Abstract
Context:
An evolution in conceptual understanding, coupled with technical innovations, has enabled hip preservation surgeons to address complex pathomorphologies about the hip joint to reduce pain, optimize function, and potentially increase the longevity of the native hip joint. Technical aspects of hip preservation surgeries are diverse and range from isolated arthroscopic or open procedures to hybrid procedures that combine the advantages of arthroscopy with open surgical dislocation, pelvic and/or proximal femoral osteotomy, and biologic treatments for cartilage restoration.
Evidence Acquisition:
PubMed and CINAHL databases were searched to identify relevant scientific and review articles from January 1920 to January 2015 using the search terms hip preservation, labrum, surgical dislocation, femoroacetabular impingement, peri-acetabular osteotomy, and rotational osteotomy. Reference lists of included articles were reviewed to locate additional references of interest.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
Thoughtful individualized surgical procedures are available to optimize the femoroacetabular joint in the presence of hip dysfunction.
Conclusion:
A comprehensive understanding of the relationship between femoral and pelvic orientation, morphology, and the development of intra-articular abnormalities is necessary to formulate a patient-specific approach to treatment with potential for a successful long-term result.
Keywords: hip preservation, peri-acetabular osteotomy, surgical dislocation, labrum, arthroscopy
The influence of abnormal joint morphology on the progression of osteoarthritis has been postulated for years.6,18,27,36,40,47,67,68,78 In addition, compensatory changes to the peri-articular myotendinous envelope and lower extremity kinematics are becoming better understood.6,31,46,50 Often, pathologies within the hip joint (labral-chondral injuries, synovitis, ligamentum teres tears) are associated with underlying abnormalities of bony morphology, rotation, version, or alignment. Modern hip preservation techniques aim to restore an optimal relationship between structure and joint kinematics. These techniques have shown promise for providing a durable solution for pain and dysfunction while avoiding the limitations and disadvantages inherent to joint arthroplasty.28,55,61,80
Anatomy and Biomechanics
Hip pathomorphology may interfere with physiologic motion due to anatomic conflict between the femoral head-neck junction and the acetabular rim. Soft tissue impingement, while less well understood, may also further restrict motion and lead to inhibition patterns of weakness and instability.48 Compromised joint stability can result in increased femoral translation, capsular attenuation, and increased shear stresses on the articular cartilage.30 In addition, atraumatic instability may increase the demand on adjacent peri-articular muscle groups, leading to compensatory adaptations during functional tasks.44,76 Over time, these cumulative biomechanical changes may result in progressive damage to intra-articular labral and chondral structures.5,50
During functional movements, postural control is regulated by dynamic force coupling, allowing distribution of imparted stresses and torque.26 Efficient mobility of the hip requires 40° to 50° of frontal plane motion and tolerance of one-third of an individual’s body weight during stationary double-leg stance.82 During unassisted stance and upright tasks, contributions of the psoas and abductor complex stabilize the lumbar spine while maintaining stability of the trunk in an erect position.2 Joint reactive forces reach a peak during toe-off and heel strike, necessitating increased activation of the adductor group and pectineus.82 Forward propulsion during ambulation requires the peri-articular musculature to generate a force of at least 6 times an individual’s mass to counteract the body’s weight and maintain pelvic stability.3 Cooperation between complementary peri-articular muscular groups and torque provided by tensioning of the iliotibial band/complex are necessary to maintain pelvic equilibrium.51 Abnormal pelvic elevation or depression compromises pelvic stability by limiting contributions from osseous structures and disrupting the balance between dynamic stabilizers (Figure 1). When pelvic elevation exceeds normal alignment by 15°, muscular demands must increase to maintain pelvic symmetry.42 Pelvic depression escalates fascial tension required to maintain pelvic stability with minimal to no recruitment of desirably involved musculature.51
Figure 1.

A 25-year-old woman with left lateral hip pain and right anterior groin pain. Plain radiographs demonstrate relative acetabular overcoverage on the right and undercoverage on the left due to leg length inequality and pelvic tilt. Acetabular undercoverage of the left hip placed increased demand on the peri-articular myofascial envelope (TFL, GMax, and ITB) and resulted in fatigue overload of these structures. Overcoverage on the right hip resulted in symptomatic FAI with labral and chondral injuries. Left proximal femoral shortening osteotomy corrected pelvic obliquity, normalized coverage, and rebalanced peri-articular myofascial stabilizers. FAI, femoroacetabular impingement; GMax, gluteus maximus; ITB, iliotibial band/complex; TFL, tensor fascia lata.
The combination of pathologic joint kinematics, dysfunctional peri-articular force coupling, and joint incongruence propagates altered joint reaction forces and potentially accelerates degenerative changes.32
Clinical Manifestation
Abnormal arthrokinematics are an expected consequence of structural abnormalities, muscular imbalances, and pain associated with hip pathologies.64 The “layer concept”31 has been proposed as a theoretical model to understand the presence and progression of hip joint dysfunction. Abnormalities involving any layer may lead to compensatory reactions from others and eventually result in linked pathomechanical changes within the proximal or distal segments of the kinetic chain. Antalgic gait patterns frequently manifest as a result of mechanical alterations and associated dynamic neuromuscular impairment. Gait abnormalities are often a product of pain or insufficient dynamic stability. Lateral trunk movement toward the dysfunctional hip is a strategy commonly employed to unload intra-articular pressures by displacing the center of gravity and enhance the mechanical advantage of the abductor complex when gluteal activation is poor.51,84 With gluteal weakness, adductor magnus activity will increase to maintain pelvic stability. Abductor strength may be compromised by abnormal femoral head positioning due to increased activation angle of the gluteus medius (GMed) caused by the augmented abductor lever arm.66 Supplementary recruitment of internal rotators is also employed as a compensatory strategy to increase abductor efficiency.17,34 Altered motor patterns that facilitate muscular disuse and dysfunction are further potentiated as the result of neuromuscular inhibition and habitual preference.49,52
Pathophysiology
Acetabular Dysplasia
In acetabular dysplasia, there is insufficient containment of the femoral head by the acetabulum, creating a focused distribution of joint reactive forces across a narrow segment of articular cartilage (Figure 2). Dysplasia may be characterized by focal regions of insufficient volume within the acetabular fossa or global undercoverage, where there is diffuse insufficiency of bony containment. Patterns and location of symptoms as well as compensatory peri-articular adaptations are often reflective of the specific anatomic region of structural instability.24 Uncorrected symptomatic acetabular dysplasia may increase the risk of functional impairment and degenerative joint disease due to associated labral hypertrophy and pathology, bony impingement, and capsular attenuation.25,30,37,54,81 Previous studies have linked acetabular dysplasia to premature osteoarthritis and the increased likelihood of requiring arthroplasty.20,23,25,52,69,79 Acetabular dysplasia is responsible for 20% to 50% of Americans suffering from symptomatic hip osteoarthritis.45
Figure 2.

A 16-year-old swimmer with symptomatic right hip acetabualar dysplasia.
Alteration of Proximal Femoral Alignment
Excessive anteversion, retroversion, or inclination of the proximal femur may lead to chronic pain, instability, and progressive functional decline32,40,41,57 (Figure 3). Increased sheer and translational forces caused by joint incongruity may accelerate degradation of the joint as a result of focused compression on the articular cartilage.79 Proximal femoral anteversion, defined as greater than 25°, referenced off the ipsilateral femoral condyles, has been linked to atraumatic anterior hip instability and posterior impingement, while femoral retroversion may predispose to anterior impingement, reduced internal rotation, and posterior hip instability.12,32,53,56 The inclination angle, defined as the angle subtended by the femoral neck and shaft of the proximal femur, affects leg length and influences dynamic abductor function and force coupling.12,32 Clinically, abduction is limited due to trochanteric-pelvic impingement and intervening soft tissues, which discourages abductor muscular recruitment. Coxa valga is often asymptomatic, but may require surgical correction to improve distribution forces across the weightbearing surface of the joint and limit chondrolabral injury.59,75 Excessive valgus angulation can perpetuate mechanical instability and ultimately lead to focal chondral loss due to edge loading at the lateral margin of the acetabular rim.22 Coxa vara, on the other hand, is less common but may predispose to trochanteric-pelvic impingement or, due to increased offset, lead to peritrochanteric pain and iliotibial band/complex contracture.58
Figure 3.

A 17-year-old soccer player with excessive proximal femoral valgus and concomitant symptomatic femoroacetabular impingement.
Femoroacetabular Impingement
Morphologic alterations of the proximal femur and/or acetabulum may lead to pathologic anatomic conflict during dynamic activities (Figure 4).62 Progressive chondral and labral injuries may ultimately occur, leading to pain, joint dysfunction, and alterations in adjacent body segments within the kinetic chain. Impaired motion between the proximal femur and acetabulum may also lead to reactive changes in the other portions of the “pelvic joint,” including pubic symphysis, pelvic brim, sacroiliac joint, and lumbar spine.11,46 The location of impingement may be intra-articular, including the proximal femur and acetabulum, or extra-articular, most commonly involving the proximal femur and anterior inferior iliac spine, between the greater trochanter and pelvis and between the ischium and lesser trochanter. Femoroacetabular impingement (FAI) has been proposed as a significant contributor to the development of premature hip arthritis due to repetitive forceful collision between the proximal femur and acetabulum, leading to labral-chondral injury and resultant joint deterioration.41
Figure 4.
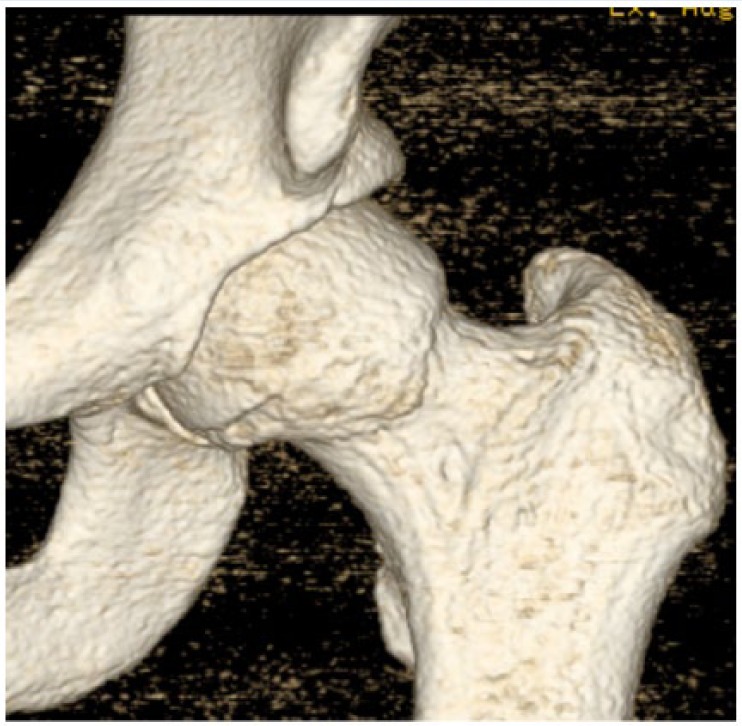
A 28-year-old recreational athlete with symptomatic left hip femoroacetabular impingement (FAI) and reduced femoral head-neck demonstrated on computed tomography with 3-dimensional reconstruction.
Joint-Preserving Techniques
Peri-acetabular Osteotomy
The Bernese peri-acetabular osteotomy (PAO),24 often referred to as the Ganz osteotomy, is currently the preferred technique for large-scale correction of acetabluar dysplasia.1,39 It has been championed for its ability to affect global improvement in femoral head coverage and balance force concentration through the weightbearing portion of the femoral head. By preserving the integrity of the posterior column of the pelvis, this osteotomy allows earlier weightbearing through preservation of an intact posterior column and a more aggressive rehabilitative approach. In addition to its utility in low-volume acetabulum conditions such as acetabular dysplasia, the PAO has been used in FAI to offset dysmorphism of the proximal femur as well as aid in correction of global anteversion or retroversion of the acetabulum (Figure 5).77 There are occasions where structural instability exists in the presence of concomitant avascular necrosis (AVN). PAO may be used in conjunction with surgical dislocation and osteoarticular allograft transplantation system (OATS) (Figures 6 and 7). A reorientation procedure may lend itself to the redistribution of force across the acetabulum and potentially decelerate joint degeneration seen in acetabular dysplasia.80 A PAO may be performed as an isolated procedure with exposure of the anterior hip via arthrotomy or in conjunction with hip arthroscopy for minimally invasive joint access and central and peripheral compartment work (Figure 8). Clinical studies have demonstrated a high rate of intra-articular pathology at the time of arthrotomy or arthroscopy.29,74 Failure to address concomitant intra-articular joint disease at the time of reorientation osteotomy may lead to persistent pain and incomplete recovery.29,43
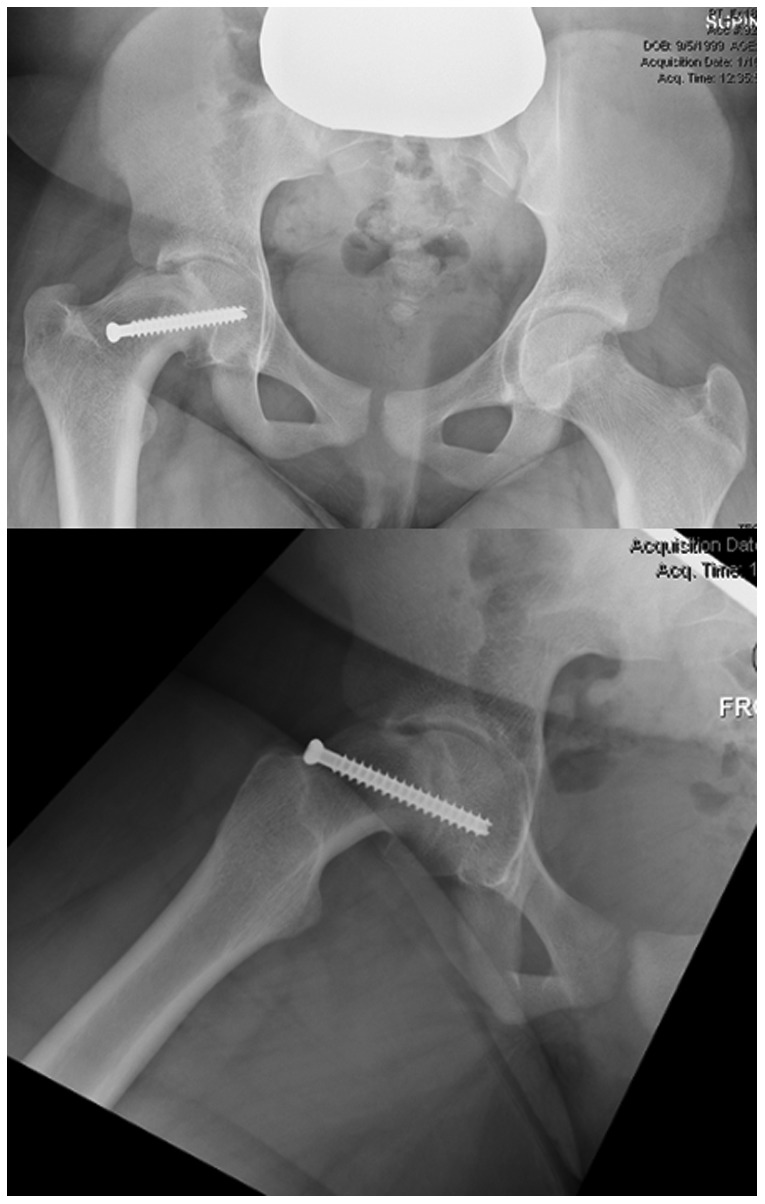
Figure 5.
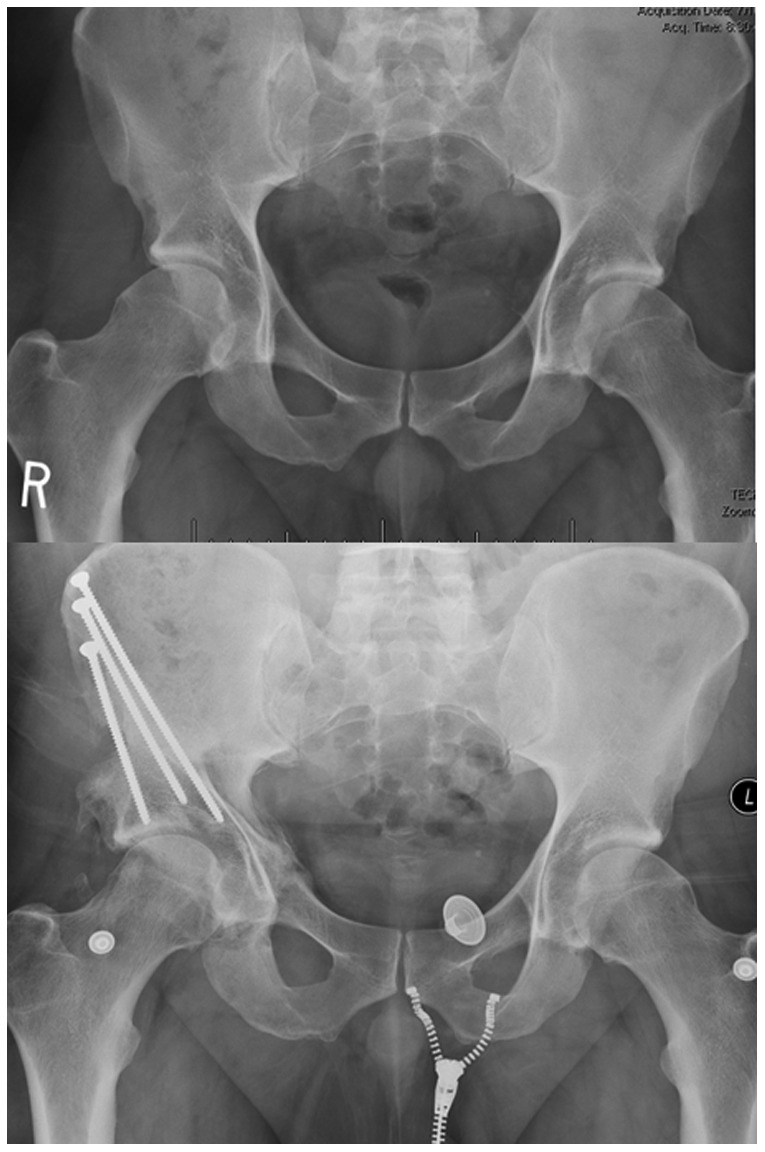
Pre- and postoperative radiographic images of a 32-year-old man with a low-volume acetabulum and concomitant femoroacetabular impingement (FAI) treated with arthroscopic FAI decompression and peri-acetabular osteotomy to correct structural instability, abnormal bony morphology, and intra-articular labral-chondral injury.
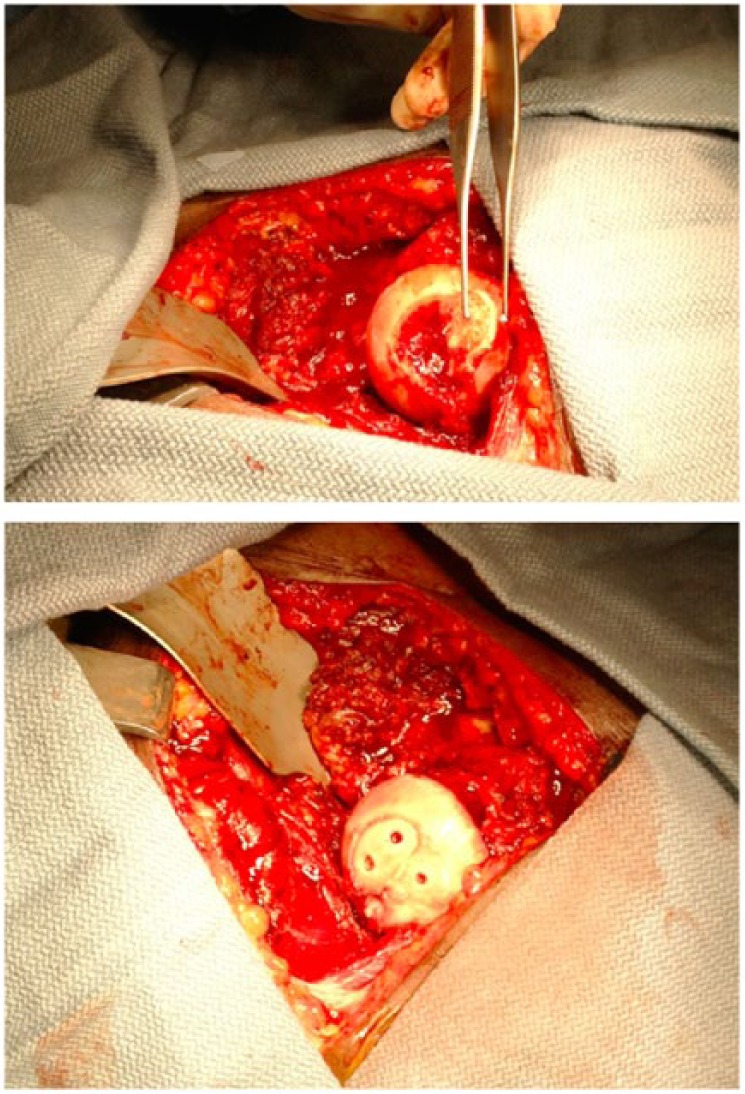
Figure 6.
Pre- and postoperative images of a 26-year-old woman with acetabular dysplasia and AVN of the femoral head treated with peri-acetabular osteotomy and femoral head OATS using a vessel-sparing SD. AVN, avascular necrosis; OATS, osteoarticular allograft transplantation system; SD, surgical dislocation.
Figure 7.

Intraoperative images depicting the exposed femoral head after osteoarticular allograft transplantation system (OATS) with excellent graft contour and smooth press-fit.
Figure 8.
Preoperative lateral and intraoperative image demonstrating reduced femoral head-neck offset and subsequent correction using arthroscopic decompression.
The decision whether to utilize arthrotomy or arthroscopy as an adjunct to PAO is largely surgeon- and resource-dependent. In addition, arthroscopy can confirm the suspected pattern of joint mechanics by demonstrating edge-loading on articular cartilage and further help refine the necessary corrective rotation of the PAO. Patients with larger body habitus may also benefit from an arthroscopic approach because of more challenging visualization with an open approach and arthrotomy.
Proximal Femoral Osteotomy
Derotational osteotomy techniques are performed for excessive anteversion or retroversion, whereas varus/valgus correction of angulation redirects the femoral head to modify contact surfaces, diminish shear vector, and optimize the biomechanical advantage of the peri-articular myotendinous envelope (Figure 9).59 A varus osteotomy may decrease edge-loading by recentering the femoral head within the acetabulum.89 This may consequently lead to decreased gluteal muscle recruitment. Conversely, a valgus osteotomy may shorten and enhance efficiency of the abductor lever arm and increase joint congruence through distalization of the greater trochanter.59 Proximal femoral osteotomies may improve the mechanical environment of the joint and delay total hip arthroplasty.89 Conditions such as Legg-Calve-Perthes (LCP) and slipped capital femoral epiphysis (SCFE) are often associated with global deformities of the femoral head and neck and may benefit from proximal femoral osteotomy. Proximal femoral osteotomy is a powerful tool that can be used to reorient the region of femoral-sided impingement away from conflicting acetabluar segment, thus allowing indirect decompression of FAI.57
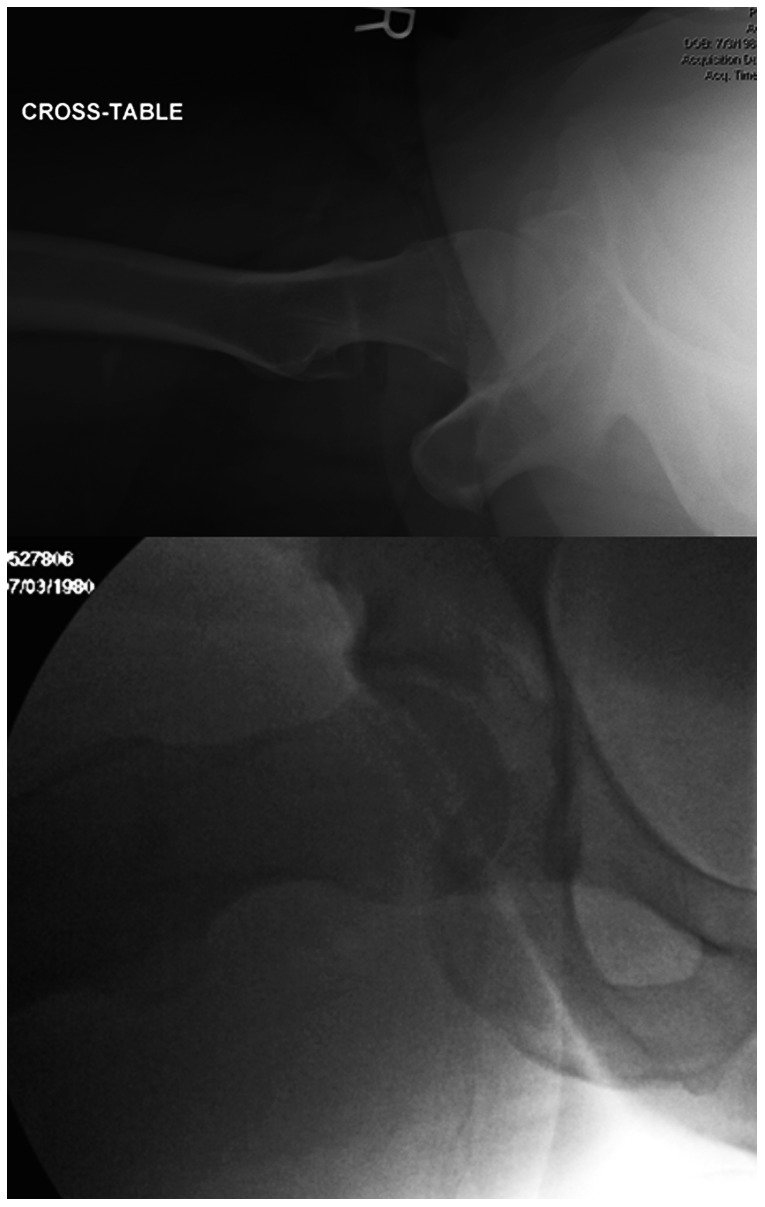
Figure 9.

Patient from Figure 2 after varus proximal femoral osteotomy. This patient also underwent arthroscopic femoroacetabular impingement decompression and labral repair.
Cartilage Restoration
Functional outcome studies after cartilage restoration of the hip are sparse. Microfracture, OATS, autologous chondrocyte techniques (ACT), and matrix-associated autologous chondrocyte implantation (MACI) have been increasingly applied in the knee and ankle with midterm success rates as high as 90%.8,19,35,71,86 These cartilage restoration techniques have been applied to the hip with encouraging short-term clinical outcomes.16,63,72 Femoral head OATS has a success rate of 80% in patients with nonsteroid-induced osteonecrosis (see Figure 7).63 Microfracture of the hip also has favorable outcomes for both femoral head and acetabular defects.16,72 However, for larger lesions, OATS63 or ACI14,71 procedures may provide a more durable solution. (Figure 10).
Figure 10.
A 16-year-old soccer player with large osteochondral defect of the femoral head. The lesion was noted to have a stable articular surface and viable subchondral bone. Therefore, drilling and bioabsorbable compression screw fixation was used to stabilize the lesion.
Surgical Dislocation
Traditionally, FAI was treated with osteoplasty of the acetabular rim and/or proximal femur utilizing an open vessel-sparing surgical dislocation (SD), usually via trochanteric osteotomy.38 In some centers, SD remains the gold standard for gaining circumferential access to the femoral head and permits unobstructed visualization of the central compartment of the hip for treatment of labral and chondral injuries. Studies comparing open versus arthroscopic femoral osteoplasty techniques have shown equivalence in bony correction, although for global femoral head deformities, SD remains a preferable means of addressing superolateral and posterosuperior abnormalities.7,13,38,57 Furthermore, sequelae of LCP, SCFE, or AVN are often associated with relative femoral neck shortening, which can contribute to ischiofemoral, trochanteric-pelvic, and other iterations of extra-articular FAI (Figure 11). A trochanteric osteotomy is often used as a technical step in this approach and can later be distalized to increase the mechanical advantage of the hip abductor complex and achieve “relative femoral neck lengthening,” effectively minimizing extra-articular impingement sources (Figure 12).2
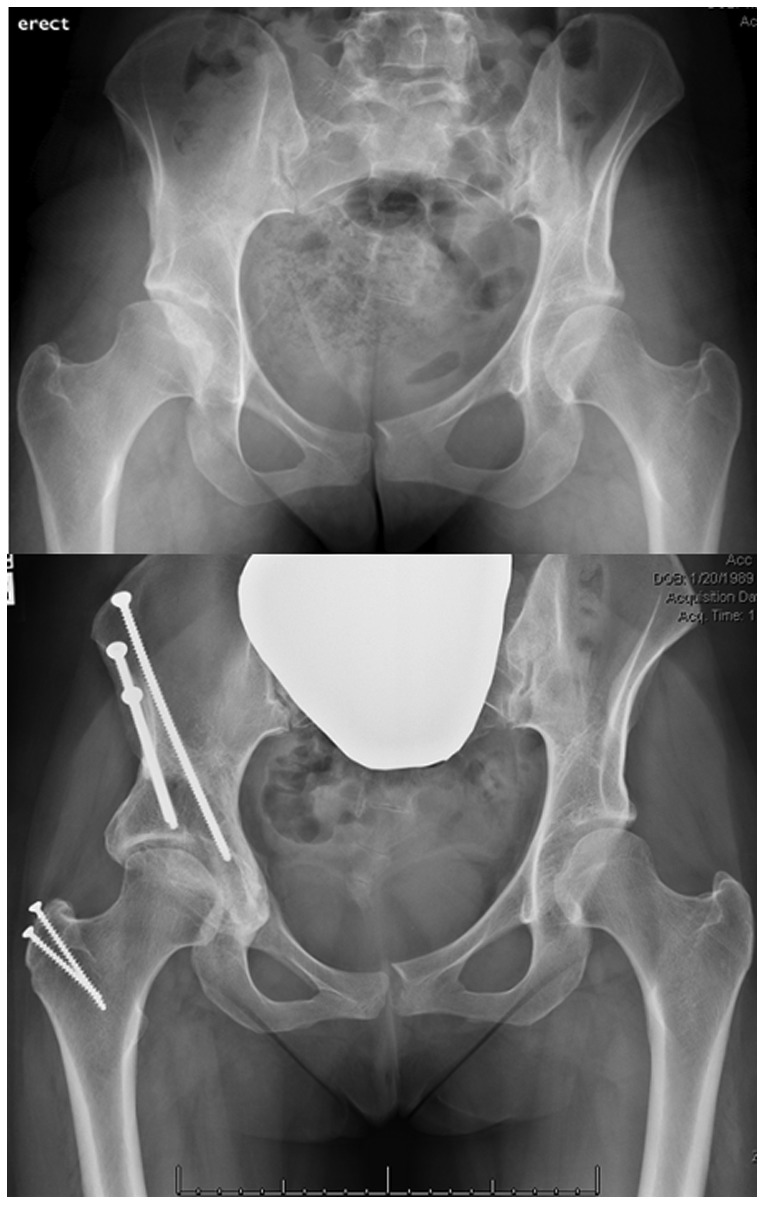
Figure 11.
A 14-year-old girl demonstrating sequelae of treatment for unstable slipped capital femoral epiphysis (SCFE) with subsequent severe rotational and structural abnormalities of the proximal femur.
Figure 12.
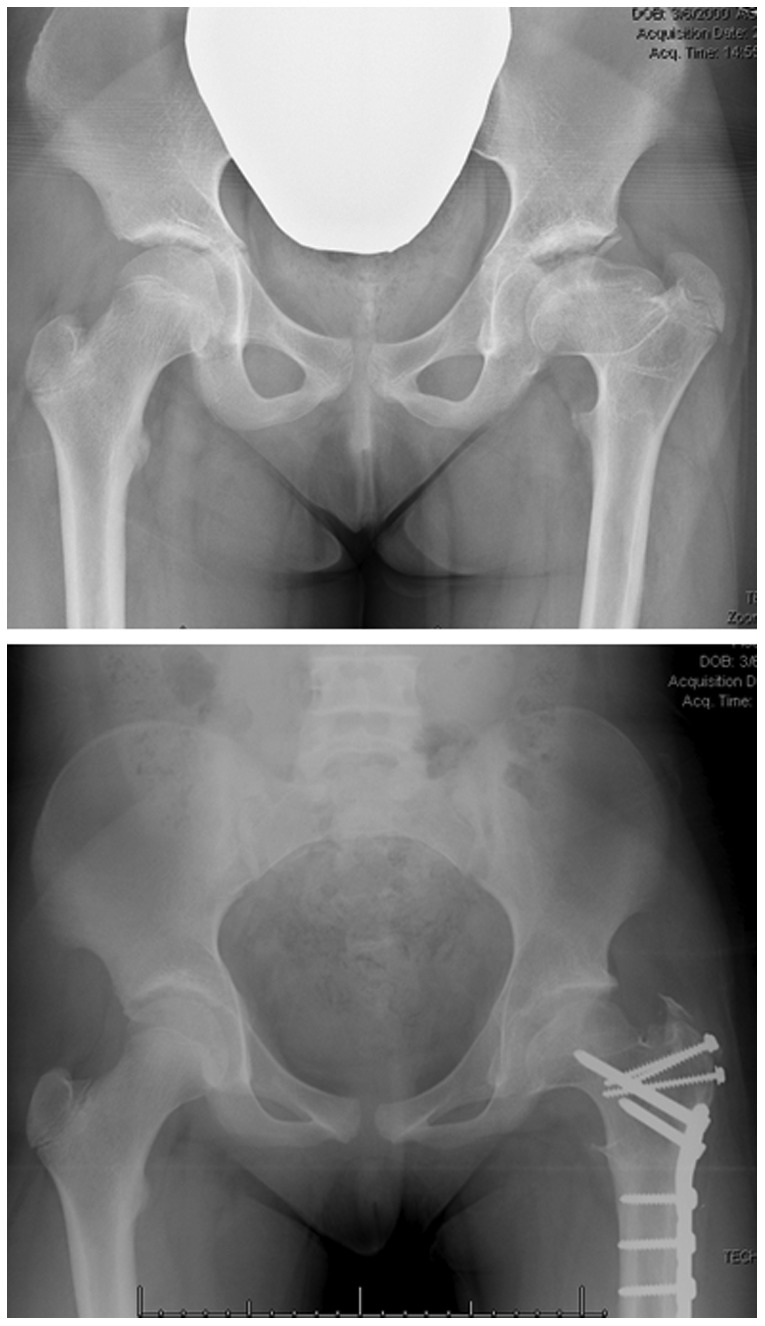
A 15-year-old girl demonstrating sequelae of Legg-Calve-Perthes with severe femoral head deformity, coxa breva, and rotational abnormality of the proximal femur. Treatment consisted of osteochondroplasty of the femoral head via surgical dislocation, relative femoral neck lengthening, and proximal femoral osteotomy.
In select individuals who demonstrate normal femoral neck length and offset, SD can be accomplished without trochanteric osteotomy, which can have important implications for rehabilitation strategies (Figure 13). Using a modified Watson-Jones approach,10 fibers of the hip abductor complex are elevated away from the iliocapsularis and anterior capsule. If tissue mobility allows, the trochanter can be left intact, which can facilitate more aggressive rehabilitation as it eliminates the need to achieve bony union prior to advancing weightbearing. However, patient selection is crucial with this approach, since obese patients or patients with less compliant soft tissues are typically not appropriate candidates for this technique and would be better served with trochanteric osteotomy. Furthermore, trochanteric osteotomy is a key technical step in achieving a relative femoral neck lengthening in patients with coxa breva and should be utilized when this clinical scenario is present.4,33
Figure 13.

A 26-year-old woman with a history of graft-versus-host disease who developed widespread heterotopic bone formation as a result of her treatment. She underwent bilateral open femoracetabular impingement decompression via surgical dislocation without the use of trochanteric osteotomy.
One of the most controversial uses of SD in the hip is in the treatment of acute SCFE. A modified Dunn technique can be used to gain access to the unstable and slipped femoral head and neck.88 A portion of the neck is shortened, restoring proper anatomic positioning of the femoral head on the neck. Potential advantages of this procedure include the reduced need of further surgery to correct residual deformity. In acute SCFE, this procedure may reduce the rate of AVN of the femoral head.60
Arthroscopy
As FAI became recognized as a causative factor in the progression of idiopathic osteoarthritis,41 application of arthroscopic techniques has evolved to correct FAI. Correction of structural pathomorphology via reorientation and restoration procedures may provide limited benefit if underlying intra-articular pathology is left unaddressed (Figure 14).83 Arthroscopic labral preservation with capsulorrhaphy may benefit select candidates with borderline acetabular dysplasia.30 In patients with more severe acetabular insufficiency, arthroscopic treatment of labral and chondral abnormalities is more controversial,15 and careful patient selection and counseling regarding potential risks is recommended. There is an increased risk of iatrogenic instability in this patient population due to the inability of an arthroscopic procedure to correct the structural instability inherent to this population.9,30,70,73
Figure 14.
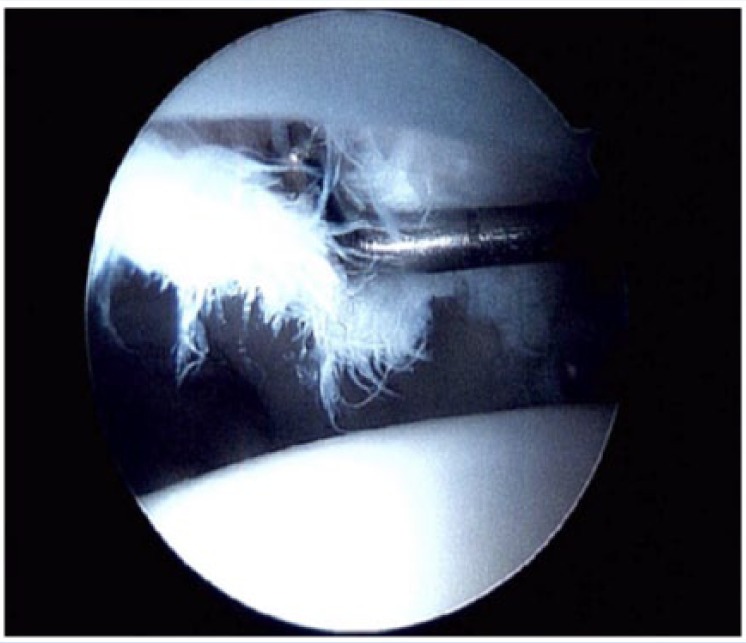
Intraoperative image demonstrating labral-chondral injury treated arthroscopically during combined arthroscopic and open hip preservation surgery.
Formerly, PAO was performed as an index procedure in isolation, with successful outcomes at short- and mid-term assessments.61 Unsatisfactory long-term results have been reported,65 with rates of conversion to total hip arthroplasty as high as 17%.21,74 In the setting of acetabular undercoverage, the labrum and ligamentum teres often undergo hypertrophy to compensate for a lack of containment and stability of the femoral head.87 Consequently, the labral-chondral transitional zone and ligamentum teres are often damaged as the result of focal edge-loading and increased shear force across the weightbearing surface of the acetabulum.
The use of adjuvant hip arthroscopy to address intra-articular hip disease with large-scale open structural correction offers potential benefits and strengths of both procedures and may further optimize clinical outcomes at mid- and long-term follow-up.85
Conclusion
A comprehensive understanding of the relationship between femoral and pelvic orientation, morphology, and the development of intra-articular abnormalities is necessary to formulate an effective and patient-specific treatment strategy that has the potential to produce a favorable and durable outcome for the patient.
Footnotes
The following authors declared potential conflicts of interest: P. Christopher Cook, MD, FRCS(C), is a paid consultant for Arthrex. Yi-Meng Yen, MD, PhD, is a paid consultant for Orthopediatrics, Smith & Nephew, and Arthrex. Brian D. Giordano, MD, is a paid consultant for Arthrex.
References
- 1. Albers C, Steppacher S, Ganz R, Siebenrock K, Tannast M. Optimal acetabular reorientation and offset correction improve the long term results after periacetabular osteotomy. J Bone Joint Surg Br. 2012;94(suppl 37):585. [Google Scholar]
- 2. Albers CE, Steppacher SD, Ganz R, Siebenrock KA, Tannast M. Joint-preserving surgery improves pain, range of motion, and abductor strength after Legg-Calvé-Perthes disease. Clin Orthop Relat Res. 2012;470:2450-2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521-533. [DOI] [PubMed] [Google Scholar]
- 4. Anderson LA, Erickson JA, Severson E, Peters CL. Sequelae of Perthes disease: treatment with surgical hip dislocation and relative femoral neck lengthening. J Pediatr Orthop. 2010;30:758-766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Arokoski JP, Jurvelin JS, Vaatainen U, Helminen HJ. Normal and pathological adaptations of articular cartilage to joint loading. Scand J Med Sci Sports. 2000;10:186-198. [DOI] [PubMed] [Google Scholar]
- 6. Bedi A, Dolan M, Leunig M, Kelly BT. Static and dynamic mechanical causes of hip pain. Arthroscopy. 2011;27:235-251. [DOI] [PubMed] [Google Scholar]
- 7. Bedi A, Zaltz I, De La Torre K, Kelly BT. Radiographic comparison of surgical hip dislocation and hip arthroscopy for treatment of cam deformity in femoroacetabular impingement. Am J Sports Med. 2011;39(suppl):20S-28S. [DOI] [PubMed] [Google Scholar]
- 8. Behrens P, Bitter T, Kurz B, Russlies M. Matrix-associated autologous chondrocyte transplantation/implantation (MACT/MACI)—5-year follow-up. Knee. 2006;13:194-202. [DOI] [PubMed] [Google Scholar]
- 9. Benali Y, Katthagen BD. Hip subluxation as a complication of arthroscopic debridement. Arthroscopy. 2009;25:405-407. [DOI] [PubMed] [Google Scholar]
- 10. Bertin KC, Röttinger H. Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Relat Res. 2004;429:248-255. [PubMed] [Google Scholar]
- 11. Birmingham PM, Kelly BT, Jacobs R, McGrady L, Wang M. The effect of dynamic femoroacetabular impingement on pubic symphysis motion: a cadaveric study. Am J Sports Med. 2012;40:1113-1118. [DOI] [PubMed] [Google Scholar]
- 12. Botser IB, Ozoude GC, Martin DE, Siddiqi AJ, Kuppuswami S, Domb BG. Femoral anteversion in the hip: comparison of measurement by computed tomography, magnetic resonance imaging, and physical examination. Arthroscopy. 2012;28:619-627. [DOI] [PubMed] [Google Scholar]
- 13. Botser IB, Smith TW, Jr, Nasser R, Domb BG. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy. 2011;27:270-278. [DOI] [PubMed] [Google Scholar]
- 14. Briggs TW, Mahroof S, David LA, Flannelly J, Pringle J, Bayliss M. Histological evaluation of chondral defects after autologous chondrocyte implantation of the knee. J Bone Joint Surg Br. 2003;85:1077-1083. [DOI] [PubMed] [Google Scholar]
- 15. Byrd J, Jones KS. Hip arthroscopy in the presence of dysplasia. Arthroscopy. 2003;19:1055-1060. [DOI] [PubMed] [Google Scholar]
- 16. Byrd J, Jones KS. Microfracture for grade IV chondral lesions of the hip (SS-89). Arthroscopy. 2004;20:e41. [Google Scholar]
- 17. Casartelli NC, Maffiuletti NA, Item-Glatthorn JF, et al. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthritis Cartilage. 2011;19:816-821. [DOI] [PubMed] [Google Scholar]
- 18. Chegini S, Beck M, Ferguson SJ. The effects of impingement and dysplasia on stress distributions in the hip joint during sitting and walking: a finite element analysis. J Orthop Res. 2009;27:195-201. [DOI] [PubMed] [Google Scholar]
- 19. Choi NY, Kim BW, Yeo WJ, et al. Gel-type autologous chondrocyte (Chondron) implantation for treatment of articular cartilage defects of the knee. BMC Musculoskelet Disord. 2010;11:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Clohisy JC, Beaulé PE, O’Malley A, Safran MR, Schoenecker P. AOA symposium. Hip disease in the young adult: current concepts of etiology and surgical treatment. J Bone Joint Surg Am. 2008;90:2267-2281. [DOI] [PubMed] [Google Scholar]
- 21. Clohisy JC, John LS, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009;467:2041-2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL. Incidence and characteristics of femoral deformities in the dysplastic hip. Clin Orthop Relat Res. 2009;467:128-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Clohisy JC, Nunley RM, Curry MC, Schoenecker PL. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J Bone Joint Surg Am. 2007;89:1417-1423. [DOI] [PubMed] [Google Scholar]
- 24. Coobs BR, Xiong A, Clohisy JC. Contemporary concepts in the young adult hip patient: periacetabular osteotomy for hip dysplasia [published online March 25, 2015]. J Arthroplasty. doi: 10.1016/j.arth.2015.02.045. [DOI] [PubMed] [Google Scholar]
- 25. Cooperman DR, Wallensten R, Stulberg SD. Acetabular dysplasia in the adult. Clin Orthop Relat Res. 1983;(175):79-85. [PubMed] [Google Scholar]
- 26. Correa TA, Crossley KM, Kim HJ, Pandy MG. Contributions of individual muscles to hip joint contact force in normal walking. J Biomech. 2010;43:1618-1622. [DOI] [PubMed] [Google Scholar]
- 27. Doherty M, Courtney P, Doherty S, et al. Nonspherical femoral head shape (pistol grip deformity), neck shaft angle, and risk of hip osteoarthritis: a case-control study. Arthritis Rheum. 2008;58:3172-3182. [DOI] [PubMed] [Google Scholar]
- 28. Domb B, LaReau J, Redmond JM. Combined hip arthroscopy and periacetabular osteotomy: indications, advantages, technique, and complications. Arthroscopy Tech. 2014;3:e95-e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Domb BG, Lareau JM, Baydoun H, Botser I, Millis MB, Yen Y-M. Is intraarticular pathology common in patients with hip dysplasia undergoing periacetabular osteotomy? Clin Orthop Relat Res. 2014;472:674-680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Domb BG, Philippon MJ, Giordano BD. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: relation to atraumatic instability. Arthroscopy. 2013;29:162-173. [DOI] [PubMed] [Google Scholar]
- 31. Draovitch P, Edelstein J, Kelly BT. The layer concept: utilization in determining the pain generators, pathology and how structure determines treatment. Curr Rev Musculoskelet Med. 2012;5:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ecker TM, Tannast M, Puls M, Siebenrock KA, Murphy SB. Pathomorphologic alterations predict presence or absence of hip osteoarthrosis. Clin Orthop Relat Res. 2007;465:46-52. [DOI] [PubMed] [Google Scholar]
- 33. Eilert RE, Hill K, Bach J. Greater trochanteric transfer for the treatment of coxa brevis. Clin Orthop Relat Res. 2005;434:92-101. [DOI] [PubMed] [Google Scholar]
- 34. Ferber R, Noehren B, Hamill J, Davis I. Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J Orthop Sports Phys Ther. 2010;40(2):52-58. [DOI] [PubMed] [Google Scholar]
- 35. Fontana A, Bistolfi A, Crova M, Rosso F, Massazza G. Arthroscopic treatment of hip chondral defects: autologous chondrocyte transplantation versus simple debridement—a pilot study. Arthroscopy. 2012;28:322-329. [DOI] [PubMed] [Google Scholar]
- 36. Freeman CR, Azzam MG, Leunig M. Hip preservation surgery: surgical care for femoroacetabular impingement and the possibility of preventing hip osteoarthritis. J Hip Preserv Surg. 2014;1(2):46-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Fujii M, Nakashima Y, Jingushi S, et al. Intraarticular findings in symptomatic developmental dysplasia of the hip. J Pediatr Orthop. 2009;29:9-13. [DOI] [PubMed] [Google Scholar]
- 38. Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119-1124. [DOI] [PubMed] [Google Scholar]
- 39. Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias technique and preliminary results. Clin Orthop Relat Res. 1988;(232):26-36. [PubMed] [Google Scholar]
- 40. Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112-120. [DOI] [PubMed] [Google Scholar]
- 42. Gebhart JJ, Streit JJ, Bedi A, Bush-Joseph CA, Nho SJ, Salata MJ. Correlation of pelvic incidence with cam and pincer lesions. Am J Sports Med. 2014;42:2649-2653. [DOI] [PubMed] [Google Scholar]
- 43. Ginnetti JG, Pelt CE, Erickson JA, Van Dine C, Peters CL. Prevalence and treatment of intraarticular pathology recognized at the time of periacetabular osteotomy for the dysplastic hip. Clin Orthop Relat Res. 2013;471:498-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Giordano BD. Assessment and treatment of hip pain in the adolescent athlete. Pediatr Clin North Am. 2014;61:1137-1154. [DOI] [PubMed] [Google Scholar]
- 45. Goldstein RY, Kaye ID, Slover J, Feldman D. Hip dysplasia in the skeletally mature patient. Bull Hosp Joint Dis. 2014;72:28-42. [PubMed] [Google Scholar]
- 46. Hammoud S, Bedi A, Voos JE, Mauro CS, Kelly BT. The recognition and evaluation of patterns of compensatory injury in patients with mechanical hip pain. Sports Health. 2014;6:108-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2013;72:918-923. [DOI] [PubMed] [Google Scholar]
- 48. Hetsroni I, Poultsides L, Bedi A, Larson CM, Kelly BT. Anterior inferior iliac spine morphology correlates with hip range of motion: a classification system and dynamic model. Clin Orthop Relat Res. 2013;471:2497-2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hoaglund FT, Yau AC, Wong WL. Osteoarthritis of the hip and other joints in southern Chinese in Hong Kong. J Bone Joint Surg Am. 1973;55:545-557. [PubMed] [Google Scholar]
- 50. Hulet C, Hurwitz D, Andriacchi T, Galante J, Vielpeau C. Functional gait adaptations in patients with painful hip [in French]. Rev Chir Orthop Réparatrice Appar Mot. 2000;86:581-589. [PubMed] [Google Scholar]
- 51. Inman VT. Functional aspects of the abductor muscles of the hip. J Bone Joint Surg Am. 1947;29:607-619. [PubMed] [Google Scholar]
- 52. Janda V. Muscle Function Testing. London, England: Butterworths; 1983. [Google Scholar]
- 53. Kelly BT, Bedi A, Robertson CM, Dela Torre K, Giveans MR, Larson CM. Alterations in internal rotation and alpha angles are associated with arthroscopic cam decompression in the hip. Am J Sports Med. 2012;40:1107-1112. [DOI] [PubMed] [Google Scholar]
- 54. Klaue K, Durnin C, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423-429. [DOI] [PubMed] [Google Scholar]
- 55. Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015-1021. [DOI] [PubMed] [Google Scholar]
- 56. Larson CM, Stone RM. Current concepts and trends for operative treatment of FAI: hip arthroscopy. Curr Rev Musculoskelet Med. 2013;6:242-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Leunig M, Ganz R. The evolution and concepts of joint-preserving surgery of the hip. Bone Joint J. 2014;96:5-18. [DOI] [PubMed] [Google Scholar]
- 58. Lewis CL. Extra-articular snapping hip: a literature review. Sports Health. 2010;2:186-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Louahem M’sabah D, Assi C, Cottalorda J. Proximal femoral osteotomies in children. Orthop Traumatol Surg Res. 2013;99(1 suppl):S171-S186. [DOI] [PubMed] [Google Scholar]
- 60. Madan S, Cooper A, Davies A, Fernandes J. The treatment of severe slipped capital femoral epiphysis via the Ganz surgical dislocation and anatomical reduction. A prospective study. Bone Joint J. 2013;95:424-429. [DOI] [PubMed] [Google Scholar]
- 61. Matheney T, Kim Y-J, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg. 2009;91:2113-2123. [DOI] [PubMed] [Google Scholar]
- 62. Matheney T, Sandell L, Foucher K, Lamontagne M, Grodzinsky AJ, Peters CL. Motion analysis, cartilage mechanics, and biology in femoroacetabular impingement: current understanding and areas of future research. J Am Acad Orthop Surg. 2013;21(suppl 1):S27-S32. [DOI] [PubMed] [Google Scholar]
- 63. Meyers MH. Osteonecrosis of the femoral head. Pathogenesis and long-term results of treatment. Clin Orthop Relat Res. 1988;(231):51-61. [PubMed] [Google Scholar]
- 64. Murphy SB, Ganz R, Muller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985-989. [DOI] [PubMed] [Google Scholar]
- 65. Nakamura S, Ninomiya S, Takatori Y, Morimoto S, Umeyama T. Long-term outcome of rotational acetabular osteotomy 145 hips followed for 10-23 years. Acta Orthop. 1998;69:259-265. [DOI] [PubMed] [Google Scholar]
- 66. Nepple JJ, Byrd JT, Siebenrock KA, Prather H, Clohisy JC. Overview of treatment options, clinical results, and controversies in the management of femoroacetabular impingement. J Am Acad Orthop Surg. 2013;21(suppl 1):S53-S58. [DOI] [PubMed] [Google Scholar]
- 67. Ng KG, Rouhi G, Lamontagne M, Beaulé PE. Finite element analysis examining the effects of cam FAI on hip joint mechanical loading using subject-specific geometries during standing and maximum squat. HSS J. 2012;8:206-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Nicholls AS, Kiran A, Pollard TC, et al. The association between hip morphology parameters and nineteen-year risk of end-stage osteoarthritis of the hip: a nested case-control study. Arthritis Rheum. 2011;63:3392-3400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Nozawa M, Shitoto K, Matsuda K, Maezawa K, Kurosawa H. Rotational acetabular osteotomy for acetabular dysplasia. A follow-up for more than ten years. J Bone Joint Surg Br. 2002;84:59-65. [DOI] [PubMed] [Google Scholar]
- 70. Parvizi J, Bican O, Bender B, et al. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty. 2009;24:110-113. [DOI] [PubMed] [Google Scholar]
- 71. Peterson L, Vasiliadis HS, Brittberg M, Lindahl A. Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med. 2010;38:1117-1124. [DOI] [PubMed] [Google Scholar]
- 72. Philippon MJ, Schenker ML, Briggs KK, Maxwell RB. Can microfracture produce repair tissue in acetabular chondral defects? Arthroscopy. 2008;24:46-50. [DOI] [PubMed] [Google Scholar]
- 73. Ranawat AS, McClincy M, Sekiya JK. Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip. A case report. J Bone Joint Surg Am. 2009;91:192-197. [DOI] [PubMed] [Google Scholar]
- 74. Ross JR, Zaltz I, Nepple JJ, Schoenecker PL, Clohisy JC. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med. 2011;39(1 suppl):72S-78S. [DOI] [PubMed] [Google Scholar]
- 75. Sanchez-Sotelo J, Trousdale RT, Berry DJ, Cabanela ME. Surgical treatment of developmental dysplasia of the hip in adults: I. Nonarthroplasty options. J Am Acad Orthop Surg. 2002;10:321-333. [DOI] [PubMed] [Google Scholar]
- 76. Shindle MK, Ranawat AS, Kelly BT. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med. 2006;25:309-326. [DOI] [PubMed] [Google Scholar]
- 77. Siebenrock KA, Steppacher SD, Tannast M, Büchler L. Anteverting periacetabular osteotomy for acetabular retroversion. JBJS Essent Surg Tech. 2015;5(1):e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Solomon L. Geographical and anatomical patterns of osteoarthritis. Br J Rheumatol. 1984;23:177-180. [DOI] [PubMed] [Google Scholar]
- 79. Solomon L. Patterns of osteoarthritis of the hip. J Bone Joint Surg Br. 1976;58:176-183. [DOI] [PubMed] [Google Scholar]
- 80. Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year follow-up of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633-1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Tönnis D, Legal H, Graf R. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin, Germany: Springer-Verlag; 1987. [Google Scholar]
- 82. Torry MR, Schenker ML, Martin HD, Hogoboom D, Philippon MJ. Neuromuscular hip biomechanics and pathology in the athlete. Clin Sports Med. 2006;25:179-197. [DOI] [PubMed] [Google Scholar]
- 83. Tsumura H, Kaku N, Ikeda S, Torisu T. A computer simulation of rotational acetabular osteotomy for dysplastic hip joint: does the optimal transposition of the acetabular fragment exist? J Orthop Sci. 2005;10:145-151. [DOI] [PubMed] [Google Scholar]
- 84. Watelain E, Dujardin F, Babier F, Dubois D, Allard P. Pelvic and lower limb compensatory actions of subjects in an early stage of hip osteoarthritis. Arch Phys Med Rehabil. 2001;82:1705-1711. [DOI] [PubMed] [Google Scholar]
- 85. Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;(426):145-150. [DOI] [PubMed] [Google Scholar]
- 86. Wiewiorski M, Leumann A, Buettner O, Pagenstert G, Horisberger M, Valderrabano V. Autologous matrix-induced chondrogenesis aided reconstruction of a large focal osteochondral lesion of the talus. Arch Orthop Trauma Surg. 2011;131:293-296. [DOI] [PubMed] [Google Scholar]
- 87. Yamamuro T, Ishida K. Recent advances in the prevention, early diagnosis, and treatment of congenital dislocation of the hip in Japan. Clin Orthop Relat Res. 1984;(184):24-40. [PubMed] [Google Scholar]
- 88. Zaltz I, Georgiadis AG. Slipped capital femoral epiphysis: acute and chronic. In: Nho S, Leunig M, Larson CM, Bedi A, Kelly BT, eds. Hip Arthroscopy and Hip Joint Preservation Surgery. New York, NY: Springer; 2014:459-474. [Google Scholar]
- 89. Zweifel J, Hönle W, Schuh A. Long-term results of intertrochanteric varus osteotomy for dysplastic osteoarthritis of the hip. Int Orthop. 2011;35:9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]


