Abstract
Background
Resorbable anchors are widely used in arthroscopic stabilization of the shoulder as a means of soft tissue fixation to bone. Their function is to ensure repair stability until they are replaced by host tissue. Complications include inflammatory soft tissue reactions, cyst formation, screw fragmentation in the joint, osteolytic reactions, and enhanced glenoid rim susceptibility to fracture.
Purpose
To evaluate resorption of biodegradable screws and determine whether they induce formation of areas with poor bone strength that may lead to glenoid rim fracture even with minor trauma.
Study Design
Case series; Level of evidence, 4.
Methods
This study evaluated 12 patients with anterior shoulder instability who had undergone arthroscopic stabilization with the Bankart technique and various resorbable anchors and subsequently experienced redislocation. The maximum interval between arthroscopic stabilization and the new dislocation was 52 months (mean, 22.16 months; range, 12-52 months). The mean patient age was 31.6 years (range, 17-61 years). The persistence or resorption of anchor holes; the number, area, and volume of osteolytic lesions; and glenoid erosion/fracture were assessed using computed tomography scans taken after redislocation occurred.
Results
Complete screw resorption was never documented. Osteolytic lesions were found at all sites (mean diameter, 5.64 mm; mean depth, 8.09 mm; mean area, 0.342 cm2; mean volume, 0.345 cm3), and all exceeded anchor size. Anterior glenoid rim fracture was seen in 9 patients, even without high-energy traumas (75% of all recurrences).
Conclusion
Arthroscopic stabilization with resorbable devices is a highly reliable procedure that is, however, not devoid of complications. In all 12 patients, none of the different implanted anchors had degraded completely, even in patients with longer follow-up, and all induced formation of osteolytic areas. Such reaction may lead to anterior glenoid rim fracture according to the literature and as found in 75% of the study patients with local osteolysis (9/12). Reducing anchor number and/or size may reduce the risk of osteolytic areas and anterior glenoid rim fracture.
Keywords: resorbable, devices, stabilization, shoulder
For decades, open Bankart repair and capsular shift have been the gold standard surgical treatments for anterior shoulder instability. Advances in arthroscopic techniques have involved a steady shift toward arthroscopic procedures.17,24 Further technical progress has vastly improved arthroscopy, so much so that recent studies comparing current arthroscopic techniques with open procedures report similar rates of recurrence.4,5,7,12 Advances in biomedical materials have led to the introduction of a succession of new, effective devices to achieve fixation of the capsulolabral complex to the scapular glenoid.10 The main disadvantages of metal implants include magnetic resonance imaging (MRI) artifacts, the release of metal ions in tissue, the need for a surgical procedure in case of device removal, and increased complexity of revision surgery. For these reasons, biodegradable anchors are commonly preferred in arthroscopic stabilization procedures. Resorbable anchors are compatible with MRI and computed tomography (CT), and they provide options for easier revision surgery9 while ensuring primary stability equivalent to that obtained with nonresorbable devices.15 A major characteristic of biodegradable materials is that they are eventually replaced by host tissue. Although the early stages of degradation involve formation of fibrous tissue,19,27,28 little is known about actual anchor resorption and replacement with host tissue. Complete device replacement by bone has not been demonstrated either experimentally or clinically in most patients.29 Complications associated with biodegradable devices include cyst formation, inflammatory reactions, fragment dispersion in the joint, and local osteolysis.6,18,30 Although several investigators have reported osteolytic lesions at the site of the bioresorbable implants,§ an association between osteolysis and poor clinical outcomes has never been documented. The study’s purpose was to evaluate the consistent finding of osteolysis about bioresorbable suture anchors in 12 cases of redislocation after arthroscopic repair and its potential role as a predisposing factor to glenoid fracture. Our hypothesis was that in the presence of osteolytic lesions, the anterior glenoid rim is less resistant to trauma, and therefore the use of bioresorbable suture anchors should not be recommended in contact sport athletes.
Methods
This study was conducted at the Department of Shoulder Surgery at Cervesi Hospital (Cattolica, Italy), directed by the senior author (G.P.). It involved 12 male patients, all of whom had undergone arthroscopic stabilization of the shoulder by the Bankart technique and subsequently experienced a redislocation. The original operation had been performed by the same surgeon (G.P.). Redislocation was treated by open stabilization with Bristow-Latarjet coracoid transfer. We analyzed the epidemiological and CT findings of patients who experienced recurrence. There were 9 left (75%) and 3 (25%) right shoulders. Different types of anchors, with different diameters, had been implanted in the 12 patients: Lupine Loop Plus suture anchor with No. 2 Panacryl, polylactic acid (PLA; DePuy Mitek) (6 patients [50%]; anchor diameter, 2.8 mm), Bio Mini-Revo Anchor Self-Reinforced 96L/4D PLA with No. 2 Hi-Fi high-strength suture (ConMed Linvatec) (4 patients [33.3%]; anchor diameter, 3.1 mm), and Impact Suture Anchor Self-Reinforced 96L/4D PLA Copolymer with 2 strands of braided polyester (ConMed Linvatec) (2 patients [16.6%]; anchor diameter, 3.5 mm). Labrum repair was performed with different numbers of anchors: 7 patients had received 2 anchors (58.3%), and 5 patients had received 3 anchors (41.6%) (Table 1). The mean patient age was 31.6 years (range, 17-61 years). The maximum interval between arthroscopic stabilization and the new dislocation was 52 months (mean, 22.16 months; range, 12-52 months). The cause of recurrence was a sport injury in 7 patients (58.3%; all professional athletes), and simple trauma with the shoulder in abduction and external rotation was observed in 2 patients (16.6%). Three patients experienced recurrence after a motorcycle accident (25%). The reports and videos of the earlier procedures were reviewed by a blinded, unbiased surgeon for technical errors such as incorrect topographic positioning of the anchor. None of the patients had had glenoid erosion before arthroscopic stabilization, and none had associated lesions detected intraoperatively; all patients reported good shoulder stability without instability symptoms prior to the new dislocation. The persistence or enlargement of anchor holes; the number, area, and volume of osteolytic lesions; and glenoid erosion/fracture were assessed on CT scan (32-detector CT scanner; General Electric) performed at our hospital after injury.
TABLE 1.
Patient and Anchor Characteristics, Cause of Trauma, and Presence of Osteolysis and Glenoid Rim Fractures
| Patient Characteristics | Anchor Characteristics | Cause of Trauma | Time From Surgery to Recurrence, mo | No. of Osteolytic Lesions | Glenoid Rim Fracture | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient No. | Age, y | Sex | Side | Type | No. of Screws | Screw Diameter, mm | ||||
| 1 | 35 | Male | Right | Lupine | 2 | 2.8 | Sport | 21 | 2 | Yes |
| 2 | 37 | Male | Right | Lupine | 2 | 2.8 | Simple | 52 | 2 | No |
| 3 | 35 | Male | Right | Bio Mini-Revo | 3 | 3.1 | Motorcycle accident | 12 | 3 | Yes |
| 4 | 36 | Male | Left | Bio Mini-Revo | 3 | 3.1 | Sport | 23 | 3 | Yes |
| 5 | 19 | Male | Left | Bio Mini-Revo | 3 | 3.1 | Sport | 16 | 3 | Yes |
| 6 | 21 | Male | Right | Lupine | 2 | 2.8 | Sport | 22 | 2 | Yes |
| 7 | 17 | Male | Left | Lupine | 2 | 2.8 | Motorcycle accident | 24 | 2 | No |
| 8 | 61 | Male | Right | Bio Mini-Revo | 2 | 3.1 | Simple | 23 | 2 | Yes |
| 9 | 43 | Male | Right | Impact | 3 | 3.5 | Sport | 33 | 3 | Yes |
| 10 | 19 | Male | Left | Lupine | 2 | 2.8 | Sport | 14 | 2 | Yes |
| 11 | 25 | Male | Left | Impact | 3 | 3.5 | Motorcycle accident | 44 | 3 | Yes |
| 12 | 28 | Male | Right | Lupine | 2 | 2.8 | Sport | 13 | 2 | No |
Data Processing, Radiographic Evaluation Criteria, and Statistical Analysis
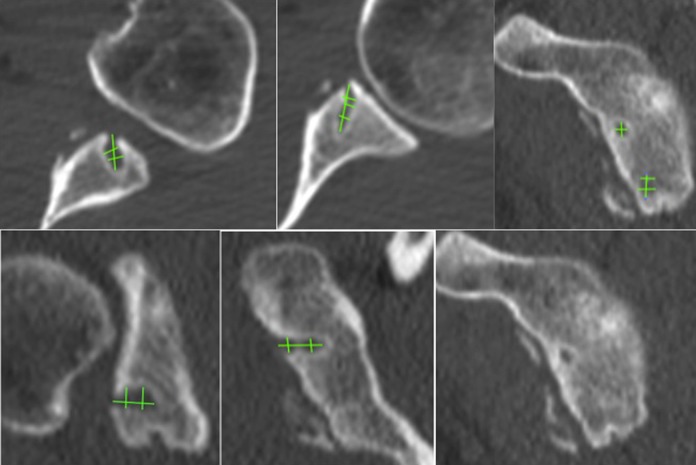
The CT scan evaluation and all measurements were performed using the image processing software OsiriX (v 3.7.1; Pixmeo). Osteolytic lesions were defined as areas (zones) of bone resorption having a diameter and volume exceeding those of the anchor. The volume of each lesion (in cm3) was calculated by measuring its area on the sagittal plane and its depth on the axial and coronal planes (Figure 1). The mean dimensions of osteolytic lesions were obtained from measurements performed by 3 independent raters (orthopaedic surgeons with 20 years of experience in shoulder surgery) at 3 different points of time. The Pearson correlation coefficient was applied to test interobserver reliability.
Figure 1.
Measurement of the osteolytic lesion dimensions.
Results
We found no statistically significant association between glenoid rim fracture and anchor number, anchor type, or volume of osteolytic lesion. We also did not find any correlation between patient age and the incidence of osteolytic lesions or glenoid rim fracture.
Among the 12 patients with recurrence of shoulder dislocation, we observed that all were characterized by the presence of osteolysis around the anchors. In these patients, none of the anchors implanted showed signs of resorption. Seven patients presented 2 osteolytic lesions, and 5 presented 3 osteolytic lesions. We observed 9 patients with anterior glenoid rim fracture (75%).
Patients’ epidemiological data, anchor number and characteristics, type of trauma, presence of osteolysis, and glenoid rim fractures are listed in Table 1.
The mean (±SD) diameter of the osteolytic lesions detected was 5.64 ± 3.48 mm (range, 2.85-14.5 mm). The mean depth of the osteolytic lesions was 8.09 ± 3.37 mm (range, 3.2-15.4 mm). The mean osteolytic area was 0.342 ± 0.43 cm2 (range, 0.06-1.87 cm2), and the mean volume of the lesions was 0.345 ± 0.52 cm3 (range, 0.2-2.14 cm3).
The mean diameter of the osteolytic lesions (measured on the sagittal plane) and their maximum depth (measured on the axial and coronal planes) are reported in Table 2. The mean dimensions of the osteolytic lesions are reported in Table 3. The Pearson correlation coefficient was 0.86 (nearly perfect agreement) for all measurements (P < .05).
TABLE 2.
Mean Diameter and Maximum Depth of the Osteolytic Lesionsa
| Patient No. | Mean Osteolytic Lesion Diameter, mm | Maximum Depth, mm | ||||
|---|---|---|---|---|---|---|
| Lesion 1 | Lesion 2 | Lesion 3 | Lesion 1 | Lesion 2 | Lesion 3 | |
| 1 | 3.3 | 4.7 | 3.6 | 5.3 | 3.5 | |
| 2 | 3.1 | 3.1 | 3.2 | |||
| 3 | 4.25 | 3.7 | 3.2 | 4.5 | 5.7 | 3.5 |
| 4 | 4.3 | 3.95 | 7.65 | 8.7 | 3.9 | 6.5 |
| 5 | 2.85 | 4.8 | 3.05 | 8.4 | 7.3 | 8.3 |
| 6 | 3.9 | 6.05 | 8.5 | 9.7 | ||
| 7 | 2.95 | 3.25 | 8.7 | 8.7 | ||
| 8 | 14.5 | 2.95 | 12.4 | 11.5 | ||
| 9 | 8.05 | 5.65 | 6.3 | 7.9 | 15.4 | 14 |
| 10 | 8.3 | 8.65 | 8.1 | 9.4 | ||
| 11 | 8.65 | 4.25 | 3.1 | 12 | 9.3 | 12.2 |
| 12 | 8.2 | 7 | 10.2 | 12.7 | ||
aLesion diameter was measured on the sagittal plane and lesion depth was measured on the axial and coronal planes of computed tomography scans.
TABLE 3.
Mean Overall Dimensions of the Osteolytic Lesions
| Diameter, mm | Depth, mm | Area, cm2 | Volume, cm3 |
|---|---|---|---|
| 5.64 | 8.09 | 0.342 | 0.345 |
Discussion
Implanting metal fixation anchors in the joint space involves more complications than using resorbable implants, but the latter devices may also entail some complications. Among these, formation of osteolytic lesions at the anchor site has attracted the interest of the orthopaedic community because it might closely correlate with the clinical outcomes of patients treated for shoulder instability. Bioresorbable devices can induce formation of large osteolytic defects, since they often fail to be replaced with bone tissue, but the cause is still unclear. Previous clinical studies found considerable drill hole enlargement after bioresorbable anchor use. Ejerhed et al11 found visible or cystic drill holes on plain radiographs 33 months after surgery; moreover, visible drill holes or drill holes with cystic changes did not appear to heal during the follow-up period. A recent clinical radiographic study of the drill holes in patients subjected to arthroscopic capsulolabral repair25 found that drill holes tended to enlarge over time, negatively affecting clinical outcomes. As defect enlargement was not found in equal measure at all implant sites, local factors besides the presence of the anchor itself may be involved. To the best of our knowledge, no studies have attempted to correlate these osteolytic reactions with clinical data after shoulder instability surgery. In a recent study, Kim et al16 reported the presence of different grades of osteolytic lesions after the use of biodegradable suture anchors (poly(l-lactic acid) [PLLA] and poly(l-dl-lactide) [PLDLA]) for arthroscopic cuff repair in half of their study population, without correlation with repair integrity. One possible effect of osteolytic reactions is loss of holding force, resulting in nonunion of the capsular-labral complex to bone. In a case report, Takubo et al26 described 3 patients with anchor hole enlargement detected by MRI 3 months after arthroscopic Bankart repair with resorbable suture anchors. Although osteolytic lesions have been described after implantation of resorbable screws, their relationship with clinical findings and new dislocation episodes is unclear. Nonetheless, osteolytic lesions involving cortical bone do have the potential to impair its strength and resistance to shear forces. This could have important implications in patients who practice contact sports, since it may entail an increased risk of glenoid rim fracture even with minor trauma. The incidence of glenoid rim fractures resulting from dislocation of a healthy shoulder ranges from 5.4% to 44%8,20,21,23; greater rates may be likely in the presence of osteolytic lesions, even though no data are available in this regard. A recent report describes a traumatic fracture of the anterior rim of the glenoid cavity in 3 professional athletes who had previously been treated for shoulder instability by arthroscopic fixation of the glenoid labrum using resorbable anchors.2 Because all 3 fractures involved the anchor site, those authors suggested that osteolysis resulting from the implantation of resorbable anchors impaired the resistance to trauma of the anterior margin of the glenoid and questioned their use in professional athletes. Fritsch et al13 reported 4 cases of glenoid rim fracture after anchor repair, highlighting the possibility of glenoid fractures with both resorbable and nonresorbable anchors and of dislocation/fracture being caused even by minor injury. This implies a more complex origin of the fracture than simply secondary to cyst formation around a degrading bioresorbable implant. Anchor number, size, material, and insertion pattern may all play a role. Furthermore, osteolysis generated by bioresorbable screws causes bone loss that makes arthroscopic revision of these lesions more complicated. In our study, the anchors had not degraded in all 12 patients affected by recurrence. We also found an osteolytic lesion at each anchor site independently from the used device. Their mean diameter and length were 5.64 mm and 8.09 mm, respectively. But the most significant finding was that the mean volume was 0.345 cm3, which may be far from trivial in terms of overall glenoid volume. In 3 lesions, total bone loss approached 1 cm3. Since the osteolytic lesions detected in our patients varied widely in size, local factors may be involved besides the presence of the anchor itself. Moreover, in all 9 patients with a glenoid rim fracture, the fracture line passed through the line connecting the osteolytic lesions. It is thus reasonable to assume that such lesions weaken the glenoid, increasing the risk of fracture in the event of trauma. It is still reasonable that more screws can increase that risk even if our data do not suggest a statistical relation between the presence of 2 or 3 osteolytic lesions and the incidence of glenoid rim fractures (P = .082). A greater risk of glenoid fracture in the presence of osteolytic lesions has already been reported, particularly in contact sport athletes.2 We found no statistically significant association between glenoid rim fracture and anchor number, anchor type, and volume of osteolytic lesion. We also did not find any correlation between age of the patients and the incidence of osteolytic lesions and glenoid rim fracture. In our opinion, the risk of a glenoid rim fracture should increase as a function of the number of anchors implanted. Several studies have addressed the surgical technique and the number of anchors to be used in arthroscopic shoulder stabilization. Athwal et al1 reported 4 cases of osteolytic lesions and glenohumeral synovitis and chondral damage after use of bioresorbable knotless suture anchors for Bankart repair (Bioknotless suture anchor; Mitek). In their opinion, osteolysis may have developed secondary to micromotion after the anchors lost their initial stability. The poor initial anchor stability was due to the interplay of at least 3 factors: the number of the anchors used (5 in each patient), the knotless concept, and the anchor design. On the basis of the findings of this report, the authors do not recommend the use of these devices when there is a risk of anchor convergence within the glenoid. Boileau et al3 suggested using 4 or more anchors to prevent recurrence of dislocation after arthroscopic stabilization because 3 or fewer anchors would entail a higher risk of redislocation. A recent study by Witney-Lagen et al31 suggested that with the use of 3 or fewer screws for arthroscopic Bankart repair, it is possible to achieve successful shoulder stabilization, with a failure rate of 6.1%. According to other researchers, osteolytic lesions and foreign body reactions with use of resorbable devices are not very frequent.14 In our patients, resorbable anchors induced osteolytic lesions at the anchor site and involved a glenoid rim fracture in 75% of all recurrences. Our data suggest the role of these devices in lowering the bone stock of the anterior glenoid rim in cases of osteolytic lesions. Two patients still had an intact screw (Figure 2), suggesting that even in devices that are claimed to be resorbable, complete degradation may not take place. Our results do not show any correlation between the type and diameter of the screw implanted and the diameter of the osteolytic lesion. In our opinion, the use of smaller anchors or the use of osteoinductive materials can lead to a lower incidence of osteolytic lesions, as reported in the literature.22
Figure 2.

Resorbable devices (2 Bio Mini-Revo anchors) recovered from a patient who experienced redislocation (patient 8) after 23 months of follow-up. A large glenoid rim fracture was found along the anchor holes.
Limitations
This study has some limitations. The devices implanted in our 12 patients were different in size, number, and material, preventing correlation of osteolytic lesions to anchor type. Second, although all 12 patients experienced a redislocation, the presence of osteolysis cannot be generalized to all patients with recurrent dislocation because of the lack of a control group. Moreover, the absence of a control group means that it cannot be demonstrated whether these lesions are also found in asymptomatic patients. The advantages of our study include the fact that all patients were operated on with the same technique by the surgeon who had previously performed the arthroscopic stabilization procedures. Moreover, none of the 12 patients had a glenoid fracture at the time of the stabilization procedure, indicating an intact anterior glenoid rim. Finally, the osteolytic lesions were measured 3 times by 3 different orthopaedic surgeons to maximize accuracy.
Conclusion
Arthroscopic stabilization of the shoulder using resorbable fixation devices is a highly reliable surgical procedure that is, however, not devoid of complications. One of the most insidious problems is formation of osteolytic lesions at the anchor site. Our study showed that most of the anchors had not completely degraded and had induced osteolysis at the screw site. These lesions may weaken the anterior glenoid rim, increasing the risk of a glenoid rim fracture. The use of bioresorbable devices should thus be carefully evaluated, especially in young, active patients like contact sport athletes. New, smaller devices made from osteoinductive materials could help reduce the incidence and/or size of osteolytic lesions.
References
- 1. Athwal GS, Shridharani SM, O’Driscoll SW. Osteolysis and arthropathy of the shoulder after use of bioresorbable knotless suture anchors. A report of four cases. J Bone Joint Surg Am. 2006;88:1840–1845. [DOI] [PubMed] [Google Scholar]
- 2. Banerjee S, Weiser L, Connell D, Wallace AL. Glenoid rim fracture in contact athletes with resorbable suture anchor reconstruction. Arthroscopy. 2009;25:560–562. [DOI] [PubMed] [Google Scholar]
- 3. Boileau P, Villalba M, Héry J-Y, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88:1755–1763. [DOI] [PubMed] [Google Scholar]
- 4. Bottoni CR, Smith EL, Berkowitz MJ, Towle RB, Moore JH. Arthroscopic versus open shoulder stabilization for recurrent anterior instability: a prospective randomized clinical trial. Am J Sports Med. 2006;34:1730–1737. [DOI] [PubMed] [Google Scholar]
- 5. Brophy RH, Marx RG. The treatment of traumatic anterior instability of the shoulder: nonoperative and surgical treatment. Arthroscopy. 2009;25:298–304. [DOI] [PubMed] [Google Scholar]
- 6. Burkhart SS. Case report by Drs. Glueck, Wilson, and Johnson entitled “Extensive osteolysis after rotator cuff repair with a bioresorbable suture anchor” (May 2005, pages 742-744). Am J Sports Med. 2005;33:1768. [DOI] [PubMed] [Google Scholar]
- 7. Cole BJ, L’Insalata J, Irrgang J, Warner JJ. Comparison of arthroscopic and open anterior shoulder stabilization. A two to six-year follow-up study. J Bone Joint Surg Am. 2000;82-A:1108–1114. [DOI] [PubMed] [Google Scholar]
- 8. De Palma AF. Fractures and fracture-dislocations of the shoulder girdle In: Jacob RP, Kristiansen T, Mayo K, Ganz R, Mueller ME, eds. Surgery of the Shoulder. 3rd ed Philadelphia, PA: Lippincott; 1983:366–367. [Google Scholar]
- 9. Dejong ES, DeBerardino TM, Brooks DE, Judson K. In vivo comparison of a metal versus a biodegradable suture anchor. Arthroscopy. 2004;20:511–516. [DOI] [PubMed] [Google Scholar]
- 10. Dhawan A, Ghodadra N, Karas V, Salata MJ, Cole BJ. Complications of bioresorbable suture anchors in the shoulder. Am J Sports Med. 2012;40:1424–1430. [DOI] [PubMed] [Google Scholar]
- 11. Ejerhed L, Kartus J, Funck E, Köhler K, Sernert N, Karlsson J. Resorbable implants for open shoulder stabilization: a clinical and serial radiographic evaluation. J Shoulder Elbow Surg. 2000;9:93–98. [PubMed] [Google Scholar]
- 12. Fabbriciani C, Milano G, Demontis A, Fadda S, Ziranu F, Mulas PD. Arthroscopic versus open treatment of Bankart lesion of the shoulder: a prospective randomized study. Arthroscopy. 2004;20:456–462. [DOI] [PubMed] [Google Scholar]
- 13. Fritsch B, Arciero R, Taylor DC. Glenoid rim fracture after anchor repair: a report of 4 cases. Am J Sports Med. 2010;38:1682–1686. [DOI] [PubMed] [Google Scholar]
- 14. Glueck D, Wilson TC, Johnson DL. Extensive osteolysis after rotator cuff repair with a bioresorbable suture anchor: a case report. Am J Sports Med. 2005;33:742–744. [DOI] [PubMed] [Google Scholar]
- 15. Goradia VK, Mullen DJ, Boucher HR, Parks BG, O’Donnell JB. Cyclic loading of rotator cuff repairs: a comparison of bioresorbable tacks with metal suture anchors and transosseous sutures. Arthroscopy. 2001;17:360–364. [DOI] [PubMed] [Google Scholar]
- 16. Kim SH, Oh JH, Lee O-S, Lee H-R, Hargens AR. Postoperative imaging of bioresorbable anchors in rotator cuff repair. Am J Sports Med. 2014;42:552–557. [DOI] [PubMed] [Google Scholar]
- 17. Kropf EJ, Tjoumakaris FP, Sekiya JK. Arthroscopic shoulder stabilization: is there ever a need to open? Arthroscopy. 2007;23:779–784. [DOI] [PubMed] [Google Scholar]
- 18. Nho SJ, Provencher MT, Seroyer ST, Romeo AA. Bioresorbable anchors in glenohumeral shoulder surgery. Arthroscopy. 2009;25:788–793. [DOI] [PubMed] [Google Scholar]
- 19. Nordström P, Pihlajamäki H, Toivonen T, Törmälä P, Rokkanen P. Tissue response to polyglycolide and polylactide pins in cancellous bone. Arch Orthop Trauma Surg. 1998;117:197–204. [DOI] [PubMed] [Google Scholar]
- 20. Palmer I, Widén A, Sweden S. The bone block method for recurrent dislocation of the shoulder joint. J Bone Joint Surg Br. 1948;30-B:53–58. [PubMed] [Google Scholar]
- 21. Porcellini G, Campi F, Paladini P. Arthroscopic approach to acute bony Bankart lesion. Arthroscopy. 2002;18:764–769. [DOI] [PubMed] [Google Scholar]
- 22. Randelli P, Compagnoni R, Aliprandi A, et al. Long-term degradation of poly-lactic co-glycolide/β-tricalcium phosphate biocomposite anchors in arthroscopic Bankart repair: a prospective study. Arthroscopy. 2014;30:165–171. [DOI] [PubMed] [Google Scholar]
- 23. Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60:1–16. [PubMed] [Google Scholar]
- 24. Stein DA, Jazrawi L, Bartolozzi AR. Arthroscopic stabilization of anterior shoulder instability: a review of the literature. Arthroscopy. 2002;18:912–924. [DOI] [PubMed] [Google Scholar]
- 25. Take Y, Yoneda M, Hayashida K, Nakagawa S, Mizuno N. Enlargement of drill holes after use of a biodegradable suture anchor: quantitative study on consecutive postoperative radiographs. Arthroscopy. 2008;24:251–257. [DOI] [PubMed] [Google Scholar]
- 26. Takubo Y, Morihara T, Namura T, et al. Anchor hole enlargement after arthroscopic Bankart repair using resorbable suture anchors: a report of three cases. J Shoulder Elbow Surg. 2008;17:e16–e18. [DOI] [PubMed] [Google Scholar]
- 27. Vainionpää S. Biodegradation of polyglycolic acid in bone tissue: an experimental study on rabbits. Arch Orthop Trauma Surg. 1986;104:333–338. [DOI] [PubMed] [Google Scholar]
- 28. Weiler A, Helling HJ, Kirch U, Zirbes TK, Rehm KE. Foreign-body reaction and the course of osteolysis after polyglycolide implants for fracture fixation: experimental study in sheep. J Bone Joint Surg Br. 1996;78:369–376. [PubMed] [Google Scholar]
- 29. Weiler A, Hoffmann RF, Stähelin AC, Helling HJ, Südkamp NP. Biodegradable implants in sports medicine: the biological base. Arthroscopy. 2000;16:305–321. [DOI] [PubMed] [Google Scholar]
- 30. Weiler A, Windhagen HJ, Raschke MJ, Laumeyer A, Hoffmann RFG. Biodegradable interference screw fixation exhibits pull-out force and stiffness similar to titanium screws. Am J Sports Med. 1998;26:119–128. [DOI] [PubMed] [Google Scholar]
- 31. Witney-Lagen C, Perera N, Rubin S, Venkateswaran B. Fewer anchors achieves successful arthroscopic shoulder stabilization surgery: 114 patients with 4 years of follow-up. J Shoulder Elbow Surg. 2014;23:382–387. [DOI] [PubMed] [Google Scholar]