Abstract
AIM: To investigate coping mechanisms, constipation symptoms and anorectal physiology in 80 constipated subjects and 18 controls.
METHODS: Constipation was diagnosed by Rome II criteria. Coping ability and anxiety/depression were assessed by validated questionnaires. Transit time and balloon distension test were performed.
RESULTS: 34.5% patients were classified as slow transit type of constipation. The total colonic transit time (56 h vs 10 h, P < 0.0001) and rectal sensation including urge sensation (79 mL vs 63 mL, P = 0.019) and maximum tolerable volume (110 mL vs 95 mL, P = 0.03) differed in patients and controls. Constipated subjects had significantly higher anxiety and depression scores and lower SF-36 scores in all categories. They also demonstrated higher scores of ‘monitoring’ coping strategy (14 ± 6 vs 9 ± 3, P = 0.001), which correlated with the rectal distension sensation (P = 0.005), urge sensation (P=0.002), and maximum tolerable volume (P = 0.035). The less use of blunting strategy predicted slow transit constipation in both univariate (P = 0.01) and multivariate analysis (P = 0.03).
CONCLUSION: Defective or ineffective use of coping strategies may be an important etiology in functional constipation and subsequently reflected in abnormal anorectal physiology.
Keywords: Constipation, Anorectal physiology, Coping mechanism
INTRODUCTION
Functional constipation is a common problem in clinical practice. In the Western population, the prevalence was reported to be as high as 24% in elderly subjects and more commonly among women[1]. We observed a prevalence of 14% of constipation in Asian population[2].
There are growing interests in exploring the role of psychological factors on the pathogenesis of functional constipation. These patients report high levels of emotional distress[3-5]. Patients with functional constipation generally have a higher prevalence of anxiety, depression, and social dysfunction than do normal controls[6,7].
It has been reported that voluntary holding in healthy people can remarkably delay defecation and at the same time slow transit through the ascending colon and the recto-sigmoid tract[8]. This type of mechanism often produces constipation in children, which in some leads to constipation with megarectum-megacolon. This type of constipation can continue into adulthood as an acquired illness behavior[9]. In addition, a recent study[10] demonstrated that general psychosocial function, somatization, anxiety, depression, and feelings about the female role are impaired in women with constipation and are associated with altered rectal mucosal blood flow, which is an indirect measurement of the autonomic function. Furthermore, constipated subjects with slow bowel transit are associated with more psycho-social distress than those with normal bowel transit[11]. These findings suggest that behavior and psychological factors could lead to and be reflected by changes in anorectal physiology.
Drossman et al[12] have proposed that life factors will later influence psycho-social experiences, physiological functioning or susceptibility to developing a functional gastrointestinal disorder, including functional constipation. These psycho-social factors include coping ability and social support and play a role in modulating the effect of stress[13,14]. Coping ability plays an important role in amelioration of the stressful events and behaviors[14]. Penley et al[15] reported that coping ability was correlated with health outcomes.
Despite that psychological dysfunction in constipated patients is well reported, these patients have rarely been subjected to systematic psychiatric and anorectal physiology study. In addition, their general coping ability has not been investigated. We hypothesized that stresses if not coped will be “internalized” and may lead to symptom expression and different clinical outcomes, as mediated through central nervous system/enteric nervous system pathways. Hence, patients with functional constipation have different coping mechanisms and stress levels from normal subjects, which might contribute to the pathogenesis of functional constipation. We examined this hypothesis by testing the stress level, coping strategies used and anorectal physiology in both constipated patients and healthy subjects.
MATERIALS AND METHODS
The 80 patients in this study were a consecutive group, referred for assessment of constipation. All 80 subjects had been assessed by a gastroenterologist and had chronic constipation, defined by the Rome II criteria as follows: At least 12 wk, which need not be consecutive, in the preceding 12 mo of two or more of: less than three bowel movements per week, straining at stool more than 25% of the time, passage of lumpy or hard stools more than 25% of the time, sensation of incomplete evacuation for more than 25% of the time, sensation of anorectal obstruction/blockage for more than 25% of the time and manual maneuvers to facilitate more than 25% of the time of defecation. In addition, loose stools are not present, and there were insufficient criteria for the diagnosis of irritable bowel syndrome[16]. Patients with associated medical conditions that might result in constipation (i.e. secondary causes) were excluded. In addition, patients with associated psychological illness and/or being followed up by a psychiatrist were also excluded from the present study. Eighteen healthy volunteers were recruited as controls.
The volunteers were recruited through advertisement. They were interviewed by the research nurse about their health status. They did not have any past chronic medical disease including gastrointestinal diseases. They were currently asymptomatic, did not attend any medical practitioners, and had not taken any sick leave or medication over the past 2 mo.
Assessment of bowel transit time
Normal and slow transit constipation were confirmed by X-ray and colonic motility studies performed in all 80 patients, who had been shown to have long-standing severe constipation. Colonic transit time was assessed through the use of radiopaque markers. In brief, four sets of distinctive radiopaque markers of different shapes and size (circle on d 1, semi-cylinder on d 2, dot on d 3 and cylinder on d 4) were ingested by the volunteers on 4 consecutive d. X-ray of the abdomen was taken on d 5 and 7 to assess the mouth to anal transit and segmental colon transit. Transit in the right, left, and recto-sigmoid colon was calculated by adding all markers seen in these regions on d 5 and 7. Slow total colonic transit was defined as >67 h, the mean transit plus 2SD averaged from published studies[17,18].
Rectal sensation
Balloon distension is used to detect the threshold for three common sensations, the first detectable sensation, the sensation of urgency to defecate and the sensation of pain. A commercially available anorectal catheter was connected with a terminal polyethylene balloon (Zinetics: Anorectal Replacement Balloons, one size). The rectal sensation was evaluated by sequentially inflating the rectal balloon with a hand-held syringe using the following volumes: 10, 20, 30, 40, 50, 60, 80, 100, 150, and 200 mL of air. Each inflation was maintained for 1 min after deflation, a rest period of 2 min was allowed before re-inflating the balloon. During this test, the volumes of air inflated were recorded at the following sensations: the first sensation, urge to defecate and the maximum tolerable volume[19].
Questionnaire measures
Psychological well being was assessed by anxiety and depression. The anxiety and depression were assessed by the multiple affect adjective check list (MAACL)[20]. A combined score of anxiety and depression (the MAACL score) was generated by adding anxiety and depression scores.
Coping questionnaire: The coping questionnaires were based on the extended version of Miller Behavioral Style Scale[21,22]. The questionnaire examined the frequency of use of different coping strategies with different controllable (C) and uncontrollable (U) situations. The coping strategies included monitoring, blunting, problem solving, distancing, ventilation, wishful thinking and social support. The questionnaire has been validated and demonstrated previously to have good internal consistency[22]. It was delivered by one investigator [NYHW] to allow consistency.
Outcome measurement: The outcome measurement was measured in terms of the quality of life. The quality of life was assessed by the Short Form 36 (SF-36) health survey questionnaire. The SF-36 is a 36 question survey, which is well tested, valid, and reliable self-report tool developed for use in the Medical Outcomes Study[23,24]. The SF-36 is scored so that higher scores represent better functioning on both the two summary measures and on all eight subscales.
This study was approved by the Ethics Committee of the University of Hong Kong.
Statistical analysis
Comparison between groups was made by Mann-Whitney U tests for the demographic, colonic transit and the anal rectal pressures, anxiety and depression scores and the coping scores. Scoring of the SF-36 was performed following the scoring algorithms found in the SF-36 Health Survey Manual and Interpretation Guideline. The data from the SF-36 were expressed as mean ± SE of the means. Spearman’s rank correlation was used to assess for correlations between coping strategies, SF-36 and MAACL score. Regression analysis was performed for identifying independent predicting factors for anorectal physiology variables. A stepwise regression analysis was carried out. All statistical analysis was performed using SPSS software.
RESULTS
Demographic characteristics
There were 8 men and 72 women in the patient group and 8 men and 10 women in the control group. The mean patient age was 42 ± 16 years (range from 18 to 83 years) and that in the control group was 41 ± 11 years (range from 25 to 64 years) (P = 0.7).
The mean duration of constipation in the patients was 7.2 ± 8 years (range from 1 to 40 years). Sixty-five percent of the patients had straining for more than one quarter of the time, 57% had lumpy or hard stool, 82% had sensation of incomplete evacuation, 47% had anorectal blockade/ obstruction, 78% had fewer than three times of spontaneous opening per week, and 43% need digital evacuation. There were 34.5% patients classified as having slow colonic transit.
Anorectal physiology, anxiety, depression, coping strategies, and SF-36 scores in patients and controls
The readings of transit time and rectal sensation are sum-marized in Table 1. Transit time, including, left colon, sigmoid-rectal segment, and total colon, differed significantly in patients and controls (Table 1). Constipated patients also differed significantly from controls in the urge sensation and maximum tolerable volume in the assessment of rectal sensation (Table 2).
Table 1.
Transit time and anorectal physiological assessment in patients and controls (mean±SD)
| Control (n = 17) | Patient (n = 80) | P | |||
| Transit time | |||||
| Right segment | 7.3 | 6.4 | 12.7 | 11.5 | 0.08 |
| Left segment | 5.8 | 6.3 | 17.8 | 6.8 | < 0.0001 |
| Sigmoid-rectal segment | 6.1 | 6.2 | 23.9 | 19.1 | < 0.0001 |
| Total colon | 10.4 | 7.6 | 56.2 | 29.1 | < 0.0001 |
| Balloon measurements (mL) | |||||
| First sensation | 33 | 9 | 39 | 17 | 0.2 |
| Constant sensation/urge | 63 | 20 | 79 | 30 | 0.019 |
| Maximum tolerable volume | 95 | 16 | 110 | 38 | 0.03 |
Table 2.
Correlation between anxiety/depression (the MAACL score) and the scores of various coping strategies
| Coping strategies | Correlation coefficient | P |
| Monitoring | 0.2 | 0.9 |
| Blunting | -0.05 | 0.6 |
| Social support | -0.4 | 0.003 |
| Controllable problem solving | -0.4 | < 0.0001 |
| Uncontrollable problem solving | -0.3 | 0.03 |
| Controllable catharsis | -0.3 | 0.009 |
| Uncontrollable catharsis | -0.2 | 0.1 |
| Controllable wishful thinking | -0.2 | 0.1 |
| Uncontrollable wishful thinking | -0.2 | 0.3 |
| Controllable distancing | 0.1 | 0.7 |
| Uncontrollable distancing | 0.002 | 0.9 |
Anxiety and depression scores, and hence the MAACL score, differed significantly in patients and controls (34 ± 8 vs 26 ± 7 for anxiety score, P = 0.009; 32 ± 7 vs 26 ± 7 for depression score, P < 0.0001; 66 ± 14 vs 52 ± 14 for MAACL score, P = 0.001). Constipated patients also differed significantly from the normal subjects in all eight categories of the SF-36 scores (Figure 1).
Figure 1.
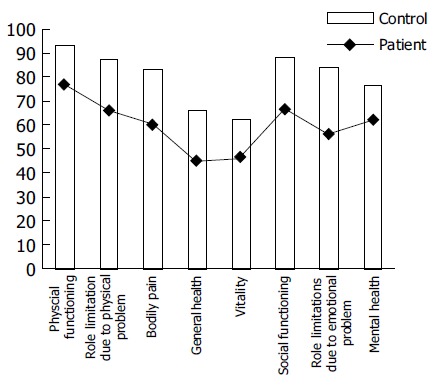
Self assessment of physical and mental health (SF-36) in patients and controls. Mean values of SF-36 scores for patients with constipation (line) compared with normal subjects (bar). Constipated patients differed from the normal subjects in all eight categories. They had decreased physical functioning scores (77 vs 93, P < 0.0001), role-physical scores (66 vs 87, P = 0.009), bodily pain scores (60 vs 83, P = 0.001), general health scores (45 vs 68, P < 0.0001), vitality scores (46 vs 62, P = 0.002), social functioning scores (67 vs 88, P < 0.0001), role emotional scores (56 vs 84, P = 0.001), and mental health scores (61 vs 76, P = 0.003).
The correlation between the MAACL score and the scores of coping strategies are summarized in Table 2. Significant correlation was observed between the MAACL score and social support (P = 0.003), controllable problem solving (P < 0.0001), uncontrollable problem solving (P = 0.03), and controllable catharsis (P = 0.009). The scores of coping strategies are summarized in Table 3. Patients with constipation had more frequent use (higher scores) of the ‘monitoring’ coping strategy than the controls, but no difference in the other coping strategies (14 ± 6 vs 9 ± 3, P = 0.001). When patients were stratified according to transit time, those with slow transit type of constipation had less frequent use (lower scores) of the ‘blunting’ coping strategy than other patients (7 ± 3 vs 10 ± 3, P = 0.01). When stratified according to rectal sensation, it was found that the use of the ‘monitoring’ coping strategy in constipated subjects correlated positively with the balloon volume at the first sensation (P = 0.005), the urge sensation (P =0.002), and the maximum tolerable volume (P = 0.035).
Table 3.
Coping scores in patients and controls
| Coping strategies |
Patient (n = 80) |
Control (n = 18) |
P | ||
| Median scores | Range | Median scores | Range | ||
| Monitoring | 14 | 3-27 | 9 | 2-15 | 0.001 |
| Blunting | 8 | 1-16 | 9 | 5-16 | 0.9 |
| Social support | 43 | 33-56 | 41 | 34-51 | 0.3 |
| Controllable problem solving | 6 | 1-11 | 6 | 1-12 | 0.3 |
| Uncontrollable problem solving | 5 | 1-11 | 5 | 1-9 | 0.8 |
| Controllable catharsis | 6 | 1-12 | 6 | 2-10 | 0.7 |
| Uncontrollable catharsis | 5 | 1-11 | 5 | 1-10 | 0.9 |
| Controllable wishful thinking | 5 | 1-12 | 5 | 1-12 | 0.6 |
| Uncontrollable wishful thinking | 4 | 1-12 | 5 | 1-12 | 0.3 |
| Controllable distancing | 4 | 1-10 | 3 | 1-7 | 0.4 |
| Uncontrollable distancing | 5 | 1-12 | 5 | 1-12 | 0.9 |
Multivariate analysis for predicting duration of constipation and anorectal physiology
Variables including sex, age, various coping strategies and MAACL score were entered for the regression analysis for the prediction of symptoms of constipation. It was observed that female sex (P = 0.01) and age (P = 0.002) were the independent predictive variables for symptom of duration of constipation, despite that there were not enough men to comment on the predictive value of gender.
Variables including sex, age, various coping strategies and MAACL score were entered for the regression analysis for the prediction of anorectal physiology. We observed that the more often use of coping strategies of blunting (P = 0.03) predicted slow transit type of constipation. On the other hand, there was no significant independent predictive factor for rectal sensation.
DISCUSSION
High prevalence of emotional distress including anxiety, depression, and social dysfunction in patients with functional constipation has been well reported[6,7]. Our study further supported this observation and the observation was corroborated by objective evidence from anorectal physiology study. Emotional distress can cause physical problems but the reverse is also true: having a physical problem may cause distress. We examined the former link and at a higher level: by hypothesizing that defective coping mechanisms existed in patients with functional constipation and that defective coping mechanism subsequently led to internalization of stress and hence reflected as psycho-somatic disease such as functional constipation. Our study confirmed this hypothesis, showing that defective coping mechanisms existed in these patients and were independent factors for predicting abnormal anorectal physiology.
The present study demonstrated that coping strategies of monitoring and blunting were associated with anorectal physiology. Blunting (information avoiding coping style) has been shown to directly associate with the reporting of symptoms associated with infections like common colds and flu-like symptoms[25]. Similar finding was observed in the current study that blunting was directly associated with the slow transit type of constipation. “Monitoring” or information-gathering coping style was associated with more anticipatory anxiety[26]. Similar finding was observed in our present study that frequent use of monitoring coping strategy was found in constipation patients and associated with larger balloon volume at first sensation, urge sensation and maximum tolerable volume. These ineffective or less use of coping strategies are in accordance with the recent finding that constipated subjects have more social dysfunction and less satisfaction in their sexual life[6]. Testing for both controllable and uncontrollable situations, which were employed in the present study allowed for better assessment of the coping response because uncontrollable life events are better predictive of psychological distress over time[27]. Problem solving and catharsis are strategies that have been used to deal with a variety of stressful situations with different characteristics[15,28] and correlate with health outcomes[15]. Patients with functional dyspepsia have also been reported to have a non-discriminative, action-oriented coping style[29]. Hence we postulated that defective coping mechanism also exists and is an important etiology factor in patients with functional constipation. In addition, the defective coping strategy in the constipated subjects could not be explained by the associated anxiety and depression as there was no correlation observed in the current study between the MAACL score and the coping strategies of monitoring and blunting.
The current study again demonstrated significant anxiety and depression level in constipated patients, which has already been reported previously[2,4-7]. However, it is worth noting that the patients’ anxiety and depression scores were relatively higher than individuals in the control group, rather than having absolute high levels in anxiety and depression. SF-36 scale, as a measurement of quality of life, has been demonstrated to be low in patients with functional constipation. This is again further confirmed in our study.
The limitation of our study was that the constipated patients were recruited in the hospital in the present study. Caution should be taken when attempting to generalize the present results to non-consulters. Another limitation was the small sample size of the normal controls. Taking into account the high prevalence of emotional and behavioral abnormalities in general population, a small control group could underestimate the real prevalence of psychological disorders in “healthy” volunteers. Nonetheless, our results suggested the role of defective coping mechanisms as another psychological factor in the pathogenesis of functional constipation. It is possible that failure to cope with stressful situation results in stress internalization and in turn leads to anxiety and other psychological distress. These are in accordance with the findings in this study that coping was associated with both physical and mental well being (SF-36) as well as anxiety and depression. These distresses may act via the enteric nervous system to inhibit colonic motility and thus prolonged colonic transit, as demonstrated in the present study. This was supported by a recent study[10] demonstrating constipated subjects with psychological abnormality was associated with altered extrinsic gut innervation. Furthermore in cats, it has been demonstrated that stimulation of the pelvic nerves affects colonic contractions[30]. These findings suggest a link between central brain activity, enteric nervous system and gut dysfunction. The current study broadens our knowledge on the pathogenetic mechanisms of constipation and might provide clue to treatment, such as psychotherapy directing at the defective coping mechanisms.
Footnotes
Science Editor Guo SY Language Editor Elsevier HK
References
- 1.Talley NJ, O'Keefe EA, Zinsmeister AR, Melton LJ. Prevalence of gastrointestinal symptoms in the elderly: a population-based study. Gastroenterology. 1992;102:895–901. doi: 10.1016/0016-5085(92)90175-x. [DOI] [PubMed] [Google Scholar]
- 2.Cheng C, Chan AO, Hui WM, Lam SK. Coping strategies, illness perception, anxiety and depression of patients with idiopathic constipation: a population-based study. Aliment Pharmacol Ther. 2003;18:319–326. doi: 10.1046/j.1365-2036.2003.01663.x. [DOI] [PubMed] [Google Scholar]
- 3.Fisher SE, Keighley MRB, Brecon K, Smart V, Andrews H. Do patients with disordered defecation have a primary per-sonality disorder? Gut. 1987;28:A1373. [Google Scholar]
- 4.Devroede G, Girard G, Bouchoucha M, Roy T, Black R, Camerlain M, Pinard G, Schang JC, Arhan P. Idiopathic constipation by colonic dysfunction. Relationship with personality and anxiety. Dig Dis Sci. 1989;34:1428–1433. doi: 10.1007/BF01538081. [DOI] [PubMed] [Google Scholar]
- 5.Wald A, Hinds JP, Caruana BJ. Psychological and physiological characteristics of patients with severe idiopathic constipation. Gastroenterology. 1989;97:932–937. doi: 10.1016/0016-5085(89)91500-x. [DOI] [PubMed] [Google Scholar]
- 6.Mason HJ, Serrano-Ikkos E, Kamm MA. Psychological morbidity in women with idiopathic constipation. Am J Gastroenterol. 2000;95:2852–2857. doi: 10.1111/j.1572-0241.2000.02313.x. [DOI] [PubMed] [Google Scholar]
- 7.Nehra V, Bruce BK, Rath-Harvey DM, Pemberton JH, Camilleri M. Psychological disorders in patients with evacuation disorders and constipation in a tertiary practice. Am J Gastroenterol. 2000;95:1755–1758. doi: 10.1111/j.1572-0241.2000.02184.x. [DOI] [PubMed] [Google Scholar]
- 8.Klauser AG, Voderholzer WA, Heinrich CA, Schindlbeck NE, Müller-Lissner SA. Behavioral modification of colonic function. Can constipation be learned? Dig Dis Sci. 1990;35:1271–1275. doi: 10.1007/BF01536418. [DOI] [PubMed] [Google Scholar]
- 9.Whitehead WE. Illness behaviour. in Constipation, ed. M Kamm & JE Lennard-Jones; Wrightson Biomedical Publishing LTD Petersfield UK; 1994. pp. 95–100. [Google Scholar]
- 10.Emmanuel AV, Mason HJ, Kamm MA. Relationship between psychological state and level of activity of extrinsic gut innervation in patients with a functional gut disorder. Gut. 2001;49:209–213. doi: 10.1136/gut.49.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dykes S, Smilgin-Humphreys S, Bass C. Chronic idiopathic constipation: a psychological enquiry. Eur J Gastroenterol Hepatol. 2001;13:39–44. doi: 10.1097/00042737-200101000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Drossman DA, Creed FH, Olden KW, Svedlund J, Toner BB, Witehead WE. Psychosocial aspects of the functional gas-trointestinal disorders. In: The functional gastrointestinal disorders., editor. Ed. Drossman DA, Corazziari E, Talley N, Thompson WG, Whitehead WE; 2000. pp. 165–166. [Google Scholar]
- 13.Cobb S. Presidential Address-1976. Social support as a moderator of life stress. Psychosom Med. 1976;38:300–314. doi: 10.1097/00006842-197609000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Springer; 1984. [Google Scholar]
- 15.Penley JA, Tomaka J, Wiebe JS. The association of coping to physical and psychological health outcomes: a meta-analytic review. J Behav Med. 2002;25:551–603. doi: 10.1023/a:1020641400589. [DOI] [PubMed] [Google Scholar]
- 16.Drossman DA. The functional gastrointestinal disorders and the Rome II process. Gut. 1999;45 Suppl 2:II1–II5. doi: 10.1136/gut.45.2008.ii1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chaussade S, Khyari A, Roche H, Garret M, Gaudric M, Couturier D, Guerre J. Determination of total and segmental colonic transit time in constipated patients. Results in 91 patients with a new simplified method. Dig Dis Sci. 1989;34:1168–1172. doi: 10.1007/BF01537263. [DOI] [PubMed] [Google Scholar]
- 18.Metcalf AM, Phillips SF, Zinsmeister AR, MacCarty RL, Beart RW, Wolff BG. Simplified assessment of segmental colonic transit. Gastroenterology. 1987;92:40–47. doi: 10.1016/0016-5085(87)90837-7. [DOI] [PubMed] [Google Scholar]
- 19.Whitehead WE, Schuster MM. Anorectal physiology and pathophysiology. Am J Gastroenterol. 1987;82:487–497. [PubMed] [Google Scholar]
- 20.Bloom PM, Brady JP. An ipsative validation of the multiple affect adjective check list. J Clin Psychol. 1968;24:45–46. doi: 10.1002/1097-4679(196801)24:1<45::aid-jclp2270240112>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 21.Miller SM, Mangan CE. Interacting effects of information and coping style in adapting to gynecologic stress: should the doctor tell all? J Pers Soc Psychol. 1983;45:223–236. doi: 10.1037//0022-3514.45.1.223. [DOI] [PubMed] [Google Scholar]
- 22.Cheng C, Hui W, Lam S. Perceptual style and behavioral pattern of individuals with functional gastrointestinal disorders. Health Psychol. 2000;19:146–154. doi: 10.1037//0278-6133.19.2.146. [DOI] [PubMed] [Google Scholar]
- 23.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 24.Ware E SF-36 Health Survey Manual and interpretation guide, The Medical Outcomes Trust, Boston, 1993 [Google Scholar]
- 25.Davey GC, Tallis F, Hodgson S. The relationship between information-seeking and information-avoiding coping styles and the reporting of psychological and physical symptoms. J Psychosom Res. 1993;37:333–344. doi: 10.1016/0022-3999(93)90135-3. [DOI] [PubMed] [Google Scholar]
- 26.Lerman C, Rimer B, Blumberg B, Cristinzio S, Engstrom PF, MacElwee N, O'Connor K, Seay J. Effects of coping style and relaxation on cancer chemotherapy side effects and emotional responses. Cancer Nurs. 1990;13:308–315. [PubMed] [Google Scholar]
- 27.McFarlane AH, Norman GR, Streiner DL, Roy R, Scott DJ. A longitudinal study of the influence of the psychosocial environment on health status: a preliminary report. J Health Soc Behav. 1980;21:124–133. [PubMed] [Google Scholar]
- 28.Gellis ZD. Coping with occupational stress in healthcare: A comparison of social workers and nurses. Administration Social Work. 2002;26:37–52. [Google Scholar]
- 29.Cheng C, Hui WM, Lam SK. Coping style of individuals with functional dyspepsia. Psychosom Med. 1999;61:789–795. doi: 10.1097/00006842-199911000-00011. [DOI] [PubMed] [Google Scholar]
- 30.Andersson PO, Bloom SR, Järhult J. Colonic motor and vascular responses to pelvic nerve stimulation and their relation to local peptide release in the cat. J Physiol. 1983;334:293–307. doi: 10.1113/jphysiol.1983.sp014495. [DOI] [PMC free article] [PubMed] [Google Scholar]


