonroutine discharge for total shoulder arthroplasty. These particular adverse outcomes were chosen because they are measurable, important, and have been shown to be significantly related to provider volume.11,13,17,18 The baseline values for each of these and their sources are found in Table 1.
TABLE 1.
Base Case Model Parametersa
| Variable | Base Case Probability, % | Adjusted Odds Ratio (95% CI) |
|---|---|---|
| Rotator cuff repair | ||
| Nonroutine discharge | ||
| High volume | 0.8 | 1.0 |
| Medium volume | 0.8 | 1.5 (0.7-3.1) |
| Low volume | 1.5 | 2.8 (0.9-9.1) |
| Extended stay | ||
| High volume | 21.5 | 1.0 |
| Medium volume | 26.8 | 1.3 (0.7-2.6) |
| Low volume | 39.2 | 2.3 (1.2-4.4) |
| ACL reconstruction | ||
| Readmission | ||
| High volume | 2.3 | 1.0 |
| Medium volume | 5.0 | 1.18 (0.99-1.39) |
| Low volume | 5.6 | 1.44 (1.19-1.75) |
| Subsequent knee surgery | ||
| High volume | 6.1 | 1.0 |
| Medium volume | —b | 1.41 (1.01-1.48) |
| Low volume | —b | 1.19 (1.01-1.41) |
| Total shoulder arthroplasty | ||
| Complication | ||
| High volume | 0.8 | |
| Medium volume | 1.34 | 1.5 (0.7-3.0) |
| Low volume | 1.46 | 1.4 (0.6-3.0) |
| Nonroutine discharge | ||
| High volume | 26.8 | 1.0 |
| Medium volume | 28.7 | 0.98 (0.8-1.2) |
| Low volume | 30.9 | 1.1 (0.8-1.4) |
aACL, anterior cruciate ligament.
bThese values were obtained from the author of this source and were requested to be left out of the article directly.
Provider Volume Characteristics
Provider volume characteristics varied for each procedure. These numbers and classification of high-, medium-, and low-volume providers were obtained from our literature search and not determined ourselves. For ACL reconstruction, high-volume providers were defined as those performing greater than 52 cases annually (ie, 1 case weekly). Low-volume providers performed less than 6 procedures annually. All others were considered medium volume. Lyman et al16 found that low-volume providers as defined above had a higher complication rate as compared with medium- and high-volume providers. For rotator cuff repair, high-volume providers were defined as those performing greater than 30 cases annually. Low-volume providers performed fewer than 15 procedures annually. All others were considered medium volume. Jain et al12 found a higher likelihood for an extended length of stay for patients with rotator cuff repairs performed by low-volume surgeons when compared with those operated on by high-volume surgeons, as above. For total shoulder arthroplasty, high-volume providers were defined as those performing greater than 5 cases annually. Low-volume providers perform less than 2. All others were considered medium volume. Jain et al12 found an increased length of stay for patients who had a total shoulder arthroplasty performed by low-volume providers as compared with high-volume providers.
Cost Estimates
A cost attributable to each adverse outcome was calculated and is noted in Table 2. All costs were converted to 2010 US dollars.5 It should be noted that none of the cost values used in this study were charges. These values measured costs or costs estimated from charges using a cost-to-charge ratio. The source and methodology for estimating these costs follows. If standard deviation or confidence intervals were available, a range of values were used in the model.
TABLE 2.
Base Case Parameters: Costsa
| Parameter | 2010 US$ | Range Tested | Source |
|---|---|---|---|
| Nonroutine discharge (TSA, RCR) | $5293 | $494-$11,989 | Hervey et al6 |
| Extended stay (RCR) | $1850 | $1100-$3300 | Baldwin et al1 |
| Additional knee surgery (ACL) | $4366 | $2498-$6234 | Medicare |
| Readmission (ACL) | $10,000 | $10,000 | Ilizaliturri et al8; Lau et al15 |
| Postoperative complication (TSA) | $5625 | $3676-$8920 | Lyman et al16 |
aACL, anterior cruciate ligament; RCR, rotator cuff repair; TSA, total shoulder arthroplasty.
Readmission is frequently discussed as a target for improved resource utilization and is tracked nationally by the Centers for Medicare and Medicaid Services. The Agency for Health Care Research and Quality reported the average cost of a readmission to be approximately $7400 in 1999 dollars. We converted this to 2010 dollars, using $10,000 for this input value.6 Other authors have reported similar findings.14
Additional knee surgery was assigned a cost of $4366. The Current Procedural Terminology (CPT) code for diagnostic knee arthroscopy (29870) plus the ambulatory facility fee combined for a cost of $2498 based on current Medicare charges. Six weeks of additional physical therapy at $1868 made up the additional cost. This is a conservative estimate, as diagnostic arthroscopy is the least expensive arthroscopic procedure that could be performed.
Medicare reimbursement of skilled nursing facilities was used to estimate the cost of nonroutine discharge. DeJong et al3 found total knee and hip arthroplasty patients to have enough physical and occupational therapy to qualify for 3 resource utilization groups (RUG) in addition to the daily fee. Rehabilitation for the 3 procedures in this study does not differ greatly from that of hip and knee arthroplasty from a billing or duration of physical therapy standpoint. From these findings using current Medicare reimbursement charge data, the daily cost of nonroutine discharge was estimated to be $495 per day. DeJong et al3 reported a mean length of stay (±SD) of 10.7 ± 6.9 days for the same group. The mean and 95% confidence interval for the cost of nonroutine discharge is therefore $5293 ($494-$11,989).2
Khan et al14 reported the median cost of all noncardiac inpatient surgery complications at $4278 (95% CI, $2743-$6656). These data were collected from all adult (16 years and older) noncardiac surgery patients at a single 750-bed tertiary care and academic teaching hospital in Canada between July 1996 and March 1998. Patients undergoing same-day surgery were excluded. This cost was converted to 2010 US dollars at $5625 (95% CI, $3676-$8920). Available data on the specific complications for total shoulder arthroplasty are not available; therefore, we used the mean value.
Finally, the cost of increased length of stay for rotator cuff and total shoulder arthroplasty was estimated at $1850. The Agency for Healthcare Research and Quality reported the average daily cost of hospitalization based on the Healthcare Cost and Utilization Project (HCUP) data to be $1600 in 2004 US dollars.7 This HCUP data set included all patients other than trauma patients (excluding patients with head injuries, spinal cord injuries, fractures, dislocation, burns, open wounds, and sprains/strain) admitted to over 1000 community hospitals in 2004, representing over 36 million individual hospital stays. These trauma patients were excluded, as their average hospitalizations were found to cost even more than other patients at $2100.7 Our final dollar figures are derived after converting the initial $1600 to 2010 dollars. We conservatively assumed 1 additional day for the increased length of stay.
Base Case Financial Analysis
Annual costs attributable to adverse outcomes were calculated. First, the cost attributable to measurable adverse outcomes was calculated per surgical case for each provider volume. Based on national volume estimates for the 3 procedures and the proportion performed by each provider volume, the number of cases performed annually by high-, medium-, and low-volume providers was calculated. The per-case cost was multiplied by these numbers to estimate the dollars spent annually on the care of adverse outcomes. This was done simply by multiplying the cost of each adverse event times the probability of occurrence of each event multiplied by the annual incidence of each procedure in the United States.
The United Healthcare database (UHD), based in Minneapolis, Minnesota, was used to calculate national case volumes for each procedure. The UHD consists of inpatient, outpatient, and physician charges from orthopaedic records within the database, which covers approximately 10% of private-payer insurance in the United States. This database spans from 2004 to 2009 and allows for full patient tracking through outpatient, inpatient, and physician-directed orthopaedic care. We collaborated with PearlDiver Technologies to create a subset of patients within the searchable database of Health Insurance Portability and Accountability Act–compliant records from orthopaedic patients included in the UHD. These patient records were searched by use of International Classification of Diseases, 9th Edition, clinical modification codes, as well as Current Procedural Terminology, 4th Revision (CPT-4) codes.
The standard deviation was reported using Monte Carlo microsimulation of the annual incidence of these procedures in the United States. A Monte Carlo simulation is a decision model that utilizes random sampling to obtain the probability distribution of an unknown event. In this case, our Monte Carlo simulation was run to determine the incidence of the above adverse events in the entire US population.
Sensitivity Analysis
Sensitivity analysis was employed to assess the financial impact of varying the proportion of cases performed by high-volume providers. A sensitivity analysis examines the effect of a dependent variable on the output of a model. In this case, we investigated the effect of an increased or decreased number of high-volume surgeons on national cost savings. Five theoretical scenarios were investigated: an increase of 50% and 25% or a decrease of 50% and 25% in the proportion of cases performed by high-volume providers. The final scenario represented the savings associated with all cases being performed by high-volume providers. Finally, the impact of these scenarios over time was examined by calculating the cumulative economic gains or losses from national volume projections for ACL reconstruction, rotator cuff repair, and total shoulder arthroplasty. Such analyses can demonstrate how much of the total cost of these 3 procedures could be modified by changes in the proportion of high-volume surgeons nationally.
Results
Base Case
The results of the base case financial analysis including the cost per case attributable to adverse outcomes for each provider volume level are noted in Table 3. The costs per case attributable to adverse outcomes for ACL reconstruction were $496 ± $7, $781 ± $8, and $868 ± $8 for high-, medium-, and low-volume providers, respectively. For rotator cuff repair, these numbers were $523 ± $3, $640 ± $3, and $872 ± $3, respectively. Last, for total shoulder arthroplasty, these values were $1692 ± $26, $1876 ± $27, and $2021 ± $28, respectively.
TABLE 3.
Cost per Case Attributable to Adverse Eventsa
| Provider Volume | Rotator Cuff Repair | ACL Reconstruction | Total Shoulder Arthroplasty | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Cost per Case (SD) | Cases, % | Annual Costb | Cost per Case (SD) | Cases, % | Annual Costb | Cost per Case (SD) | Cases, % | Annual Costb | |
| High | $523 (2) | 33.6 | $43,932 | $496 (6) | 21.7 | $11,314 | $1692 (25) | 28.9 | $4890 |
| Medium | $640 (2) | 24.7 | $39,520 | $781 (7) | 62 | $50,940 | $1876 (26) | 37.6 | $7054 |
| Low | $872 (2) | 41.7 | $90,906 | $868 (7) | 18.1 | $16,514 | $2021 (27) | 33.5 | $6770 |
aAll costs are in 2010 US dollars. ACL, anterior cruciate ligament.
bTotal annual cost in thousands to the health system from each provider volume level.
Sensitivity Analysis
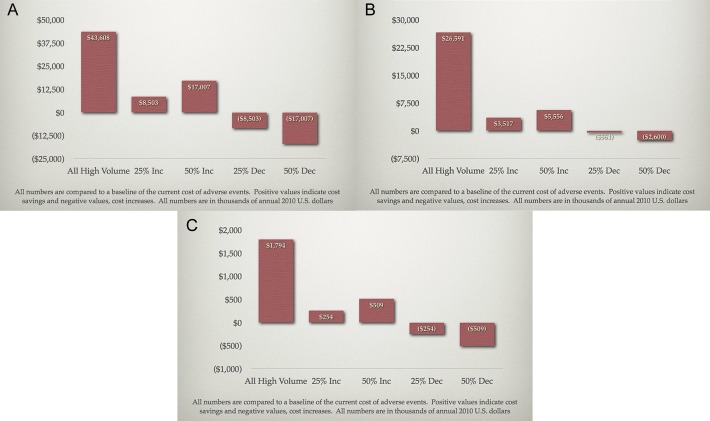
The results of the sensitivity analysis on proportion of cases performed by high-volume providers are found in Figure 2. ACL reconstruction is represented in Figure 2A, rotator cuff repair in Figure 2B, and total shoulder arthroplasty in Figure 2C. The annual cost savings or increase based on these policy examples is substantial.
Figure 2.
Sensitivity analysis for the proportion of cases performed by high-volume providers. (A) Rotator cuff tears, (B) anterior cruciate ligament tears, and (C) shoulder arthroplasty.
Discussion
Our hypothesis was accepted: High-volume providers do convey substantial societal economic savings related to their rates of readmission, prolonged admission, and subsequent surgery in sports medicine. Furthermore, in quantifying the effect, we showed that this economic savings is quite substantial. Though this savings is small compared with the $576 billion spent per year on musculoskeletal care in the United States, it is none the less a substantial sum.2
A number of recent papers have found that higher provider procedure volumes are associated with fewer adverse events in the field of sports medicine. Jain et al10 examined the New York State Ambulatory Surgery Database from 1997 through 2000 for the association between provider volume and both length of stay and discharge disposition. They found that low-volume providers (less than 15 procedures) had a higher adjusted odds ratio of extended length of stay (2.3; 95% CI, 1.2-4.4) and nonroutine discharge status (2.8; 95% CI, 0.9-9.1) than did high-volume providers (greater than 30 procedures).
Jain et al12 also examined the Nationwide Inpatient Sample Database from 1988 to 2000 (a database of 5-8 million inpatient admission per year) for the effects of provider volume on a variety of outcome indicators following total shoulder arthoplasty. Their analysis revealed providers who performed less then 2 total shoulder arthoplasties per year had higher risk adjusted rates of complications (including postoperative infections, pulmonary embolism, and thrombophlebitis; 1.46 vs 0.80), mortality (0.36 vs 0.20), and nonroutine discharge (30.9% vs 26.8%) than did high-volume providers (greater than 4 or 5 procedures per year). Providers who performed less than 2 total shoulder arthroplasties per year also had a longer average length of stay as compared with providers performing 5 or more per year (4 vs 3.3 days; P = .001).
Finally, Jain et al11 reviewed the State Ambulatory Surgery Database from 1997 to 2000 for the correlation between ACL provider volume and discharge disposition and operative time. They disovered that low-volume providers (<25 ACL repairs per year) had a higher adjusted odds ratio of nonroutine discharges (3.5; 95% CI, 1.7-7.2) and spent on average 27 more minutes in the operating room as compared with high-volume providers (>75 ACLs per year). These results are all consistent with what we have found in this study.11
Given the increasing focus on reducing health care expenditures, increasing the proportion of surgical cases performed by high-volume providers may contribute to reducing the rate of cost growth. Further study is certainly needed to identify how to maximize the proportion of cases performed by high-volume providers as compared with low- or medium-volume providers. Additional research could also help elucidate how to design training programs to produce the appropriate number of high-volume providers.
One potential way to increase the proportion of high-volume providers is to increase the number of trainees undergoing fellowship training or to bring the concepts of specialization into training programs earlier. During fellowship, trainees spend time honing their skills on a smaller number of procedures than they do during residency, potentially allowing them to become better and more efficient at these procedures. Though there are currently no data on the effects of surgical specialization on procedure volumes, it is certainly conceivable that increased fellowship training could lead to an increased proportion of high-volume providers. However, on a system level, increased subspecialty training is costly, and it is unclear whether the increased cost of subspecialty training could be offset by an increase in the proportion of high-volume providers. Given that some data exist on the cost of fellowship training, further research could help elucidate this point.
Another strategy for increasing the proportion of high-volume providers is to bring patients from rural areas to high-volume providers to undergo elective procedures. Research from Fitzgerald et al4 indicated that in 2001, 11,550 Medicare patients underwent total knee arthroplasties in low-volume centers. Of these, 1506 patients would have had to travel >50 miles and 259 patients would have had to travel >100 miles to reach a high-volume provider.4 Thus, transportion costs are likely substantial. However, it is possible the net economic effect to society of savings from high-volume providers minus increased transportion costs could be positive, thereby decreasing total societal heath care cost. Additionally, developing incentives created by the Patient Protection and Affordable Care Act that increase cost sharing (eg, tiering) could incentivize patients to pay the out-of-pocket transportation costs to receive less expensive care from high-volume providers.
It should be noted that our financial estimates are highly conservative. These savings are based on only 3 of the many procedures performed at an expert level by sports medicine surgeons. It does not include other orthopaedic subspecialties known to have specialization benefits such as total joint arthroplasty.15,19 Furthermore, other unreported adverse outcomes are possible. Finally, the outcomes we examine are short term; we do not account for long-term outcomes that may offer additional cost savings such as future shoulder arthroplasty, ACL revisions, or meniscus tears in ACL-deficient knees. While these entities could further support high-volume providers, the financial importance of these providers is clear from the few outcomes examined in this study.
There are several weaknesses in this study. First, the cost of the adverse outcomes is likely fluid, and the data used for the complications estimate was 12 years old. Second, the data on provider volume are from a single point in time and may not reflect current health care system values. Additionally, much of the data used in this study come from the state of New York, and thus, these data could certainly vary based on a different geographical region.
We also recognize that some of the estimated nonroutine discharge cost data for ACL reconstruction and rotator cuff repair are based on total joint arthroplasty readmission data. Though estimations of readmission data for these procedures would be ideal, unfortunately, such high-quality data have not been published in the current literature. Thus, total joint arthroplasty cost data were used as there are excellent, robust data on the cost of joint arthroplasty readmissions. Additionally, it was felt that the inpatient costs per day for ACL reconstruction or rotator cuff repair were unlikely to vary substantially from the cost of an additional inpatient day for a joint arthoplasty patient, given that most of the relevant costs (provider labor costs, facility charges, medications) were likely to be very similar. Thus, these cost data were felt to be the best proxy for these costs available in the current literature.
Clearly missing from this analysis is the effectiveness of provider volume. We only examine cost, but high provider volume may produce effectiveness gains as well.9,15 In particular, a systematic review found poorer outcomes for low-volume providers in total joint arthroplasty, specifically increased infection rates, length of stay, and worse patient-reported outcomes.15 Another study noted that low-volume providers had a 26% increased mortality rate for total knee arthroplasties as compared with high-volume providers.9 Additionally, this further supports that our analysis is conservative in reporting the benefits of specialization.
We recognize that access challenges may limit the impact of policies aimed to increase high-volume providers and may not be practical or possible in all circumstances. Other authors have demonstrated the inherent difficulties in models of increasing the proportion of high-volume providers.1
Conclusion
High-volume surgeons confer clear and substantial economic benefits based on the rates of postoperative readmission, prolonged admission, and subsequent surgery compared with low- and medium-volume surgeons. Furthermore, the specific numbers from our analysis could only represent a portion of the potential economic savings. Further research is needed to elucidate what other benefits high-volume providers may have over low-volume providers in the field of sports medicine.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: A.D. is a paid consultant for Arthrex, Smith & Nephew Endoscopy, and Symbionix.
References
- 1. Baldwin LM, Cai Y, Larson EH, et al. Access to cancer services for rural colorectal cancer patients. J Rural Health. 2008;24:390–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Burden of Musculoskeletal Diseases in the United States: Prevalence, Societal and Economic Cost. Rosemont, IL: American Association of Orthopaedic Surgeons; 2008:7. [Google Scholar]
- 3. DeJong G, Horn SD, Smout RJ, Tian W, Putman K, Gassaway J. Characterizing rehabilitation services for patients with knee and hip replacement in skilled nursing facilities and inpatient rehabilitation facilities. Arch Phys Med Rehabil. 2009;90:1269–1283. [DOI] [PubMed] [Google Scholar]
- 4. Fitzgerald JD, Soohoo NF, Losina E, Katz JN. Potential impact on patient residence to hospital travel distance and access to care under a policy of preferential referral to high-volume knee replacement hospitals. Arthritis Care Res (Hoboken). 2012;64:890–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Friedman B, Basu J. The rate and cost of hospital readmissions for preventable conditions. Med Care Res Rev. 2004;61:225–240. [DOI] [PubMed] [Google Scholar]
- 6. Hervey SL, Purves HR, Guller U, Toth AP, Vail TP, Pietrobon R. Provider volume of total knee arthroplasties and patient outcomes in the HCUP-nationwide inpatient sample. J Bone Joint Surg Am. 2003;85-A:1775–1783. [DOI] [PubMed] [Google Scholar]
- 7. HCUP Statistical Brief #18: Frequency and Costs of Hospital Admissions for Injury, 2004. Rockville, MD: Agency for Health Care Policy and Research; 2006:1–7. [PubMed] [Google Scholar]
- 8. Ilizaliturri VM, Jr, Orozco-Rodriguez L, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of cam-type femoroacetabular impingement: preliminary report at 2 years minimum follow-up. J Arthroplasty. 2008;23:226–234. [DOI] [PubMed] [Google Scholar]
- 9. Jain N, Guller U, Pietrobon R, Bond T, Higgins L. Comorbidities increase complication rates in patients having arthroplasty. Clin Orthop Relat Res. 2005;(435):232–238. [DOI] [PubMed] [Google Scholar]
- 10. Jain N, Pietrobon R, Guller U, Ahluwalia A, Higgins L. Influence of provider volume on length of stay, operating room time, and discharge status for rotator cuff repair. J Shoulder Elbow Surg. 2005;14:407–413. [DOI] [PubMed] [Google Scholar]
- 11. Jain N, Pietrobon R, Guller U, Shankar A, Ahulwalia AS, Higgins LD. Effect of provider volume on resource utilization for surgical procedures of the knee. Knee Surg Sports Traumatol Arthrosc. 2005;13:302–312. [DOI] [PubMed] [Google Scholar]
- 12. Jain N, Pietrobon R, Hocker S, Guller U, Shankar A, Higgins L. The relationship between surgeon and hospital volume and outcomes for shoulder arthroplasty. J Bone Joint Surg Am. 2004;86-A:496–505. [DOI] [PubMed] [Google Scholar]
- 13. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. [DOI] [PubMed] [Google Scholar]
- 14. Khan NA, Quan H, Bugar JM, Lemaire JB, Brant R, Ghali WA. Association of postoperative complications with hospital costs and length of stay in a tertiary care center. J Gen Intern Med. 2006;21:177–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lau RL, Perruccio AV, Gandhi R, Mahomed NN. The role of surgeon volume on patient outcome in total knee arthroplasty: a systematic review of the literature. BMC Musculoskelet Disord. 2012;13:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91:2321–2328. [DOI] [PubMed] [Google Scholar]
- 17. Paterson JM, Williams JI, Kreder HJ, et al. Provider volumes and early outcomes of primary total joint replacement in Ontario. Can J Surg. 2010;53:175–183. [PMC free article] [PubMed] [Google Scholar]
- 18. Salsberg ES, Grover A, Simon MA, Frick SL, Kuremsky MA, Goodman DC. An AOA critical issue. Future physician workforce requirements: implications for orthopaedic surgery education. J Bone Joint Surg Am. 2008;90:1143–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. SooHoo NF, Farng E, Lieberman JR, Chambers L, Zingmond DS. Factors that predict short-term complication rates after total hip arthroplasty. Clin Orthop Relat Res. 2010;468:2363–2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. SooHoo NF, Lieberman JR, Ko CY, Zingmond DS. Factors predicting complication rates following total knee replacement. J Bone Joint Surg Am. 2006;88:480–485. [DOI] [PubMed] [Google Scholar]
- 21. Specialists provide the best, most cost-efficient care for migraine headache patients. Health Care Cost Reengineering Rep. 1998;3:106–108. [PubMed] [Google Scholar]
- 22. Wei MH, Lin YL, Shi HY, Chiu HC. Effects of provider patient volume and comorbidity on clinical and economic outcomes for total knee arthroplasty. J Arthroplasty. 2010;25:906–912. [DOI] [PubMed] [Google Scholar]