Abstract
We report a case of hepatocellular carcinoma (HCC) treated successfully by transarterial chemoembolization (TACE) followed by combination therapy of 5-fluorouracil (5-FU) and pegylated interferon-α (PEG-IFN-α). In the present case, the patient had massive and advanced HCC with a diameter of over 8 cm located in segment 7 (S7) of the liver. Furthermore, the tumor invaded into the major branch of the portal vein (Vp3). After TACE, combined administration of 5-FU and PEG-IFN-α was performed for 5 mo. HCC was totally eradicated and the serum levels of tumor markers were markedly decreased by the treatment. Although it has been reported that the combined use of conventional IFN-α and 5-FU showed striking effects on HCC in some cases, this case may suggest the more promising effect of PEG-IFN-α with a long-lasting effect, in the combined use with 5-FU for the treatment of massive advanced HCC.
Keywords: Hepatocellular carcinoma, 5-Fluorouracil, Pegylated interferon-α, Combination therapy
INTRODUCTION
Despite the recently innovated treatment modalities including radiofrequency ablation (RFA), hepatocellular carcinoma (HCC) is still one of the most progressive malignancies resistant to the local treatment or chemotherapy. Repeated recurrences often occur due to the multicentric carcinogenesis and intrahepatic metastasis. For the treatment of advanced HCC invading into the major branches of the portal tract, the effectiveness of the combination therapy of 5-fluorouracil (5-FU) and interferon-α (IFN-α) has been reported[1-4]. In the reports, conventional IFN-α has been used as a component of the combination therapy. In the present study, instead of conventional IFN-α, pegylated (PEG) IFN-α was used once a week with continuous infusion of 5-FU for the treatment of advanced HCC and its effectiveness was evaluated.
CASE REPORT
A 74-year-old female had been followed as a diabetes mellitus and chronic hepatitis (non-B and non-C) at Kagawa University Hospital since 1988. The first HCC emerged in S4, S5 and S6 of the liver in 1995. As her hepatic reserve was enough for surgical operation, partial hepatectomy was performed for the multiple HCC. Recurrence of HCC occurred in the middle of 2001, 6 years after the operation. The solitary tumor was detected in S7 of the liver. As it was a relatively small-sized tumor with a diameter of 1 cm, regional treatment by the combination of percutaneous ethanol injection and radiofrequency ablation (PEI-RFA), innovated at our department[5], was performed. The tumorous lesion was totally destroyed by PEI-RFA. Since then she was followed for her liver function and periodically checked for detection of new HCC by blood examination and computed tomography (CT). In January 2002, serum levels of AFP and AFP-L3, tumor markers for HCC, was 13 ng/mL and 4.1%, respectively. Both levels were kept within normal ranges until the end of 2003 and newly developed HCC was not detected by CT or ultrasonography during the period. Both tumor markers suddenly jumped up in March 2004. The levels of AFP reached 555 ng/mL in March and 2 888 ng/mL in June, and AFP-L3 reached 81.7% in April 2004. CT taken in March 2004 showed the development of massive HCC located in S6 and S7 of the liver, with the maximum diameter of over 8 cm. Moreover, HCC invaded into the main branch of the portal vein. The patient was admitted to Kagawa Prefectural Central Hospital for the treatment of HCC. The patient immediately underwent angiography. The angiography clearly showed the massive hypervascular tumor occupying the wide area of the right hepatic artery (Figure 1A). Furthermore, tumor thrombus was present in the portal tract (Figure 1B). Therefore, in addition to transarterial chemoembolization (TACE) using Farmorubicin (Kyowa Hakko Co., Tokyo, Japan) and gelfoam (Figure 1C), a reservoir for intra-arterial infusion was inserted into the proper hepatic artery (Figure 1D) and the injection port was subcutaneously implanted. From early May 2004, combination therapy of IFN-α and 5-FU was initiated. The patient was treated with subcutaneous administration of PEG-IFN-α-2a (Pegasys, Chugai Pharmaceutical Co., Ltd, Tokyo) and continuous intra-arterial infusion of 5-FU (Kyowa Hakko Co., Tokyo, Japan). Continuous infusion of 5-FU (250 mg/d) was performed for 2 wk with an interval of 2 wk via the implanted reservoir port according to the regimen previously published[2]. PEG-IFN-α-2a (90 μg) was administrated on d 1 of every week. Between May and November, 6 repeated cycles of administration of continuous 5-FU and PEG-IFN-α were performed. No significant side effects were observed. A series of CT examination revealed the marked anti-tumor effect of the combination therapy. Massive HCC in the right hepatic lobe was gradually reduced and the portal tumor thrombus finally disappeared in October 2004, 5 mo after the initiation of the combination therapy. The level of AFP was also decreased to 38 ng/mL in October 2004. No recurrence of HCC has not been detected on enhanced dynamic CT and no elevation of the tumor markers has not been observed so far (Figures 2A-D).
Figure 1.
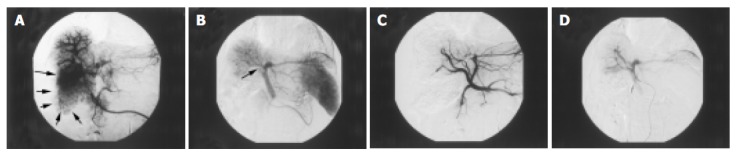
Angiography of the celiac artery before and after TACE was taken on April 15, 2004. Massive tumor stain (small arrow) was exhibited by the celiac arteriography (A). Large arterioportal shunt (big arrow) was exhibited above the massive tumor stain. The right branch of the portal vein was not exhibited by the portography (arrow) (B). The tumor stain disappeared after the TACE (C). The reservoir for intra-arterial infusion was inserted into the proper hepatic artery (D).
Figure 2.
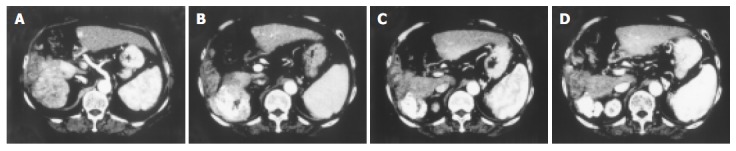
Photographs of enhanced dynamic CT in the time course of the combination therapy of PEG-IFN-α and 5-FU on March 29, 2004 (A), June 21, 2004 (B), August 27, 2004 (C) and October 8, 2004 (D). Massive tumor was rapidly reduced during the combination therapy. Only the accumulation of lipiodol remained in the final CT taken on October 8, 2004.
DISCUSSION
HCC is one of the world’s most common malignancies, especially in Asia. Despite the advances in diagnostic and therapeutic techniques, HCC often progress to an advance stage regardless of several treatment modalities. RFA technique is one of the promising treatment modalities recently innovated for the treatment of HCC and is used worldwide at present. This newly developed technique appears very effective to induce wider coagulated necrosis rather than percutaneous ethanol injection therapy without major complications, but the efficacy of RFA is limited to relatively small-sized HCC with the maximum diameter of 3 cm or less. Thus, we have developed the combination therapy of PEI-RFA for inducing wider coagulated necrosis[5,6] and for achieving safer treatment of HCC[7]. Nevertheless, recurrences of the tumor after the local treatment often occurs and some of the tumor progress to an advanced stage. For these advanced HCC, chemotherapy alone is not necessarily effective. Recently, combination therapy of some chemical reagents, such as 5-FU and cisplatin, and systemic administration of IFN-α was shown to be effective for the treatment of HCC[1-4]. Indeed, this newly developed therapy could increase the therapeutic effect on HCC that could not be treated by any other therapeutic modalities. However, according to the reports cited above, the response rate including the complete response (CR) and partial response are not necessarily high. Especially, the number of CR cases was extremely small. In the present case, not only the massive tumor but also the tumor thrombus in the major branch of the portal vein was eradicated completely by the combination therapy of 5-FU and PEG-IFN-α. The response to the combination therapy in this case is considered to be CR. Disappearance of massive large-sized HCC of more than 8 cm in diameter as shown in the present case has never been reported. To our knowledge, this case is the first descriptive report of the case with massive HCC successfully treated with the new combination therapy of systemic administration of PEG-IFN-α and intra-arterial administration of 5-FU. The major difference between the PEG-IFN-α and conventional IFN-α is the retention time of the effect. High concentration of IFN-α in the blood is retained for a week by administration of PEG-IFN-α, whereas high and low concentrations of IFN-α are repeated by turns in the conventional IFN-α treatment. Thus, the present case showing CR to the combination therapy may give us an insight into the promising anti-tumor effects of the combined use of PEG-IFN-α and chemical agents such as 5-FU and cisplatin. Although the study including a large number of patients with advanced HCC is necessary, the combination therapy of PEG-IFN-α and chemical agents may open up a new avenue for the treatment of advanced HCC.
Footnotes
Science Editor Guo SY Language Editor Elsevier HK
Co-correspondents: Kazutaka Kurokohchi
References
- 1.Chung YH, Song IH, Song BC, Lee GC, Koh MS, Yoon HK, Lee YS, Sung KB, Suh DJ. Combined therapy consisting of intraarterial cisplatin infusion and systemic interferon-alpha for hepatocellular carcinoma patients with major portal vein thrombosis or distant metastasis. Cancer. 2000;88:1986–1991. [PubMed] [Google Scholar]
- 2.Kaneko S, Urabe T, Kobayashi K. Combination chemotherapy for advanced hepatocellular carcinoma complicated by major portal vein thrombosis. Oncology. 2002;62 Suppl 1:69–73. doi: 10.1159/000048279. [DOI] [PubMed] [Google Scholar]
- 3.Sakon M, Nagano H, Dono K, Nakamori S, Umeshita K, Yamada A, Kawata S, Imai Y, Iijima S, Monden M. Combined intraarterial 5-fluorouracil and subcutaneous interferon-alpha therapy for advanced hepatocellular carcinoma with tumor thrombi in the major portal branches. Cancer. 2002;94:435–442. doi: 10.1002/cncr.10246. [DOI] [PubMed] [Google Scholar]
- 4.Patt YZ, Hassan MM, Lozano RD, Brown TD, Vauthey JN, Curley SA, Ellis LM. Phase II trial of systemic continuous fluorouracil and subcutaneous recombinant interferon Alfa-2b for treatment of hepatocellular carcinoma. J Clin Oncol. 2003;21:421–427. doi: 10.1200/JCO.2003.10.103. [DOI] [PubMed] [Google Scholar]
- 5.Kurokohchi K, Watanabe S, Masaki T, Hosomi N, Funaki T, Arima K, Yoshida S, Miyauchi Y, Kuriyama S. Combined use of percutaneous ethanol injection and radiofrequency ablation for the effective treatment of hepatocelluar carcinoma. Int J Oncol. 2002;21:841–846. doi: 10.3892/ijo.21.4.841. [DOI] [PubMed] [Google Scholar]
- 6.Kurokohchi K, Watanabe S, Masaki T, Hosomi N, Funaki T, Arima K, Yoshida S, Nakai S, Murota M, Miyauchi Y, et al. Combination therapy of percutaneous ethanol injection and radiofrequency ablation against hepatocellular carcinomas difficult to treat. Int J Oncol. 2002;21:611–615. [PubMed] [Google Scholar]
- 7.Kurokohchi K, Watanabe S, Masaki T, Hosomi N, Miyauchi Y, Himoto T, Kimura Y, Nakai S, Deguchi A, Yoneyama H, et al. Comparison between combination therapy of percutaneous ethanol injection and radiofrequency ablation and radiofrequency ablation alone for patients with hepatocellular carcinoma. World J Gastroenterol. 2005;11:1426–1432. doi: 10.3748/wjg.v11.i10.1426. [DOI] [PMC free article] [PubMed] [Google Scholar]


