Abstract
Context:
Ulnar collateral ligament (UCL) injuries lead to pain and loss of performance in the thrower’s elbow. Ulnar collateral ligament reconstruction (UCLR) is a reliable treatment option for the symptomatic, deficient UCL. Injury to the UCL usually occurs because of chronic accumulation of microtrauma, although acute ruptures occur and an acute-on-chronic presentation is also common.
Evidence Acquisition:
Computerized databases, references from pertinent articles, and research institutions were searched for all studies using the search terms ulnar collateral ligament from 1970 until 2015.
Study Design:
Clinical review.
Level of Evidence:
Level 5.
Results:
All studies reporting outcomes for UCLR are level 4. Most modern fixation methodologies appear to be biomechanically and clinically equivalent. Viable graft choices include ipsilateral palmaris longus tendon autograft, gracilis or semitendinosus autograft, and allograft. Clinical studies report excellent outcomes of UCLR for both recreational and elite level athletes with regard to return to sport and postoperative performance. Complications, although rare, include graft rerupture or attenuation, ulnar nerve symptoms, stiffness, pain, and/or weakness leading to decreased performance.
Conclusion:
Injuries to the UCL have become commonplace among pitchers. Nonoperative treatment should be attempted, but the limited studies have not shown promising results. Operative treatment can be performed with several techniques, with retrospective studies showing promising results. Complications include ulnar neuropathy as well as failure to return to sport. Detailed preoperative planning, meticulous surgical technique, and a comprehensive rehabilitation program are essential components to achieving a satisfactory result.
Keywords: ulnar collateral ligament reconstruction, Tommy John, elbow, surgical management, biomechanics, instability, throwing athlete, pitcher
Epidemiology of Medial Elbow Pain and Ulnar Collateral Ligament Reconstruction
Medial elbow pain is common among baseball pitchers and can also be seen in gymnasts, javelin throwers, wrestlers, quarterbacks, and offensive linemen.18,20,33,34,64 In collegiate pitchers, elbow injuries are the most common cause of time loss (over 10 days).14 Among National Collegiate Athletic Association (NCAA) baseball players, the upper extremity accounts for 45% of all injuries, with the elbow accounting for 7% to 8% of injuries.14 More than 97% of elbow pain in pitchers is located medially.10
Ulnar collateral ligament (UCL) deficiency is rapidly increasing in incidence. The number of Major League Baseball (MLB) pitchers who have undergone ulnar collateral ligament reconstruction (UCLR) significantly increased between 1986 and 2012.22 Revision surgery, although rare, is also beginning to occur in MLB pitchers and other athletes.19,32 Unfortunately, the results of revision UCLR are not as predictable as primary UCLR, with lower return-to-sport rates seen in MLB pitchers.42 However, more concerning is the evolution to high school pitchers. For instance, in a single surgeon’s series there was an 11-fold increase in UCLR performed in high school pitchers between 1988 and 2003.53
Historical Perspective
The initial technique by Jobe et al31 for UCLR involved an elevation of the flexor muscles off the medial epicondyle and submuscular transposition of the ulnar nerve. Drill holes (3.2 mm) were created in the ulna (2 holes) and medial epicondyle (3 holes) to mimic the attachment points of the native UCL, and a donor tendon (palmaris longus) was passed in a figure-of-8 configuration and sutured to itself.12 With the initial Jobe technique, >60% of elite throwing athletes were able to return to their preinjury level of sport (RTS). Although 21% of these patients developed postoperative ulnar neuropathy, these all resolved within 7 years.12 Since the initial technique described by Jobe et al,31 the technique has undergone several modifications of the approach to the flexor-pronator mass and ulnar nerve, fixation, graft type, and configuration (Table 1 in Appendix 1, available at http://sph.sagepub.com/content/by/supplemental-data).3,12,16,25,27-29,36,43,45,56,61
Applied Surgical Anatomy/Biomechanics
Soft Tissue Restraints
Soft tissue restraints afford 50% of elbow stability and can be broken down into dynamic muscular restraints and static ligamentous restraints.37,52 For valgus instability, the main dynamic stabilizer is the flexor-pronator mass and the main static stabilizers are the UCL and the medial joint capsule.37,52 Cadaveric studies demonstrate that within the flexor-pronator mass, the flexor carpi ulnaris provides the most significant contribution to resisting valgus stress, followed by the flexor digitorum superficialis, with the pronator teres contributing the least dynamic valgus restraint.37,52 The UCL is a dynamic structure that undergoes hypertrophy with training; the mean thickness of the UCL was 6.2 ± 1.6 mm in the throwing arm compared with 4.8 ± 1.3 mm on the nonthrowing arm (P < 0.001).11
The UCL is composed of 3 separate bundles: anterior (the primary restraint to valgus restraint and the most commonly injured bundle), posterior, and transverse, with a mean length of 4.7 to 5.4 cm (Figure 1, A and B).23,59,62 The anterior bundle is composed of 2 distinct bands: the anterior band, which is taut and serves as the primary valgus stabilizer from 30° to 90° of flexion, and the posterior band, which is taut and serves as the primary stabilizer from 90° to 120° of flexion.9,46,59 It is fan-shaped and originates on the medial epicondyle of the humerus and inserts onto the medial aspect of the semilunar notch of the ulna. Finally, the transverse bundle is variably present, originates from the medial olecranon, and inserts onto the inferomedial aspect of the coronoid process. It does not cross the elbow joint and affords no support to valgus stress.10
Figure 1.
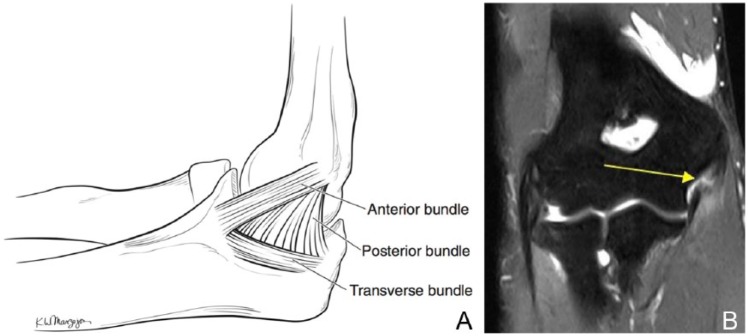
(A) Anatomy of the ulnar collateral ligament (UCL). (B) Magnetic resonance image demonstrating a tear of the UCL at the tip of the arrow.
Elbow Throwing Biomechanics
During the late cocking and early acceleration phases, the medial elbow experiences significant force—approximately 64 N•m—and the UCL is most vulnerable to injury.24 Because the elbow is usually at 90° to 100° of flexion, the posterior band of the anterior bundle of the UCL is the most critical stabilizer. Eccentric contraction within the flexor pronator mass also serves to resist this valgus force, but >50% of the valgus load is transmitted through the UCL, correlating with stresses greater than 32 N•m.15,46 The mean ultimate load to failure for a native UCL is 34.29 N•m and for a reconstructed UCL is 30.55 N•m; thus, the stress placed on the UCL during the late cocking phase of every pitch is nearly sufficient to cause a UCL tear.2,46
Many of the overall biomechanical concepts are the same for the overhead throwing motions of football, javelin, and other sports, although some differences exist. In football, quarterbacks tend to flex their elbow more in the cocking phase and undergo an abbreviated follow-through phase to avoid contact between their hand and arm and another player. This abbreviated deceleration phase in quarterbacks reduces the torque on the elbow, thereby protecting the UCL from injury.38 Javelin throwers have a similar overall motion but with a prolongation of the acceleration phase, which occurs between foot strike and javelin release and is termed the “thrust” phase, to produce increased distance throws.18,47 The tennis serve is also akin to a baseball throw, making the elbow vulnerable during this phase of tennis.
Clinical Evaluation
History
It is imperative to determine how long the patient has had pain, the point in the pitch cycle that causes pain, whether there has been a change in pitching velocity or accuracy, and whether the patient has any mechanical symptoms. The athlete may also complain of changes in stamina and strength of their throws.8,12 Pitchers often complain of pain during the acceleration phase (85%), while some also complain of pain during the follow-through phase (25%).12 Ulnar nerve symptoms must be closely evaluated since chronic UCL injuries are associated with ulnar neuropathy.71
Physical Examination
A thorough examination of the medial elbow structures is imperative. The examiner should check to see whether the patient has a palmaris longus on either arm by having the patient flex his or her wrist and oppose the thumb and small finger. Evaluation of bilateral shoulder rotational range of motion for glenohumeral internal rotation deficit (GIRD) is a critical part of the examination.17,26 Elbow flexion contractures and pain at terminal extension are common among pitchers secondary to posterior osteophytes (seen in up to 65% of pitchers who undergo elbow surgery),3 likely caused by valgus extension overload syndrome (VEOS). A variety of specialized tests for the UCL have been developed (Figures 2-4), with accompanying videos available online (see video supplements, available at http://sph.sagepub.com/content/by/supplemental-data). Other provocative tests include the Tinel test at the cubital tunnel for ulnar nerve irritability and resisted forearm pronation for medial epicondylitis.31,71
Figure 2.
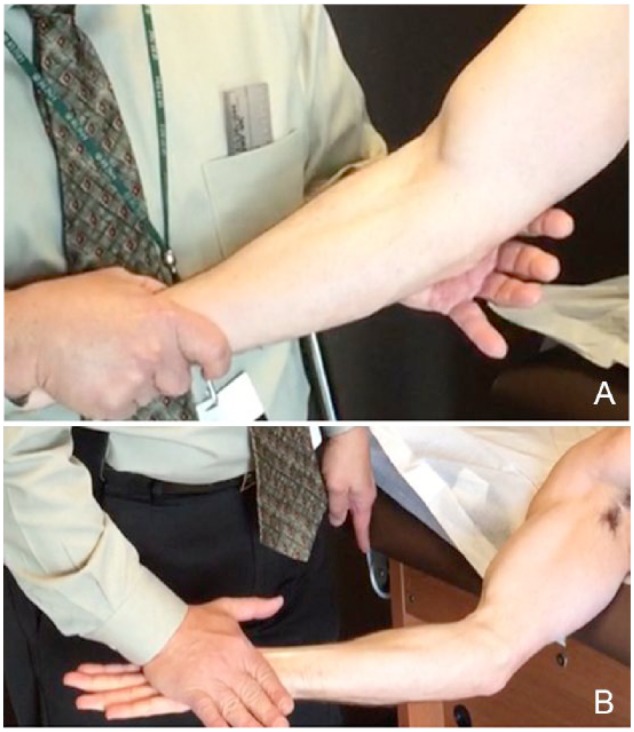
Valgus stress test. The anterior bundle of the ulnar collateral ligament (UCL) is the primary restraint to valgus stress about the elbow. The valgus stress test is used to evaluate the anterior bundle of the UCL and is performed with the patient sitting or supine and the forearm held between the examiner’s trunk and forearm. This is similar to a varus/valgus stress test of the knee. The patient is placed in a (A) standing or (B) supine position. The elbow is flexed to 20° to 30°, which removes the osseous constraint of the ulnohumeral joint, and a valgus stress is applied. During this maneuver, the examiner palpates along the course of the UCL, with tenderness or laxity without a firm endpoint indicating a UCL injury. A small side-to-side difference in laxity can be normal in pitchers11,21 (see Video 1, available at http://sph.sagepub.com/content/by/supplemental-data).
Figure 3.

Milking maneuver. This test evaluates the posterior band of the anterior bundle of the ulnar collateral ligament (UCL) and is performed with the forearm supinated, shoulder extended and externally rotated, and elbow flexed at 90°. The examiner pulls the patient’s thumb, thereby generating a valgus stress at the elbow. Pain and apprehension with the maneuver is indicative of a UCL injury.71 Video supplement available online (Video 2, available at http://sph.sagepub.com/content/by/supplemental-data).
Figure 4.

Moving valgus stress test. This test is performed with the shoulder abducted to 75°. The examiner maximally flexes the elbow and externally rotates the shoulder and exerts a constant valgus load to the elbow as the elbow is extended quickly to 30°. The test, reported to be 100% sensitive and 75% specific, is positive when the pain generated during the examination mimics the medial elbow pain on throwing and when the pain is most significant between 120° and 70° (referred to as the shear range) as the elbow is extended. This correlates with the late cocking/early accelerations phases50 (Video 3, available at http://sph.sagepub.com/content/by/supplemental-data).
Imaging Studies
Stress views have been described in which a progressive valgus stress is applied and the degree of joint widening measured, with a difference of 1 to 3 mm from the contralateral side suggestive of UCL injury.59,71 However, interpretation of these views is unclear, as normal, asymptomatic pitchers can have increased gapping of the medial joint of their dominant elbow.11,21
The UCL is best visualized on more advanced imaging such as magnetic resonance imaging (MRI), magnetic resonance arthrography (MRA), and ultrasound.5,41 Sensitivity and specificity for diagnosis of UCL injuries of computed tomography arthrography (CTA) is 86% and 91%, and of MRI is 57% and 100%, respectively.63 MRA has a sensitivity of 92% and specificity of 100% and has the best interobserver reliability.9,60 While a healthy UCL has a low signal intensity on T1,48 an injured UCL will show a fluid-like, bright, high signal intensity on fat-suppressed T2-weighted images (see Figure 1). MRI studies have demonstrated that the UCL is injured more frequently at its origin on the medial epicondyle.35,54 MRI may also be prognostic: Retrospective studies suggest that a UCL with a higher T2 signal intensity is less likely to respond to conservative treatment.35 A reconstructed UCL may have a variable appearance on MRI.67
Treatment
Nonoperative
Although widely used, few studies have been published regarding nonoperative treatment. In a retrospective review of 20 pitchers, 9 infielders, and 2 javelin throwers, a 42% rate of return to sport was found with nonoperative treatment at a mean 24.5 weeks from the date of diagnosis.55 Their treatment regimen consisted of 2 phases: Phase 1 involved rest from pitching for 2 to 3 months, daily icing of the elbow, anti-inflammatory medications, a splint or brace at night, and therapy with range of motion of the flexors and pronators. Once a pain-free elbow is achieved, phase 2 begins, which consists of strengthening, progressive return to throwing over 3 months, and a hyperextension brace, if needed.
Surgical Indications
The primary surgical indication is failure of an exhaustive attempt at nonoperative treatment, with significant dysfunction and persistent medial elbow pain coupled with a desire to return to competition at the same or higher level. Patients with MRI-documented complete UCL ruptures secondary to an acute event can be offered surgery earlier on. Contraindications include inability or unwillingness to complete the rigorous postoperative rehabilitation program and significant ulnotrochlear or radiocapitellar arthritis. Recent evidence has shown that, in the college and adolescent athlete with a normal quality UCL and a UCL injury isolated to the proximal and/or distal end, UCL repair is an option, with an RTS rate of 97% and a failure rate of 6.7%.58 UCLR should never be offered as a performance enhancer to improve velocity, accuracy, or stamina as the procedure has risks and is unpredictable with regard to these outcomes.
Surgical Techniques
Many variations on the original Jobe technique for UCLR have been proposed and are outlined in the Appendix (see Table 1 [Appendix 1] and Appendix 2).3,12,16,27-29,31,43,45,56,61 Each of these techniques is performed in the supine position on an arm board with a tourniquet (Figure 5A and B). The main differences between techniques involve treatment of the ulnar nerve, graft configuration, and how the graft is attached to the ulna and medial epicondyle. No studies have shown a clear benefit of one technique over another, although studies directly comparing various surgical techniques are lacking.65
Figure 5.
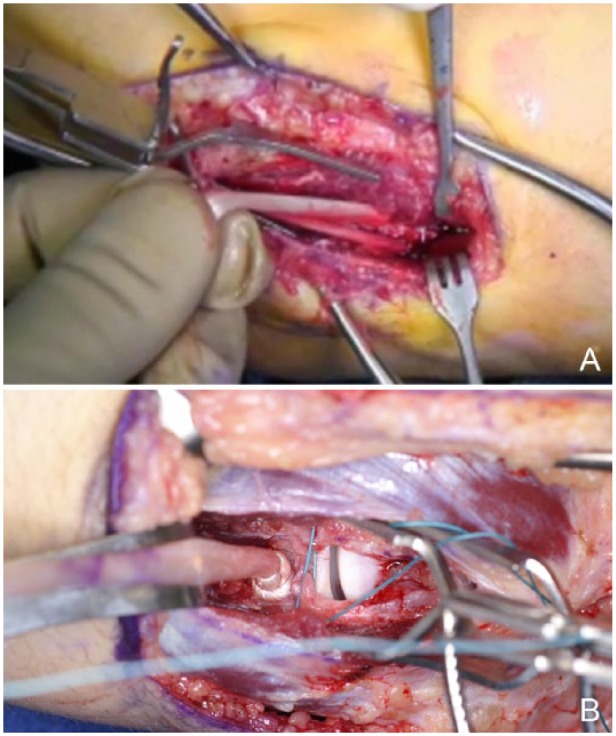
(A) Intraoperative photograph demonstrating the standard docking technique. The graft has been passed through a tunnel created in the ulna and is being prepared to be docked into the medial epicondyle. Notice the 2 strands of the palmaris longus autograft that are available to be docked into the medial epicondyle. A cricket is used to maintain exposure. (B) Intraoperative photograph demonstrating the double-docking technique. The hamstring autograft has been docked into the ulna and is being prepared to be docked into the medial epicondyle. Notice the gapping present at the ulnohumeral joint, indicating an incompetent ulnar collateral ligament.
Graft Choices
While studies have shown that palmaris longus autograft is the most common graft used in UCLR (50%-74%), there have been no studies to date that have clearly shown 1 graft is superior to another.7,16,57,65 Graft choices for UCLR include either gracilis or semitendinosus autograft, toe extensor autograft, plantaris autograft, patellar tendon autograft, Achilles autograft, or allograft.7,27,57 Recent biomechanical evidence has shown that an increase in graft diameter does not effect valgus stability of the elbow.13
Postoperative Rehabilitation
Phase 1 (weeks 0-3) aims to promote healing while preventing stiffness. The elbow is immobilized for the first week and then gentle range of motion (ROM) is started in a hinged elbow brace from 30° to 100° for week 2 and 15° to 110° for week 3 postoperatively. Generally, ROM goals are increased by 5° of extension and 10° of flexion each week until full ROM is achieved. The brace is generally discontinued at 6 weeks postoperatively.
Phase 2 (weeks 4-8) aims to restore strength. While ROM continues to progress and to focus on achieving full elbow extension, the athlete begins exercises with 1-pound weights, increasing by 1 pound per week. Exercises focus on the elbow, shoulder, and scapular stabilizers.68-70
Phase 3 (weeks 9-13) aims to restore more comprehensive upper extremity neuromuscular function. The main focus is on flexibility. Isotonic and manual resistance exercises are begun, along with proprioception and dynamic stabilization drills. At 12 weeks, athletes begin a sport-specific plyometric program. Proper throwing mechanics are emphasized during this phase.
Phase 4, the final stage from weeks 14 to 26, aims to restore throwing specifically. Athletes begin a throwing progression with short toss (throws of 45 feet) and gradually progresses to lofted long toss (throws of 120 feet), followed by long toss throws on a line. The athlete then throws from their knees to isolate the arm. The final progression is to throw from the mound, game-simulation throwing, and finally, return to competition.
The entire rehabilitation process can take a variable amount of time based on the player and any concomitant pathology. Generally, players can begin competitive throwing at 7 to 9 months. For most athletes, it takes significantly longer before they are game ready, with many taking between 10 and 18 months.22
Surgical Outcomes
Surgical outcomes from the literature are listed in Table 2 (see Appendix 1).6,7,16,18,33,44,49,51,57 Despite the public opinion that pitchers who undergo UCLR throw harder after surgery, evidence has shown that pitchers either maintain the same or lose a very small amount of velocity.1,30 Unfortunately, no studies to date have shown a benefit to routine ulnar nerve transposition versus transposition in symptomatic patients. Similarly, the ideal time to return to sport has yet to be identified.
On the whole, no technique or graft choice appears to be consistently biomechanically superior.29,39,40,45 A recent systematic review of 21 biomechanical and clinical studies including 1368 patients concluded that the docking technique resulted in a higher rate of return to play and lower complication rate compared with both the Jobe and modified Jobe techniques.66 Comparative clinical studies regarding graft choice are not available.
Unfortunately, there is no standard to determine whether a pitcher has successfully returned to baseball after UCLR. Most studies to date have evaluated various statistical and sabermetric parameters and have shown mixed results.22 Studies have shown that 83% of MLB pitchers are able to RTS after UCLR.22 MLB pitchers tend to pitch fewer innings, throw fewer complete games, and have fewer wins per season. However, MLB pitchers also have a less walks plus hits per inning pitched (WHIP), fewer home runs given up, fewer walks given up, and a lower earned run average (ERA).22 Hence, while a UCL tear is no longer a career-ending injury, pitchers should understand their ability to RTS is not 100%.
Complications/Pearls to Prevent Complications
Complication rates range from 8.8% to 40% based on patient selection and previous surgeries.4,19 Complications include graft harvest site pain or paresthesias (4%),4,53 synovitis (7%),19 elbow stiffness (13%),19 ulnar neuropathy (26%),12 medial epicondyle avulsion fracture (0.5%),7 and reoperation (2%).4 A meticulous graft harvest, careful dissection and protection of the ulnar nerve, early postoperative ROM, and proper rehabilitation can help reduce complication rates.
Conclusion
Injuries to the ulnar collateral ligament have become commonplace among pitchers. Nonoperative treatment should be attempted, but limited studies have not shown promising results. Operative treatment can be performed in a variety of manners, with retrospective studies showing promising results. Complications include ulnar neuropathy as well as failure to return to sport. Detailed preoperative planning, meticulous surgical technique, and a comprehensive rehabilitation program are essential components to achieving a satisfactory result.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
The following authors declared potential conflicts of interest: Bernard R. Bach Jr, MD, had grants/grants pending from Arthrex, Conmed, DJO, Ossur, Smith & Nephew, and Tornier and received royalties from SLACK. Nikhil N. Verma, MD, has grants/grants pending from Arthrex, Arthrosurface, DJO, Smith & Nephew, Athletico, and Conmed; receives royalties from Smith & Nephew and Vindico; and has stock/stock options from Omeros, Minivasive, and Cymedica. Charles A. Bush-Joseph, MD, is a paid consultant and lecturer for Arthrex; has grants/grants pending from DJO, Ossur, Smith & Nephew, and Arthrex; and receives royalties from Saunders/Mosby.
References
- 1. Ahmad CS, Grantham WJ, Greiwe RM. Public perceptions of Tommy John surgery. Phys Sportsmed. 2012;40:64-72. [DOI] [PubMed] [Google Scholar]
- 2. Ahmad CS, Lee TQ, ElAttrache NS. Biomechanical evaluation of a new ulnar collateral ligament reconstruction technique with interference screw fixation. Am J Sports Med. 2003;31:332-337. [DOI] [PubMed] [Google Scholar]
- 3. Andrews JR, Timmerman LA. Outcome of elbow surgery in professional baseball players. Am J Sports Med. 1995;23:407-413. [DOI] [PubMed] [Google Scholar]
- 4. Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28:16-23. [DOI] [PubMed] [Google Scholar]
- 5. Bica D, Armen J, Kulas AS, Youngs K, Womack Z. Reliability and precision of stress sonography of the ulnar collateral ligament. J Ultrasound Med. 2015;34:371-376. [DOI] [PubMed] [Google Scholar]
- 6. Bowers AL, Dines JS, Dines DM, Altchek DW. Elbow medial ulnar collateral ligament reconstruction: clinical relevance and the docking technique. J Shoulder Elbow Surg. 2010;19(suppl):110-117. [DOI] [PubMed] [Google Scholar]
- 7. Cain EL, Jr, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38:2426-2434. [DOI] [PubMed] [Google Scholar]
- 8. Cain EL, Jr, Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31:621-635. [DOI] [PubMed] [Google Scholar]
- 9. Callaway GH, Field LD, Deng XH, et al. Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg Am. 1997;79:1223-1231. [DOI] [PubMed] [Google Scholar]
- 10. Carrino JA, Morrison WB, Zou KH, Steffen RT, Snearly WN, Murray PM. Noncontrast MR imaging and MR arthrography of the ulnar collateral ligament of the elbow: prospective evaluation of two-dimensional pulse sequences for detection of complete tears. Skeletal Radiol. 2001;30:625-632. [DOI] [PubMed] [Google Scholar]
- 11. Chen FS, Rokito AS, Jobe FW. Medial elbow problems in the overhead-throwing athlete. J Am Acad Orthop Surg. 2001;9:99-113. [DOI] [PubMed] [Google Scholar]
- 12. Ciccotti MG, Atanda A, Jr, Nazarian LN, Dodson CC, Holmes L, Cohen SB. Stress sonography of the ulnar collateral ligament of the elbow in professional baseball pitchers: a 10-year study. Am J Sports Med. 2014;42:544-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74:67-83. [PubMed] [Google Scholar]
- 14. Dargel J, Kupper F, Wegmann K, Oppermann J, Eysel P, Muller LP. Graft diameter does not influence primary stability of ulnar collateral ligament reconstruction of the elbow. J Orthop Sci. 2015;20:307-313. [DOI] [PubMed] [Google Scholar]
- 15. Dick R, Sauers EL, Agel J, et al. Descriptive epidemiology of collegiate men’s baseball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42:183-193. [PMC free article] [PubMed] [Google Scholar]
- 16. Dines JS, ElAttrache NS, Conway JE, Smith W, Ahmad CS. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med. 2007;35:2039-2044. [DOI] [PubMed] [Google Scholar]
- 17. Dines JS, Frank JB, Akerman M, Yocum LA. Glenohumeral internal rotation deficits in baseball players with ulnar collateral ligament insufficiency. Am J Sports Med. 2009;37:566-570. [DOI] [PubMed] [Google Scholar]
- 18. Dines JS, Jones KJ, Kahlenberg C, Rosenbaum A, Osbahr DC, Altchek DW. Elbow ulnar collateral ligament reconstruction in javelin throwers at a minimum 2-year follow-up. Am J Sports Med. 2012;40:148-151. [DOI] [PubMed] [Google Scholar]
- 19. Dines JS, Yocum LA, Frank JB, ElAttrache NS, Gambardella RA, Jobe FW. Revision surgery for failed elbow medial collateral ligament reconstruction. Am J Sports Med. 2008;36:1061-1065. [DOI] [PubMed] [Google Scholar]
- 20. Dodson CC, Slenker N, Cohen SB, Ciccotti MG, DeLuca P. Ulnar collateral ligament injuries of the elbow in professional football quarterbacks. J Shoulder Elbow Surg. 2010;19:1276-1280. [DOI] [PubMed] [Google Scholar]
- 21. Ellenbecker TS, Mattalino AJ, Elam EA, Caplinger RA. Medial elbow joint laxity in professional baseball pitchers. A bilateral comparison using stress radiography. Am J Sports Med. 1998;26:420-424. [DOI] [PubMed] [Google Scholar]
- 22. Erickson BJ, Gupta AK, Harris JD, et al. Rate of return to pitching and performance after Tommy John surgery in Major League Baseball pitchers. Am J Sports Med. 2014;42:536-543. [DOI] [PubMed] [Google Scholar]
- 23. Farrow LD, Mahoney AJ, Stefancin JJ, Taljanovic MS, Sheppard JE, Schickendantz MS. Quantitative analysis of the medial ulnar collateral ligament ulnar footprint and its relationship to the ulnar sublime tubercle. Am J Sports Med. 2011;39:1936-1941. [DOI] [PubMed] [Google Scholar]
- 24. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233-239. [DOI] [PubMed] [Google Scholar]
- 25. Furukawa K, Pichora J, Steinmann S, Faber KJ, Johnson JA, King GJ. Efficacy of interference screw and double-docking methods using palmaris longus and GraftJacket for medial collateral ligament reconstruction of the elbow. J Shoulder Elbow Surg. 2007;16:449-453. [DOI] [PubMed] [Google Scholar]
- 26. Garrison JC, Cole MA, Conway JE, Macko MJ, Thigpen C, Shanley E. Shoulder range of motion deficits in baseball players with an ulnar collateral ligament tear. Am J Sports Med. 2012;40:2597-2603. [DOI] [PubMed] [Google Scholar]
- 27. Hechtman KS, Zvijac JE, Wells ME, Botto-van Bemden A. Long-term results of ulnar collateral ligament reconstruction in throwing athletes based on a hybrid technique. Am J Sports Med. 2011;39:342-347. [DOI] [PubMed] [Google Scholar]
- 28. Jackson A, Maerz T, Koueiter DM, Andrecovich CJ, Baker KC, Anderson K. Strength of ulnar fixation in ulnar collateral ligament reconstruction: a biomechanical comparison of traditional bone tunnels to the tension-slide technique. J Shoulder Elbow Surg. 2012;21:1674-1679. [DOI] [PubMed] [Google Scholar]
- 29. Jackson TJ, Adamson GJ, Peterson A, Patton J, McGarry MH, Lee TQ. Ulnar collateral ligament reconstruction using bisuspensory fixation: a biomechanical comparison with the docking technique. Am J Sports Med. 2013;41:1158-1164. [DOI] [PubMed] [Google Scholar]
- 30. Jiang JJ, Leland JM. Analysis of pitching velocity in Major League Baseball players before and after ulnar collateral ligament reconstruction. Am J Sports Med. 2014;42:880-885. [DOI] [PubMed] [Google Scholar]
- 31. Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68:1158-1163. [PubMed] [Google Scholar]
- 32. Jones KJ, Conte S, Patterson N, ElAttrache NS, Dines JS. Functional outcomes following revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. J Shoulder Elbow Surg. 2013;22:642-646. [DOI] [PubMed] [Google Scholar]
- 33. Jones KJ, Dines JS, Rebolledo BJ, et al. Operative management of ulnar collateral ligament insufficiency in adolescent athletes. Am J Sports Med. 2014;42:117-121. [DOI] [PubMed] [Google Scholar]
- 34. Kenter K, Behr CT, Warren RF, O’Brien SJ, Barnes R. Acute elbow injuries in the National Football League. J Shoulder Elbow Surg. 2000;9:1-5. [DOI] [PubMed] [Google Scholar]
- 35. Kim NR, Moon SG, Ko SM, Moon WJ, Choi JW, Park JY. MR imaging of ulnar collateral ligament injury in baseball players: value for predicting rehabilitation outcome. Eur J Radiol. 2011;80:e422-e426. [DOI] [PubMed] [Google Scholar]
- 36. Koh JL, Schafer MF, Keuter G, Hsu JE. Ulnar collateral ligament reconstruction in elite throwing athletes. Arthroscopy. 2006;22:1187-1191. [DOI] [PubMed] [Google Scholar]
- 37. Lin F, Kohli N, Perlmutter S, Lim D, Nuber GW, Makhsous M. Muscle contribution to elbow joint valgus stability. J Shoulder Elbow Surg. 2007;16:795-802. [DOI] [PubMed] [Google Scholar]
- 38. Loftice J, Fleisig GS, Zheng N, Andrews JR. Biomechanics of the elbow in sports. Clin Sports Med. 2004;23:519-530. [DOI] [PubMed] [Google Scholar]
- 39. Lynch JL, Maerz T, Kurdziel MD, Davidson AA, Baker KC, Anderson K. Biomechanical evaluation of the TightRope versus traditional docking ulnar collateral ligament reconstruction technique: kinematic and failure testing. Am J Sports Med. 2013;41:1165-1173. [DOI] [PubMed] [Google Scholar]
- 40. Lynch JL, Pifer MA, Maerz T, et al. The GraftLink ulnar collateral ligament reconstruction: biomechanical comparison with the docking technique in both kinematics and failure tests. Am J Sports Med. 2013;41:2278-2287. [DOI] [PubMed] [Google Scholar]
- 41. Magee T. Accuracy of 3-T MR arthrography versus conventional 3-T MRI of elbow tendons and ligaments compared with surgery. AJR Am J Roentgenol. 2015;204:W70-W75. [DOI] [PubMed] [Google Scholar]
- 42. Marshall NE, Keller RA, Lynch JR, Bey MJ, Moutzouros V. Pitching performance and longevity after revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2015;43:1051-1056. [DOI] [PubMed] [Google Scholar]
- 43. McGraw MA, Kremchek TE, Hooks TR, Papangelou C. Biomechanical evaluation of the docking plus ulnar collateral ligament reconstruction technique compared with the docking technique. Am J Sports Med. 2013;41:313-320. [DOI] [PubMed] [Google Scholar]
- 44. Merolla G, Del Sordo S, Paladini P, Porcellini G. Elbow ulnar collateral ligament reconstruction: clinical, radiographic, and ultrasound outcomes at a mean 3-year follow-up. Musculoskelet Surg. 2014;98:87-93. [DOI] [PubMed] [Google Scholar]
- 45. Morgan RJ, Starman JS, Habet NA, et al. A biomechanical evaluation of ulnar collateral ligament reconstruction using a novel technique for ulnar-sided fixation. Am J Sports Med. 2010;38:1448-1455. [DOI] [PubMed] [Google Scholar]
- 46. Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11:315-319. [DOI] [PubMed] [Google Scholar]
- 47. Morriss C, Bartlett R. Biomechanical factors critical for performance in the men’s javelin throw. Sports Med. 1996;21:438-446. [DOI] [PubMed] [Google Scholar]
- 48. Munshi M, Pretterklieber ML, Chung CB, et al. Anterior bundle of ulnar collateral ligament: evaluation of anatomic relationships by using MR imaging, MR arthrography, and gross anatomic and histologic analysis. Radiology. 2004;231:797-803. [DOI] [PubMed] [Google Scholar]
- 49. O’Brien DF, O’Hagan T, Stewart R, et al. Outcomes for ulnar collateral ligament reconstruction: a retrospective review using the KJOC assessment score with two-year follow-up in an overhead throwing population. J Shoulder Elbow Surg. 2015;24:934-940. [DOI] [PubMed] [Google Scholar]
- 50. O’Driscoll SW, Lawton RL, Smith AM. The “moving valgus stress test” for medial collateral ligament tears of the elbow. Am J Sports Med. 2005;33:231-239. [DOI] [PubMed] [Google Scholar]
- 51. Osbahr DC, Cain EL, Jr, Raines BT, Fortenbaugh D, Dugas JR, Andrews JR. Long-term outcomes after ulnar collateral ligament reconstruction in competitive baseball players: minimum 10-year follow-up. Am J Sports Med. 2014;42:1333-1342. [DOI] [PubMed] [Google Scholar]
- 52. Park MC, Ahmad CS. Dynamic contributions of the flexor-pronator mass to elbow valgus stability. J Bone Joint Surg Am. 2004;86-A:2268-2274. [DOI] [PubMed] [Google Scholar]
- 53. Petty DH, Andrews JR, Fleisig GS, Cain EL. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med. 2004;32:1158-1164. [DOI] [PubMed] [Google Scholar]
- 54. Podesta L, Crow SA, Volkmer D, Bert T, Yocum LA. Treatment of partial ulnar collateral ligament tears in the elbow with platelet-rich plasma. Am J Sports Med. 2013;41:1689-1694. [DOI] [PubMed] [Google Scholar]
- 55. Rettig AC, Sherrill C, Snead DS, Mendler JC, Mieling P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med. 2001;29:15-17. [DOI] [PubMed] [Google Scholar]
- 56. Rohrbough JT, Altchek DW, Hyman J, Williams RJ, 3rd, Botts JD. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med. 2002;30:541-548. [DOI] [PubMed] [Google Scholar]
- 57. Savoie FH, 3rd, Morgan C, Yaste J, Hurt J, Field L. Medial ulnar collateral ligament reconstruction using hamstring allograft in overhead throwing athletes. J Bone Joint Surg Am. 2013;95:1062-1066. [DOI] [PubMed] [Google Scholar]
- 58. Savoie FH, 3rd, Trenhaile SW, Roberts J, Field LD, Ramsey JR. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med. 2008;36:1066-1072. [DOI] [PubMed] [Google Scholar]
- 59. Schwab GH, Bennett JB, Woods GW, Tullos HS. Biomechanics of elbow instability: the role of the medial collateral ligament. Clin Orthop Relat Res. 1980;(146):42-52. [PubMed] [Google Scholar]
- 60. Schwartz ML, al-Zahrani S, Morwessel RM, Andrews JR. Ulnar collateral ligament injury in the throwing athlete: evaluation with saline-enhanced MR arthrography. Radiology. 1995;197:297-299. [DOI] [PubMed] [Google Scholar]
- 61. Thompson WH, Jobe FW, Yocum LA, Pink MM. Ulnar collateral ligament reconstruction in athletes: muscle-splitting approach without transposition of the ulnar nerve. J Shoulder Elbow Surg. 2001;10:152-157. [DOI] [PubMed] [Google Scholar]
- 62. Timmerman LA, Andrews JR. Histology and arthroscopic anatomy of the ulnar collateral ligament of the elbow. Am J Sports Med. 1994;22:667-673. [DOI] [PubMed] [Google Scholar]
- 63. Timmerman LA, Schwartz ML, Andrews JR. Preoperative evaluation of the ulnar collateral ligament by magnetic resonance imaging and computed tomography arthrography. Evaluation in 25 baseball players with surgical confirmation. Am J Sports Med. 1994;22:26-31. [DOI] [PubMed] [Google Scholar]
- 64. Tullos HS, Erwin WD, Woods GW, Wukasch DC, Cooley DA, King JW. Unusual lesions of the pitching arm. Clin Orthop Relat Res. 1972;88:169-182. [DOI] [PubMed] [Google Scholar]
- 65. Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med. 2008;36:1193-1205. [DOI] [PubMed] [Google Scholar]
- 66. Watson JN, McQueen P, Hutchinson MR. A systematic review of ulnar collateral ligament reconstruction techniques. Am J Sports Med. 2014;42:2510-2516. [DOI] [PubMed] [Google Scholar]
- 67. Wear SA, Thornton DD, Schwartz ML, Weissmann RC, 3rd, Cain EL, Andrews JR. MRI of the reconstructed ulnar collateral ligament. AJR Am J Roentgenol. 2011;197:1198-1204. [DOI] [PubMed] [Google Scholar]
- 68. Wilk KE, Arrigo C, Andrews JR. Rehabilitation of the elbow in the throwing athlete. J Orthop Sports Phys Ther. 1993;17:305-317. [DOI] [PubMed] [Google Scholar]
- 69. Wilk KE, Macrina LC, Cain EL, Dugas JR, Andrews JR. Rehabilitation of the overhead athlete’s elbow. Sports Health. 2012;4:404-414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Wilk KE, Reinold MM, Andrews JR. Rehabilitation of the thrower’s elbow. Tech Hand Up Extrem Surg. 2003;7:197-216. [DOI] [PubMed] [Google Scholar]
- 71. Wilkins KE, Morrey BF, Jobe FW, et al. The elbow. Instr Course Lect. 1991;40:1-87. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


