Abstract
Wilson disease (WD) is an autosomal recessive disorder of copper metabolism resulting in copper accumulation in a number of organs including the liver, brain, and cornea, predominantly leading to hepatic, neurologic, and psychiatric manifestations. An association between WD and sleep problems is not commonly recognized, and sleep complaints are often overlooked. Daytime hypersomnolence is even more rarely reported in this population. We report a case of WD and hypersomnolence objectively confirmed by a multiple sleep latency test (MSLT). Consequently, we suggest that increased awareness, assessment, and treatment of sleep disorders, including daytime sleepiness, may help improve patients' quality of life.
Citation:
Amann VC, Maru NK, Jain V. Hypersomnolence in Wilson disease. J Clin Sleep Med 2015;11(11):1341–1343.
Keywords: Wilson disease, hypersomnolence, excessive daytime sleepiness, sleep disturbance
REPORT OF CASE
A 26-year-old woman presented with excessive daytime sleepiness (EDS) for about 3 months. She had been diagnosed with WD 9 years prior, after presenting with elevated liver function tests. Kayser-Fleischer rings were noted on exam. WD was diagnosed on laboratory tests and urinalysis. A liver biopsy showed micronodular hepatic cirrhosis and strongly positive rhodanine staining for copper in many histiocytes and hepatocytes. The patient was diagnosed with anxiety and bipolar disorder four and seven years later, respectively, which at the time of presentation, was well controlled on escitalopram 10 mg and lamotrigine 50 mg a day.
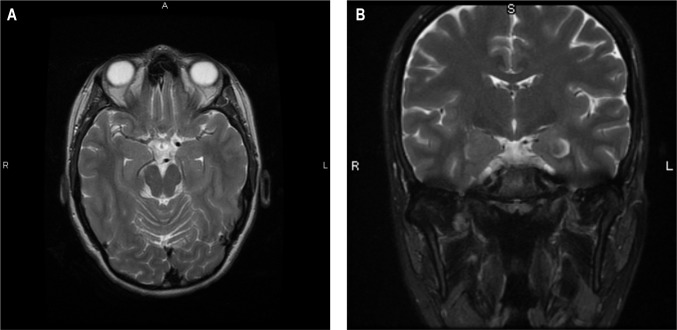
The patient reported excessive daytime sleepiness despite sleeping 7–8 h/night, which manifested in falling asleep at work, usually leading to a 3- to 5-minute nap. She mentioned feeling better after involuntary naps and also reported waking 1–2 times per night, usually from nightmares. Her Epworth Sleepiness Scale (ESS) score was 13. She denied any snoring, choking, or gasping for air and did not admit to any symptoms of cataplexy, sleep paralysis, acting out dreams, or abnormal leg movements. She further denied any abnormal sensations, difficulty falling asleep or general restlessness. Her partner did not recall her acting out dreams or any excessive motor activity. For WD, the patient was initially treated with D-penicillamine for 2.5 years, followed by a combination of D-penicillamine and zinc for 6 months. At the time of presentation, she was on maintenance therapy with 50 mg of zinc a day while avoiding copper-rich foods. She had normal serum and 24-h urine levels of copper and zinc and LFTs. CBC, iron, and ferritin measures were within normal limits (Table 1). She had normal brain magnetic resonance imaging (MRI; Figure 1) and head magnetic resonance angiography (MRA). Her physical examination, including full neurologic examination, was normal.
Table 1.
Laboratory values including CBC, ferritin, and iron.
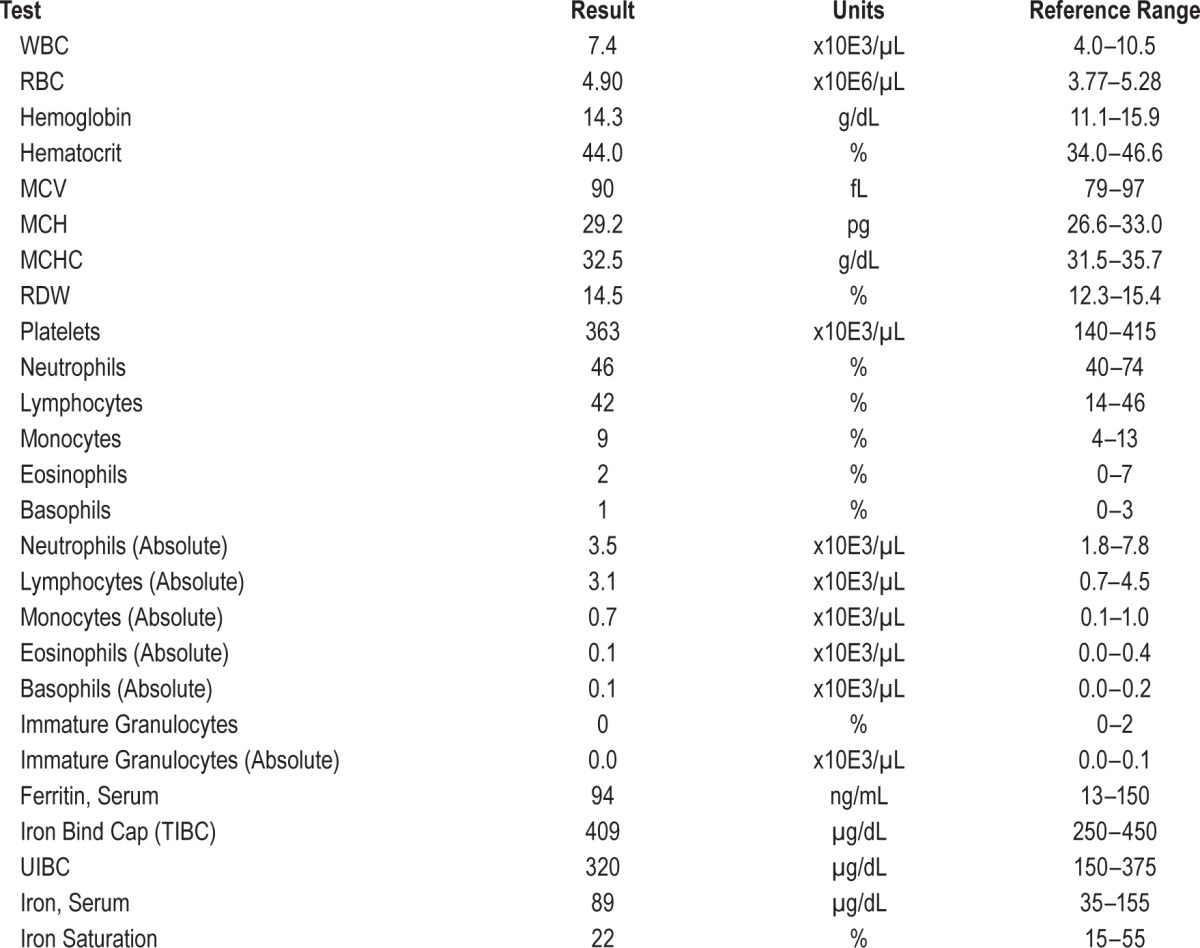
Figure 1. Brain MRI scans.
(A) Axial T2-weighted sequence. (B) Coronal T2-weighted sequence.
The patient underwent overnight polysomnography (PSG) followed by a multiple sleep latency test (MSLT). PSG did not show any abnormality that would explain her EDS: total sleep time was 8.5 h, she had normal sleep continuity, apnea-hypopnea index was 1.5 events/h, and there were no periodic limb movements of sleep (limb movement index 0.0). The number of awakenings was 16 (1.58/h), wakefulness after sleep onset (WASO) was 55.0 min, sleep efficiency was 83.6% and sleep latency was 44.5 min. She was on escitalopram at the time of the PSG. The MSLT with 5 nap opportunities demonstrated a mean sleep onset latency (SOL) of 2.2 min, without sleep-onset REM periods (SOREMPs), consistent with a diagnosis of hypersomnolence.
The patient was opposed to taking stimulant medication, given her history of bipolar disorder. Since presentation, her EDS has not subjectively improved. She is currently managing it by taking scheduled naps during the day and has stopped driving altogether.
DISCUSSION
Our findings are consistent with a possible association between WD and hypersomnolence, with compelling objective data (MSLT) supporting the subjective complaints. The prevalence of idiopathic hypersomnolence is about 1/100,000. In most populations WD has a prevalence of 1/30,000. Therefore, the likelihood of these two disorders co-occurring by chance would be about 1 in 3 billion. Such an association has been reported before, with hypersomnia as the main presenting symptom of WD. Unlike in our patient, hypersomnolence was present when WD was not controlled, and resolved gradually with D-penicillamine treatment.1
The prevalence of sleep disturbances in WD patients ranged from 40% to 80% in several questionnaire-based studies. Sleep abnormalities consisted mainly of increased nocturnal awakenings, daytime fatigue, and features related to alterations in REM sleep regulation (cataplexy and sleep paralysis). Of note, WD patient cohort numbers ranged from 24 to 55 patients in these studies.2–4
Data implicating Wilson disease in hypersomnolence are limited and inconsistent. This may be because of the subjective and variable nature of questionnaire-based characterization of sleepiness. The only other study using an objective MSLT assessment confirmed a higher than expected prevalence of shorter SOL in WD.3 Specifically, Portala et al. did not find any significant differences in reported daytime sleepiness between WD patients and controls using a standardized questionnaire, but no objective methods.4 On the other hand, Nevsimalova et al. did find a higher prevalence of excessive daytime sleepiness in their cohort of WD patients compared to controls (25.5% vs 9.1%, p = 0.043). The mean ESS score, evaluated by Mann-Whitney rank sum test, was higher in WD patients (7.945 ± 4.71 vs 6.057 ± 2.96; p = 0.046). 24 of 55 WD patients also underwent PSG followed by a MSLT. Pathologic sleepiness (mean SOL ≤ 8 min) was found in 4 of 24 patients.3 In another questionnaire-based study, no statistically significant difference in mean ESS score was found between patients and controls. This study, however, found that patients with duration of illness > 8 years and those on decoppering treatment reported significantly less daytime sleepiness.2 This is at odds with our patient, who had been diagnosed with WD nine years prior, which was well controlled.
Whether D-penicillamine reduces the risk of EDS remains to be determined. Firneisz et al. reported resolution of EDS in their patient after treatment.1 In addition, Netto et al. noted in subgroup analysis that patients on decoppering treatment had less daytime somnolence.2 However, our patient had not received D-penicillamine for 6 years before experiencing excessive daytime sleepiness. There are presently no studies specifically examining the effects of decoppering agents on sleep in patients with WD. Indeed, further studies with larger WD patient cohorts using objective methods are needed to comprehensively characterize sleep in WD and provide more robust epidemiological data.
Liver disease has been associated with daytime sleepiness. However, cirrhosis tends to be associated with circadian abnormalities and subsequent inversion of sleep pattern rather than with hypersomnolence.5 Our patient was diagnosed with cirrhosis nine years prior and did not display any circadian rhythm abnormalities.
We feel that her hypersomnolence is most likely a consequence of WD, perhaps secondary to central neural structural or functional changes that may or may not be detectable on MRI. The association we report should serve to increase the awareness of sleep disorders, particularly hypersomnolence, in WD patients. This has implications for proactive interventions to minimize consequences such as motor vehicle accidents, and improve quality of life. Further research is needed to delineate the pathophysiologic mechanisms linking WD to EDS.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest. This work was performed at the George Washington University in Washington, DC. Informed consent to publish this report was obtained from the patient described in this manuscript.
ABBREVIATIONS
- CBC
complete blood count
- EDS
excessive daytime sleepiness
- ESS
Epworth Sleepiness Scale
- LFTs
liver function tests
- MSLT
multiple sleep latency test
- PSG
polysomnography
- SOL
sleep onset latency
- SOREMPs
sleep-onset rapid eye movement periods
- WASO
wake after sleep onset
- WD
Wilson disease
REFERENCES
- 1.Firneisz G, Szalay F, Halasz P, Komoly S. Hypersomnia in Wilson's disease: an unusual symptom in an unusual case. Acta Neurol Scand. 2000;101:286–8. doi: 10.1034/j.1600-0404.2000.101004286.x. [DOI] [PubMed] [Google Scholar]
- 2.Netto AB, Sinha S, Taly AB, Panda S, Rao S. Sleep in Wilson's disease: questionnaire based study. Ann Indian Acad Neurol. 2011;14:31–4. doi: 10.4103/0972-2327.78047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nevsimalova S, Buskova J, Bruha R, et al. Sleep disorders in Wilson's disease. Eur J Neurol. 2011;18:184–90. doi: 10.1111/j.1468-1331.2010.03106.x. [DOI] [PubMed] [Google Scholar]
- 4.Portala K, Westermark K, Ekselius L, Broman JE. Sleep in patients with treated Wilson's disease. A questionnaire study. Nord J Psychiatry. 2002;56:291–7. doi: 10.1080/08039480260242796. [DOI] [PubMed] [Google Scholar]
- 5.De Cruz S, Espiritu JR, Zeidler M, Wang TS. Sleep disorders in chronic liver disease. Semin Respir Crit Care Med. 2012;33:26–35. doi: 10.1055/s-0032-1301732. [DOI] [PubMed] [Google Scholar]