Abstract
Study Objectives:
To compare the use of sleep diagnostic tests, the risks, and cofactors, and outcomes of the care of Indigenous and non-indigenous Australian adults in regional and remote Australia in whom sleep related breathing disorders have been diagnosed.
Methods:
A retrospective cohort study of 200 adults; 100 Aboriginal and Torres Strait Islander and 100 non-indigenous adults with a confirmed sleep related breathing disorder diagnosed prior to September 2011 at Alice Springs Hospital and Cairns Hospital, Australia.
Results:
Results showed overall Indigenous Australians were 1.8 times more likely to have a positive diagnostic sleep study performed compared with non-indigenous patients, 1.6 times less likely in central Australia and 3.4 times more likely in far north Queensland. All regional and remote residents accessed diagnostic sleep studies at a rate less than Australia overall (31/100,000/y (95% confidence interval, 21–44) compared with 575/100,000/y).
Conclusion:
The barriers to diagnosis and ongoing care are likely to relate to remote residence, lower health self-efficacy, the complex nature of the treatment tool, and environmental factors such as electricity and sleeping area. Indigeneity, remote residence, environmental factors, and low awareness of sleep health are likely to affect service accessibility and rate of use and capacity to enhance patient and family education and support following a diagnosis. A greater understanding of enablers and barriers to care and evaluation of interventions to address these are required.
Commentary:
A commentary on this article appears in this issue on page 1255.
Citation:
Woods CE, McPherson K, Tikoft E, Usher K, Hosseini F, Ferns J, Jersmann H, Antic R, Maguire GP. Sleep disorders in Aboriginal and Torres Strait Islander people and residents of regional and remote Australia. J Clin Sleep Med 2015;11(11):1263–1271.
Keywords: Australia, indigenous population, obstructive sleep apnoea, polysomnography, sleep
Sleep related breathing disorders are a common and under-diagnosed problem in Australia.1 Obstructive sleep apnoea (OSA) is one of the most common, and is associated with intermittent upper airway obstruction.2 Symptoms include snoring, witnessed apnoeas (breathing cessation), disrupted sleep (arousals), and excessive daytime sleepiness.2 Polysomnography (PSG) is the ‘gold standard’ method of OSA diagnosis.3 Management may include lifestyle modification (weight loss, and alcohol and smoking cessation), continuous positive airway pressure (CPAP), surgery or the use of oral devices that hold the lower jaw forward.4 OSA has an effect on health and well-being and 5.3% of the risk of stroke, 1.1% of heart failure, 3.6% of coronary heart disease, and 6.2% of depression can be attributed to OSA.1
BRIEF SUMMARY
Current Knowledge/Study Rationale: There are currently no published data relating to the nature of sleep related breathing disorders affecting Aboriginal and Torres Strait Islander adults. Addressing these knowledge gaps is particularly relevant as access to diagnostic and treatment services for sleep related breathing disorders for Indigenous Australians is likely to be influenced by their lifestyle and cultural and geographic factors, all of which can impede access to health care and the ability to comply with management plans.
Study Impact: Our data from northern and central Australia have demonstrated that Aboriginal and Torres Strait Islander peoples have a reduced rate of use of diagnostic sleep services and there are significant difficulties in ensuring follow-up and thus, by extension, the implementation and refinement of treatment. Education regarding the health risks of untreated OSA and the benefits of treatment is essential, as is support for patients and local health care providers to persevere through the difficult adjustment period when commencing continuous positive airway pressure treatment therapy.
The reported prevalence of OSA in Australia varies5,6 with a range of methods used to define diagnostic criteria and populations, and is rapidly rising. Bearpark et al. reported a prevalence of OSA (defined as respiratory disturbance index [RDI] ≥ 10) of 9.9% among her sample of 294 Australian males aged 40– 65 y, with 3% of participants having symptoms.5 Olsen et al.'s Australian study of 1,233 males and 969 females aged 35–69 y reported a lower prevalence of OSA (apnoea-hypopnoea index [AHI] ≥ 15) of 3.6% in a sample encompassing a younger population; 5.7% in males and 1.2% in females.6 A report by the Sleep Health Foundation estimated the prevalence of OSA in Australia in 2010 was 4.7% or approximately 750,000 Australians.1 A recent Australian community cohort study reported an OSA (AHI ≥ 10) prevalence of 53% in males age 40 y or older, and a moderate (AHI 20–29) to severe (AHI ≥ 30) OSA prevalence of 26%.7 Comparable studies of indigenous peoples from New Zealand8 and Canada9 reported a Māori OSA prevalence of 14% (RDI ≥ 5), 11% (RDI ≥ 10) and 6% (RDI ≥ 15), and American Indian OSA prevalence of 33% (AHI 5–14) and 23% (AHI ≥ 15).
The Australian study reported prevalence is increasing and is thought to relate to a corresponding rise in comorbidities, particularly hypertension, diabetes, and obesity.7 Results from the 2009 annual South Australian Health Omnibus Survey found a high prevalence of factors associated with sleep related breathing disorders including: snoring 49.7%, waking unrefreshed 24.8%, excessive daytime sleepiness 27.7%, high blood pressure 28.3%, and overweight or obese 46.7%.10 Overall 57% of males and 20% of females were classified at high risk of OSA, with a combined prevalence of 27.8%, and increased risk with age.10
Despite its significant effect in Australia, the nature and burden of sleep related breathing disorders in Australia's adult Aboriginal and Torres Strait Islanders has not been studied. The three studies that have examined sleep health in Indigenous Australians have been restricted to children.11–13 Blunden and Chervin investigated symptoms of sleep disorders in 25 Indigenous and 25 matched non-indigenous participants aged 7–11 y in northern Australia.11 Sleep disordered breathing was reported in 5% of the sample (3% of Indigenous and 2% of non-indigenous children), and excessive daytime sleepiness was reported in 9% (5% of Indigenous and 4% of non-indigenous children). Cooper et al.'s similarly small study of 21 Indigenous children age 6–13 y in northern Australia suggested that increasing age was significantly associated with greater sleep latency and reduced sleep efficacy, and that movement during sleep and sleep fragmentation was associated with reduced academic performance.12 The third and larger study by Valery et al. investigated the prevalence of snoring and restlessness and its relationship with asthma in 1,650 Indigenous children in five communities in the Torres Strait region.13 The prevalence of restless sleep was 6% and snoring 14.2% and both were associated with a coexistent diagnosis of asthma.
Despite Aboriginal and Torres Strait Islander people having increased risk factors for OSA (diabetes, obesity) and high levels of comorbid associated conditions (chronic non-communicable diseases),14 there are currently no published data relating to the nature of sleep related breathing disorders affecting Aboriginal and Torres Strait Islander adults. Although there is considerable information from metropolitan services regarding diagnostic and management pathways for OSA, there is less information regarding care for Australians living in regional and remote Australia and particularly for Indigenous Australians. Addressing these knowledge gaps is particularly relevant as access to diagnostic and treatment services for sleep related breathing disorders for Indigenous Australians is likely to be influenced by their lifestyle, and cultural and geographic factors, all of which can impede access to healthcare and the ability to comply with management plans.1
The purpose of this study was therefore to compare the level of use of sleep services and prevalence of clinical factors associated with OSA and the management of OSA among Aboriginal and Torres Strait Islander peoples and non-indigenous people living in regional and remote northern and central Australia and to use this information to inform health service development, to highlight knowledge gaps and identify targets for future research and intervention.
METHODS
Setting
Study sites were hospital-based sleep clinics in Cairns Hospital in the tropical north and Alice Springs Hospital in the arid center of Australia (Figure 1). Cairns Hospital serves a population of approximately 250,000 people with a significant proportion of Aboriginal and Torres Strait Islander people (15% of the hospital catchment population are Indigenous Australians,15 compared with 3.6% in all of Queensland,16 and 2.5% for Australia overall16). The clinic is based at Cairns Hospital and is permanently staffed with two specialist sleep and respiratory physicians, a specialist trainee, one senior respiratory/sleep scientist, and two sleep technologists. Approximately 204 diagnostic PSG studies are performed each year [J. Ferns, personal communication, August 5, 2013]. All studies are performed in a hospital-based sleep laboratory. Medicare funded hospital or sleep clinic-based PSG studies require continuous monitoring of oxygen saturation and breathing using a multichannel polygraph, and recordings of electroencephalogram (EEG), electro-oculogram (EOG), submental electromyogram (EMG), anterior tibial EMG, respiratory movement, airflow, oxygen saturation, and electrocardiogram (ECG) and are performed with a technician in continuous attendance. Results are analyzed by the senior respiratory/sleep scientist and reported by a sleep physician. A physician and specialist trainee also conduct regular outreach clinics to remote communities in the health service catchment (Figure 1) to review current patients and assess referred patients. Although this is the only publically funded sleep clinic in the Cairns area and the Cape York and Torres Strait catchments north of Cairns, private sleep clinics also operate in this area. It is assumed most local Indigenous people utilize the public service due to the high cost of private sleep clinic studies17 and some non-indigenous residents may utilize private clinics or travel to larger centers for diagnostic studies.
Figure 1.

Study sites (Alice Springs and Cairns) and associated health service catchment (gray).
All Queensland residents in receipt of a welfare payment or a low-income concession card are eligible for a government-provided CPAP machine but patients must purchase the mask and tubing.
The central Australian site has a catchment population of approximately 45,000 people,18 of whom approximately 36.2% identify as Indigenous (predominantly Aboriginal Australians) compared with 26.8% in all of the Northern Territory.16 The sleep service is based at Alice Springs Hospital and provided by visiting respiratory and sleep physicians from Adelaide in South Australia working with local respiratory and sleep nurses, technicians and administrative staff (Figure 1). On average, 97 diagnostic sleep studies are performed each year (P. Singh, personal communication, August 6, 2013), and all are home based. Type II home-based sleep studies using Medicare-funded limited channel portable polysomnogram monitors are required to monitor a minimum of seven physiological parameters: continuous EEG, continuous ECG, airflow, thoracoabdominal movement, oxygen saturation, and at least two of the following: EOG, chin EMG, and body position.19 The main difference between hospital and home-based PSG is the presence or absence of a technologist. Portable monitors are an acceptable alternative to PSG and the available literature shows portable monitoring can be as accurate as PSG for diagnosis in populations without significant comorbidities.20
Central Australian sleep study results are analysed by senior sleep scientists and reported by senior sleep physicians in Adelaide. This is the only sleep clinic in central Australia and although it is assumed most local Indigenous people use this service,17 some non-indigenous residents may travel to large centers for diagnostic studies.
All central Australian residents in receipt of a disability or age pension and Indigenous Australian patients with complex chronic disease needs are eligible for a government-provided CPAP machine and initial mask and tubing.
Data Collection and Analysis
A retrospective audit was conducted in 2012–2013. Ethics approvals from the Cairns and Hinterland Hospital and Health Service District, central Australian human research ethics committees (HREC) and James Cook University HREC were obtained. Consecutive records of Indigenous and non-indigenous patients having diagnostic PSG were reviewed. The aim was to identify and review 50 Indigenous and 50 non-indigenous records that met the inclusion criteria at each site with a total of 200 records reviewed.
Inclusion criteria were PSG occurring prior to September 1, 2011 and apnoea-hypopnoea index (AHI) ≥ 5 if symptoms were present (snoring, witnessed apnoeas, motor vehicle accident due to fatigue, and history of fatigue/excessive daytime sleepiness) or AHI ≥ 15 in asymptomatic patients.
Data collected included: demographic information (age, sex, height, weight, body mass index (BMI), and indigenous status), comorbidities, indications for referral, Epworth Sleepiness Scale (ESS) score, PSG result, treatment prescription, and 12-mo follow-up and management of those in whom OSA was diagnosed. Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 20 (IBM SPSS, Chicago, IL, USA). Univariate statistics were used to describe the sample. Bivariate analyses were performed to compare Indigenous and non-indigenous data and differences between study sites. These included chi-square and Fisher exact test for categorical variables and t-tests or Mann-Whitney U tests for continuous variables depending on the normality of distribution. Rates/100,000 were calculated based on 2011 census data from the Australian Bureau of Statistics. Odds ratios were calculated to compare outcomes between groups. All tests were two sided and a p value less than 0.05 was taken to indicate statistical significance.
RESULTS
Overall 62% (200/324) of sequential studies reviewed met study selection criteria. This proportion did not vary by site (χ2 not significant). Aboriginal and Torres Strait Islander patients tended to be more likely to meet selection criteria (69%) compared with non-indigenous Australian patients (56%) but this difference was not statistically significant (χ2 p = 0.16). At both sites 17 mo of non-indigenous studies and 48 mo of Indigenous studies were reviewed to identify sufficient subjects who met inclusion criteria. Study subjects who did not meet the inclusion criteria included those with a documented AHI < 5 if symptoms were present or AHI < 15 in asymptomatic patients, and those with a diagnosis other than a sleep related breathing disorder (e.g., restless legs syndrome). No demographic or clinical information was collected from excluded studies.
Descriptive data relating to the study sample stratified by Indigenous and non-indigenous subjects are outlined in Table 1. Indigenous patients with a confirmed diagnosis of a sleep related breathing disorder were more likely to be female, live in a very remote location, have a coexistent chronic disease, and a higher BMI compared with non-indigenous Australian patients. Day time sleepiness as assessed by the ESS score and the clinical indications for referral were comparable.
Table 1.
Description of demographics and comorbidities in the study sample stratified by whether Aboriginal and/or Torres Strait Islander or non-indigenous patients.
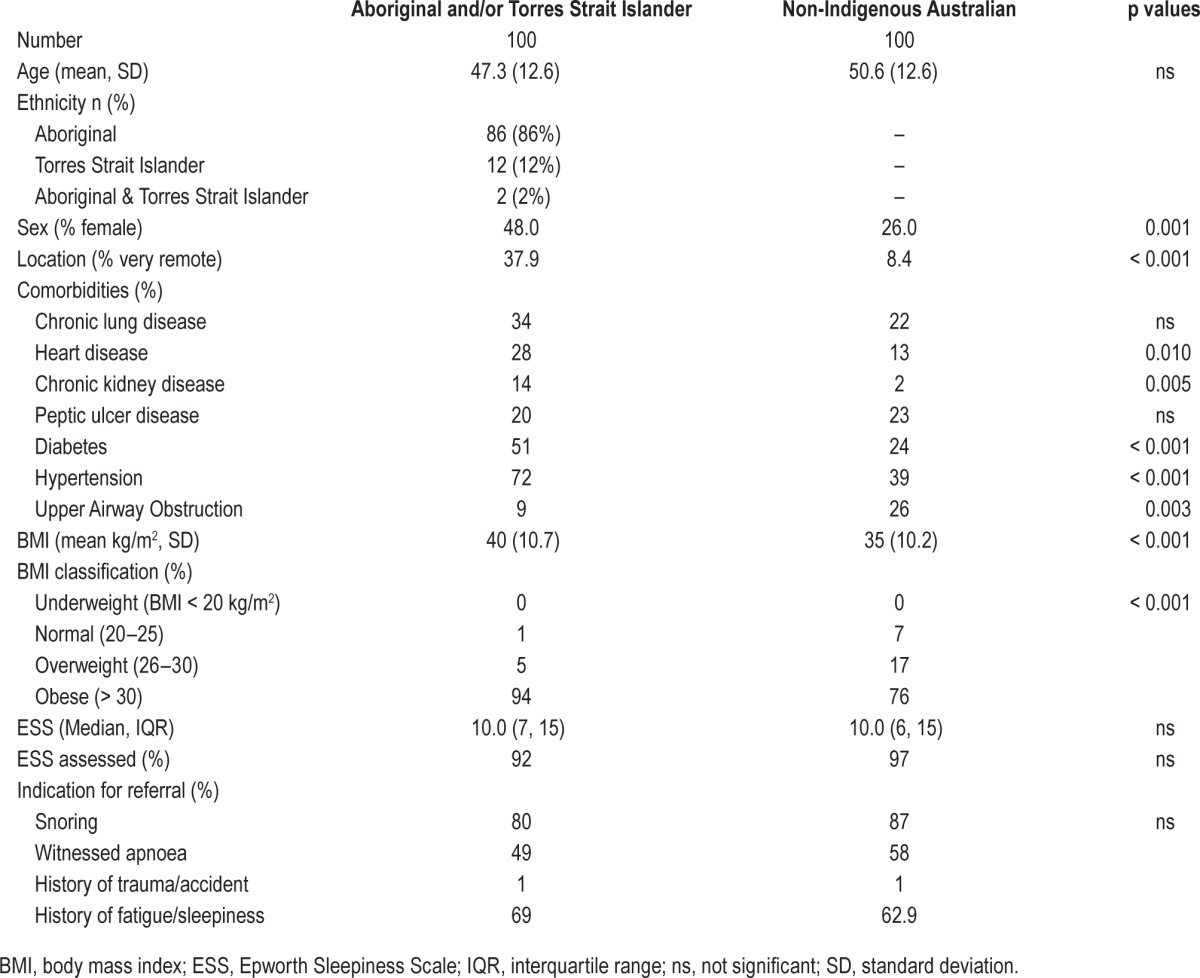
When Indigenous and non-indigenous subjects were compared at each study site, central Australian Indigenous patients were more likely to have heart disease (p = 0.003) and chronic kidney disease (p = 0.001) but less likely to have a clinician recorded diagnosis of upper airway obstruction (p = 0.001). Northern Australian Indigenous patients were more likely to have chronic obstructive pulmonary disease (p = 0.032), and Indigenous patients at both sites were more likely to have diabetes and hypertension (p < 0.05).
Diagnosis, treatment, and review data relating to the study sample stratified by indigeneity are outlined in Table 2. The majority of patients at both sites received a diagnosis of OSA and Indigenous and non-indigenous patients did not differ significantly in severity of OSA as assessed by AHI. Overall, 35 patients (17.5%) had an AHI greater than 5 and less than 15, and 165 (82.5%) had an AHI ≥ 15 ranging from 15 to 136.8. Median AHI was greater in central Australian (50.2, interquartile range [IQR] 25.3 – 84.4) than northern Queensland patients (21.9, IQR 11.0 – 41.9, p < 0.001).
Table 2.
Description of study sample regarding diagnosis and treatment stratified by whether Aboriginal and/or Torres Strait Islander or non-indigenous patients 2007–2011.
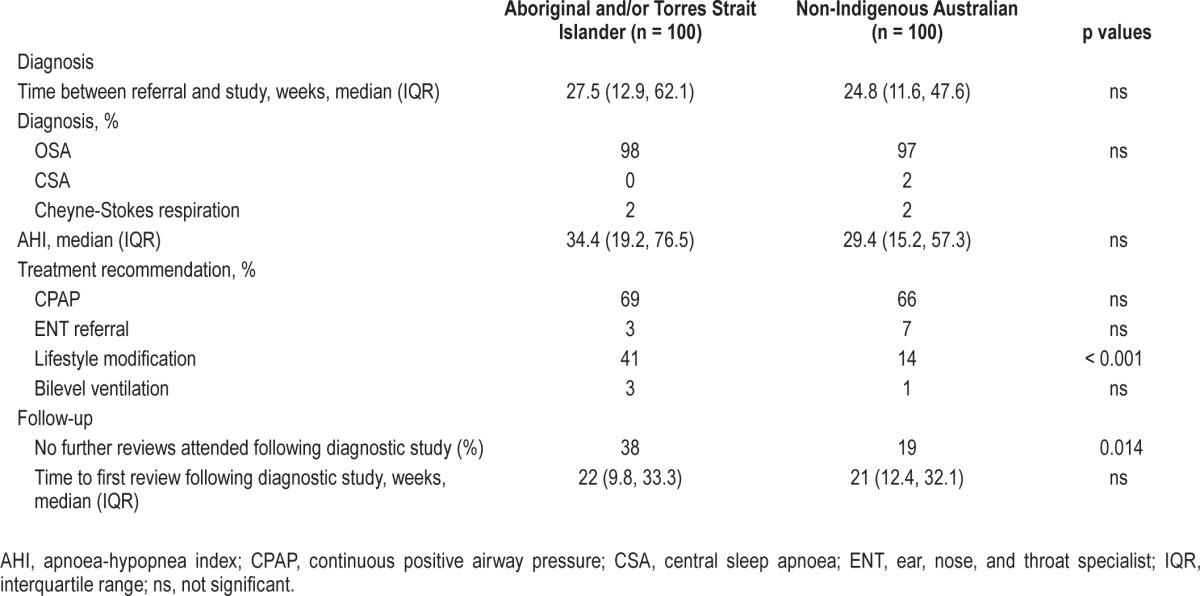
CPAP treatment was recommended for two-thirds of both Indigenous and non-indigenous patients. Indigenous patients were more likely to have documented lifestyle modification (weight loss) advice (42%, 95% confidence interval [CI] 32–52 compared with 14%, 8–23, p < 0.001), and were twice as likely not to attend follow-up appointments in the 12 mo following their diagnostic study (38%, 95% CI 27–49 compared with 19%, 11–30, p = 0.014).
When Indigenous and non-indigenous data were analyzed separately for each site, Indigenous patients at both sites were more likely to have documented lifestyle modification (weight loss) advice than non-indigenous patients (p < 0.05) whereas Indigenous patients in central Australia were less likely than non-indigenous patients to attend a review in the 12 mo after diagnostic PSG (p = 0.008).
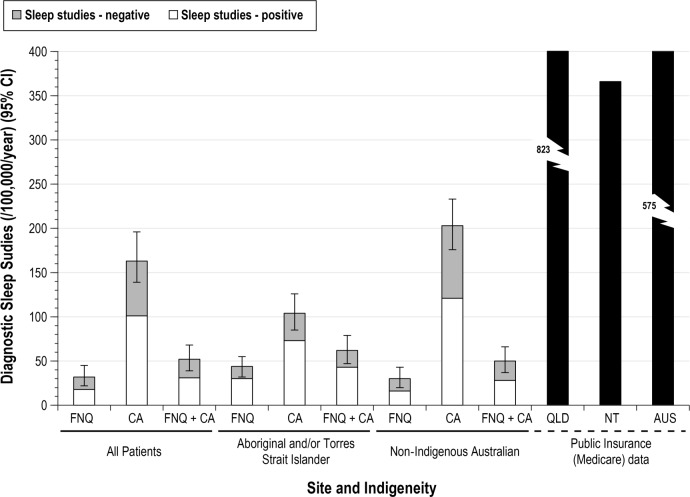
The annualized rates of performance of sleep studies and those subsequently confirmed to reflect an underlying sleep disorder per 100,000 population are presented in Figure 2.
Figure 2.
Rate of sleep studies performed per 100,000 population (divided by whether study subsequently confirmed a sleep related breathing disorder or not) in far north Queensland (FNQ), Central Australia (CA) and (combined (FNQ+CA) stratified by whether Aboriginal and/or Torres Strait Islander or non-indigenous Australian patients. Comparative Medicare rebate data for sleep studies performed are provided for Queensland (QLD), Northern Territory (NT), and Australia (AUS) overall (www.medicareaustralia.gov.au). Note: Medicare data includes diagnostic as well as titration studies, and also repeated studies.
Based on the hospital population catchment of each region and the number of diagnostic sleep studies undertaken over the period of review, Aboriginal and Torres Strait Islander people were 1.8 times more likely to have a positive diagnostic sleep study performed/100,000 adult population/y compared with non-indigenous patients (odds ratio [OR] 1.8, p = 0.016, 95% CI 1.1–2.8), 1.6 times less likely (OR 1.6, p = 0.416, 95% CI 0.5–5.3) in central Australia and 3.4 times more likely (OR 3.4, p = 0.0045, 95% CI 1.5–7.9) in far north Queensland. Aboriginal and Torres Strait Islander patients were also twice as likely (OR 2.2, p = 0.007, 95% CI 1.2–3.8) not to attend follow-up appointments in the 12 mo following their diagnostic study. This was particularly the case in central Australia (OR 3.1, p = 0.008, 95% CI 1.3–7.2) with follow-up not being significantly different in far north Queensland (OR 1.6, p = 0.225, 95% CI 0.7–3.7).
DISCUSSION
Residents of regional and remote Australia often face a range of barriers to accessing health care including specialist services. This is particularly the case for Aboriginal and Torres Strait Islander peoples who are more likely to reside in such settings. Nonetheless, the effect of remoteness is also shared with non-indigenous Australians. The effect of residing in a remote area as compared to the general urbanized Australian population, with regard to accessibility of sleep studies and OSA treatments, may be greater that the effects of ethnicity. Health care accessibility barriers relate not only to local health service systems but also include individual beliefs, knowledge, prior experience, and competing priorities which in turn influence health care seeking behaviors. We have reported here the first study to provide an insight into the nature and care of sleep disorders in a regional and remote Australian setting with a particular focus on Aboriginal and Torres Strait Islander people.
Findings from this study indicate that Aboriginal and Torres Strait Islander patients with a confirmed sleep related breathing disorder are less likely to attend for follow-up care. Anecdotal evidence indicates accessibility in this setting is affected by remoteness, unfamiliarity with the concept of sleep disordered breathing, screening processes and criteria, systems for booking of appointments, variable health self-efficacy, the complex nature of treatment tools such as CPAP, need for electricity, environmental and behavioral issues affecting sleep hygiene, and personal commitment to chronic care.
Compared with non-indigenous patients, Aboriginal and Torres Strait Islander patients with a confirmed sleep related breathing disorder were younger and were more likely to be female and reside in a remote community. In addition comorbidities and obesity were more prevalent in this selected population. This higher prevalence of comorbidities in part reflects the greater burden of these conditions borne by Australian Aboriginal and Torres Strait Islander people. Nonetheless, it also indicates the increased risk and greater absolute contribution sleep related breathing disorders, and especially OSA, are likely to make to the Aboriginal and Torres Strait Islander health disadvantage, particularly as this relates to heart and lung disease, diabetes, and hypertension.
Residing in a remote community contributes to the difficulty in accessing specialized sleep services. Although northern Queensland sleep physicians conduct outreach clinics in remote communities, this does not occur in remote central Australian communities. However, patients in remote northern Queensland and central Australia must still travel long distances to access sleep services. Our data would nonetheless suggest that even in the absence of remote outreach services the uptake of diagnostic studies, while remaining less than Australia overall, is greater in central Australia compared with northern Queensland.
Although the provision of diagnostic sleep services per 100,000 population in central Australia was greater than that in northern Queensland (104 Indigenous and 203/100,000 non-indigenous studies in central Australia, 44 Indigenous and 30/100,000 non-indigenous studies in northern Australia) the subsequent follow-up was less. The explanations for these differences are, as reported in other studies, likely to include difficulties with remoteness, language, available transport, financial difficulties, and the accessibility of culturally appropriate healthcare services.17 Although remote specialist outreach in northern Queensland may not have enhanced accessibility to diagnosis, and indeed may have diverted patients away from the need for PSG, it may also have enhanced follow-up following a diagnosis based on the greater proportion of patients having a review in northern Queensland in the 12 mo following diagnosis.
Inpatient PSG studies were not available in central Australia due to bed space constraints. The sole use of ‘home-based’ PSG studies is likely to create an additional accessibility barrier for all people, and particularly Aboriginal Australians living in circumstances not suitable for performing studies or where remote area of residence means equipment and expertise are not available to undertake such studies. The selection of patients to undergo a sleep study includes an assessment of their capacity and willingness to be treated. If they are unable to have a sleep study due to remoteness, homelessness, or a lack of electricity, then it is much more difficult to consider treatment with CPAP. This policy is likely to have affected a higher proportion of Aboriginal patients in central Australia. In such settings a new approach and model of care for diagnosis and management is required. Furthermore, the concept of treatment with devices and their ongoing care, and the capacity to review patients are dominant issues in this setting and require a new approach and model of care. A greater shared understanding of systems of care, linking patients and care providers, is likely to yield insights into how service development initiatives such as information sharing, screening tool validation, and telehealth may be used to enhance care in remote settings.
Although Indigenous Australians may have particular difficulty in accessing sleep diagnostic services the issue in regional and remote Australia also affects, to a lesser extent, non-indigenous Australians (Figure 1). In 2012, Medicare data shows 671 clinic-based PSG studies and 152 home-based PSG studies per 100,000 population were performed in Queensland.21 In comparison, 30 non-indigenous and 44 Indigenous clinic-based sleep studies per 100,000 population were performed in our northern Queensland catchment. In 2012, Medicare data shows 201 clinic-based and 165 home-based PSG studies per 100,000 population were performed in the Northern Territory21 compared with 203 non-indigenous and 104 Indigenous home-based PSG studies per 100,000 population performed in central Australia. Although there are no accurate data regarding the underlying burden of sleep related breathing disorders in regional and remote Australia, these data from northern and central Australia nonetheless would suggest that all Australians, and particularly Aboriginal and Torres Strait Islander people residing in rural and remote regions, face barriers to accessing sleep diagnostic and management services.
It is more difficult to ascertain the level of accessibility to sleep services for non-indigenous Australians given the opportunities that such patients, based on often being less remote and more affluent, have in accessing distant urban and private sleep diagnostic and treatment services. Nonetheless, the possibility we have underestimated accessibility for non-indigenous patients would widen the gap in comparison with Aboriginal and Torres Strait Islander patients. This is unlikely to fully explain the substantial differences we have noted between our non-indigenous patients and national and jurisdictional data regarding sleep diagnostic services (Figure 2). One potential explanation for this gap may also be that health care providers who work with Indigenous patients have only recently become more aware of the effect of sleep related breathing disorders on health.
The ESS is currently used in Australia to assess excessive daytime sleepiness and, although not specifically validated for use in this or other settings, is often used as a de facto screening tool to prioritize referral to diagnostic sleep services. Although ESS scores of Indigenous and non-indigenous Australians did not differ significantly, the ESS has not been validated in the Indigenous population. Cultural and linguistic differences in the meaning of fatigue and daytime sleepiness may have biased the results. Finally, the ESS refers to watching television, driving and being a passenger in a car, and sitting in a theater or a meeting.22 Residents in remote Australian communities, and particularly Aboriginal and Torres Strait Islander people, often bear significant social and economic disadvantage14; they may not have electricity or a car and would rarely attend the theatre due to the distance involved. Thus, scores for these questions will necessarily be low because sleepiness does not occur in such contexts. Linguistic differences and delivery of the questionnaire in English are also likely to prevent accurate rating of ESS items in a setting where English is often one of many languages spoken. Additionally, male subjective sleepiness differs from that of females in the non-indigenous people and it is critical to understand whether this is the same or different in Indigenous Australians.23–26
Rather than use an unvalidated tool, the priority should therefore be to develop and validate an appropriate screening tool for Aboriginal and Torres Strait Islander people. Given the significant existing uptake of the ESS, it is nonetheless likely the utility and utilization of an appropriate and validated tool will be high.
Making a diagnosis of a sleep related breathing disorder is only the initial step in the journey to addressing the problem. Additional steps must necessarily include agreeing on a management plan, follow-up to assess response and titrating or altering treatment. Although waiting times, diagnoses (including severity), and treatment prescriptions were comparable, the fact that all patients waited on average 6 mo for a sleep study would indicate significant opportunities to enhance pathways to diagnosis. Although Indigenous and non-indigenous Australians waited an average of 6 mo for PSG testing, this was nonetheless comparable to that seen elsewhere in Australia including in urban settings.27 The proportion of positive tests seen in this study, and particularly for Aboriginal and Torres Strait Islander people, and the higher prevalence of associated comorbidities in indigenous patients may suggest that a degree of selective referral may be occurring. In this case there may be an emphasis on selecting those who are willing and able to be treated subsequently given that a diagnosis per se is un-helpful if no benefits follow. The development of a validated screening tool for this population would serve to ensure more efficient use of available and finite services, with only those at high risk for sleep related breathing disorders and with the capacity for therapy being referred and reviewed.
Of particular note, Indigenous Australians were twice as likely to not attend any follow-up appointments in the 12 mo following diagnosis, with more than half being essentially lost to follow-up. Although this study did not specifically map the details of follow-up after diagnosis it is likely geographic isolation, the financial cost associated with commencing and maintaining treatment, and patient, family, and primary health care understanding of the value and aims of treatment may all have been relevant. A more detailed understanding of these and other barriers and enablers to treatment uptake will be important in informing the future development of treatment services for sleep related breathing disorders in Aboriginal and Torres Strait Islander and remote populations.
Given the high and increasing prevalence estimates of OSA in the Australian population, the low rate of diagnosis, and the considerable health consequences of untreated OSA, it is important that culturally and linguistically appropriate diagnosis, education, and care pathways for Indigenous Australians are identified and implemented. Engagement with Aboriginal and Torres Strait Islander people, and especially Indigenous people already working in health care, will be fundamental to the development of culturally appropriate screening tools, clinical pathways for diagnosis, and overall models of care.
Recent Australian studies with non-indigenous populations have shown that accurate diagnosis of clinically significant OAS using a simplified two stage model of care28 and nurse-led care of OSA29 is not inferior to traditional methods of diagnosis and care and has potential cost benefits. However, the additional and unaccounted influence of remoteness, socioeconomic factors, and comorbidities in Indigenous populations means trials of these models are needed to expand our understanding and capacity to develop tailored models of care for underdiagnosed groups. In 2004–2005 an estimated 27% of all Indigenous Australians age 18 y and older lived in overcrowded households; Northern Territory 65%, Queensland 29%.30 It is inevitable that those living in overcrowded households will experience a level of sleep disruption and these and other factors must be taken into account when developing tailored screening tools and models of care.
Limitations
The retrospective nature of this study meant it was limited by reliance on existing documentation in patient records. Review and treatment information, which may have occurred but was not recorded on patient records, could be underreported in our study. Nonetheless, given the substantial differences seen in comparison to national data, this is unlikely to alter the findings of this study.
CONCLUSION
Sleep related breathing disorders are a significant issue in Australia. Although Aboriginal and Torres Strait Islander people are likely to be subject to an equivalent or increased risk of disease, there are currently no published data to inform the development of screening, diagnostic, and management pathways that reflect the realities of regional and remote Australia and the needs and beliefs of Indigenous Australians. However, previous studies of chronic condition management in Indigenous communities have identified similar barriers to care as did this study and also successfully trialled management strategies tailored to suit a remote and Indigenous Australian setting.31,32 Our data from northern and central Australia has demonstrated that Aboriginal and Torres Strait Islander peoples have a reduced rate of use of diagnostic sleep services. We have also shown there are significant difficulties in ensuring follow-up and thus, by extension, the implementation and refinement of treatment. Further innovation in health service delivery and research is needed to develop and validate tools and care pathways for OSA screening, diagnosis and treatment for residents of regional and remote Australia and particularly for Aboriginal and Torres Strait Islander people. It will be important to ensure screening tools are validated for this relatively unique setting, and to identify and address barriers to treatment uptake to ensure a valid and rational approach to the utilisation of diagnostic and management services for sleep related breathing disorders.
There is increasing recognition of the importance of involving Aboriginal and Torres Strait Islander people with chronic conditions as active partners in their care and self-management of their condition. Health may not however always be a priority with other pressing issues to cope with. Education regarding the health risks of untreated OSA and the benefits of treatment is essential, as is support for patients and local health care providers to persevere through the difficult adjustment period when commencing CPAP treatment therapy.
DISCLOSURE STATEMENT
This was not an industry supported study. This project received funding from an internally competitive James Cook University Faculty Grant. A/Prof. Maguire is supported by an NHMRC Practitioner Fellowship and the Margaret Ross Chair in Indigenous Health. The authors have indicated no financial conflicts of interest. Work on this project was performed at Cairns Hospital, Alice Springs Hospital, and James Cook University.
ACKNOWLEDGMENTS
The authors thank Dr. Tri Susilawati and Ms. Louise Burns for their assistance with data collection and data entry and the medical records staff of Cairns and Alice Springs Hospitals.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- BMI
body mass index
- CPAP
continuous positive airway pressure
- CSA
central sleep apnea
- EEG
electroencephalogram
- ENT
ear, nose, and throat specialist
- EMG
electromyogram
- EOG
electro-oculogram
- ESS
Epworth Sleepiness Scale
- HREC
human research ethics committees
- IQR
interquartile range;
- OSA
obstructive sleep apnea
- PSG
polysomnography
- RDI
respiratory disturbance index
- SD
standard deviation
REFERENCES
- 1.Canberra: Sleep Health Foundation; 2011. Deloitte Access Economics Reawakening Australia: The Economic Cost of Sleep Disorders in Australia, 2010. [Google Scholar]
- 2.American Academy of Sleep Medicine. Chicago, IL: American Academy of Sleep Medicine; 2001. International classification of sleep disorders, revised: diagnostic and coding manual. [Google Scholar]
- 3.Usmani ZA, Chai-Coetzer CL, Antic NA, McEvoy RD. Obstructive sleep apnoea in adults. Postgrad Med J. 2013;89:148–56. doi: 10.1136/postgradmedj-2012-131340. [DOI] [PubMed] [Google Scholar]
- 4.Thoracic Society of Australia and New Zealand, Australasian Sleep Association, Australian Lung Foundation. Sydney: Thoracic Society of Australia and New Zealand; 2010. Respiratory and sleep health in Indigenous Australians. [Google Scholar]
- 5.Bearpark H, Elliott L, Grunstein R, et al. Occurrence and correlates of sleep disordered breathing in the Australian town of Busselton: a preliminary analysis. Sleep. 1993;16:S3–5. [PubMed] [Google Scholar]
- 6.Olson L, King M, Hensley M, Saunders N. A community study of snoring and sleep-disordered breathing. Prevalence. Am J Respir Crit Care Med. 1995;152:711–16. doi: 10.1164/ajrccm.152.2.7633731. [DOI] [PubMed] [Google Scholar]
- 7.Adams R, Appleton S, Vakulin A, et al. High prevalence of undiagnosed OSA in a community sample of men aged 40 years and over. Sleep Biological Rhythms. 2012;(Suppl 1):42. [Google Scholar]
- 8.Mihaere K. New Zealand: Wellington Campus; 2004. Obstructive sleep apnoea in Aotearoa/New Zealand: an objective and questionnaire-based approach to population prevalence and clinical screening: a thesis presented in partial fulfilment of the requirements for the degree of Doctor of Philosophy in Public Health at Massey University. [Google Scholar]
- 9.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–39. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 10.Adams RJ, Piantadosi C, Appleton SL, et al. Investigating obstructive sleep apnoea: will the health system have the capacity to cope? A population study. Aust Health Rev. 2012;36:424–9. doi: 10.1071/AH11098. [DOI] [PubMed] [Google Scholar]
- 11.Blunden S, Chervin RD. Sleep, performance and behaviour in Australian indigenous and non-indigenous children: an exploratory comparison. J Paediatr Child Health. 2010;46:10–6. doi: 10.1111/j.1440-1754.2009.01610.x. [DOI] [PubMed] [Google Scholar]
- 12.Cooper P, Kohler M, Blunden S. Sleep and academic performance in Indigenous Australian children from a remote community: an exploratory study. J Paediatr Child Health. 2012;48:122–7. doi: 10.1111/j.1440-1754.2011.02059.x. [DOI] [PubMed] [Google Scholar]
- 13.Valery PC, Masters IB, Chang AB. Snoring and its association with asthma in Indigenous children living in the Torres Strait and Northern Peninsula Area. J Paediatr Child Health. 2004;40:461–5. doi: 10.1111/j.1440-1754.2004.00428.x. [DOI] [PubMed] [Google Scholar]
- 14.Trewin D. National Aboriginal and Torres Strait Islander Health Survey, Australia, 2004-05. Australian Bureau of Statistics. 2006 [Google Scholar]
- 15.Internal Medicine Society of Australia and New Zealand. [cited 7 August 2013]; Available from: http://www.imsanz.org.au/jobs/QLD-training-sites/cairns-base-hospital.
- 16.Australian Bureau of Statistics. 2011 Census QuickStats. [cited 7 August 2013]; Available from: http://www.censusdata.abs.gov.au/census_services/getproduct/census/2011/quickstat/3?opendocument&navpos=220.
- 17.Australian Bureau of Statistics & Australian Institute of Health and Welfare. Canberra: ABS & AIHW; 2008. The health and welfare of Australia's Aboriginal and Torres Strait Islander peoples 2008. ABS cat. no. 4704.0. AIHW cat. no. IHW 21. [Google Scholar]
- 18.Secombe P, Stewart P, Brown A, Brown PSA. Functional outcomes in high risk ICU patients in Central Australia: a prospective case series. Rural Remote Health. 2013;13:2128. [PubMed] [Google Scholar]
- 19.Allen RK. Diagnostic tests - home sleep studies. Aust Prescr. 2012;35:62–4. [Google Scholar]
- 20.Collop NA, Anderson WM, Boehlecke B, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. J Clin Sleep Med. 2007;3:737–47. [PMC free article] [PubMed] [Google Scholar]
- 21.Medicare Australia. Medicare Item Reports. 2013. [cited 25 July 2013]; Available from: https://www.medicareaustralia.gov.au/statistics/mbs_item.shtml.
- 22.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 23.Baldwin CM, Kapur VK, Holberg CJ, Rosen C, Nieto F. Associations between gender and measures of daytime somnolence in the Sleep Heart Health Study. Sleep. 2004;27:305–12. doi: 10.1093/sleep/27.2.305. [DOI] [PubMed] [Google Scholar]
- 24.Chervin RD, Aldrich MS. The Epworth Sleepiness Scale may not reflect objective measures of sleepiness or sleep apnea. Neurology. 1999;52:125–31. doi: 10.1212/wnl.52.1.125. [DOI] [PubMed] [Google Scholar]
- 25.Chervin RD. Sleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apnea. Chest. 2000;118:372–9. doi: 10.1378/chest.118.2.372. [DOI] [PubMed] [Google Scholar]
- 26.Lindberg E, Janson C, Gislason T, Björnsson E, Hetta J, Boman G. Sleep disturbances in a young adult population: can gender differences be explained by differences in psychological status? Sleep. 1997;20:381–7. doi: 10.1093/sleep/20.6.381. [DOI] [PubMed] [Google Scholar]
- 27.Flemons WW, Douglas NJ, Kuna ST, Rodenstein DO, Wheatley J. Access to diagnosis and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med. 2004;169:668–72. doi: 10.1164/rccm.200308-1124PP. [DOI] [PubMed] [Google Scholar]
- 28.Chai-Coetzer CL, Antic NA, Rowland LS, et al. A simplified model of screening questionnaire and home monitoring for obstructive sleep apnoea in primary care. Thorax. 2011;66:213–9. doi: 10.1136/thx.2010.152801. [DOI] [PubMed] [Google Scholar]
- 29.Antic NA, Buchan C, Esterman A, et al. A randomized controlled trial of nurse-led care for symptomatic moderate-severe obstructive sleep apnea. Am J Respir Crit Care Med. 2009;179:501–8. doi: 10.1164/rccm.200810-1558OC. [DOI] [PubMed] [Google Scholar]
- 30.Australian Bureau of Statistics. Canberra: ABS; 2006. National Aboriginal and Torres Strait Islander Health Survey 2004-05. ABS cat. no. 4715.0. [Google Scholar]
- 31.Kowanko I, Helps Y, Harvey P, et al. Adelaide: Flinders University and the Aboriginal Health Council of South Australia; 2012. Chronic Condition Management Strategies in Aboriginal Communities: Final Report 2011. [Google Scholar]
- 32.Ware V. Resource sheet no. 27 produced for the Closing the Gap Clearinghouse. Canberra: Australian Government; 2013. Improving the accessibility of health services in urban and regional settings for Indigenous people. [Google Scholar]