Abstract
PURPOSE
We aimed to investigate the angular changes after Y-stenting of the basilar bifurcation aneurysms.
METHODS
A total of 19 patients (age range, 27–80 years; mean age, 52.5 years) underwent Y-stent coiling for basilar bifurcation aneurysm. Three vascular angles (α, β1, β2) were measured in the anteroposterior plane. β1 and β2 represented the angles between the basilar artery and the proximal P1 segments of the right and left posterior cerebral arteries, respectively. α represented the complementary angle between the β1 and β2 angles. Angles were measured before and after stent deployment. Diameters of the basilar artery and P2 segment of the posterior cerebral artery were measured at both sides. Correlation between vascular diameter and angular change of the basilar bifurcation was investigated.
RESULTS
Statistically significant α, β1, and β2 angle changes were found after stent deployment (P < 0.001). There was no statistically significant relationship between the diameter of the basilar artery and the α, β1, β2 angle changes (P > 0.05). There was no statistically significant relationship between the diameter of the posterior cerebral artery and the β angle change (P > 0.05). We found a statistically significant inverse correlation between pre-stent β angle and post-stent angle change (right side, P = 0.008; left side, P < 0.001).
CONCLUSION
Y-stenting narrows the effective neck and straightens the vascular bifurcation angle. Most of the angular remodeling occurs on the side that had a more acute angle before stent deployment.
The basilar artery (BA) bifurcation is the most common site for aneurysms arising from the posterior circulation (1). Hemodynamic stress at the basilar bifurcation causes elevated wall shear stress and predisposes aneurysm formation in the vessel (2, 3). The crossing Y-stenting technique has highly encouraging technical and clinical results in wide-neck basilar bifurcation aneurysms. Y-stent coiling narrows the effective neck and straightens the vascular bifurcation angle (angular remodeling). Straightening of the vascular bifurcation angle results in statistically significant migration of the flow impingement zone to the distal vessel as well as a narrowing of its width (4, 5). In this study, we have investigated the angular changes just after Y-stent coiling of basilar bifurcation aneurysms.
Methods
Patient population
Between May 2010 and April 2014, 19 patients (13 females and six males; age range, 27–80 years; mean age, 52.5 years) underwent Y-stent coiling to treat wide-neck basilar bifurcation aneurysm using intracranial nitinol self-expanding stent with the closed-cell design, Enterprise stent (Enterprise, Codman & Shurtleff; n=17) and LVIS Jr. stent (LVIS Jr, MicroVention; n=2). The institutional ethics committee approved this retrospective study. Written informed consent was obtained from all patients. Most of the aneurysms were un-ruptured, except for two. Patients presented with headache (n=14), recurrence of previously balloon-assisted aneurysm (n=1), and acute subarachnoid hemorrhage (n=2). In two patients the aneurysms were found incidentally. Patient demographics and aneurysm characteristics are listed in Table 1.
Table 1.
Demographic, clinical, and technical data for included patients
| Patient | Age (y)/sex | Aneurysm size (mm) | Dome-to-neck ratio | Ruptured | Stents used |
|---|---|---|---|---|---|
| 1 | 28/F | 5.3 | 1.2 | Yes | Enterprise |
| 2 | 51/F | 7.3 | 1.4 | Yes | Enterprise |
| 3 | 58/M | 14.8 | 1.2 | No | Enterprise |
| 4 | 58/M | 17.6 | 2.8 | No | Enterprise |
| 5 | 27/M | 7 | 1.1 | No | Enterprise |
| 6 | 63/F | 9.6 | 1 | No | Enterprise |
| 7 | 50/F | 12.6 | 1.6 | No | Enterprise |
| 8 | 49/F | 14.3 | 1.6 | No | Enterprise |
| 9 | 80/F | 12 | 1.2 | No | Enterprise |
| 10 | 38/F | 14 | 1.2 | No | Enterprise |
| 11 | 69/F | 15.1 | 1 | No | Enterprise |
| 12 | 57/M | 19.1 | 1.9 | No | Enterprise |
| 13 | 52/M | 18.2 | 1.4 | No | Enterprise |
| 14 | 55/F | 14.1 | 1.4 | No | Enterprise |
| 15 | 57/F | 9.7 | 1.4 | No | Enterprise |
| 16 | 48/F | 7.1 | 1 | No | Enterprise |
| 17 | 64/F | 6.6 | 1.3 | No | Enterprise |
| 18 | 54/M | 4.7 | 1 | No | LVIS Jr. |
| 19 | 59/F | 6.4 | 1 | No | LVIS Jr. |
F, female; M, male.
Y-stent coiling procedure
All patients, except for two ruptured patients, were premedicated with antiplatelet therapy consisting of 300 mg/day aspirin and 75 mg/day of clopidogrel or 10 mg/day prasugrel in case of clopidogrel resistance. In two ruptured patients, a loading dose of 300 mg clopidogrel was given through the nasogastric catheter just after the placement of stents. The clopidogrel response was investigated in all patients before the procedure using the rapid platelet function assay VerifyNow P2Y12 (VN-P2Y12, Accumetrics), and a ratio between 30% and 70% was found in all.
All interventions were performed under general anesthesia. A 6F long sheath was introduced into the V1 segment of the vertebral artery (VA). In some cases a 6F intracranial guiding catheter was inserted into the V2-V3 segment of the VA due to access tortuosity to provide backup support. After 3D rotational angiography with reconstruction images, the working projections were obtained, and the more challenging posterior cerebral artery (PCA) branch that has a more acute angle relative to the BA was selected to be catheterized first. A microcatheter (Prowler Select Plus, Cordis) with a 0.016-inch microguidewire (GT wire, Terumo) was used to catheterize the designated branch, under roadmapping guidance. Then, the first stent was deployed inside the first branch extending from P2 segment of the PCA to the BA. After deployment of the first stent, the same microcatheter with the same microguidewire was advanced into the other PCA through the interstices of the first stent. After stabilization of the microcatheter within the second branch, a second microcatheter (Headway 17, MicroVention/Terumo) with a 0.014-inch microguidewire (X-pedion, Covidien/EV3 Neurovascular) was inserted into the aneurysm sac. After catheterization of the aneurysm sac, the second stent was deployed with one half of the stent in the second branch and the other half within the lumen of the first stent. Thus, the second microcatheter was jailed between two proximal halves of the two stents. At this step, a flat panel detector CT (Vaso-CT) was performed for morphological assessment and visualizing adaptation of the stents to the wall. The second stent which passes through the interstices of the first stent always showed a tubular narrowing at the cross-point (Fig. 1). Then, the aneurysm sac was coiled with dense packing. For two patients, LVIS Jr. stent was used through the Headway 17 microcatheter. During the procedure and at least 12 hours after the procedure all patients received intravenous heparin with the goal of elevating the activated clotting time to two to three times the baseline value. Puncture site hemostasis was achieved by manual compression. Low-molecular-weight heparin was administered subcutaneously for three days, and the patients were discharged on life-long aspirin and clopidogrel or prasugrel for six months.
Figure 1.

Flat-detector CT image of the two crossing closed-cell stents deployed in a Y-configuration with an extensive tubular collapse of the second stent (arrow) due to the fixed cell of the first stent at the crossing point. Two proximal half of the stents were placed in a telescopic configuration. The microcatheter was jailed between the two proximal halves of the stents.
Main points
The basilar bifurcation is the most common site for aneurysms arising from the posterior circulation, and among the bifurcation aneurysms, basilar bifurcation aneurysms have a higher prevalence of rupture than internal carotid artery and middle cerebral artery bifurcation aneurysms.
The crossing Y-stenting technique has highly encouraging technical and clinical results in wide-neck basilar bifurcation aneurysms.
There is no statistically significant relationship between diameter of the basilary artery and α, β1, β2 angle changes after Y-stenting.
There is no statistically significant relationship between diameter of the posterior cerebral artery and β angle change on both sides after Y-stenting.
A smaller pre-stent β angle corresponds to a larger β angle change after stent deployment.
3D modeling and vascular angle measurement
All interventions were performed with biplane 2D digital subtraction angiography, 3D rotational angiography, and Vaso-CT guiding on the same system (Allura Xper FD20, Philips Healthcare). After 3D rotational angiography of the basilar bifurcation, the 3D volumetric datasets were automatically transferred to the workstation (XtraVision, Philips Healthcare) and analyzed. Three interventional neuroradiologists having at least six years of experience performed all measurements and the decisions were made on consensus. Pretreatment aneurysm size and neck size were measured. The volumetric dataset of each patient was visualized using multiplanar reconstruction on coronal plane, orienting to the basilar bifurcation. After deployment of the stents, thick-slice Vaso-CT images were used for the same purpose. The vascular angles (α, β1, and β2) were measured in the anteroposterior plane. β1 and β2 represented the angle between the BA and the proximal P1 segments of the right and left PCAs, respectively. α represented the complementary angle between the β1 and β2 angles. Angles were measured before and after the stent deployment (Figs. 2, 3). The same multiplanar reconstruction on coronal plane was used to measure the diameter of the BA at midsegment and the diameter of the P2 segments of the left and right PCAs. Probable relationships between the α, β1, and β2 angles and the diameter of the BA, left and right PCAs, and the side of the second stent were investigated.
Figure 2.
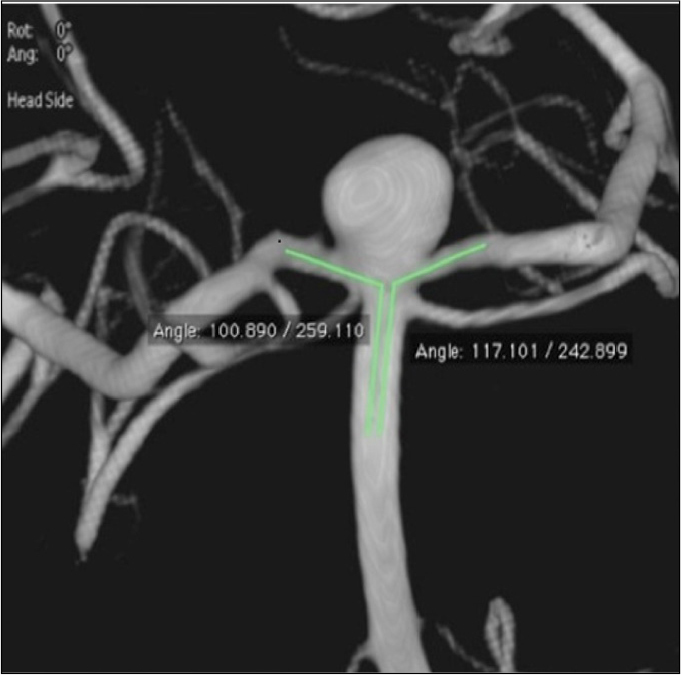
Volume rendering of three-dimensional volumetric dataset before stent deployment in a Y-configuration.
Figure 3.

Thick-slab flat-detector CT image after stent deployment in the same patient. The pretreatment angles β1 and β2 between the basilar artery and the right and left posterior cerebral artery increased immediately after the stent deployment.
Statistical analysis
Because of the relatively small sample size, we used nonparametric statistical tests with descriptive statistics (median, minimum, and maximum). Correlation analyses were performed between diameters of the BA and the right and left PCAs, and α, β1, and β2 angles and Spearman correlation coefficient was computed. Side of the second stent and α, β1, and β2 angle changes were compared using the Mann-Whitney U test. Wilcoxon signed ranks test was used for comparing pre-stent and post-stent angle values. Correlation between pre-stent β angle and post-stent angle change was performed with Spearman correlation coefficient. The intra-class correlation coefficient (ICC) was used to determine the agreement of measurements between the three neuroradiologists. All statistical analyses were performed using SPSS 15.0 for Windows (SPSS Inc.). Statistical significance was set at P < 0.05.
Results
An excellent agreement was established between the three neuroradiologists (averages measures ICC, 0.991). Aneurysm size ranged from 4.4 mm to 17.7 mm (mean± standard deviation [SD], 10.30±4.27 mm) and the neck ranged from 4.3 mm to 14.8 mm (mean±SD, 8.20±2.97 mm). Statistically significant α, β1, and β2 angle changes were found after stent deployment (P < 0.001). Descriptive statistics regarding α, β1, and β2 angle changes after the stent deployment are summarized in Table 2. There was no statistically significant relationship between the diameter of the BA and the α, β1, and β2 angle changes (P = 0.699, P = 0.604, and P = 0.856, respectively). There was no statistically significant relationship between the diameter of the right PCA and the β1 angle change and also between the diameter of the left PCA and the β2 angle change (P = 0.196 and P = 0.587, respectively). The second stent was located at the right side in six patients and at the left side in 13 patients. There was no statistically significant relationship between the side of the second stent and the α, β1, and β2 angle changes (Table 3). There was a significant difference between pre-stent and post-stent angle values (P < 0.001). We found a statistically significant reverse correlation between pre-stent β angle and post-stent β angle change (i.e., the smaller the pre-stent β angle, the bigger the β angle change after stent deployment; P = 0.008, r= −0.591 for β1 and P < 0.001, r= −0.733 for β2).
Table 2.
Measurements of the α, β1, and β2 angles before and after stent deployment (n=19)
| Angle | Radiologist | Pre-stent (°) Median (min, max) | Post-stent (°) Median (min, max) | Angle change (°) Median (min, max) |
|---|---|---|---|---|
| α | 1 | 177 (101, 263) | 122 (73, 212) | 41 (8, 122) |
| 2 | 177 (103, 259) | 120 (75, 201) | 48 (15, 132) | |
| 3 | 175 (101, 253) | 122 (74, 202) | 45 (14, 124) | |
| β1 | 1 | 89 (36, 119) | 117 (60, 137) | 27 (3, 74) |
| 2 | 86 (41, 117) | 119 (66, 133) | 28 (7, 74) | |
| 3 | 86 (42, 113) | 113 (67, 131) | 26 (5, 67) | |
| β2 | 1 | 103 (57, 158) | 121 (88, 160) | 13 (2, 67) |
| 2 | 100 (56, 154) | 124 (92, 158) | 18 (2, 72) | |
| 3 | 104 (51, 159) | 126 (91, 161) | 17 (2, 78) |
Table 3.
Relationship between the side of the second stent and the angle change
| α angle change | β1 angle change | β2 angle change | |
|---|---|---|---|
| P | P | P | |
| Radiologist 1 | 0.293 | 0.792 | 0.095 |
| Radiologist 2 | 0.312 | 0.759 | 0.065 |
| Radiologist 3 | 0.313 | 0.792 | 0.095 |
Second stent was located on the right side in six patients and on the left side in 13 patients.
Discussion
Our results show that Y-stenting of basilar bifurcation narrowed the vascular bifurcation angle. The diameter of the BA did not affect the α, β1, and β2 angle changes and similarly the diameter of PCA did not affect the β angle change. We also observed that most of the angular remodeling occurred on the side that had a smaller β angle before stent deployment.
Basilar bifurcation is the most common site for aneurysms arising from the posterior circulation. Among the bifurcation aneurysms, basilar bifurcation aneurysms have a higher prevalence of rupture than internal carotid artery and middle cerebral artery bifurcation aneurysms (1). The apex of arterial bifurcations is the site of maximal hemodynamic stress; the blood flow velocity is fastest in the middle of the vessel. This flow velocity impinges directly at the bifurcation apex. So, the arterial bifurcation apex faces highly variable regions of wall shear stress, characteristic of flow separation. It is believed that the elevated wall shear stress causes injury to the endothelial cells of the vessel wall and predisposes the vessel to aneurysm formation (2, 3).
The treatment of wide-neck basilar bifurcation aneurysms with Y-stenting technique has highly encouraging technical and clinical results. In the literature, three types of Y-stenting configuration have been described: kissing Y-stenting, in which the second stent is not advanced through the struts of the first stent, but rather proximal portions of the two stents are placed parallel in the main trunk; crossing Y-stenting, in which the second stent is advanced through the interstices of the first stent; and nonoverlapping Y-stenting, in which the first stent is placed from the main trunk to the left distal vessel and another stent is placed within the right distal vessel without overlapping the second stent (6–9). We have used the crossing Y-stenting technique in all patients, because it was observed to have the greatest reduction in velocity or wall shear stress (8). It was also shown that angular remodeling is more significant just after Y-stenting and during the first six months of follow-up. After that, a steady-state is seen because the potential energy of the stent is mostly released (10).
Y-stent coiling narrows the effective neck and straightens the vascular bifurcation angle (angular remodeling), which may effectively convert the morphology of a bifurcation aneurysm closer to that of a sidewall type. It preserves patency of the parent artery while serving as a buttress to prevent coil prolapse and allowing increased packing density (11). The degree of angular remodeling after Y-stenting seems to be different at various bifurcations. The greatest angular remodeling is seen at the anterior communicating artery, followed by the BA, the middle cerebral artery, and the internal carotid artery bifurcation (10). In our study, mean angle changes in α, β1, and β2 angles were determined as 47.3°, 27.9°, and 19.4°, respectively. We also noticed that more angular remodeling occurs on the side that had a more acute angle before stent deployment.
Straightening the vascular bifurcation angle results in statistically significant migration of the flow impingement zone to the distal vessel as well as narrowing its width which, in effect, fundamentally alters the underlying wall shear stress and decreases the pressure at the bifurcation (4, 5). Additionally, it is known that, the flow vortices at the arterial bifurcation tend to be larger if the combined size of the distal vessels is much larger than the parent artery or if the bifurcation angle is large (2). So, Y-stenting may also contribute to decrease the flow vortices at the arterial bifurcation by straightening the vascular bifurcation angle. Blood flow at high velocities causes static pressure to the apical point of the bifurcation. After Y-stenting, the bifurcation angle decreases; the incoming blood flow narrows its area of impingement on the apical point of the bifurcation, and the focus of increased pressure narrows at the bifurcation. In a study by Gao et al. (10), vessel diameter played a determinant role on the angular remodeling: smaller proximal vessel diameter was related with a bigger angular increase caused by Y-stenting, suggesting that a vessel with a bigger diameter has more resistance against the straightening force of the stent. On the other hand, there was no significant relationship between the distal diameter of the stented-vessel and angular remodeling. In contrast to the above study, we did not find any statistically significant relationship between the diameters of the BA and the right and left PCAs and α, β1, and β2 angle changes. Y-stenting may also promote progressive aneurysm occlusion compared with coiling alone by flow remodeling effect and enhancing endothelialization (12–14). Flow remodeling effect is achieved by narrowing of structures, which lowers the porosity of stents and redirects flow (8).
This study has a few limitations, such as its retrospective nature, the limited number of patients, and different angiographic and clinical follow-up period in each patient due to changing patient follow-up protocols with increased experience. Pre- and post-stent angle measurements could have been oriented to the skull of each patient for standardization. Finally, we had a patient population with a wide age range of 27 to 80 years; it is not clear how vessel elasticity and atherosclerosis might affect the angular remodeling in different age groups.
In conclusion, Y-stenting narrows the effective neck and straightens the vascular bifurcation angle. Most of the angular remodeling occurs on the side that had a more acute angle before stent deployment.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Van der Kolk NM, Algra A, Rinkel G. Risk of aneurysm rupture at intracranial arterial bifurcations. J Cerebrovasc Dis. 2010;74:29–35. doi: 10.1159/000313441. http://dx.doi.org/10.1159/000313441. [DOI] [PubMed] [Google Scholar]
- 2.Hademenos GJ, Massoud TF. Biophysical mechanisms of stroke. Stroke. 1997;28:2067–2077. doi: 10.1161/01.str.28.10.2067. http://dx.doi.org/10.1161/01.STR.28.10.2067. [DOI] [PubMed] [Google Scholar]
- 3.Takeuchi S, Karino T. Flow patterns and distributions of fluid velocity and wall shear stress in the human internal carotid and middle cerebral arteries. World Neurosurg. 2010;73:174–185. doi: 10.1016/j.surneu.2009.03.030. http://dx.doi.org/10.1016/j.surneu.2009.03.030. [DOI] [PubMed] [Google Scholar]
- 4.Gao B, Baharoglu MI, Malek AM. Angular remodeling in single stent-assisted coiling displaces and attenuates the flow impingement zone at the neck of intracranial bifurcation aneurysms. Neurosurgery. 2013;72:739–748. doi: 10.1227/NEU.0b013e318286fab3. http://dx.doi.org/10.1227/NEU.0b013e318286fab3. [DOI] [PubMed] [Google Scholar]
- 5.Meng H, Swartz DD, Wang Z, et al. A model system for mapping vascular responses to complex hemodynamics at arterial bifurcations in vivo. Neurosurgery. 2006;59:1094–1100. doi: 10.1227/01.NEU.0000245599.92322.53. http://dx.doi.org/10.1227/01.neu.0000245599.92322.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Henkes H, Kirsch M, Mariushi W, Miloslavski E, Brew S, Kühne D. Coil treatment of a fusiform upper basilar trunk aneurysm with a combination of “kissing” Neuroform stents, TriSpan-, 3D-and fibered coils, and permanent implantation of the microguidewires. Neuroradiology. 2004;46:464–468. doi: 10.1007/s00234-004-1192-4. http://dx.doi.org/10.1007/s00234-004-1192-4. [DOI] [PubMed] [Google Scholar]
- 7.Klisch J, Eger C, Sychra V, Strasilla C, Basche S, Weber J. Stent-assisted coil embolization of posterior circulation aneurysms using solitaire ab: preliminary experience. Neurosurgery. 2009;65:258–266. doi: 10.1227/01.NEU.0000348295.44970.C8. http://dx.doi.org/10.1227/01.NEU.0000348295.44970.C8. [DOI] [PubMed] [Google Scholar]
- 8.Kono K, Terada T. Hemodynamics of 8 different configurations of stenting for bifurcation aneurysms. AJNR Am J Neuroradiol. 2013;34:1980–1986. doi: 10.3174/ajnr.A3479. http://dx.doi.org/10.3174/ajnr.A3479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhao KJ, Yang PF, Huang QH, et al. Y-configuration stent placement (crossing and kissing) for endovascular treatment of wide-neck cerebral aneurysms located at 4 different bifurcation sites. AJNR Am J Neuroradiol. 2012;33:1310–1316. doi: 10.3174/ajnr.A2961. http://dx.doi.org/10.3174/ajnr.A2961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gao B, Baharoglu MI, Cohen AD, Malek AM. Stent-assisted coiling of intracranial bifurcation aneurysms leads to immediate and delayed intracranial vascular angle remodeling. AJNR Am J Neuroradiol. 2012;33:649–654. doi: 10.3174/ajnr.A2841. http://dx.doi.org/10.3174/ajnr.A2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bendok BR, Parkinson RJ, Hage ZA, Adel JG, Gounis MJ. The effect of vascular reconstruction device-assisted coiling on packing density, effective neck coverage, and angiographic outcome: an in vitro study. Neurosurgery. 2007;61:835–840. doi: 10.1227/01.NEU.0000298913.24625.26. http://dx.doi.org/10.1227/01.NEU.0000298913.24625.26. [DOI] [PubMed] [Google Scholar]
- 12.Fargen KM, Hoh BL, Welch BG, et al. Long-term results of enterprise stent-assisted coiling of cerebral aneurysms. Neurosurgery. 2012;71:239–244. doi: 10.1227/NEU.0b013e3182571953. http://dx.doi.org/10.1227/NEU.0b013e3182571953. [DOI] [PubMed] [Google Scholar]
- 13.Cekirge HS, Yavuz K, Geyik S, Saatci I. A novel “Y” stent flow diversion technique for the endovascular treatment of bifurcation aneurysms without endosaccular coiling. AJNR Am J Neuroradiol. 2011;32:1262–1268. doi: 10.3174/ajnr.A2475. http://dx.doi.org/10.3174/ajnr.A2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lawson MF, Newman WC, Chi YY, Mocco JD, Hoh BL. Stent-associated flow remodeling causes further occlusion of incompletely coiled aneurysms. Neurosurgery. 2011;69:598–603. doi: 10.1227/NEU.0b013e3182181c2b. http://dx.doi.org/10.1227/NEU.0b013e3182181c2b. [DOI] [PubMed] [Google Scholar]


