Abstract
PURPOSE
The correlation between imaging findings and pathologic characteristics of tumors may provide information for diagnosis and treatment of cancer. The aim of this study is to determine whether ultrasound features of breast cancer are associated with molecular subtype, histologic grade, and hormone receptor status, as well as assess the predictive value of these features.
METHODS
A total of 201 consecutive invasive breast cancer patients were reviewed from the database according to the Breast Imaging and Reporting Data System (BI-RADS). Tumor margins were classified as circumscribed and noncircumscribed. Noncircumscribed group was divided into indistinct, spiculated, angular, and microlobulated. The posterior acoustic features were divided into four categories: shadowing, enhancement, no change, and mixed pattern.
RESULTS
Tumors with posterior shadowing were more likely to be of nontriple negative subtype (odds ratio [OR], 7.42; 95% CI, 2.10–24.99; P = 0.002), low histologic grade (grade 1 or 2 vs. grade 3: OR, 2.42; 95% CI, 1.34–4.35; P = 0.003) and having at least one positive receptor (OR, 3.36; 95% CI, 1.55–7.26; P = 0.002). Tumors with circumscribed margins were more often triple-negative subtype (OR, 6.72; 95% CI, 2.56–17.65; P < 0.001), high grade (grade 3 vs. grade 1 or 2: OR, 5.42; 95% CI, 2.66–11.00; P < 0.001) and hormone receptor negative (OR, 4.87; 95% CI, 2.37–9.99; P < 0.001).
CONCLUSION
Sonographic features are strongly associated with molecular subtype, histologic grade, and hormone receptor status of the tumor. These findings may separate triple-negative breast cancer from other molecular subtypes.
Breast cancer is the most common malignant tumor and the major cause of death from cancer among women worldwide. Breast cancer is also a heterogeneous and complex disease with different morphologic, biologic, and molecular characteristics (1). Although histopathologic characteristics of tumors have been used to determine prognosis and treatment of breast cancer, they do not provide sufficient information due to tumor heterogeneity. For this reason, several distinct molecular subtypes of breast cancer have been defined based on gene expression patterns (2). The St. Gallen International Expert Consensus determined a new biologic classification system based on the expression of tumor markers: estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor 2–neu (HER2), and more recently, Ki-67, which are evaluated routinely because of their utility in guiding clinical care. The classification system categorizes invasive breast carcinomas into five molecular subtypes: luminal A, luminal B (HER 2−), luminal B (HER 2+), HER 2, and triple-negative (1–5).
Molecular subtyping of breast cancer is a common practice for individualized cancer management, to understand prognosis of disease and avoid overtreatment. Radiologic imaging has an important role in diagnosis, staging, treatment, and follow-up of patients with breast cancer, and it may also help to predict molecular subtypes of patients with breast cancer for guiding treatment (4, 5). It is important for breast radiologists to understand the differences of these molecular subtypes.
Many studies have already determined the imaging features of breast cancer and a few studies focused on the association between ultrasonography (US) findings, different histologic grades, and hormone receptor status. However, the relationship between US features and molecular subtypes is not clear yet. The prediction of triple-negative molecular sub-type by US may be important for diagnosis, prognosis, treatment, and understanding of the biologic behavior. It may also predict treatment efficacy of breast cancer. The purpose of our study was to investigate whether US features (e.g., tumor margins and posterior acoustic features) of breast cancer are associated with molecular subtypes, histologic grade, and hormone receptor status, as well as assess the predictive value of these features.
Methods
Patients
The US features of 220 consecutive primary invasive breast cancer patients, who were treated and followed up at our breast cancer center between November 2011 and August 2013, were retrospectively evaluated using electronic database. Of 220 patients, 19 patients with treatment of neo-adjuvant chemotherapy, prior cancer history, pregnancy, and bilateral and recurrent breast cancer were excluded. Thirty-three of 201 invasive breast cancers (16.4%) were multifocal; in these cases, the largest lesion was evaluated for the purpose of this study. All patients had histologically proven breast cancer and molecular subtypes from surgical specimens. The study was approved by the institutional review board.
Ultrasonography
US scans were performed with a 13–5 MHz linear transducer (Acuson Antares, Siemens Medical) and evaluated by two breast radiologists who had at least five-year experience on breast imaging. Both radiologists were blinded to the histopathology results. One radiologist assessed the US images of each tumor from the PACS and the soft copy images; the second radiologist was consulted if a case was unclear. All US exams were performed by radiologists, and multiple images were recorded.
Main points
Radiologic imaging has an important role in diagnosis, staging, treatment, and follow-up of patients with breast cancer, and it may also help to predict molecular subtypes of patients with breast cancer for guiding treatment.
The prediction of triple-negative molecular subtype by ultrasonography (US) may be important for diagnosis and management.
Breast US performed by experienced radiologists may also help to predict hormone receptor status.
Sonographic features such as margins and posterior acoustic features were found to be significantly associated with molecular subtype, histologic grade, and hormone receptor status.
US findings of margins and posterior acoustic features were retrospectively analyzed based on the criteria of the breast imaging reporting and data system (BI-RADS) (6, 7).
Posterior acoustic features were divided into four categories: shadowing, enhancement, mixed pattern, and no change. Tumor margins were categorized as circumscribed and noncircumscribed. Noncircumscribed category was divided into subgroups as indistinct, spiculated, angular, and microlobulated. These US findings were then correlated with molecular subtype, histologic grade, and hormone receptor status. Non-circumscribed and circumscribed groups were compared with each other.
Histologic analysis
Histologic grading was based on the modified Scarff-Bloom-Richardson system (8) and classified as: grade 1 (well-differentiated), grade 2 (moderately differentiated) and grade 3 (poorly differentiated). For the purpose of the study, grade 1 and 2 were considered as low grade, whereas grade 3 was considered as high grade. Differentiation between ductal and lobular carcinomas was made using E-cadherin stains in cases of equivocal histologic appearance.
Immunohistochemistry
The expression status of the ER, PR, HER2, and Ki-67 antigen was assessed by an immunohistochemical analysis with antibodies. Breast cancers were classified as hormone receptor-positive and negative and grouped into five molecular subtypes. Cells that had receptors for one of the estrogen or progesterone hormones, or both of them (ER+ and/or PR+), were considered “hormone receptor-positive.” Molecular subtypes were defined as follows: Luminal A: ER+, PR+, HER2−, and low Ki-67 index; luminal B (HER2−): ER+, PR+ or PR−, HER2−, and high Ki-67 index; luminal B (HER2+): ER+, PR+, HER2+; HER2: ER−, PR−, HER2+; and triple-negative: ER−, PR−, HER2−. In our study, the Ki-67 index was scored as high when 14% or more of the tumor cells were immunohistostained in accordance with the St. Gallen International Expert Consensus guidelines (1). Immunohistochemistry results were taken from the reports and recorded.
Statistical analysis
All analyses were performed with the use of statistical software (SPSS, version 17.0; SPSS), with P < 0.05 and 95% CI indicating a significant difference. Logistic regression analyses were used to determine the association between tumor molecular subtype, grade, hormone receptor status, and US features. Distribution of demographic, radiologic, and pathologic findings according to molecular classification were evaluated using Pearson’s chi-square test and Fisher Freeman Halton test with Monte Carlo procedure. Multivariate logistic regression analyses were used to evaluate the association between posterior acoustic changes and tumor margins.
Results
Our study population’s tumor characteristics and US imaging features are shown in Table 1. The mean age at diagnosis was 50±23 years (range, 23–83 years) and the ultrasonographic mean tumor size was 22±14.1 mm. Histologic grade was 1 or 2 in 73 patients (36.3%) and grade 3 in 128 patients (63.7%). Among 201 patients with invasive breast cancer, molecular subtype was luminal A in 58 (28.9%), luminal B in 99 (49.3%), HER2 in 18 (9.0%), and triple-negative in 26 (12.9%). Tumors with hormone receptor-positive status (n=154) were more likely to have noncircumscribed margins (n=108, 70.1%) and tumors with hormone receptor-negative status (n=47) were more likely to have circumscribed margins (n=32, 68.1%) (P < 0.001).
Table 1.
Distribution of demographic, radiologic, and pathologic findings according to molecular classification
| Dependent variables | Independent variables, n (%) | Pa | ||||
|---|---|---|---|---|---|---|
| All cases n=201 | Lum A n=58 | Lum B n=99 | Her2 n=18 | TNBC n=26 | ||
| Age (years) | 0.038 | |||||
| ≤50 | 102 (50.7) | 23 (39.7) | 52 (52.5) | 8 (44.4) | 19 (73.1) | |
| >50 | 99 (49.3) | 35 (60.3) | 47 (47.5) | 10 (55.6) | 7 (26.9) | |
| Menopausal status | 0.189 | |||||
| Premenopausal | 96 (47.8) | 24 (41.4) | 48 (48.5) | 7 (38.9) | 17 (65.4) | |
| Postmenopausal | 105 (52.2) | 34 (58.6) | 51 (51.5) | 11 (61.1) | 9 (34.6) | |
| Sonographic tumor size (mm) | 0.014 | |||||
| <20 | 106 (52.7) | 39 (67.2) | 51 (51.5) | 5 (27.8) | 11 (42.3) | |
| ≥20 | 95 (47.3) | 19 (32.8) | 48 (48.5) | 13 (72.2) | 15 (57.7) | |
| Margins | <0.001 | |||||
| Circumscribed | 78 (38.8) | 17 (29.3) | 31 (31.3) | 10 (55.6) | 20 (76.9) | |
| Noncircumscribed | 123 (61.2) | 41 (70.7) | 68 (68.7) | 8 (44.4) | 6 (23.1) | |
| Posterior acoustic features | 0.041 | |||||
| Shadowing | 88 (43.8) | 29 (50.0) | 49 (49.5) | 7 (38.9) | 3 (11.5) | |
| Mixed | 23 (11.4) | 4 (6.9) | 12 (12.1) | 3 (16.7) | 4 (15.4) | |
| Enhancement | 27 (13.4) | 7 (12.1) | 10 (10.1) | 2 (11.1) | 8 (30.8) | |
| No change | 63 (31.3) | 18 (31.0) | 28 (28.3) | 6 (33.3) | 11 (42.3) | |
| Tumor grade | <0.001 | |||||
| 1 or 2 | 73 (36.3) | 45 (77.6) | 25 (25.3) | 2 (11.1) | 1 (3.8) | |
| 3 | 128 (63.7) | 13 (22.4) | 74 (74.7) | 16 (88.9) | 25 (96.2) | |
Lum A, luminal A breast cancer; Lum B, luminal B breast cancer; Her2, human epidermal growth factor 2–neu; TNBC, triple-negative breast cancer.
Pearson’s chi-square test.
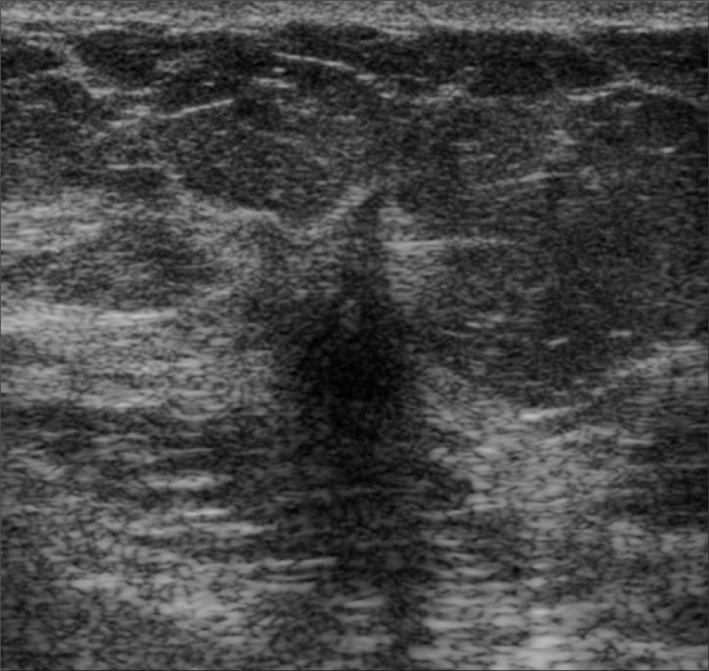
Tumors with posterior shadowing were more likely to be of nontriple-negative subtype (odds ratio [OR], 7.42; 95% CI, 2.10–24.99; P = 0.002), low histologic grade (grade 1 or 2 vs. grade 3: OR, 2.42; 95% CI, 1.34–4.35; P = 0.003), and having at least one positive hormone receptor (OR, 3.36; 95% CI, 1.55–7.26; P = 0.002) (Fig. 1).
Figure 1.
A 55-year-old woman with hormone receptor-positive (luminal B subtype) invasive ductal carcinoma (low grade). US image shows noncircumscribed hypoechoic mass with indistinct margins and posterior acoustic shadowing in the right upper breast.
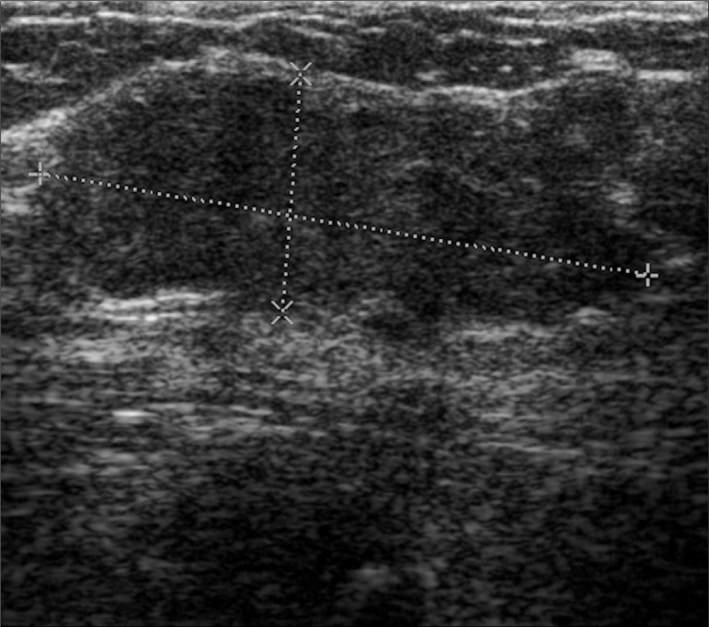
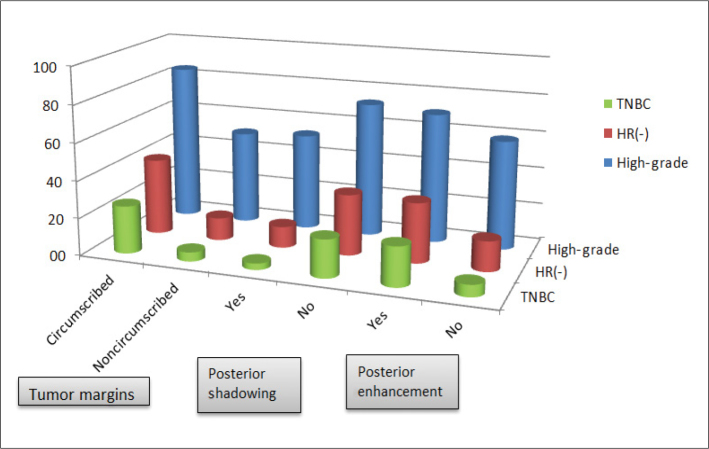
Tumors with circumscribed margins were more often triple-negative subtype (OR, 6.72; 95% CI, 2.56–17.65; P < 0.001), high grade (grade 3 vs. grade 1 or 2: OR, 5.42; 95% CI, 2.66–11.00; P < 0.001) and hormone receptor-negative (OR, 4.87; 95% CI, 2.37–9.99; P < 0.001) (Fig. 2). Tumors with posterior acoustic enhancement were commonly high grade (OR, 1.65, 95% CI, 0.92–2.97) though there was no statistical significance (P =0.095). There was, however, a strong association between posterior enhancement and hormone receptor negativity (OR, 2.46; 95% CI, 1.26–4.8; P = 0.009) and triple negativity (OR, 3.98; 95% CI, 1.59–9.95; P = 0.003). Posterior tumor enhancement and circumscribed margins were together significantly associated with high grade, and they were different from tumors with only posterior acoustic enhancement. This situation increases the likelihood of hormone receptor negativity having a triple-negative status. Together, posterior shadowing and noncircumscribed margins were significantly correlated with low grade, hormone receptor positivity and nontriple-negative subtype (Table 2, Fig. 3).
Figure 2.
A 44-year-old woman with triple-negative invasive ductal carcinoma (high grade). US image shows lobulated, circumscribed hypoechoic mass with posterior enhancement in the left upper breast.
Table 2.
Comparison of US features, hormone receptor status, histologic grade, and molecular subtypes
| US features | Outcome characteristics | OR (95% CI) | P |
|---|---|---|---|
| Circumscribed vs. noncircumscribed | HR− vs. HR+ | 4.87 (2.37–9.99) | <0.001 |
| TNBC vs. Lum A+Lum B+Her2 | 6.72 (2.56–17.65) | <0.001 | |
| High grade tumor | 5.41 (2.66–11.00) | <0.001 | |
| Posterior tumor shadowing vs. no shadowing | HR+ vs. HR − | 3.36 (1.55–7.26) | 0.002 |
| Lum A+Lum B+Her2 vs. TNBC | 7.24 (2.10–24.99) | 0.002 | |
| Low grade tumor | 2.42 (1.34–4.35) | 0.003 | |
| Noncircumscribed margins+shadowing vs. others | HR+ vs. HR− | 4.75 (2.08–10.83) | <0.001 |
| Lum A+Lum B+Her2 vs. TNBC | 10.58 (2.43–46.14) | 0.002 | |
| Low grade tumor | 2.53 (1.40–4.57) | 0.002 | |
| Posterior tumor enhancement vs. no enhancement | HR− vs. HR+ | 2.46 (1.26–4.81) | 0.009 |
| TNBC vs. Lum A+Lum B+Her2 | 3.98 (1.59–9.95) | 0.003 | |
| High grade tumor | 1.65 (0.92–2.97) | 0.095 | |
| Posterior tumor enhancement +circumscribed margins vs. others | HR− vs. HR+ | 3.18 (1.37–7.39) | 0.007 |
| TNBC vs. Lum A+Lum B+Her2 | 3.65 (1.39–9.52) | 0.008 | |
| High grade tumor | 5.39 (1.56–18.57) | 0.008 |
US, ultrasonography; OR, odds ratio; CI, confidence interval; HR, hormone receptor; TNBC, triple-negative breast cancer; Lum A, luminal A breast cancer; Lum B, luminal B breast cancer; Her2, human epidermal growth factor 2–neu.
Logistic regression, P < 0.05.
Figure 3.
Comparison of US features, hormone receptor (HR) status, histologic grade, and molecular subtypes. TNBC, triple negative breast cancer.
In our study most patients had luminal A and luminal B subtypes (78%) and only 13% had triple-negative breast cancer. Luminal A (n=41, 70%) and luminal B (n=68, 68.7%) subtypes were more often associated with noncircumscribed margins. Triple-negative breast cancers often had circumscribed margins (n=20, 76.9%), with only 23% of them having noncircumscribed margins (P < 0.001) (Table 1).
Discussion
Our study showed that sonographic features such as posterior acoustic features and margins were significantly associated with molecular subtype and histologic grade. Luminal A and luminal B subtypes were more often associated with noncircumscribed margins and triple-negative breast cancers commonly had circumscribed margins.
Breast cancer is a heterogeneous disease with different histopathologic and biologic features. Hence, suitable classification is needed for appropriate individual management (9–11). Currently due to the inadequate prognostic power and predictive accuracy of existing classifications, a modified classification according to molecular characteristics of breast cancer was defined by the 13th St. Gallen Breast Cancer Conference to categorize breast cancers into molecular subtypes (1). Despite the lack of a complete overlap among molecular classes and their immunohistochemical status, the St. Gallen Breast Cancer Conference accepted immunohistochemistry as a basic methodology to identify breast cancer subtypes. This new molecular classification may overcome the limitations of previous schemes (9). Most of the patients in our study had luminal A and B molecular subtypes (78%) and only 13% had triple-negative breast cancer.
The use of breast US exam has become an effective method to differentiate benign from malignant lesions, especially in young women with dense breast tissue (12). Although many previous studies have focused on the sonographic appearance of breast cancer according to grade, the same is not true for the association between tumor sub-types (3, 8). We have very limited imaging data with regards to the determination of the sonographic features of molecular subtypes. As compared with hormone receptor-negative status, tumors with hormone receptor-positive status were more likely to have noncircumscribed margins. In our study, tumors with posterior shadowing and noncircumscribed margins were more likely to be of nontriple-negative subtype.
Previously, the majority of malignant breast tumors were expected to have posterior acoustic shadowing at US and have poorly defined spiculated margins (13, 14). However, it is now widely known that many tumors may have variable posterior acoustic features; new studies have shown that well-defined margins and posterior enhancement are more likely to represent higher grade tumors and negative receptor status (13, 15, 16). Our results are consistent with these findings and there is a strong statistically significant correlation between these parameters.
Lacroix et al. (20) determined that grade 1 tumors (low grade) and grade 2 tumors (intermediate grade) show stromal reaction, which results in spicules and perilesional hyperechogenic halo, while grade 3 (high grade) tumors do not develop stromal reaction and have a round shape. Conversely, Lamb et al. (15) found that higher grade tumors are significantly more likely than lower grade ones to show indistinct margins and posterior acoustic enhancement. Rotstein and Neerhut (11) mentioned that grade 3 invasive ductal cancers show the classic feature of acoustic shadowing. These studies did not use BI-RADS lexicon to categorize sonographic features. All these studies showed different results and there was no concordance between them.
The presence of receptors is important for good prognosis and indicates hormone sensitivity. Shin et al. (16) showed that masses with circumscribed margins and posterior acoustic enhancement are associated with high grade and negative hormone status. In our study, similar to these results, tumors with circumscribed margins and posterior enhancement were more likely to be triple-negative, high grade, and hormone-receptor negative. Receptor positivity is associated with an irregular shape and spiculated margins, and it is significantly more frequent than triple-negative cancers (11). Our results are consistent with this finding and a strong relationship was observed between noncircumscribed margins and hormone receptor positivity.
Blaichman et al. (3) determined that triple-negative cancers were almost always high grade at diagnosis and showed posterior enhancement more commonly. Additionally, the presence of shadowing was strongly associated with low grade (about 92% were low grade in their study). Kojima et al. (17) mentioned that triple-negative breast cancers were more likely to be lobulated in shape and having circumscribed margins and less likely to show posterior attenuating. Our results confirm the findings of these studies. Triple-negative breast cancers were likely to be histologically intermediate and high-grade tumors. This trend was the same for patients with ER−/PR−/ HER2+ breast cancers, compared with patients with ER+/PR−/HER2− breast cancers. Although a triple-negative breast cancer may have similar sonographic features to a benign lesion, sonographic imaging recognition can assist in both pretreatment planning and understanding biologic behavior of this entity (18).
The posterior enhancement is seen more often in hormone receptor-negative HER2+ cancers (50%) than hormone receptor-positive HER2− cancers (29%) (16). Triple-negative tumors present with round, oval, and lobular shapes having an indistinct or microlobulated contour (19, 20). Posterior enhancement is determined in 35.5% to 49% of triple-negative cancers and 50% of hormone receptor-negative HER2+ cancers (16, 18). In our study, we did not investigate the enhancement for all subtypes separately; however, posterior acoustic enhancement was more common in the triple-negative subtype than in the other subtypes.
Histopathologic evaluation is an essential requirement for breast cancer diagnosis and treatment. Advanced pathologic procedures including ER, PR, and HER2/neu status are also needed as prognostic and predictive factors. The reliability of hormone receptor status is dependent on tissue handling and processing. These steps can lead to false-negative results if quality control is not sufficient. The issues related to pathology services in low-middle income countries include limited financial resources, limited equipment, as well as inadequate numbers of expert pathologists and technologists (21, 22). Due to these negative factors, hormone receptors are not routinely determined. Our findings suggest that breast US performed by experienced radiologists may help predict the hormone receptor status and molecular subtypes of tumors. In countries without resources for receptor testing, US features may be used to make the decision for hormone therapy.
Our study has many limitations such as its retrospective design, small sample size, and lack of some sonographic features determined in BI-RADS US lexicon. Furthermore, our results cannot completely reflect actual clinical conditions, because the analyses were carried out on selected images rather than images that were acquired during real-time scanning. Despite these limitations, our study provides a new additional insight into US features of breast cancer lesions.
In conclusion, sonographic features such as margins and posterior acoustic features were found to be significantly associated with molecular subtype, histologic grade, and hormone receptor status. Being able to predict the molecular subtype, especially the triple-negative subtype by US might also have an important role for earlier management and treatment. Further work with larger populations and prospective nature are necessary to determine the full potential of US in the evaluation of the molecular subtypes of malignant breast lesions.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Yaganawa M, Ikemot K, Kawauchi S, et al. Luminal A and Luminal B (HER2 negative) subtypes of breast cancer consist of a mixture of tumors with different genotype. BMC Res Notes. 2012;5:376. doi: 10.1186/1756-0500-5-376. http://dx.doi.org/10.1186/1756-0500-5-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Irshad A, Leddy R, Pisano E, et al. Assessing the role of ultrasound in predicting the biological behavior of breast cancer. AJR Am J Roentgenol. 2013;200:284–290. doi: 10.2214/AJR.12.8781. http://dx.doi.org/10.2214/AJR.12.8781. [DOI] [PubMed] [Google Scholar]
- 3.Blaichman J, Marcus JC, Alsaadi T, et al. Sonographic appearance of ductal carcinoma of the breast according to histologic grade. AJR Am J Roentgenol. 2012;199:W402–W408. doi: 10.2214/AJR.11.7374. http://dx.doi.org/10.2214/AJR.11.7374. [DOI] [PubMed] [Google Scholar]
- 4.Reis-Filho JS, Simpson PT, Gale T, et al. Molecular evolution of breast cancer. J Pathol. 2005;205:248–254. doi: 10.1002/path.1691. http://dx.doi.org/10.1002/path.1691. [DOI] [PubMed] [Google Scholar]
- 5.Bosch A, Eroles P, Zaragoza R, et al. Triple negative breast cancer: Molecular features, pathogenesis, treatment and current lines of research. Cancer Treat Rev. 2010;36:206–215. doi: 10.1016/j.ctrv.2009.12.002. http://dx.doi.org/10.1016/j.ctrv.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Levy L, Suissa M, Chiche JF, Teman G, Martin B. BIRADS ultrasonography. Eur J Radiol. 2007;61:202–211. doi: 10.1016/j.ejrad.2006.08.035. http://dx.doi.org/10.1016/j.ejrad.2006.08.035. [DOI] [PubMed] [Google Scholar]
- 7.Costantini M, Belli P, Lombardi R, et al. Characterization of solid breast masses use of the sonographic breast imaging reporting and data system lexicon. J Ultrasound Med. 2006;25:649. doi: 10.7863/jum.2006.25.5.649. [DOI] [PubMed] [Google Scholar]
- 8.Bloom HJG, Richarson WW. Histologic grading and prognosis in breast cancer: A study of 1709 cases of which 359 have been followed for 15 years. Br J Cancer. 1957;11:353–377. doi: 10.1038/bjc.1957.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Viale G. The current state of breast cancer classification. Ann Oncol. 2012;23(Suppl 10):207–210. doi: 10.1093/annonc/mds326. [DOI] [PubMed] [Google Scholar]
- 10.Elsawaf Z, Sinn HS, Rom J, et al. Biological subtypes of triple negative breast cancer are associated with distinct morphological changes and clinical behavior. The Breast. 2013;22:986–992. doi: 10.1016/j.breast.2013.05.012. http://dx.doi.org/10.1016/j.breast.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 11.Rotstein AH, Neerhut PK. Ultrasound characteristics of histologically proven grade 3 invasive ductal breast carcinoma. Australas Radiol. 2005;49:476–479. doi: 10.1111/j.1440-1673.2005.01515.x. http://dx.doi.org/10.1111/j.1440-1673.2005.01515.x. [DOI] [PubMed] [Google Scholar]
- 12.Skaane P, Engedal K. Analysis of sonographic features in the differentiation of fibroadenoma and invasive ductal carcinoma. AJR Am J Roentgenol. 1998;170:109–114. doi: 10.2214/ajr.170.1.9423610. http://dx.doi.org/10.2214/ajr.170.1.9423610. [DOI] [PubMed] [Google Scholar]
- 13.Aho M, Irshad A, Ackerman SJ. Correlation of sonographic features of invasive ductal carcinoma with age, tumor grade, and hormone-receptor status. J Clin Ultrasound. 2013;41:10–17. doi: 10.1002/jcu.21990. http://dx.doi.org/10.1002/jcu.21990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weinstein SP, Conant EF, Mies C, et al. Posterior acoustic shadowing in benign breast lesions: sonographic-pathologic correlation. J Ultrasound Med. 2004;23:73–83. doi: 10.7863/jum.2004.23.1.73. [DOI] [PubMed] [Google Scholar]
- 15.Lamb PM, Perry NM, Vinnicombe SJ, et al. Correlation between ultrasound characteristics, mammographic findings and histological grade in patients with invasive ductal carcinoma of the breast. Clin Radiol. 2000;55:40–44. doi: 10.1053/crad.1999.0333. http://dx.doi.org/10.1053/crad.1999.0333. [DOI] [PubMed] [Google Scholar]
- 16.Shin HJ, Kim HH, Huh MO, et al. Correlation between mammographic and sonographic findings and prognostic factors in patients with node-negative invasive breast cancer. Br J Radiol. 2011;84:19–30. doi: 10.1259/bjr/92960562. http://dx.doi.org/10.1259/bjr/92960562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kojima Y, Tsunoda H. Mammography and ultra-sound features of triple negative breast cancer. Breast Cancer. 2011;18:146–151. doi: 10.1007/s12282-010-0223-8. http://dx.doi.org/10.1007/s12282-011-0261-x. [DOI] [PubMed] [Google Scholar]
- 18.Ko ES, Lee AH, Kim H, et al. Triple-negative breast cancer: correlation between imaging and pathological findings. Eur Radiol. 2010;20:1111–1117. doi: 10.1007/s00330-009-1656-3. http://dx.doi.org/10.1007/s00330-009-1656-3. [DOI] [PubMed] [Google Scholar]
- 19.Wang Y, Ikeda DM, Narasimhan B, et al. Estrogen receptor-negative invasive breast cancer: imaging features of tumors with and without human epidermal growth factor receptor type 2 overexpression. Radiology. 2008;246:367–375. doi: 10.1148/radiol.2462070169. http://dx.doi.org/10.1148/radiol.2462070169. [DOI] [PubMed] [Google Scholar]
- 20.Boisserie-Lacroix M, Mac Grogan G, Debled M, et al. Radiological features of triple negative breast cancers (about 73 cases) Diagn Interv Imaging. 2012;93:196–203. doi: 10.1016/j.diii.2012.01.006. http://dx.doi.org/10.1016/j.diii.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 21.El Saghir NS, Adebamowo CA, Anderson BO, et al. Breast cancer management in low resource countries (LRCs): consensus statement from the Breast Health Global Initiative. Breast. 2011;20(Suppl 2):S3–11. doi: 10.1016/j.breast.2011.02.006. http://dx.doi.org/10.1016/j.breast.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 22.Shyyan R, Masood S, Badwe RA, et al. Breast cancer in limited-resource countries: diagnosis and pathology. Breast J. 2006;12(Suppl 1):S27–37. doi: 10.1111/j.1075-122X.2006.00201.x. http://dx.doi.org/10.1111/j.1075-122X.2006.00201.x. [DOI] [PubMed] [Google Scholar]