Abstract
Background
Valid comparison of outcomes after surgical procedures requires consensus on which instruments and parameters should be used, including the recording and evaluation of surgical complications. An international standard outlining the terminology and definitions of surgical complications in orthopaedics is lacking.
Purpose
This study systematically reviewed the literature for terms and definitions related to the occurrence of negative events or complications after arthroscopic rotator cuff repair (ARCR) with specific focus on shoulder stiffness.
Study Design
Systematic review; Level of evidence, 4.
Methods
PubMed, EMBASE, Cochrane Library, and Scopus databases were searched for reviews, clinical studies, and case reports of complications associated with ARCR. Reference lists of selected articles were also screened. The terminology of complications and their definitions were extracted from all relevant original articles by a single reviewer and verified by a second reviewer. Definitions of shoulder stiffness or equivalent terms were tabulated.
Results
Of 654 references published after 2007 and obtained from the search, 233 full-text papers (44 reviews, 155 studies, 31 case reports, and 3 surgical technique presentations) were reviewed. Twenty-two additional references cited for a definition were checked. One report defined the term surgical complication. There were 242 different terms used to describe local events and 64 to describe nonlocal events. Furthermore, 16 definitions of terms such as frozen shoulder, shoulder stiffness, or stiff painful shoulder were identified. Diagnosis criteria for shoulder stiffness differed widely; 12 various definitions for restriction in range of motion were noted. One definition included a gradation of stiffness severity, whereas another considered the patient’s subjective assessment of motion.
Conclusion
The literature does not consistently report on complications after ARCR, making valid comparison of the incidence of these events among published reports impossible. Specifically, the variation in criteria used to diagnose shoulder stiffness is problematic for valid and accurate reporting of this event. A standard for reporting this event and other complications after ARCR is needed.
Clinical Relevance
This review serves as the basis for the development of a uniform documentation process for shoulder stiffness and the standardization of complication definitions in ARCR following international consensus.
Keywords: shoulder, rotator cuff, shoulder stiffness, complications, standardization
In surgery, the recording of complications is used to critically analyze the quality of health care.52 Complication management is an essential part of clinical routine and quality control. Outlining the risk-benefit profiles of specific surgical interventions, together with acknowledging patient preferences, is fundamental in the shared decision-making process between surgeon and patient. Adequate and accurate reporting of harms is therefore essential.20 Valid comparison of the outcomes after surgical procedures requires consensus on which clinical parameters and outcome instruments should be used,12 including the recording and evaluation of surgical complications.
There is a lack of consensus on what actually constitutes a complication, which allows clinicians and researchers to create definitions to suit their purpose. In general surgery, Martin et al29 found that a definition of at least 1 complication was provided in only 34% of 119 studies, and a severity grading in only 20%. In addition, multiple definitions for specific events were identified. A similar observation was made in orthopaedics, with only 8 of 112 trials (7%) defining at least 1 complication,13 leading to a proposal as to how complications could be systematically documented in clinical studies.1 Only few initiatives have supported the standardization of surgical complications in orthopaedics such as in an orthopaedic clinic27 or, more specifically, regarding the repair of distal radius fractures,31 knee arthroplasty,17 or spine surgery.32
Rotator cuff tears are a common clinical problem with multifactorial etiology combining age-related degenerative changes and trauma.48 Approximately 25% of individuals show full-thickness rotator cuff tears in their 60s, and this proportion increases to 50% after 80 years of age. Symptomatic tears are a source of significant morbidity. Their surgical treatment developed markedly in recent years with a significant change toward using arthroscopic procedures.55 A number of systematic reviews summarized the patient outcomes after arthroscopic rotator cuff repair (ARCR) yet did not outline any complication events or consider the variability in recording methodology.4,10,41,45,46 Strauss et al46 found postoperative complication rates ranging from 2.5% to 11.9% that were derived from 4 of 16 studies; a clear definition of this parameter was not provided. A more recent literature review found shoulder stiffness to be a commonly reported complication after ARCR, with rates ranging from 1.5% to 11.1%.39 This wide range is likely associated with not only differences in patient risk profiles but also a lack of common understanding of how shoulder stiffness should be defined and recorded.
We established a process toward the development of an international standard for the documentation of surgical complications after ARCR. As an initial step, the objective of this systematic review was to search the literature for terms and definitions used for these negative events. Detailed results regarding shoulder stiffness are presented and discussed.
Methods
Database Search
A systematic literature search was conducted by a qualified librarian to target all scientific publications related to ARCR in humans, with special focus on the reporting of adverse events and complications. Keywords for the main search were identified through PubMed PubReMiner version 1.1325 using the following search query: (“ROTATOR CUFF” AND (TEAR* OR REPAIR OR SURGERY)) AND (ARTHROSCOP*) AND (“COMPLICATIONS” OR “ADVERSE EFFECTS” OR “ADVERSE EVENTS”). The literature databases PubMed, EMBASE, Cochrane Library, and Scopus were searched using more elaborate and database-specific search strategies without language or time restriction. An initial search was conducted on February 4, 2013, and updated using the same strategy on November 21, 2013.
Article Selection
The first author (L.A.) screened the reference titles and abstracts published after 2007 to identify human clinical studies, reviews, or educational papers; classify the type of study; and document reported adverse events or complications as well as make a preliminary selection for full-paper review. Selected references were systematic reviews, analyses of register data, clinical investigations (eg, randomized controlled trials, cohort studies, case series), as well as other references (eg, narrative reviews, technical papers, health economic analyses, or case reports) mentioning complications in the abstract. Only reports in English or German were considered. A second author checked and supported the selection of initially chosen references as well as some for which uncertainty remained regarding their relevance. References were excluded when only an abstract was published. Finally, the reference lists of all reviewed articles were screened for additional references that were clearly focused on surgical complications after ARCR; in particular, the full articles of all references quoted for specific complication definitions were retrieved to confirm the correctness of the provided definitions.
Data Extraction From Full Articles
One author (R.B.) searched full articles for information pertaining to the terminology of surgical complications and their definition. The following information was extracted from each article: the journal and year of publication, the publication type (systematic/narrative review, clinical investigations, case report on complications, technical paper), any general definition of a surgical complication and any definition of a specific complication event as well as associated references (if any), all terms used to name adverse events and/or complications, and any additional relevant articles identified from reference lists. Review data were collected and managed using REDCap (Vanderbilt University) electronic data capture tools.15 The first author (L.A.) monitored the data collection for correctness and completeness.
Data Analysis
Data analyses were implemented using Stata version 13 (StataCorp LP). Reviewed articles were described by type and reporting of definitions. Complication terms were counted, grouped, and distinguished as either local (affecting the operated shoulder) or nonlocal (affecting the rest of the body) to facilitate the identification of synonyms. Extracted definitions were tabulated and compared according to similar event types.
Results
Article Selection
The initial database search resulted in a pool of 1348 references (Figure 1). After the exclusion of articles published before 2008, the titles and abstracts (if available) of 654 references were screened for eligibility leading to 412 exclusions, including 31 duplicates. An additional 23 references were excluded because 12 full reports did not meet the eligibility criteria, and only abstracts were available for the other 11 publications. Data were extracted from 219 full articles as well as 36 articles identified from reference lists—22 of which were quoted in relation to a complication definition.
Figure 1.
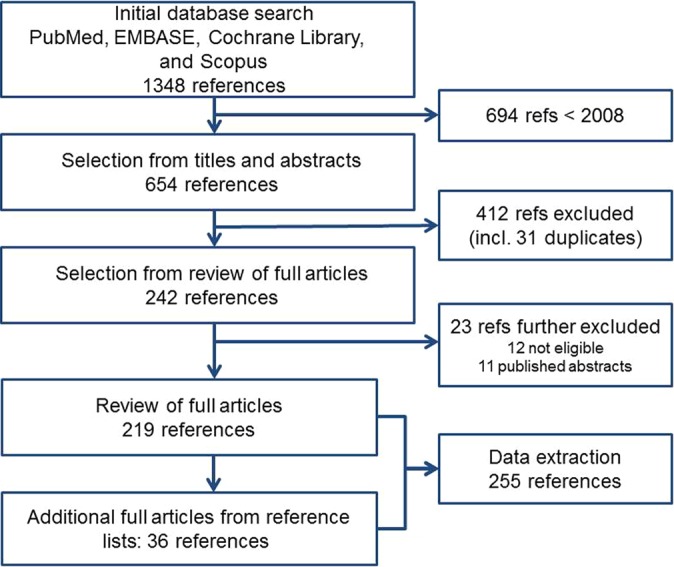
Flowchart of the literature screening and selection process.
Description of Included Articles
Of the 255 reviewed articles, 142 (56%) were published in 1 of the 4 major orthopaedic journals: Arthroscopy, The American Journal of Sports Medicine, The Journal of Shoulder and Elbow Surgery, and The Journal of Bone and Joint Surgery (American edition). The majority of articles were clinical investigations (67%) (Table 1).
TABLE 1.
Distribution of Reviewed Articles by Typea
| Type of Article | n (%) |
|---|---|
| Reviews | 44 (19) |
| Clinical guidelines | 3 |
| Systematic review | 19 |
| Review (narrative) | 22 |
| Clinical investigations | 155 (67) |
| Randomized controlled trial | 38 |
| Prospective cohort study | 12 |
| Ambidirectional cohort study | 5 |
| Prospective series | 28 |
| Ambidirectional series | 15 |
| Register | 16 |
| Before-after study | 1 |
| Retrospective cohort | 8 |
| Retrospective series | 31 |
| Cross-sectional study | 1 |
| Case report/letter (complication) | 31 (13) |
| Surgical techniques | 3 (1) |
| Total | 233 |
aThere were 22 additional articles (selected because they were quoted in relation to a definition of complication) not included in this table.
Definitions of Surgical Complication and Complication Events
A single article was identified that provided a global definition of the term complication as a “postoperative event or condition that requires additional treatment, either nonoperative or operative.”5
A total of 242 specific local event terms (including 17 terms in German) were identified, and 64 terms described nonlocal events. The majority of these terms were not defined.
Definitions of Shoulder Stiffness
There were 16 definitions for terms such as frozen shoulder, shoulder stiffness, or stiff painful shoulder (referred to only as “shoulder stiffness” throughout the remainder of this article, excluding citations) (Table 2). The majority (12/16) of these definitions described restrictions in specific ranges of motion as diagnostic criteria, which occurred either in a single direction or in any direction (Table 3). One definition was identified in the book chapter of Matsen et al30 on shoulder motion and another was from a systematic review,36 although the latter was attributed to the work of Tauro.49 Papalia and coworkers36 presented some of the definitions identified in our review. Five definitions were proposed in the context of complication reporting,5,9,28,37,38 and another 5 as diagnostic criteria for preoperative stiffness concurrent to rotator cuff tears.18,23,34,42,44 The remaining 4 definitions were unspecific, although related to restriction in shoulder motion.6,16,19,56 Huberty et al19 relied on patient dissatisfaction with shoulder motion to define shoulder stiffness, and Bunker6 presented shoulder stiffness as a morbidity that may result from local shoulder surgery. Threshold angle values to specify restrictions in shoulder motion differed (Table 3). Restricted forward flexion was used in 9 definitions and ranged from <90° to <120°. Restriction in abduction was set at 90° or 100° for 3 definitions. Restriction in external rotation was set at either less than 25° to 45° or less than 50% compared with the contralateral side for 8 definitions. Five definitions described restricted internal rotation as up to and including the sacral level, below L3, the second sacral vertebral level, or 45° (ie, ≥50% loss of passive normal motion of 90°). The total range of motion deficit was considered in 2 definitions: (1) shoulder stiffness was defined with a threshold of 270° or (2) reported as a grading system to characterize stiffness severity.
TABLE 2.
Extracted Definitions of Frozen Shoulder or Shoulder Stiffnessa
| Year | Original Reference | Term Used | Definition/Diagnosis Criteria | Cited By | Adapted From |
|---|---|---|---|---|---|
| 1992 | Shaffer et al44 | Frozen shoulder | (1) Minimum 1-month history of shoulder pain and stiffness for which no other cause could be identified and (2) documented restriction of passive glenohumeral and scapulothoracic motion of ≤100° abduction and <50% external rotation as compared with the motion of the contralateral shoulder or with sex- and age-matched control values. | Ko et al23b (term: shoulder stiffness) | Murray et al33 |
| 1993 | Zuckerman and Cuomo56 | Frozen shoulder | A condition of uncertain etiology characterized by significant restriction of both active and passive shoulder motion that occurs in the absence of a known intrinsic shoulder disorder. | Harryman and Lazarus16b | |
| 1994 | Matsen et al30 | Frozen shoulder/postsurgical stiff shoulder | Functionally significant restriction of shoulder motion with limited glenohumeral motion. Normal joint space and normal joint relationships on radiographs. Frozen shoulder: Absence of pathologic changes other than osteopenia. Limited glenohumeral motion in all directions. Postsurgical stiff shoulder: History of significant shoulder injury or surgery. Humeroscapular elevation of <90° indicates stiffness, especially if it is less than the contralateral normal shoulder. | ||
| 1997 | Mansat et al28 | Frozen shoulder | Passive elevation of <120° after 6 months of follow-up. | ||
| 2004 | Harryman and Lazarus16 | Frozen shoulder/posttraumatic stiff shoulder | Frozen shoulder: An idiopathic global limitation of humeroscapular motion resulting from contracture and loss of compliance of the glenohumeral joint capsule. Posttraumatic stiff shoulder: A limitation in humeroscapular motion occurring after an injury or low-level repetitive trauma or as part of an accompanying condition that results in a contracture of structures participating in the glenohumeral or humeroscapular motion interfaces. | Zuckerman and Cuomo56 Matsen et al30 | |
| 2007 | Brislin et al5 | Shoulder stiffness | One of the following deficits persisted for 90 days postoperatively: (1) total passive external rotation with the arm at the side of <10°, (2) total passive external rotation with the arm in 90° abduction of <30°, or (3) total passive forward flexion of <100°. | Parsons et al37b Papalia et al36c | |
| 2007 | Hsu et al18 | Shoulder stiffness | Active and passive limitation of motion of ≥half the normal range for at least 3 months. The ranges of motion were flexion ≤90°, abduction ≤90°, external rotation ≤25°, and internal rotation ≤sacral level. | Papalia et al36b, d | |
| 2008 | Ko et al23e | Shoulder stiffness | ≥50% loss of passive ROM for at least 3 months with normal ROM considered to be 180° forward flexion, 180° abduction, 90° external rotation, and 90° internal rotation. ROM deficit measurements are added together to determine the sum of ROM deficit. Patients are defined as having shoulder stiffness if the sum of ROM deficit ≥270°. | Ko and Wang22b,f | Shaffer et al44 Harryman and Lazarus16 |
| 2008 | Oh et al34 | Shoulder stiffness | Any one of the following 3 criteria is present: (1) forward elevation at <120°, (2) external rotation with the arm at the side at <30°, or (3) internal rotation at the back as lower than L3. | Chung et al8 c Chung et al7 c | |
| 2009 | Coghlan et al9 | Postoperative stiff painful shoulder | Presence of symptoms of shoulder pain and stiffness and restriction of movement of ≥30° in ≥2 planes. | ||
| 2009 | Huberty et al19 | Stiffness | Patients’ dissatisfaction with their range of motion. | Koo et al24 c | |
| 2010 | Parsons et al37 | Shoulder stiffness | Passive forward elevation <100° and passive external rotation <30°. | Papalia et al36 c | Brislin et al5 |
| 2011 | Bunker6 | Frozen shoulder | Frozen shoulder is a contracture of the shoulder joint capsule. It appears maximal in the rotator interval area, particularly around the coracohumeral ligament.g | ||
| 2012 | Seo et al42 | Shoulder stiffness | Restriction of active and passive motion of 100° of elevation or less, <50% of external rotation as compared with the motion of the contralateral shoulder, and internal rotation only to the sacrum. | Papalia et al36 c | |
| 2012 | Papalia et al36 h | Shoulder stiffness | Total passive ROM deficit (abduction, forward flexion, external rotation and internal rotation added together): 0°-20° = mild stiffness, 25°-70° = moderate stiffness, and >70° = severe stiffness. | Tauro49 | |
| 2012 | Peters et al38 | Shoulder stiffness | Forward flexion <110°, external rotation with the arm at the side <25°, or internal rotation below the second sacral vertebral level. | Brislin et al5 Oh et al34 |
aROM, range of motion.
bAdapted their own definition, as presented in this table.
cDid not change the quoted definition.
eKo et al23 presented their own definition of shoulder stiffness while citing Ozaki et al,35 Harryman and Lazarus (2nd edition),16 and Shaffer et al44; however, the closest original definition was presented by Shaffer et al.44
fKo and Wang22 did not include a duration of at least 3 months in their definition.
gFrozen shoulder is well explained in this article but not as an adverse event or complication of the arthroscopic repair of the rotator cuff: “Surgery may be another initiating factor, for instance breast surgery. It had been thought that it was the immobilization that led to the development of the frozen shoulder, but you will see, as our story unravels, it is more likely the molecular response to the injury or surgery that is responsible.”6(p12)
TABLE 3.
Summary of Diagnosis Criteria Used for Frozen Shoulder or Shoulder Stiffnessa
| Reference | Symptom Duration | Condition | Restriction of Passive Motion | TROMD | |||
|---|---|---|---|---|---|---|---|
| FE | Abd | ER | IR | ||||
| Zuckerman and Cuomo56 | — | Significant restriction of both active and passive shoulder motion | |||||
| Harryman and Lazarus16 | — | Limitation of humeroscapular motion | |||||
| Huberty et al19 | — | Patient dissatisfaction with their ROM | |||||
| Bunker6 | — | Frozen shoulder is a contracture of the shoulder joint capsule | |||||
| Shaffer et al44 | 1 mo | All restrictions | ≤100° | <50% contralateral/normal | |||
| Matsen et al30 | — | <90° | |||||
| Mansat et al28 | b | <120° | |||||
| Brislin et al5 | 90 d | Any restriction | <100° | <10°/30°c | |||
| Hsu et al18 | 3 mo | <50% normal in all | ≤90° | ≤90° | ≤25° | ≤Sacral level | |
| Ko et al23 | 3 mo | ≥50% loss | 180°d | 180°d | 90°d | 90°d | ≥270°d |
| Oh et al34 | — | Any restriction | <120° | <30° (arm at the side) | <L3 | ||
| Coghlan et al9 | — | Pain + restriction ≥30° in at least 2 planes | |||||
| Parsons et al37 | — | All restrictions passively | <100° | <30° | |||
| Seo et al42 | — | Any restriction | ≤100° | <50% contralateral | ≤Sacral level | ||
| Papalia et al36 | — | 0°-20°/ 25°-70°/ >70°e | |||||
| Peters et al38 | — | Any restriction | <110° | <25° (arm at the side) | <2nd sacral vertebral level | ||
aAbd, abduction; ER, external rotation; FE, flexion elevation; IR, internal rotation; ROM, range of motion; TROMD, total range of motion deficit (ie, abduction, forward flexion, external rotation, and internal rotation added together).
bStiffness was also defined as documented at a 6-month examination time point.
c<10° with the arm at the side, <30° with the arm in 90° of abduction.
dNormal range of motion values.
e0° to 20° = mild stiffness; 25° to 70° = moderate stiffness; and >70° = severe stiffness.
Four definitions of shoulder stiffness also considered 1- and 3-month duration periods of the symptoms as diagnosis criteria (Table 3). Coghlan et al9 defined shoulder stiffness when shoulder pain occurred together with a restriction of 30° or more in at least 2 planes.9
Discussion
The present systematic review was implemented to investigate the terminology and definitions related to the occurrence of adverse events and complications following ARCR. This is the first step toward developing a consensus core set of negative events to be documented in routine practice and clinical registers using accepted methodology.54 Such a standard has been developed in several surgical fields,21,50 including spine surgery,32 yet none truly existed for orthopaedic interventions associated with the upper extremity despite an attempt for distal radius fractures.31 While many event definitions would be valid across disciplines (eg, general or systemic events) or interventions on the same body locations (eg, events affecting the shoulder), some events are expected to remain specific to the targeted indication(s) and/or surgical procedure(s). With the establishment of a local clinical register for ARCR,11 the need to develop a relevant and valid system to record negative events became obvious.
Only 1 article provided a general definition of “complication” without referring to a specific event,5 which illustrates the lack of standardization and transparency in the documentation and reporting of these events. Rather than defining complications, various authors categorized these events as medical versus surgical, minor versus major, and early versus late complications.26,28,53 While the timing of the occurrence of adverse events needs to be considered for defining complications, assigning them according to typology, severity, or causality is an issue of classification as well as judgment and not of overall definition. Defining what constitutes a complication after surgery is needed; however, addressing this major challenge was not the main purpose of this project and would require adopting a broader perspective within the surgical field.21,32,50
Of the 242 different terms used to report specific local complications, 16 definitions were identified for the terms frozen shoulder, shoulder stiffness, or stiff painful shoulder, which represent a similar shoulder morbidity. Shoulder stiffness is a commonly recognized morbidity associated with ARCR, which was cited in each of a total of 85 articles from our review. Of these 85 articles, 15 specifically focused on describing the etiology, pathology, or evaluating therapeutic interventions of shoulder stiffness.
Shoulder stiffness negatively affects surgical outcomes, and if left untreated, can lead to substantial morbidity, and thus, failure of surgical management. Several factors that predispose a patient to the development of shoulder stiffness include the following: limited preoperative motion, type and severity of the rotator cuff tear, dominant extremity, age less than 50 years, single-tendon repair, and workers’ compensation insurance.36 Studies report rates of stiffness ranging from 4.9% to 32.7%.19 Considering the 6 primary studies that provided a definition for postoperative shoulder stiffness, occurrence rates lie between 2.6% and 23.3% (Table 4), which may be at least partly related to a definition problem regarding this pathology as well as a variation in the considered time period of observation after surgery.
TABLE 4.
Reported Occurrence of Postoperative Shoulder Stiffness From Primary Reports Providing a Definition for the Condition
| Reference | Study Type | Patients (Shoulders) | Stiffness | Risk, % | Time Point |
|---|---|---|---|---|---|
| Huberty et al19 | Local register | 489 | 24 | 4.9 | 4-19 mo (median, 8 mo) |
| Mansat et al28 | Case series | 116 | 3 | 2.6 | 6 mo |
| Brislin et al5 | Local register | 263 | 23 | 8.7 | 3 mo (90 d) |
| Coghlan et al9 | Randomized controlled triala | 70 | 13 | 18.6 | 4 mo |
| Parsons et al37 | Case series | 43 | 10 | 23.3 | 1.5-2.0 mo (6-8 wk) |
| Peters et al38 | Cohort study | 169 | Not availableb | 14-15 | 6 mo |
aIn 1 cohort, patients were treated with decompression and rotator cuff tear repair and allocated to perioperative pain management with ropivacaine or placebo.
bThese authors reported only percentages: “Examiner-determined postoperative stiffness at six weeks was common in both groups (50% in the partial-thickness group and 47% in the full-thickness group) but decreased in both groups to 21% and 19%, respectively, at three months and to 15% and 14% at six months.”38(p1081)
As demonstrated in our study, multiple terms are used to describe shoulder stiffness such as painful stiffness, stiff painful shoulder, postoperative frozen shoulder, and secondary frozen shoulder. The terms adhesive capsulitis, arthrofibrosis, and capsular synovitis are related to frozen shoulder, which was first described in 1934 as “a fairly distinct clinical entity” developing slowly without association with trauma or surgery.6 A recent consensus definition of frozen shoulder distinguished between primary (idiopathic) and secondary frozen shoulder, the latter being further classified as intrinsic, extrinsic, or systemic depending on the identified etiology or associated condition.57 Surgery is not considered a possible intrinsic etiological factor in this definition, which in fact, was not developed in the context of the occurrence of postoperative negative events. While the terms shoulder stiffness and frozen shoulder are used interchangeably to name a similar event, this event must occur postoperatively to be considered a surgical complication. The terms postoperative frozen shoulder and secondary frozen shoulder are therefore not synonyms. Postoperative shoulder stiffness and primary adhesive capsulitis (frozen shoulder) share morphology and clinical presentation. In both conditions, there is a contracture of the glenohumeral joint capsule and ligaments that results in a restriction in shoulder range of motion; these conditions are nonetheless triggered by different mechanisms. While primary frozen shoulder is an inflammatory process of still unknown etiology,47 shoulder stiffness is more related to scarring triggered by the surgical intervention and postoperative immobilization. In contrast to primary frozen shoulder, postoperative shoulder stiffness may be regarded as a surgical sequel to a certain extent and should be considered pathologic only if it increases in intensity over a given threshold or persists over a certain period of time. In search for a definition, it should be noted that this pathology is not, in fact, a dichotomous state (presence or absence) but can be represented on a continuum scale. Interestingly, the consensus definition of frozen shoulder proposed by Zuckerman and Rokito57 does not include a quantification of the sufficient functional restrictions of shoulder motion to support an objective diagnosis of the condition.
We identified 16 definitions for events related to shoulder stiffness in the context of negative events after ARCR. These definitions were not developed or proposed in isolation; for example, the definition of Peters et al38 was chosen on the basis of criteria from 2 other reports.5,34 Most authors attempted to objectively define shoulder stiffness. The criteria for shoulder stiffness mostly included restrictions in range of motion either in absolute terms or relative to contralateral or normal ranges. Some authors were guided by clinical experience to identify most relevant motion arcs.37 The sources from which the normal ranges were taken were not mentioned, yet published values reflect great variability within healthy populations, notably related to sex, age, and side dominance.2,14,40,51 Hence, consideration of uniform threshold range values for any patient is likely to misclassify shoulder status with regard to the occurrence of shoulder stiffness. Comparison with the contralateral shoulder is also problematic when this shoulder is not healthy and cannot be used as a reference. The concept of total range of motion deficit (TROMD) is interesting because it reflects the fact that motion restrictions may be better assessed using a global perspective without considering specific motion arcs only.23,36 Yet a gradation of stiffness intensity as applied by the group of Papalia,36 although with somewhat arbitrarily defined categories, offers a clinically relevant perspective to document stiffness on a continuum scale. Timing is a relevant issue that adds another dimension to defining shoulder stiffness. Four articles considered that symptoms of stiffness or frozen shoulder should last for 1 month44 to 3 months,5,18,23 and another would not diagnose stiffness before 6 months postsurgery.28 Examiner-determined 6-week postoperative stiffness as defined and reported by Peters et al38 was common in 47% to 50% of patients but decreased to 19% to 21% and 14% to 15% by the 3- and 6-month postoperative periods, respectively. To our knowledge, there is no consensus on the time point at which shoulder stiffness can be regarded as abnormal in the post-ARCR rehabilitation period. In the case of preoperative limited range of motion, the definition of an absolute time point may be even more complex. It is interesting to note that pain was included in only 1 definition, although no threshold level was considered9; hence, we can only assume that pain would need to be reported by the patient as bothersome. In effect, postoperative shoulder stiffness may not be associated with pain during rest,30 which almost systematically characterizes the occurrence of idiopathic frozen shoulder.6
There is no gold standard diagnostic process for shoulder stiffness, so in the context of surgical complications after ARCR, the patient perspective (as proposed by Huberty et al19) may be of value. Patient-reported outcomes are increasingly important in the evaluation of surgical interventions. A patient’s assessment of the intensity of restrictions in shoulder motion may be more relevant in defining stiffness than any objective measurements performed by clinicians. Ultimately, the postoperative change in magnitude of shoulder stiffness from baseline preoperative motion status, as perceived by the patient, may determine the occurrence of stiffness as a surgical complication. Many rotator cuff tears show some preoperative shoulder stiffness,43 which may explain why stiffness may not always be seen as a complication by all authors.3
This review has limitations. We restricted the search to a defined time period, and cannot exclude that additional event terms and definitions could have been identified from earlier reports. Our search criteria and literature databases, however, were broad enough to identify any reporting standard existing in the field of ARCR; the likelihood of having missed such information is small. The article selection and data extraction processes were each performed by separate reviewers, yet checked by only 1 of the authors. Extracted terms were checked for their relevance in describing negative events, but we cannot exclude that some relevant terms remain unidentified from the full reports. Finally, our focus on negative events following ARCR may have led to the exclusion of some definitions for similar events or conditions, which may occur in another medical context such as the consensus definition of frozen shoulder.57 This particular definition was not identified and quoted by any author considered in our review. A supplementary literature search would be worth conducting when considering the definition of specific negative events or pathological conditions.
Conclusion
The literature does not consistently report on surgical complications after ARCR, making valid comparison of the incidence of complications after ARCR impossible. When reporting on specific events such as shoulder stiffness, exact definitions are lacking. Until definition standards emerge in orthopaedics, authors should define what they understand as complications or which events were documented. The variation in diagnostic criteria used to diagnose shoulder stiffness is especially problematic for a valid and accurate reporting of this negative event. The patient’s perspective may be considered in any standard definition. In general, and also considering the example of the shoulder stiffness in particular, this systematic review highlights that a standard in the definition of surgical complications after ARCR is needed. The complication terminology and definitions extracted from the literature serve as the basis for defining such standard that should ideally emerge from an international expert consensus process.
Acknowledgment
The authors acknowledge the support of Dr Martina Gosteli, medical librarian at the University of Zurich, Zurich, Switzerland, for implementing the final literature database search. Dr Melissa Wilhelmi, medical writer at the Schulthess Clinic, Zurich, Switzerland, is greatly thanked for English editing the manuscript and supporting the submission process.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Audigé L, Goldhahn S, Daigl M, Goldhahn J, Blauth M, Hanson B. How to document and report orthopedic complications in clinical studies? A proposal for standardization. Arch Orthop Trauma Surg. 2014;134:269–275. [DOI] [PubMed] [Google Scholar]
- 2. Barnes CJ, Van Steyn SJ, Fischer RA. The effects of age, sex, and shoulder dominance on range of motion of the shoulder. J Shoulder Elbow Surg. 2001;10:242–246. [DOI] [PubMed] [Google Scholar]
- 3. Berjano P, Gonzalez BG, Olmedo JF, Perez-España LA, Munilla MG. Complications in arthroscopic shoulder surgery. Arthroscopy. 1998;14:785–788. [DOI] [PubMed] [Google Scholar]
- 4. Bollier M, Shea K. Systematic review: what surgical technique provides the best outcome for symptomatic partial articular-sided rotator cuff tears? Iowa Orthop J. 2012;32:164–172. [PMC free article] [PubMed] [Google Scholar]
- 5. Brislin KJ, Field LD, Savoie FH., 3rd Complications after arthroscopic rotator cuff repair. Arthroscopy. 2007;23:124–128. [DOI] [PubMed] [Google Scholar]
- 6. Bunker T. Frozen shoulder. Orthop Trauma. 2011;25:11–18. [Google Scholar]
- 7. Chung SW, Huong CB, Kim SH, Oh JH. Shoulder stiffness after rotator cuff repair: risk factors and influence on outcome. Arthroscopy. 2013;29:290–300. [DOI] [PubMed] [Google Scholar]
- 8. Chung SW, Kim JY, Kim MH, Kim SH, Oh JH. Arthroscopic repair of massive rotator cuff tears: outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med. 2013;41:1674–1683. [DOI] [PubMed] [Google Scholar]
- 9. Coghlan JA, Forbes A, McKenzie D, Bell SN, Buchbinder R. Efficacy of subacromial ropivacaine infusion for rotator cuff surgery. A randomized trial. J Bone Joint Surg Am. 2009;91:1558–1567. [DOI] [PubMed] [Google Scholar]
- 10. DeHaan AM, Axelrad TW, Kaye E, Silvestri L, Puskas B, Foster TE. Does double-row rotator cuff repair improve functional outcome of patients compared with single-row technique? A systematic review. Am J Sports Med. 2012;40:1176–1185. [DOI] [PubMed] [Google Scholar]
- 11. Flury M, Kolling C, Grobet C, Kunz SN, Audige L. Implementation of a local outcome register for arthroscopic rotator cuff tear repair. Obere Extremität. 2015;10:33–40. [Google Scholar]
- 12. Gargon E, Gurung B, Medley N, et al. Choosing important health outcomes for comparative effectiveness research: a systematic review. PLoS One. 2014;9:e99111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Goldhahn S, Sawaguchi T, Audigé L, et al. Complication reporting in orthopaedic trials. A systematic review of randomized controlled trials. J Bone Joint Surg Am. 2009;91:1847–1853. [DOI] [PubMed] [Google Scholar]
- 14. Gunal I, Köse N, Erdogan O, Göktürk E, Seber S. Normal range of motion of the joints of the upper extremity in male subjects, with special reference to side. J Bone Joint Surg Am. 1996;78:1401–1404. [DOI] [PubMed] [Google Scholar]
- 15. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harryman DT, II, Lazarus MD. The stiff shoulder In: Rockwood CA, Jr, Matsen FA, III, Wirth MA, Lippitt SB, eds. The Shoulder. 3rd ed Philadelphia: WB Saunders; 2004:1121–1172. [Google Scholar]
- 17. Healy WL, Della Valle CJ, Iorio R, et al. Complications of total knee arthroplasty: standardized list and definitions of the Knee Society. Clin Orthop Relat Res. 2013;471:215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hsu SL, Ko JY, Chen SH, Wu RW, Chou WY, Wang CJ. Surgical results in rotator cuff tears with shoulder stiffness. J Formos Med Assoc. 2007;106:452–461. [DOI] [PubMed] [Google Scholar]
- 19. Huberty DP, Schoolfield JD, Brady PC, Vadala AP, Arrigoni P, Burkhart SS. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy. 2009;25:880–890. [DOI] [PubMed] [Google Scholar]
- 20. Ioannidis JP, Evans SJ, Gotzsche PC, et al. ; CONSORT Group. Better reporting of harms in randomized trials: an extension of the CONSORT statement. Ann Intern Med. 2004;141:781–788. [DOI] [PubMed] [Google Scholar]
- 21. Jacobs JP, Benavidez OJ, Bacha EA, Walters HL, Jacobs ML. The nomenclature of safety and quality of care for patients with congenital cardiac disease: a report of the Society of Thoracic Surgeons Congenital Database Taskforce Subcommittee on Patient Safety. Cardiol Young. 2008;18(suppl 2):81–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ko JY, Wang FS. Rotator cuff lesions with shoulder stiffness: updated pathomechanisms and management. Chang Gung Med J. 2011;34:331–340. [PubMed] [Google Scholar]
- 23. Ko JY, Wang FS, Huang HY, Wang CJ, Tseng SL, Hsu C. Increased IL-1β expression and myofibroblast recruitment in subacromial bursa is associated with rotator cuff lesions with shoulder stiffness. J Orthop Res. 2008;26:1090–1097. [DOI] [PubMed] [Google Scholar]
- 24. Koo SS, Parsley BK, Burkhart SS, Schoolfield JD. Reduction of postoperative stiffness after arthroscopic rotator cuff repair: results of a customized physical therapy regimen based on risk factors for stiffness. Arthroscopy. 2011;27:155–160. [DOI] [PubMed] [Google Scholar]
- 25. Koster J. PubReMiner. http://hgserver2.amc.nl/cgi-bin/miner/miner2.cgi. Accessed March 21, 2014.
- 26. Koulouvaris P, Lyman S, Marx RG. Complications of rotator cuff repair. Minerva Orthop Traumatol. 2007;58:137–141. [Google Scholar]
- 27. Kramer KL, Clauss M. Nomenclature and classification of complications. Standard procedure at the Heidelberg University Orthopedic Clinic [in German]. Orthopade. 1999;28:299–311. [PubMed] [Google Scholar]
- 28. Mansat P, Cofield RH, Kersten TE, Rowland CM. Complications of rotator cuff repair. Orthop Clin North Am. 1997;28:205–213. [DOI] [PubMed] [Google Scholar]
- 29. Martin RC, 2nd, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg. 2002;235:803–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Matsen FA, Lippitt SB, Sidles JA, Harryman DT. Shoulder Motion: Practical Evaluation and Management of the Shoulder. Philadelphia: WB Saunders; 1994:19–109. [Google Scholar]
- 31. McKay SD, MacDermid JC, Roth JH, Richards RS. Assessment of complications of distal radius fractures and development of a complication checklist. J Hand Surg Am. 2001;26:916–922. [DOI] [PubMed] [Google Scholar]
- 32. Mirza SK, Deyo RA, Heagerty PJ, Turner JA, Lee LA, Goodkin R. Towards standardized measurement of adverse events in spine surgery: conceptual model and pilot evaluation. BMC Musculoskelet Disord. 2006;7:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Murray MP, Gore DR, Gardner GM, Mollinger LA. Shoulder motion and muscle strength of normal men and women in two age groups. Clin Orthop Relat Res. 1985;192:268–273. [PubMed] [Google Scholar]
- 34. Oh JH, Kim SH, Lee HK, Jo KH, Bin SW, Gong HS. Moderate preoperative shoulder stiffness does not alter the clinical outcome of rotator cuff repair with arthroscopic release and manipulation. Arthroscopy. 2008;24:983–991. [DOI] [PubMed] [Google Scholar]
- 35. Ozaki J, Nakagawa Y, Sakurai G, Tamai S. Recalcitrant chronic adhesive capsulitis of the shoulder. Role of contracture of the coracohumeral ligament and rotator interval in pathogenesis and treatment. J Bone Joint Surg Am. 1989;71:1511–1515. [PubMed] [Google Scholar]
- 36. Papalia R, Franceschi F, Vasta S, Gallo A, Maffulli N, Denaro V. Shoulder stiffness and rotator cuff repair. Br Med Bull. 2012;104:163–174. [DOI] [PubMed] [Google Scholar]
- 37. Parsons BO, Gruson KI, Chen DD, Harrison AK, Gladstone J, Flatow EL. Does slower rehabilitation after arthroscopic rotator cuff repair lead to long-term stiffness? J Shoulder Elbow Surg. 2010;19:1034–1039. [DOI] [PubMed] [Google Scholar]
- 38. Peters KS, McCallum S, Briggs L, Murrell GA. A comparison of outcomes after arthroscopic repair of partial versus small or medium-sized full-thickness rotator cuff tears. J Bone Joint Surg Am. 2012;94:1078–1085. [DOI] [PubMed] [Google Scholar]
- 39. Randelli P, Spennacchio P, Ragone V, Arrigoni P, Casella A, Cabitza P. Complications associated with arthroscopic rotator cuff repair: a literature review. Musculoskelet Surg. 2012;96:9–16. [DOI] [PubMed] [Google Scholar]
- 40. Roy JS, Macdermid JC, Boyd KU, Faber KJ, Drosdowech D, Athwal GS. Rotational strength, range of motion, and function in people with unaffected shoulders from various stages of life. Sports Med Arthrosc Rehabil Ther Technol. 2009;1:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Saridakis P, Jones G. Outcomes of single-row and double-row arthroscopic rotator cuff repair: a systematic review. J Bone Joint Surg Am. 2010;92:732–742. [DOI] [PubMed] [Google Scholar]
- 42. Seo SS, Choi JS, An KC, Kim JH, Kim SB. The factors affecting stiffness occurring with rotator cuff tear. J Shoulder Elbow Surg. 2012;21:304–309. [DOI] [PubMed] [Google Scholar]
- 43. Seo YJ, Yoo YS, Kim DY, Noh KC, Shetty NS, Lee JH. Trans-tendon arthroscopic repair for partial-thickness articular side tears of the rotator cuff. Knee Surg Sports Traumatol Arthrosc. 2011;19:1755–1759. [DOI] [PubMed] [Google Scholar]
- 44. Shaffer B, Tibone JE, Kerlan RK. Frozen shoulder. A long-term follow-up. J Bone Joint Surg Am. 1992;74:738–746. [PubMed] [Google Scholar]
- 45. Sheibani-Rad S, Giveans MR, Arnoczky SP, Bedi A. Arthroscopic single-row versus double-row rotator cuff repair: a meta-analysis of the randomized clinical trials. Arthroscopy. 2013;29:343–348. [DOI] [PubMed] [Google Scholar]
- 46. Strauss EJ, Salata MJ, Kercher J, et al. Multimedia article. The arthroscopic management of partial-thickness rotator cuff tears: a systematic review of the literature. Arthroscopy. 2011;27:568–580. [DOI] [PubMed] [Google Scholar]
- 47. Tamai K, Akutsu M, Yano Y. Primary frozen shoulder: brief review of pathology and imaging abnormalities. J Orthop Sci. 2014;19:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31:589–604. [DOI] [PubMed] [Google Scholar]
- 49. Tauro JC. Stiffness and rotator cuff tears: incidence, arthroscopic findings, and treatment results. Arthroscopy. 2006;22:581–586. [DOI] [PubMed] [Google Scholar]
- 50. Trotti A, Colevas AD, Setser A, et al. CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol. 2003;13:176–181. [DOI] [PubMed] [Google Scholar]
- 51. Vairo GL, Duffey ML, Owens BD, Cameron KL. Clinical descriptive measures of shoulder range of motion for a healthy, young and physically active cohort. Sports Med Arthrosc Rehabil Ther Technol. 2012;4:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Veen EJ, Janssen-Heijnen ML, Bosma E, de Jongh MA, Roukema JA. The accuracy of complications documented in a prospective complication registry. J Surg Res. 2012;173:54–59. [DOI] [PubMed] [Google Scholar]
- 53. Weber SC, Abrams JS, Nottage WM. Complications associated with arthroscopic shoulder surgery. Arthroscopy. 2002;18(suppl 1):88–95. [DOI] [PubMed] [Google Scholar]
- 54. Williamson PR, Altman DG, Blazeby JM, et al. Developing core outcome sets for clinical trials: issues to consider. Trials. 2012;13:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zhang AL, Montgomery SR, Ngo SS, Hame SL, Wang JC, Gamradt SC. Analysis of rotator cuff repair trends in a large private insurance population. Arthroscopy. 2013;29:623–629. [DOI] [PubMed] [Google Scholar]
- 56. Zuckerman JD, Cuomo F. Frozen shoulder In: Matsen FA, III, Fu FH, Hawkins RJ, eds. The Shoulder: A Balance of Mobility and Stability. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1993:253–268. [Google Scholar]
- 57. Zuckerman JD, Rokito A. Frozen shoulder: a consensus definition. J Shoulder Elbow Surg. 2011;20:322–325. [DOI] [PubMed] [Google Scholar]


