Abstract
Objective
Research and interventions targeting the relationship between work, its attendant occupational hazards, and obesity are evolving but merit further consideration in the public health arena. In this discussion paper, conceptual heuristic models are described examining the role of obesity as both a risk factor and health outcome in the occupational setting.
Methods
PubMed was searched using specific criteria from 2000 and onwards for evidence to support conceptual models in which obesity serves as a risk factor for occupational disease or an outcome of occupational exposures. Nine models are presented: four where obesity is a risk factor and five where it is an adverse effect.
Results
A broad range of work-related health effects are associated with obesity including musculoskeletal disorders, asthma, liver disease, and cardiovascular disease, among others. Obesity can be associated with occupational hazards such as shift work, sedentary work, job stress, and exposure to some chemicals.
Conclusion
Identification of combinations of risk factors pertinent to obesity in the occupational environment will provide important guidance for research and prevention.
Keywords: cardiovascular disease, diet, endocrine disruptor, intervention study, metabolism, musculoskeletal disease, occupational health, physical activity, risk assessment
Obesity is increasing worldwide with the 2009–2010 prevalence among US adults surpassing one-third (1, 2). Obesity is associated with genetic, behavioral, occupational, and environmental factors (3–5) and has significant economic impact (6). It is also associated with various health problems including musculoskeletal disorders (MSD), asthma, liver disease, and cardiovascular disease (CVD) (7–10). Moreover, neurohormonal and endocrine pathway disruption has been associated with obesity (11, 12). Work factors, including sedentary work and task-related biomechanics, have been reported as risks for obesity (13–15). Variables such as irregular work hours/sleep schedules, job stress, workplace absenteeism, and reduced productivity also contribute (16–19).
Although the related literature is growing, obesity in the occupational environment requires more study, for example, regarding low-wage workers and genes or other factors (20, 21). Body mass index (BMI), a measure of obesity, varies by population, race, gender, and socioeconomic class (22–24). Genetics may account for ≥40% of the variation in BMI (25), but such estimates can depend on the variability of environmental risk factors observed. Although major genetic changes have not accompanied the rapid rise in obesity, genes play a role in energy expenditure (20–31). The prevailing belief is that the obesity epidemic has arisen from environmental and behavioral factors (1, 2, 7, 15, 16, 22, 32–34). The association of obesity with various occupations (eg, housekeeping, service, motor vehicle operation, nursing) and exposures (sedentary work, work stress, contingent work, low physical job demands, chemicals) suggest it is important as both a risk factor and adverse health outcome in the occupational environment, but as part of a complex matrix of variables (15, 21, 32, 35–39).
Schulte and colleagues’ (38, 40) description of the relationship between occupational hazards and obesity stimulated this paper. Integrated evaluation of occupational and non-occupational factors related to obesity and the workplace have health and economic implications for workers and employers (41). For example, some analyses have found obesity to be associated with higher numbers of worker compensation claims (42). Conceptual models examining combined impacts of occupational risk factors (ORF) and personal risk factors (PRF) can be used to address the multiple factors of relevance to obesity in the workplace setting and understand risks for adverse outcomes (43). As we have noted previously, such models function to classify known or theorized relationships, will require future investigation and validation, and indicate potential avenues for basic research and subsequent design of interventions (40). Understanding risk is important for developing and targeting prevention and intervention strategies (44–47); in essence, it is a risk management strategy to prevent adverse health outcomes. Risk management for primary prevention could include workers in sedentary occupations using sit-stand workstations to increase non-exercise activity thermogenesis (caloric expenditure associated with non-exercise movement), which may have a role in obesity prevention (33, 48–50). Management of risk for tertiary prevention might focus on return-to-work protocols after injury (51). The US National Research Council (NRC) emphasizes assessing risk for chemical and non-chemical hazards for risk-management (52). A comprehensive approach to understanding combined ORF and PRF effects could strengthen risk management at all prevention levels to promote workforce health, greater productivity, and population well-being (52–56). This discussion paper focuses on basic conceptual heuristic models that consider combinations of risk factors related to obesity and the occupational environment.
Evaluating obesity and occupational health issues in a comprehensive approach
In our conceptual model approach (43), models describing combinations of ORF, PRF, and adverse outcomes among working populations are not meant to conclusively delineate specific molecular/cellular/organ/system-level causal pathways, etiologic steps, epidemiological mechanisms, or statistical relationships with respect to the illnesses or injuries discussed. Rather, these models were developed as heuristic frameworks to consider PRF and ORF and health and safety outcomes.
PubMed was searched since 2000 for English language primary studies, journal articles, meta-analyses, and reviews. Reviews were included since conceptual models are presented as a developmental exercise to stimulate hypothesis generation for research, risk assessment, and intervention design. The first search used the terms obesity, occupational health, and specific workplace exposures and health outcomes identified from recent reviews as being important for obesity (7, 8). The second search involved combining the results for these terms and yielded 1245 publications that were the basis for targeted searches (eg, genetics, interventions).
Four models describe obesity as a PRF in an occupational setting (figure 1). In model 1, obesity as a PRF present with an ORF are independent of each other with respect to their impact health outcomes. In models 2, 3, and 4, obesity and an ORF can have combined impacts on outcomes. In models 2 and 3, obesity and an ORF could alternately impact the effect of the other variable on outcomes. In model 4, obesity and an ORF could impact different adverse health processes that are associated with each other.
Figure 1.
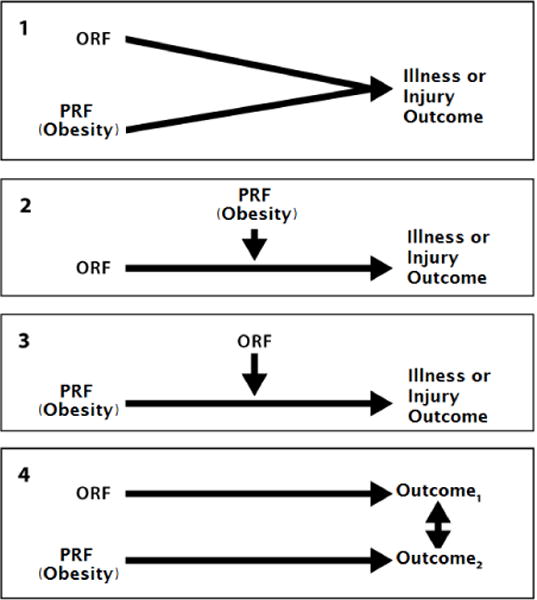
Conceptual models to delineate the combined impact on outcomes of obesity as a personal risk factor (PRF) with an occupational risk ractor (ORF). Adapted from a figure originally published in Schulte et al (43).
Five models describe obesity as an adverse health outcome (figure 2). In model 1, the PRF and ORF independently impact obesity. In models 2, 3, and 4, a PRF and ORF can have combined impacts. In models 2 and 3, the PRF and ORF alternately impact the effect of the other variable on obesity. In models 4 and 5, the ORF, or alternatively PRF, impacts obesity, in a context where more complex associations are present. For all models, the use of one versus another, or a more complex model, can change as scientific information evolves. More complex models could exist for the examples presented and potentially more complex situations are noted where appropriate.
Figure 2.
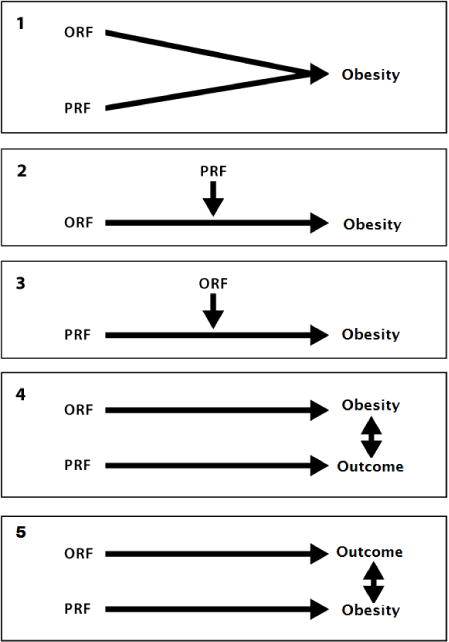
Conceptual models to delineate the combined impact on obesity of a personal risk factor (PRF) and an occupational risk factor (ORF). Adapted from a figure originally published in Schulte et al (43).
Risk factors related to obesity and the occupational environment: Obesity as a personal risk factor
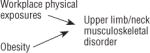
Obesity may increase the risk for various outcomes. Table 1 illustrates four examples where obesity and an ORF impact health outcomes. They are illustrative rather than exhaustive in depicting the complexity of the inter-relationships involved. The examples in this section and table 1 extend examples originally provided by Schulte et al (43).
Table 1.
Examples of the impact on illness and/or injury of the combination of obesity as a personal risk factor and various occupational risk factors (ORF). Adapted from a figure originally published in Schulte et al (43).
| Conceptual model | Selected references | |
|---|---|---|
| 1.1 Obesity and an ORF independently impact an occupational illness or injury |
|
63–68 |
| 1.2 Obesity impacts an ORF–occupational illness or injury association |
|
61, 69, 70, 73 |
| 1.3 An ORF impacts an obesity–occupational illness or injury association |
|
78, 81–83, 84 |
| 1.4 Obesity impacts one outcome, an ORF impacts another, and the two outcomes can be associated with each other |
|
85, 87–90 |
Example 1.1: Obesity, occupational physical factors, and MSD
The relationship of obesity to MSD is complex (57, 58). For instance, obesity and ineffective job-task training are considered independent risk factors for carpal tunnel syndrome (59, 60). Mechanical loading is considered an etiologic factor in MSD, particularly for concomitant osteoarthritis and obesity; other predisposing factors include joint injury, heredity, and aging (61, 62). In addition to biomechanical factors, studies of animal MSD models suggest multiple biochemical and molecular mechanisms that may interact with obesity to influence MSD development (61).
A systematic review of 21 longitudinal studies demonstrated that workplace physical factors are part of a cause–effect chain for upper-limb/neck MSD (63). These factors include manual material handling, vibration, trunk flexion/rotation, and working with hands above shoulder level. Linking obesity with complex outcomes such as MSD is challenging. For example, a Cochrane review has shown that upper-limb/neck MSD may not be a single entity (64), subgroups of which may have a different relationship to obesity and require different approaches to prevention and intervention.
Some cross-sectional (65, 66, 67) and longitudinal (68) studies have evaluated obesity and the development of MSD symptoms in working populations, but more studies are needed, particularly with more rigorous ascertainment of MSD triggering factors and symptoms. For example, the longitudinal study found associations between incident self-report shoulder pain, in the week prior to survey, and age, BMI, workplace physical factors, and psychosocial factors among workers at baseline and at three years (68). Extended work schedules (eg, shift work, long hours) were an independent risk factor for MSD among nurses (67), but work schedules are also considered an important occupational risk factor for obesity (see example 2.4). Taken together, this breadth of data examining different risk factors or outcomes in animal models as well as cross-sectional and longitudinal studies suggests the importance of considering the impact of obesity and occupational factors on MSD. One such conceptual model could focus on the impact of obesity and workplace physical factors on upper-limb/neck MSD (table 1, example 1.1).
Example 1.2: Obesity, occupational kneeling/squatting, and osteoarthritis
The association of knee osteoarthritis with occupational kneeling and squatting has been shown to increase 7-fold between the lowest and highest categories of BMI (69, 70). The impact of heavy workload, obesity, and traumatic knee injuries on the development of osteoarthritis have been reported from a prospective study of a Finnish cohort with ≥20 years of follow-up (71). The combined impact of kneeling/squatting activities and obesity may also be important for the progression of existing knee osteoarthritis symptoms (72–74). Cross-sectional and longitudinal studies of obesity and occupational risk factors for osteoarthritis in working populations support the importance of a conceptual model of obesity, occupational kneeling/squatting, and osteoarthritis. Animal data suggest that the physiologic impact of obesity on osteoarthritis (61) may be of relevance (table 1, example 1.2).
Example 1.3: Obesity, occupational allergens, and asthma
Obesity increases the risk for asthma and is associated with greater asthma-related healthcare utilization and reduced quality of life (75). Obesity is associated with decreased sensitivity to glucocorticoids, a mainstay of asthma treatment (10, 75, 76). Occupational allergens such as chemicals, dusts, fumes, or other compounds can increase the risk of asthma onset or its exacerbation (77–83). An earlier peer review concluded that controlling obesity and occupational exposures are among the best opportunities for asthma prevention (84). The literature on the relationship of occupational allergens and obesity, respectively, to asthma is long-standing and robust. Thus, an important conceptual model is the impact of occupational exposures on the relationship between obesity and asthma (table 1, example 1.3).
Example 1.4: Obesity, sleep apnea, and non-alcoholic fatty liver disease (NAFLD)
Obesity increases the risk for hypertension through salt retention, insulin resistance, dyslipidemias, sympathetic nervous system activation, systemic inflammation, and risk of sleep apnea (8). Increased risk for sleep apnea stems from the impact of elevated blood pressure and constraints on the pulmonary system from increased BMI (85, 86). NAFLD has been associated with exposures to chemicals such as organic compounds or metals in cross-sectional analysis of population data (87, 88) and among workers with or without metabolic disease (89). The association of sleep apnea with NAFLD is gaining support (90) and the association of obesity with NAFLD is becoming a greater concern given the obesity epidemic (91). Although much of the data is cross-sectional or observational, the situation raises enough concern to suggest a conceptual model in which the combined presence of obesity and an occupational chemical exposure could impact the effects of sleep apnea on NAFLD (table 1, example 1.4). This example illustrates the potential for a disease process due to obesity, along with exposure to chemicals, to be relevant in the occupational setting. Additionally, it raises the issue of more complex associations in the context of occupational exposure to chemicals that may impact NAFLD status because of the role of obesity in both sleep apnea and NAFLD. This emphasizes the need to consider multiple disease processes based on occupational and personal risk factors for evaluating the impact of obesity and the work environment.
Risk factors related to obesity and the occupational environment: Obesity as an adverse health outcome
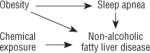
Strong evidence supports the role of genetics, family history, age, diet, physical activity, medications, and environmental factors as risk factors for obesity (2, 7, 8). Understanding the impact of ORF and PRF is important for obesity as an adverse health outcome in and of itself in the work environment. The conceptual models of ORF and PRF impacting obesity (table 2) are illustrative rather than exhaustive in depicting the complexity of the inter-relationships involved.
Table 2.
Examples of the impact of the combination of occupational risk factors (ORF) and personal risk factors (PRF) on obesity.
| Conceptual model | Selected references | |
|---|---|---|
| 2.1 An ORF and a PRF independently impact obesity |

|
19, 92, 93, 103 |
| 2.2 A PRF impacts an ORF–obesity association |
|
109, 110 |
| 2.3 An ORF impacts a PRF–obesity association |
|
16, 19, 67 92, 93, 98, 111–113 |
| 2.4 An ORF impacts obesity; a PRF impacts another outcome; obesity and that health outcome can be associated |
|
34, 67, 111, 114, 116, 118, 120, 121, 125, 126, 128, 129 |
| 2.5 A PRF impacts obesity; an ORF impacts another outcome; obesity and that health outcome can be associated |
|
34, 129–133 |
Example 2.1: Sitting/sedentary work, age, and obesity
One of the most significant modifiable variables affecting obesity is physical activity (7). Recent analysis of 3539 adults from 1999–2004 National Health and Nutrition Examination Survey (NHANES) data found that having high versus low occupational activity decreased the odds risk ratio to 0.37 [95% confidence interval (95% CI) 0.24–0.57] for abdominal obesity (92). Cross-sectional analysis of 10 785 workers from the Australian National Health Survey found that mostly standing at work, versus mostly sitting, lowered the risk for overweight/obesity to 0.88 (95% CI 0.82–0.95); physical activity and leisure-time sitting did not impact this association (93). Although cross-sectional, this evidence suggests that occupational activity levels influence obesity. A meta-analysis of 15 prospective studies suggests that “light” physical activity, or even standing instead of sitting during leisure time, may decrease the risk of obesity-associated diseases, particularly diabetes, with reported associations predominantly independent of overall physical activity (94). Such evidence supports the idea that sedentary behavior and physical activity are separate behaviors. Current thinking suggests that degree of activity may be influenced by environment and genetics (49, 95–97). Studies have found that animals can be bred to be “obesity resistant” demonstrating more spontaneous physical activity (96), and certain genes, such as the brain-specific Bsx or “fidget” gene, may impact spontaneous physical activity (97), although these findings have not been confirmed among humans. A recent examination of the impact of sedentary behavior (hours of TV watching) on the BMI of individuals with a genetic predisposition for obesity (32 well-established BMI-associated genetic variants) found that prolonged sedentary activity exacerbated genetic effects, but increased physical activity independently weakened this genetic association (98). Extended periods of inactivity among both animals and humans cause physiologic and metabolic changes, suggesting that consideration of sedentary behaviors and physical activity may be needed for interventions in the occupational setting (94, 99, 100, 101). If an individual, with a genetic predisposition for low levels of physical activity, is employed in a sedentary profession, then these factors may independently engender obesity or may interact to produce greater weight gain. From the PRF perspective, decreases in exercise levels are considered a significant factor for obesity increasing with age (102). Metabolism, hormone function, body fat distribution patterns, and other biochemical and physiologic processes also change with age, often creating a setting fostering obesity (103). A conceptual model concerning the impact of occupational activity/sitting/sedentary work and age on obesity may be important for consideration in the occupational environment (table 2, example 2.1).
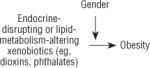
Example 2.2: Chemicals with endocrine-disrupting or lipid-metabolism-altering properties and obesity
The association of obesity with occupational exposure to endocrine-disrupting chemicals is supported by evidence from animal models as well as observational and case–control studies. Fat-soluble xenobiotics, such as benzo(a)pyrene (104) and polybrominated diphenyl esters (105), deposit in adipose tissue and have been shown to affect lipolysis and thyroid function in rodents. A complex causal relationship between polychlorinated biphenyls and obesity has been theorized with varying impact of factors, such as degree of chlorination, and time course of exposure as well as gender, in analyses of US and Swedish cohorts (37). Obesogens, chemicals suspected to be causally related to obesity, also have been proposed to include phthalates, dithiocarbamates, aryl hydrocarbon receptor ligands, and organotins, despite normal diet and exercise activities (37, 106–110). A recent cross-sectional analysis of men and women participating in a prospective cohort study in the Netherlands provided evidence that occupational exposure to endocrine disruptors in either gender was associated with an increased time to pregnancy (109). Recently, a case–control study of 1005 breast cancer cases and 1146 community controls in Canada demonstrated increased exposure to carcinogens and endocrine disrupters in a range of occupations, including agriculture and automotive plastics manufacturing (110). An important conceptual model focuses on gender differences in the impact of various endocrine disruptors on obesity (table 2, example 2.2).
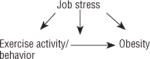
Example 2.3: Job stress, exercise activity/behavior, and obesity
Job stress has been linked to BMI (19, 38, 111). A recent cross-sectional analysis across 13 European studies, with a total of 161 746 participants, found both weight gain and loss to be modestly associated with job strain (16). Job strain may be associated with type 2 diabetes through BMI and gender dependent mechanisms (112) and kidney dysfunction in a BMI dependent manner (113). Personal exercise behavior/activity impacts obesity and type 2 diabetes (15, 92, 93, 98). Although mostly cross-sectional, the association of job stress or strain with obesity supports an important conceptual model involving exercise behavior/activity, job stress or strain, and obesity, with several inter-relationships possible (table 2, example 2.3).
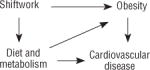
Example 2.4: Shift work, diet and metabolism, cardiovascular disease, and obesity
Shift workers have increased body weight, and working long hours has been positively associated with higher BMI (38, 111, 114). Shift work, sleep deprivation, and exposure to bright light at night have been associated with increased adiposity (115). Cross-sectional studies suggest that disrupting normal eating and sleeping patterns through night shift work or rapidly rotating day/night shifts are risks for obesity and metabolic syndrome (116). Cyclic, clock-like expression of “clock genes,” in central and peripheral tissue neurons, liver, and fat cells, with expression in rhythmic patterns synced to external environments, impacts food intake, energy expenditure, and sleep (117). In animal models of activity during normal sleep times or of fragmented sleep periods, disruption of this mechanism is associated with energy metabolism malfunction, development of obesity, and disrupted glucose utilization (118–121). Shift work and circadian disruption has also been associated with changes in gastrointestinal and metabolic processes such as fat absorption and metabolism, melatonin-related lipid metabolism, enteric autonomic function, and altered insulin signaling in human subcutaneous fat (121–125). Shift work also disrupts workers’ eating behaviors such as those related to food choice and availability as well as eating times and habits (67, 126). Recent studies have found, however, that disrupting only the fat cell clock gene Arntl caused mice to eat during their inactive phase, a type of “night eating syndrome”, and engendered obesity with no changes in activity or other behaviors. As the circadian clock was disrupted in only fat cells, these data suggest a strong communication network between fat stores and the brain (127, 128). Diet and metabolism impact obesity and CVD such as hypertension, with high calorie/high fat intake, metabolism, and high salt ingestion/retention playing differential and important roles (2, 7, 129). Animal data and observational studies in humans provide evidence on the effects of shift work/long work hours on obesity, and review the information on the role of diet and metabolism in obesity and CVD. This information strongly suggests the importance of a conceptual model that considers both physiologic and behavioral perspectives regarding the impact of shift work and diet/metabolism on obesity, with both factors significantly increasing the risk for CVD (table 2, example 2.4). This model also illustrates complexities that can arise when risk factors impact each other.
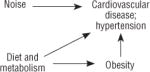
Example 2.5: Occupational noise exposure, CVD, diet and metabolism, and obesity
Analysis of the 1999–2004 NHANES data showed that chronic occupational noise exposure, compared with no exposure, resulted in 2–3 times greater prevalence of CVD, such as hypertension (130). Other findings strongly support the theory that noise exposure has an impact on hypertension, and some data suggest that hearing loss and hypertension severity is associated (131–133). As such, this cross-sectional data supports the need for further evaluation of noise and CVD. Given the relationship of diet, metabolism, obesity, and CVD (see example 2.4) a conceptual model that may be important to consider is occupational noise exposure, diet/metabolism, obesity, and CVD, providing the potential to examine more complex relationships (table 2, example 2.5).
Combinations of risk factors and special issues
The conceptual, heuristic models in tables 1 and 2 are starting points for describing the combined impacts of personal and occupational risk factors relevant to obesity and the workplace. The involvement of multiple mechanisms for a given ORF/PRF/adverse outcome combination is illustrated by examples 1.2, 1.3, 1.4, 2.3, 2.4, and 2.5. Improved understanding of these complex relationships can inform hazard definition and exposure assessment as well as drive risk assessment and management strategy development to address obesity in the occupational environment.
Defining a factor as a modifying or mediating variable can improve understanding of disease mechanisms or relevant interventions (134). Such definitions can impact the design and analysis of research studies, the conduct of risk assessment to set exposure limits, and the development and application of prevention or intervention strategies for behavioral factors such as physical activity or diet. In table 3, we revisit classic descriptions of modifying or mediating variables (134) with relevance to research, risk assessment, and prevention/intervention strategies (52). Primary, secondary, and tertiary prevention and risk management may require targeting different or multiple risk factors for optimal effect. Ultimately, in addition to assessing relative risk for these endeavors, it may also be necessary to consider attributable risk.
Table 3.
Modifying and mediating variables for research, risk assessment, and prevention or intervention strategies
| Variable type | Context | ||
|---|---|---|---|
| Research | Quantitative/qualitative risk assessment | Prevention or intervention strategies | |
| Modifying | Variables that can affect the exposure–outcome relationship | Variables to consider when assessing sensitive or other sub- populations (eg, smokers, older workers etc) | Variables that may need to be considered along with main targets for prevention or intervention strategies |
| Mediating | Variables in the causal pathway from exposure to outcome | Variables that may become the basis (ie, early effect marker) for exposure limits | Variables that may be important by themselves for prevention or intervention strategies |
Future considerations
Obesity in the occupational setting can be a personal risk factor or an adverse health outcome. This distinction affects hazard definition, exposure assessment, risk assessment, and risk management. Evaluating issues related to obesity and the workplace using a combined approach could better inform workplace intervention/prevention activities. More research is needed in this regard. For example, defining obesity and workplace physical factors as combined risks for MSD might focus prevention strategies on weight management and occupational tasks. Preventive efforts might also need to target primary versus secondary/tertiary prevention for return-to-work after an MSD differentially. Obesity defined as an adverse health outcome due to exposure to endocrine disruptors, however, might require interventions with improved exposure controls and weight management, with obesity monitoring to measure outcome status. These occupational considerations, of course, support giving greater attention to broader issues of diet, nutrition, and lifestyle in general society.
Targeted intervention/prevention strategies in the occupational setting, such as weight-reduction programs or diet consultations, are evolving; several reviews and interventional studies are currently examining this issue (135–137). Workplace interventions for obesity will likely be effective (38), but systematic evaluation of interventions is sorely needed (136). For example, Sorensen and Barbeau (138) have shown that addressing ORF and PRF together can reduce smoking, but the utility of such approaches for obesity requires investigation. Defining obesity as a personal risk factor or an adverse health outcome, and identifying and examining the combined impact of factors, with risk assessment and management of combined exposures, may lead to improved primary, secondary, and tertiary prevention for issues of obesity in the occupational setting.
Acknowledgments
The authors thank Drs Kaori Fujishiro, Dexter Kimsey, Liping Pan, Shirley Pospisil, and Gregory Wagner for their comments on drafts of this manuscript. We thank Robert Park for discussions of key points, particularly table 3, Cathy Rotunda and Seleen Collins for manuscript preparation assistance, and Devin Baker and Vanessa Wil-liams for formatting work for tables 1 and 2.
Footnotes
The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the US National Institute for Occupational Safety and Health.
References
- 1.WHO (World Health Organization) Obesity and Overweight. [cited 2012 September 12] Paris: WHO; 2013. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/ [Google Scholar]
- 2.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–7. doi: 10.1001/jama.2012.39. http://dx.doi.org/10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 3.Cheung WW, Mao P. Recent advances in obesity: Genetics and beyond. ISRN Endocrinol. 2012;2012:536905. doi: 10.5402/2012/536905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schug TT, Janesick A, Blumberg B, Heindel JJ. Endocrine disrupting chemicals and disease susceptibility. J Steroid Biochem Mol Biol. 2011;127(3–5):204–15. doi: 10.1016/j.jsbmb.2011.08.007. http://dx.doi.org/10.1016/j.jsbmb.2011.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804–14. doi: 10.1016/S0140-6736(11)60813-1. http://dx.doi.org/10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 6.Finkelstein EA, Fiebelkorn IC, Wang G. State-Level Estimates of Annual Medical Expenditures Attributable to Obesity. Obesity Research. 2004;12(1):18–24. doi: 10.1038/oby.2004.4. http://dx.doi.org/10.1038/oby.2004.4. [DOI] [PubMed] [Google Scholar]
- 7.CDC (Centers for Disease Control and Prevention) Overweight and Obesity – Causes and Consequences. [cited 2012 October 15] Georgia, USA: CDC; 2012. Available from: http://www.cdc.gov/obesity/adult/causes/index.html. [Google Scholar]
- 8.Robert Wood Johnson Foundation F as in Fat: How Obesity Threatens America’s Future. Robert Wood Johnson Foundation. [cited 2012 November 19] New Jersey, USA: RWJF; 2012. Available from: http://www.rwjf.org/en/research-publications/find-rwjf-research/2012/09/f-as-in-fat–how-obesity-threatens-america-s-future-2012.html. [Google Scholar]
- 9.Woolf AD, Vos T, March L. How to measure the impact of musculoskeletal conditions. Best Pract Res Clin Rheumatol. 2010;24(6):723–32. doi: 10.1016/j.berh.2010.11.002. http://dx.doi.org/10.1016/j.berh.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Zammit C, Liddicoat H, Moosnie I, Makker H. Obesity and Respiratory Diseases. Int J Gen Med. 2010;3:335–43. doi: 10.2147/IJGM.S11926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elobeid MA, Brock DW, Allison DB, Padilla MA, Ruden DM. Endocrine Disruptors and Obesity: An Examination of Selected Persistent Organic Pollutants in the NHANES 1999–2002 Data. Int J Environ Res Public Health. 2010 Jul;7(7):2988–3005. doi: 10.3390/ijerph7072988. http://dx.doi.org/10.3390/ijerph7072988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim MJ, Pelloux V, Guyot E, Tordjman J, Bui L-C, Chevallier A, et al. Inflammatory Pathway Genes Belong to Major Targets of Persistent Organic Pollutants in Adipose Cells. Environ Health Perspect. 2012;120:508–14. doi: 10.1289/ehp.1104282. http://dx.doi.org/10.1289/ehp.1104282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One. 2011;6(5):e19657. doi: 10.1371/journal.pone.0019657. http://dx.doi.org/10.1371/journal.pone.0019657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Capodaglio P, Castelnuovo G, Brunani A, Vismara L, Villa V, Capodaglio EM. Functional limitations and occupational issues in obesity: a review. Int J Occup Saf Ergon. 2010;16(4):507–23. doi: 10.1080/10803548.2010.11076863. [DOI] [PubMed] [Google Scholar]
- 15.Choi B, Schnall PL, Yang H, Dobson M, Landsbergis P, Israel L, et al. Sedentary work, low physical job demand, and obesity in US workers. Am J Ind Med. 2010;53(11):1088–101. doi: 10.1002/ajim.20886. http://dx.doi.org/10.1002/ajim.20886. [DOI] [PubMed] [Google Scholar]
- 16.Nyberg ST, Heikkilä K, Fransson EI, Alfredsson L, De Bacquer D, Bjorner JB, et al. IPD-Work Consortium Job strain in relation to body mass index: pooled analysis of 160 000 adults from 13 cohort studies. J Intern Med. 2012;272(1):65–73. doi: 10.1111/j.1365-2796.2011.02482.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robroek SJW, van den Berg TIJ, Plat JF, Burdorf A. The role of obesity and lifestyle behaviors in a productive workforce. Occup Environ Med. 2011;68:134–9. doi: 10.1136/oem.2010.055962. http://dx.doi.org/10.1136/oem.2010.055962. [DOI] [PubMed] [Google Scholar]
- 18.Grosch JW, Caruso CC, Rosa RR, Sauter SL. Long hours of work in the U.S.: associations with demographic and organizational characteristics, psychosocial working conditions, and health. Am J Ind Med. 2006;49(11):943–52. doi: 10.1002/ajim.20388. http://dx.doi.org/10.1002/ajim.20388. [DOI] [PubMed] [Google Scholar]
- 19.Brisson C, Larocque B, Moisan J, Vézina M, Dagenais GR. Psychosocial factors at work, smoking, sedentary behavior, and body mass index: a prevalence study among 6995 white collar workers. J Occup Environ Med. 2000;42(1):40–6. doi: 10.1097/00043764-200001000-00011. http://dx.doi.org/10.1097/00043764-200001000-00011. [DOI] [PubMed] [Google Scholar]
- 20.Parks BW, Nam E, Org E, Kostem E, Norheim F, Hui ST, et al. Genetic control of obesity and gut microbiota composition in response to high-fat, high-sucrose diet in mice. Cell Metab. 2013 Jan 8;17(1):141–52. doi: 10.1016/j.cmet.2012.12.007. http://dx.doi.org/10.1016/j.cmet.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Champagne N, Abreu M, Nobrega S, et al. Obesity/overweight and the role of working conditions: A qualitative, participatory investigation. Study Report – UMass Lowell, MassCOSH, Boston Worker’s Alliance; 2012. pp. 1–30. [Google Scholar]
- 22.CDC (Centers for Disease Control and Prevention) Overweight and Obesity: Adult Obesity Facts. [cited 2013 January 10] Georgia, USA: CDC; 2012. Available from: http://www.cdc.gov/obesity/data/adult.html. [Google Scholar]
- 23.Schiller J, Lucas J, Ward B, et al. Summary health statistics for U.S. adults: National Health Interview Survey. (Series 10, Data from The National Health Survey).Vital and Health Statistics. 2012;252:1–207. [PubMed] [Google Scholar]
- 24.Caban AJ, Lee DJ, Fleming LE, et al. Obesity in US workers: The National Health Interview Survey, 1986 to 2002. Amer J Pub Health. 2005;95:1614–22. doi: 10.2105/AJPH.2004.050112. http://dx.doi.org/10.2105/AJPH.2004.050112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hjelmborg JVB, Fagnani C, Silventoinen K, et al. Genetic influences on growth traits of BMI: a longitudinal study of adult twins. Obesity. 2008;16(4):847–52. doi: 10.1038/oby.2007.135. http://dx.doi.org/10.1038/oby.2007.135. [DOI] [PubMed] [Google Scholar]
- 26.Rankinen T, Zuberi A, Chagnon YC, Weisnagel SJ, Argyropoulos G, Walts B, et al. The human obesity gene map: the 2005 update. Obesity. 2006;14(4):529–44. doi: 10.1038/oby.2006.71. http://dx.doi.org/10.1038/oby.2006.71. [DOI] [PubMed] [Google Scholar]
- 27.McMurray F, Church CD, Larder R, McMurray F, Church CD, Larder R, Nicholson G, Wells S, Teboul L, et al. Adult onset global loss of the FTO gene alters body composition and metabolism in the mouse. PLOS Genetics. 2013;9(1):e1003166. doi: 10.1371/journal.pgen.1003166. http://dx.doi.org/10.1371/journal.pgen.1003166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fall T, Ingelsson E. Genome-wide association studies of obesity and metabolic syndrome. Mol Cell Endocrinol. 2012 Sep 3; doi: 10.1016/j.mce.2012.08.018. [Epub ahead of print] http://dx.doi.org/10.1016/j.mce.2012.08.018. [DOI] [PubMed]
- 29.Fawcett KA, Barroso I. The genetics of obesity:FTO leads the way. Trends in Genetics. 2010;26(6):266–74. doi: 10.1016/j.tig.2010.02.006. http://dx.doi.org/10.1016/j.tig.2010.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pausova Z, Syme C, Abrahamowicz, Xiao Y, Leonard GT, Perron M, et al. A common variant of the FTO gene is associated with not only increased adiposity but also elevated blood pressure in French Canadians. Circ Cardiovasc Genet. 2009;2:260–69. doi: 10.1161/CIRCGENETICS.109.857359. http://dx.doi.org/10.1161/CIRCGENETICS.109.857359. [DOI] [PubMed] [Google Scholar]
- 31.Morton GJ, Cummings DE, Baskin DG, Barsh GS, Schwartz MW. Central nervous system control of food intake and body weight. Nature. 2006;443(7109):289–95. doi: 10.1038/nature05026. http://dx.doi.org/10.1038/nature05026. [DOI] [PubMed] [Google Scholar]
- 32.Escoto KH, French SA, Harnack LJ, Toomey TL, Hannan PJ, Mitchell NR. Work hours, weight status, and weight-related behaviors: A study of metro transit workers. Int J Behav Nutr Phys Act. 2010 Dec 20;7:91. doi: 10.1186/1479-5868-7-91. http://dx.doi.org/10.1186/1479-5868-7-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Levine JA. Nonexercise activity thermogenesis – liberating the life-force. J Int Med. 2007;262:273–87. doi: 10.1111/j.1365-2796.2007.01842.x. http://dx.doi.org/10.1111/j.1365-2796.2007.01842.x. [DOI] [PubMed] [Google Scholar]
- 34.US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th. Washington DC: U.S. Government Printing Office; 2010. [cited 2013 April 4]. Available from: http://www.health.gov/dietaryguidelines/dga2010/DietaryGuidelines2010.pdf. [Google Scholar]
- 35.Buss J. Associations between obesity and stress and shift work among nurses. Workplace Health Saf. 2012 Oct;60(10):453–8. doi: 10.1177/216507991206001007. http://dx.doi.org/10.3928/21650799-20120926-66. [DOI] [PubMed] [Google Scholar]
- 36.Han K, Trinkoff AM, Storr CL, Geiger-Brown J, Johnson KL, Park S. Comparison of job stress and obesity in nurses with favorable and unfavorable work schedules. JOEM. 2012;54(8):928–32. doi: 10.1097/JOM.0b013e31825b1bfc. [DOI] [PubMed] [Google Scholar]
- 37.Lind L, Lind PM. Can persistent organic pollutants and plastic-associated chemicals cause cardiovascular disease? J Intern Med. 2012;271(6):537–53. doi: 10.1111/j.1365-2796.2012.02536.x. http://dx.doi.org/10.1111/j.1365-2796.2012.02536.x. [DOI] [PubMed] [Google Scholar]
- 38.Schulte PA, Wagner GR, Ostry A, Blanciforti LA, Cutlip RG, Krajnak KM, et al. Work, obesity, and occupational safety and health. Am J Public Health. 2007;97(3):428–36. doi: 10.2105/AJPH.2006.086900. http://dx.doi.org/10.2105/AJPH.2006.086900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cummings KJ, Kreiss K. Contingent workers and contingent health-risks of a modern economy. JAMA. 2004;299:448–50. doi: 10.1001/jama.299.4.448. http://dx.doi.org/10.1001/jama.299.4.448. [DOI] [PubMed] [Google Scholar]
- 40.Schulte PA, Wagner GR, Downes A, Miller DB. A framework for the concurrent consideration of occupational hazards and obesity. Ann Occup Hyg. 2008;52(7):555–66. doi: 10.1093/annhyg/men055. http://dx.doi.org/10.1093/annhyg/men055. [DOI] [PubMed] [Google Scholar]
- 41.Seabury SA, Lakdawalla D, Reville RT. Research Compendium: The NIOSH Total Worker Health Program Seminal Research Papers 2012. 2005. The Economics of Integrating Injury and Illness Prevention and Health Promotion Programs; pp. 185–213. (DHHS (NIOSH) Publication No. 2012-146). [Google Scholar]
- 42.Ostbye T, Dement JM, Krause KM. Obesity and Workers’ Compensation: Results from the Duke Health and Safety Surveillance System. Arch Intern Med. 2007;167:766–73. doi: 10.1001/archinte.167.8.766. http://dx.doi.org/10.1001/archinte.167.8.766. [DOI] [PubMed] [Google Scholar]
- 43.Schulte PA, Pandalai SP, Wulsin V, Chun HK. Interaction of Occupational and Personal Risk Factors in Workforce Health and Safety. Am J Pub Health. 2012;102(3):434–48. doi: 10.2105/AJPH.2011.300249. http://dx.doi.org/10.2105/AJPH.2011.300249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee R, Kean WF. Obesity and Knee Osteoarthritis. Immunopharmacol. 2012;20:53–8. doi: 10.1007/s10787-011-0118-0. [DOI] [PubMed] [Google Scholar]
- 45.Toth PP. Effective Management of the Type 2 Diabetes Patient with Cardiovascular and Renal Disease: Secondary Prevention Strategies after a Myocardial Infarction. Current Diabetes Reviews. 2012;8:219–28. doi: 10.2174/157339912800564043. http://dx.doi.org/10.2174/157339912800564043. [DOI] [PubMed] [Google Scholar]
- 46.Gibson M, Carek PJ, Sullivan B. Treatment of Comorbid Mental Illness in Primary Care: How to Minimize Weight Gain, Diabetes, and Metabolic Syndrome. Int J Psych Med. 2011;41(2):127–42. doi: 10.2190/PM.41.2.c. http://dx.doi.org/10.2190/PM.41.2.c. [DOI] [PubMed] [Google Scholar]
- 47.Rector RS, Thyfault JP. Does physical inactivity cause nonalcoholic fatty liver disease? J Appl Physiol. 2011;111(6):1828–35. doi: 10.1152/japplphysiol.00384.2011. http://dx.doi.org/10.1152/japplphysiol.00384.2011. [DOI] [PubMed] [Google Scholar]
- 48.Levine JA. Scalable obesity solutions (S.O.S.) J Physical Act Health. 2010;7(Suppl 3):S307–S312. doi: 10.1123/jpah.7.s3.s307. [DOI] [PubMed] [Google Scholar]
- 49.Levine JA, Lanningham-Foster LM, McCrady SK, et al. Interindividual variation in posture allocation: Possible role in human obesity. Science. 2005;307:584–86. doi: 10.1126/science.1106561. http://dx.doi.org/10.1126/science.1106561. [DOI] [PubMed] [Google Scholar]
- 50.Levine JA, Vander Weg MW, Hill JO, et al. Non-exercise activity thermogenesis – The crouching tiger hidden dragon of societal weight gain. Arterioscler Thromb Vasc Biol. 2006;26:729–36. doi: 10.1161/01.ATV.0000205848.83210.73. http://dx.doi.org/10.1161/01.ATV.0000205848.83210.73. [DOI] [PubMed] [Google Scholar]
- 51.Lilley R, Davie G, Ameratunga S, Derrett S. Factors predicting work status 3 months after injury: results from the Prospective Outcomes of Injury Study. BMJ Open. 2012;2(2):e000400. doi: 10.1136/bmjopen-2011-000400. http://dx.doi.org/10.1136/bmjopen-2011-000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.NRC (The National Research Council of the National Academies) Science and Decisions – Advancing Risk Assessment. Washington DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 53.Kawada T. Predictors of the development of metabolic syndrome in male workers: a 3-year follow-up study. J Occup Environ Med. 2012;54(3):292–5. doi: 10.1097/JOM.0b013e3182492070. http://dx.doi.org/10.1097/JOM.0b013e3182492070. [DOI] [PubMed] [Google Scholar]
- 54.Belenky G, Wu LJ, Jackson ML. Occupational sleep medicine: practice and promise. Prog Brain Res. 2011;190:189–203. doi: 10.1016/B978-0-444-53817-8.00012-8. http://dx.doi.org/10.1016/B978-0-444-53817-8.00012-8. [DOI] [PubMed] [Google Scholar]
- 55.Esquirol Y, Perret B, Ruidavets JB, Marquie JC, Dienne E, Niezborala M, et al. Shift work and cardiovascular risk factors: new knowledge from the past decade. Arch Cardiovasc Dis. 2011;104(12):636–68. doi: 10.1016/j.acvd.2011.09.004. http://dx.doi.org/10.1016/j.acvd.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 56.Soteriades ES, Smith DL, Tsismenakis AJ, Baur DM, Kales SN. Cardiovascular disease in US firefighters: a systematic review. Cardiol Rev. 2011;19(4):202–15. doi: 10.1097/CRD.0b013e318215c105. http://dx.doi.org/10.1097/CRD.0b013e318215c105. [DOI] [PubMed] [Google Scholar]
- 57.Kortt M, Baldry J. The association between musculoskeletal disorders and obesity. Aust Health Rev. 2002;25(6):207–14. doi: 10.1071/ah020207. http://dx.doi.org/10.1071/AH020207. [DOI] [PubMed] [Google Scholar]
- 58.Pollack KM, Cheskin LJ. Obesity and workplace traumatic injury: does the science support the link? Inj Prev. 2007 Oct;13(5):297–302. doi: 10.1136/ip.2006.014787. http://dx.doi.org/10.1136/ip.2006.014787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Moghtaderi A, Izadi S, Sharafadinzadeh N. An evaluation of gender, body mass index, wrist circumference and wrist ratio as independent risk factors for carpel tunnel syndrome. Acta Neurol Scand. 2005;112:375–9. doi: 10.1111/j.1600-0404.2005.00528.x. http://dx.doi.org/10.1111/j.1600-0404.2005.00528.x. [DOI] [PubMed] [Google Scholar]
- 60.Lam N, Thurston A. Association of obesity, gender, age and occupation with carpal tunnel syndrome. Aust N Z J Surg. 1998;68:190–3. doi: 10.1111/j.1445-2197.1998.tb04743.x. http://dx.doi.org/10.1111/j.1445-2197.1998.tb04743.x. [DOI] [PubMed] [Google Scholar]
- 61.Wang M, Shen J, Jin H, Im HJ, Sandy J, Chen D. Recent progress in understanding molecular mechanisms of cartilage degeneration during osteoarthritis. Ann N Y Acad Sci. 2011;1240:61–9. doi: 10.1111/j.1749-6632.2011.06258.x. http://dx.doi.org/10.1111/j.1749-6632.2011.06258.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Baker BA, Cutlip RG. Skeletal muscle injury versus adaptation with aging: novel insights on perplexing paradigms. Exerc Sport Sci Rev. 2010;38(1):10–6. doi: 10.1097/JES.0b013e3181c5cd7c. http://dx.doi.org/10.1097/JES.0b013e3181c5cd7c. [DOI] [PubMed] [Google Scholar]
- 63.Mayer J, Kraus T, Ochsmann E. Longitudinal evidence for the association between work-related physical exposures and neck and/or shoulder complaints: a systematic review. Int Arch Occup Environ Health. 2012;85(6):587–603. doi: 10.1007/s00420-011-0701-0. http://dx.doi.org/10.1007/s00420-011-0701-0. [DOI] [PubMed] [Google Scholar]
- 64.Hoe VCW, Urquhart DM, Kelsall HL, Sim MR. Ergonomic design and training for preventing work-related musculoskeletal disorders of the upper limb and neck in adults. Cochrane Database of Systematic Reviews. 2012 doi: 10.1002/14651858.CD008570.pub2. Issue 8. Art. No.: CD008570. http://dx.doi.org/10.1002/14651858.CD008570.pub2. [DOI] [PMC free article] [PubMed]
- 65.Koleva M, Kostova V. Occupational and personal risk factors for musculo-skeletal disorders in fertilizer plant workers. Cent Eur J Public Health. 2003;11(1):9–13. [PubMed] [Google Scholar]
- 66.Roquelaure Y, Mariel J, Dano C, Fanello S, Penneau-Fontbonne D. Prevalence, incidence and risk factors of carpal tunnel syndrome in a large footwear factory. Int J Occup Med Environ Health. 2001;14(4):357–67. [PubMed] [Google Scholar]
- 67.Han K, Trinkoff AM, Storr CL, Geiger-Brown J. Job stress and work schedules in relation to nurse obesity. J Nurs Adm. 2011;41(11):488–95. doi: 10.1097/NNA.0b013e3182346fff. http://dx.doi.org/10.1097/NNA.0b013e3182346fff. [DOI] [PubMed] [Google Scholar]
- 68.Bodin J, Ha C, Sérazin C, Descatha A, Leclerc A, Goldberg M, Roquelaure Y. Effects of individual and work-related factors on incidence of shoulder pain in a large working population. J Occup Health. 2012;54(4):278–88. doi: 10.1539/joh.11-0262-oa. http://dx.doi.org/10.1539/joh.11-0262-OA. [DOI] [PubMed] [Google Scholar]
- 69.Jensen LK. Knee osteoarthritis: influence of work involving heavy lifting, kneeling, climbing stairs or ladders, or kneeling/squatting combined with heavy lifting. Occup Environ Med. 2008;65(2):72–89. doi: 10.1136/oem.2007.032466. http://dx.doi.org/10.1136/oem.2007.032466. [DOI] [PubMed] [Google Scholar]
- 70.Coggon D, Croft P, Kellingray S, Barrett D, McLaren M, Cooper C. Occupational physical activities and osteoarthritis of the knee. Arthritis Rheum. 2000;43(7):1443–9. doi: 10.1002/1529-0131(200007)43:7<1443::AID-ANR5>3.0.CO;2-1. http://dx.doi.org/10.1002/1529-0131(200007)43:7<1443::AID-ANR5>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 71.Toivanen AT, Heliövaara M, Impivaara O, Arokoski JP, Knekt P, Lauren H, et al. Obesity, physically demanding work and traumatic knee injury are major risk factors for knee osteoarthritis–a population-based study with a follow-up of 22 years. Rheumatology (Oxford) 2010;49(2):308–14. doi: 10.1093/rheumatology/kep388. http://dx.doi.org/10.1093/rheumatology/kep388. [DOI] [PubMed] [Google Scholar]
- 72.Palmer KT. Occupational activities and osteoarthritis of the knee. Br Med Bull. 2012;102:147–70. doi: 10.1093/bmb/lds012. http://dx.doi.org/10.1093/bmb/lds012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Klussmann A, Gebhardt HJ, Nubling M, Liebers F, Perea EQ, Cordier W, et al. Individual and occupational risk factors of knee osteoarthritis: results of a case-control study in Germany. Arthritis Res Therapy. 2010;12:R88. doi: 10.1186/ar3015. http://dx.doi.org/10.1186/ar3015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Reid CR, Bush PM, Cummings NH, McMullin DL, Durrani SK. A review of occupational knee disorders. J Occup Rehabil. 2010;20(4):489–501. doi: 10.1007/s10926-010-9242-8. http://dx.doi.org/10.1007/s10926-010-9242-8. [DOI] [PubMed] [Google Scholar]
- 75.Stream AR, Sutherland ER. Obesity and asthma disease phenotypes. Curr Opin Allergy Clin Immunol. 2012;12:76–81. doi: 10.1097/ACI.0b013e32834eca41. http://dx.doi.org/10.1097/ACI.0b013e32834eca41. [DOI] [PubMed] [Google Scholar]
- 76.Pacheco KA, Tarlo SM. Work-Related Asthma: A Case-Based Approach to Management. Immunol Allergy Clin N Am. 2011;31:729–46. doi: 10.1016/j.iac.2011.07.006. http://dx.doi.org/10.1016/j.iac.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 77.Quirce S, Bernstein JA. Old and New Causes of Occupational Asthma. Immunol Allergy Clin N Am. 2011;31:677–98. doi: 10.1016/j.iac.2011.07.001. http://dx.doi.org/10.1016/j.iac.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 78.Smith AM. The Epidemiology of Work-Related Asthma. Immunol Allergy Clin N Am. 2011;31:663–75. doi: 10.1016/j.iac.2011.07.009. http://dx.doi.org/10.1016/j.iac.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 79.Kimber I, Basketter DA, Dearman RJ. Chemical Allergens – What are the Issues? Toxicology. 2010;268:139–42. doi: 10.1016/j.tox.2009.07.015. http://dx.doi.org/10.1016/j.tox.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 80.Lombardo LJ, Balmes JR. Occupational asthma: a review. Environ Health Perspect. 2000;108(Suppl 4):697–704. doi: 10.1289/ehp.00108s4697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Marabini A, Siracusa A, Stopponi R, Tacconi C, Abbritti G. Outcome of occupational asthma in patients with continuous exposure: a 3-year longitudinal study during pharmacologic treatment. Chest. 2003;124(6):2372–6. doi: 10.1378/chest.124.6.2372. http://dx.doi.org/10.1378/chest.124.6.2372. [DOI] [PubMed] [Google Scholar]
- 82.Suarthana E, Heederik D, Ghezzo H, Malo JL, Kennedy SM, Gautrin D. Risks for the development of outcomes related to occupational allergies: an application of the asthma-specific job exposure matrix compared with self-reports and investigator scores on job-training-related exposure. Occup Environ Med. 2009;66(4):256–63. doi: 10.1136/oem.2008.041962. http://dx.doi.org/10.1136/oem.2008.041962. [DOI] [PubMed] [Google Scholar]
- 83.Toren K, Brisman J, Olin AC, Blanc PD. Asthma on the job: work-related factors in new-onset asthma and in exacerbations of pre-existing asthma. Respir Med. 2000;94(6):529–35. doi: 10.1053/rmed.2000.0783. http://dx.doi.org/10.1053/rmed.2000.0783. [DOI] [PubMed] [Google Scholar]
- 84.King ME, Mannino DM, Holguin F. Risk Factors for Asthma Incidence – A review of recent prospective evidence. Panminerva Med. 2004;46:97–111. [PubMed] [Google Scholar]
- 85.Romero-Corral A, Caples SM, Lopez-Jimenez F, Somers VK. Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest. 2010;137(3):711–9. doi: 10.1378/chest.09-0360. http://dx.doi.org/10.1378/chest.09-0360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lurie A, editor. Obstructive Sleep Apnea in Adults: Epidemiology, Clinical Presentation, and Treatment Options Obstructive Sleep Apnea in Adults. Adv Cardiol Basel, Karger. 2011;(46):1–42. doi: 10.1159/000327660. [DOI] [PubMed] [Google Scholar]
- 87.Lundqvist G, Flodin U, Axelson O. A case-control study of fatty liver disease and organic solvent exposure. Am J Ind Med. 1999;35(2):132–6. doi: 10.1002/(sici)1097-0274(199902)35:2<132::aid-ajim4>3.0.co;2-i. http://dx.doi.org/10.1002/(SICI)1097-0274(199902)35:2<132::AID-AJIM4>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 88.Cave M, Appana S, Patel M, Falkner KC, McClain CJ, Brock G. Polychlorinated Biphenyls, Lead, and Mercury are Associated with Liver Disease in American Adults: NHANES 2003–2004. Environ Health Perspect. 2010;118:1735–42. doi: 10.1289/ehp.1002720. http://dx.doi.org/10.1289/ehp.1002720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cotrim HP, De Freitas LA, Freitas C, Braga L, Sousa R, Carvalho F, Paraná R, Santos-Jesus R, Andrade Z. Clinical and histopathological features of NASH in workers exposed to chemicals with or without associated metabolic conditions. Liver Int. 2004;24(2):131–5. doi: 10.1111/j.1478-3231.2004.0897.x. http://dx.doi.org/10.1111/j.1478-3231.2004.0897.x. [DOI] [PubMed] [Google Scholar]
- 90.Tanné F, Gagnadoux F, Chazouillères O, Fleury B, Wendum D, Lasnier E, et al. Chronic liver injury during obstructive sleep apnea. Hepatology. 2005;41(6):1290–6. doi: 10.1002/hep.20725. http://dx.doi.org/10.1002/hep.20725. [DOI] [PubMed] [Google Scholar]
- 91.Torres DM, Williams CD, Harrison SA. Features, Diagnosis, and Treatment of Nonalcoholic Fatty Liver Disease. Clin Gastro Hepatol. 2012;10:837–58. doi: 10.1016/j.cgh.2012.03.011. http://dx.doi.org/10.1016/j.cgh.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 92.Steeves JA, Bassett DR, Thompson DL, Fitzhugh EC. Relationships of occupational and non-occupational physical activity to abdominal obesity. Int J Obesity. 2012;36:100–6. doi: 10.1038/ijo.2011.50. http://dx.doi.org/10.1038/ijo.2011.50. [DOI] [PubMed] [Google Scholar]
- 93.Chau JY, van der Ploeg HP, Merom D, Chey T, Bauman AE. Cross-sectional associations between occupational and leisure-time sitting, physical activity and obesity in working adults. Prev Med. 2012;54(3–4):195–200. doi: 10.1016/j.ypmed.2011.12.020. http://dx.doi.org/10.1016/j.ypmed.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 94.Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55(11):2895–905. doi: 10.1007/s00125-012-2677-z. http://dx.doi.org/10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- 95.Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJF, Martin BW, for the Lancet Physical Activity Series Working Group Correlates of physical activity: why are some people physically active and other not? Lancet. 2012;380:258–71. doi: 10.1016/S0140-6736(12)60735-1. http://dx.doi.org/10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 96.Teske JA, Billington CJ, Kuskowski MA, Kotz CM. Spontaneous physical activity protects against fat mass gain. Int J Obesity. 2012;36:603–13. doi: 10.1038/ijo.2011.108. http://dx.doi.org/10.1038/ijo.2011.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sakkou M, Wiedmer P, Anlag K, Hamm A, Seuntjens E, Ettwiller L, et al. A role for brain-specific homeobox factor Bsx in the control of hyperphagia and locomotory behavior. Cell Metab. 2007;5:450–63. doi: 10.1016/j.cmet.2007.05.007. http://dx.doi.org/10.1016/j.cmet.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 98.Qi Q, Li Y, Chomistek AK, Kang JH, Curham GC, Pasquale LR, et al. Television watching, leisure time physical activity, and the genetic predisposition in relation to body mass index in women and men. Circulation. 2012;126:1821–7. doi: 10.1161/CIRCULATIONAHA.112.098061. http://dx.doi.org/10.1161/CIRCULATIONAHA.112.098061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56(11):2655–67. doi: 10.2337/db07-0882. http://dx.doi.org/10.2337/db07-0882. [DOI] [PubMed] [Google Scholar]
- 100.Thompson WG, Levine JA. Productivity of transcriptionists using a treadmill desk. Work. 2011;40(4):473–7. doi: 10.3233/WOR-2011-1258. [DOI] [PubMed] [Google Scholar]
- 101.Buckle P, Buckle J. Obesity, ergonomics, and public health. Persp Pub Health. 2011;131:17–176. doi: 10.1177/1757913911407267. http://dx.doi.org/10.1177/1757913911407267. [DOI] [PubMed] [Google Scholar]
- 102.Mathus-Vliegen EM. Obesity and the elderly. J Clin Gastroenterol. 2012;46(7):533–44. doi: 10.1097/MCG.0b013e31825692ce. http://dx.doi.org/10.1097/MCG.0b013e31825692ce. [DOI] [PubMed] [Google Scholar]
- 103.Villareal DT, Apovian CM, Kushner RF, Klein S, American Society for Nutrition; NAASO, The Obesity Society Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Am J Clin Nutr. 2005;82(5):923–34. doi: 10.1093/ajcn/82.5.923. [DOI] [PubMed] [Google Scholar]
- 104.Irigaray P, Ogier V, Jacquenet S, Notet V, Sibille P, Méjean L, et al. Benzo[a]pyrene impairs beta-adrenergic stimulation of adipose tissue lipolysis and causes weight gain in mice. A novel molecular mechanism of toxicity for a common food pollutant. FEBS J. 2006;273(7):1362–72. doi: 10.1111/j.1742-4658.2006.05159.x. http://dx.doi.org/10.1111/j.1742-4658.2006.05159.x. [DOI] [PubMed] [Google Scholar]
- 105.Hoppe AA, Carey GB. Polybrominated diphenyl ethers as endocrine disruptors of adipocyte metabolism. Obesity (Silver Spring) 2007;15(12):2942–50. doi: 10.1038/oby.2007.351. http://dx.doi.org/10.1038/oby.2007.351. [DOI] [PubMed] [Google Scholar]
- 106.De Coster S, van Larabeke N. Endocrine-Disrupting Chemical: Associated Disorders and Medchanisms of Action. J Environ Public Health. 2012;2012:713696. doi: 10.1155/2012/713696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Weiss B. The intersection of neurotoxicology and endocrine disruption. Neurotoxicology. 2012;33(6):1410–9. doi: 10.1016/j.neuro.2012.05.014. http://dx.doi.org/10.1016/j.neuro.2012.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Grun F, Blumberg B. Minireview: The case for obesogens. Mol Endocrinol. 2009;23(8):1127–34. doi: 10.1210/me.2008-0485. http://dx.doi.org/10.1210/me.2008-0485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Snijder CA, Brouwers MM, Jaddoe VW, Hofman A, Roeleveld N, Burdorf A. Occupational exposure to endocrine disruptors and time to pregnancy among couples in a large birth cohort study: the Generation R Study. Fertil Steril. 2011;95(6):2067–72. doi: 10.1016/j.fertnstert.2011.02.017. http://dx.doi.org/10.1016/j.fertnstert.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 110.Brophy JT, Keith MM, Watterson A, Park R, Gilbertson M, Maticka-Tyndale E, et al. Breast cancer risk in relation to occupations with exposure to carcinogens and endocrine disruptors: a Canadian case-control study. Environ Health. 2012;11:87. doi: 10.1186/1476-069X-11-87. http://dx.doi.org/10.1186/1476-069X-11-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ostry AS, Radi S, Louie AM, LaMontagne AD. Psychosocial and other working conditions in relation to body mass index in a representative sample of Australian workers. BMC Public Health. 2006;2:6. doi: 10.1186/1471-2458-6-53. :53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Heraclides AM, Chandola T, Witte DR, Brunner EJ. Work stress, obesity and the risk of type 2 diabetes: gender-specific bidirectional effect in the Whitehall II study. Obesity (Silver Spring) 2012;20(2):428–33. doi: 10.1038/oby.2011.95. http://dx.doi.org/10.1038/oby.2011.95. [DOI] [PubMed] [Google Scholar]
- 113.Tsurugano S, Nakao M, Takeuchi T, Nomura K, Yano E. Job stress strengthens the link between metabolic risk factors and renal dysfunction in adult men. Tohoku J Exp Med. 2012;226(2):101–8. doi: 10.1620/tjem.226.101. http://dx.doi.org/10.1620/tjem.226.101. [DOI] [PubMed] [Google Scholar]
- 114.Yamada Y, Kameda M, Noborisaka Y, Suzuki H, Honda M, Yamada S. Excessive fatigue and weight gain among cleanroom workers after changing from an 8-hour to a 12-hour shift. Scand J Work Environ Health. 2001;27(5):318–26. doi: 10.5271/sjweh.620. http://dx.doi.org/10.5271/sjweh.620. [DOI] [PubMed] [Google Scholar]
- 115.Garaulet M, Ordovás JM, Madrid JA. The chronobiology, etiology and pathophysiology of obesity. Int J Obes (Lond) 2010;34(12):1667–83. doi: 10.1038/ijo.2010.118. http://dx.doi.org/10.1038/ijo.2010.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Karlsson B, Knutsson A, Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27,485 people. Occup Environ Med. 2001;58:747–52. doi: 10.1136/oem.58.11.747. http://dx.doi.org/10.1136/oem.58.11.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Green CB, Takahashi JS, Bass J. The meter of metabolism. Cell. 2008;134:728–42. doi: 10.1016/j.cell.2008.08.022. http://dx.doi.org/10.1016/j.cell.2008.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Turek FW, Joshu C, Kohsaka A, Lin E, Ivanova G, McDearmon E, et al. Obesity and metabolic syndrome in Circadian Clock mutant mice. Science. 2005;308:1043–5. doi: 10.1126/science.1108750. http://dx.doi.org/10.1126/science.1108750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Rudic RD, McNamara P, Curtis A-M, et al. BMAL1 and CLOCK, two essential components of the circadian clock, are invovlved in glucose homeostasis. PLoS Biology. 2004;2(11):e377. doi: 10.1371/journal.pbio.0020377. http://dx.doi.org/10.1371/journal.pbio.0020377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Salgado-Delgado R, Angeles-Castellanos M, Buijs MR, et al. Internal desynchronization in a model of night-work forced activity in rats. Neurosci. 2008;154:922–31. doi: 10.1016/j.neuroscience.2008.03.066. http://dx.doi.org/10.1016/j.neuroscience.2008.03.066. [DOI] [PubMed] [Google Scholar]
- 121.Mavanji V, Billington CJ, Kotz CM, Teske JA. Sleep and obesity: A focus on animal models. Neurosci Biobehav Rev. 2012;36:1015–29. doi: 10.1016/j.neubiorev.2012.01.001. http://dx.doi.org/10.1016/j.neubiorev.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ekmekcioglu C, Touitou Y. Chronobiological aspects of food intake and metabolism and their relevance on energy balance and weight regulation. Obes Rev. 2011 Jan;12(1):14–25. doi: 10.1111/j.1467-789X.2010.00716.x. http://dx.doi.org/10.1111/j.1467-789X.2010.00716.x. [DOI] [PubMed] [Google Scholar]
- 123.Tan D-X, Manchester LC, Fuentes-Broto L, Paredes SD, Reiter RJ. Significance and application of melatonin in the regulation of brown adipose tissue metabolism: Relation to human obesity. Obes Rev. 2010;12:167–88. doi: 10.1111/j.1467-789X.2010.00756.x. http://dx.doi.org/10.1111/j.1467-789X.2010.00756.x. [DOI] [PubMed] [Google Scholar]
- 124.Garaulet M, Madrid JA. Chronobiology, genetics and metabolic syndrome. Curr Opin Lipidology. 2009;20(2):127–34. doi: 10.1097/MOL.0b013e3283292399. http://dx.doi.org/10.1097/MOL.0b013e3283292399. [DOI] [PubMed] [Google Scholar]
- 125.Broussard JL, Ehrmann DA, Van Cauter E, Tasali E, Brady MJ. Impaired insulin signaling in human adipocytes after experimental sleep restriction. Ann Intern Med. 2012;157:549–57. doi: 10.7326/0003-4819-157-8-201210160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Lowden A, Moreno C, Holmbäck U, Lennernäs M, Tucker P. Eating and shift work: Effects on habits, metabolism, and performance. Scand J Work Environ Health. 2010;36:150–62. doi: 10.5271/sjweh.2898. http://dx.doi.org/10.5271/sjweh.2898. [DOI] [PubMed] [Google Scholar]
- 127.Asterholm IW, Scherer PE. Metabolic jet lag when the fat clock is out of sync. Nat Med. 2012;18(12):1738–40. doi: 10.1038/nm.3010. http://dx.doi.org/10.1038/nm.3010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Paschos GK, Ibrahim S, Song W-L, Kunieda T, Grant G, Reyes TM, et al. Obesity in mice with adipocyte-specific deletion of clock component Arntl. Nat Med. 2012;18(12):1768–77. doi: 10.1038/nm.2979. http://dx.doi.org/10.1038/nm.2979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kovacic JC, Castellano JM, Fuster V. Cardiovascular defense challenges at the basic, clinical, and population levels. Ann N Y Acad Sci. 2012 Apr;1254:1–6. doi: 10.1111/j.1749-6632.2012.06495.x. http://dx.doi.org/10.1111/j.1749-6632.2012.06495.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gan WQ, Davies HW, Demers PA. Exposure to occupational noise and cardiovascular disease in the United States: the National Health and Nutrition Examination Survey 1999–2004. Occup Environ Med. 2011;68:183–90. doi: 10.1136/oem.2010.055269. http://dx.doi.org/10.1136/oem.2010.055269. [DOI] [PubMed] [Google Scholar]
- 131.Attarchi M, Golabadi M, Labbafinejad Y, Mohammadi S. Combined effects of exposure to occupational noise and mixed organic solvents on blood pressure in car manufacturing company workers. Am J Ind Med. 2013 Feb;56(2):243–51. doi: 10.1002/ajim.22086. http://dx.doi.org/10.1002/ajim.22086. [DOI] [PubMed] [Google Scholar]
- 132.Attarchi M, Dehghan F, Safakhah F, Nojomi M, Mohammadi S. Effect of exposure to occupational noise and shift working on blood pressure in rubber manufacturing company workers. Ind Health. 2012;50(3):205–13. doi: 10.2486/indhealth.ms1321. http://dx.doi.org/10.2486/indhealth.MS1321. [DOI] [PubMed] [Google Scholar]
- 133.Chang TY, Liu CS, Huang KH, Chen RY, Lai JS, Bao BY. High-frequency hearing loss, occupational noise exposure and hypertension: a cross-sectional study in male workers. Environ Health. 2011 Apr 25;10:35. doi: 10.1186/1476-069X-10-35. http://dx.doi.org/10.1186/1476-069X-10-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychol. 2008 Mar;27(2 Suppl):S101–8. doi: 10.1037/0278-6133.27.2(Suppl.).S101. http://dx.doi.org/10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.The Community Guide. The Guide to Community Preventive Services (home page). [cited 2013 March 15] Georgia, USA: CDC (Centers for Disease Control and Prevention); 2012. Available from: http://www.thecommunityguide.org. [Google Scholar]
- 136.Christie J, O’Halloran P, Caan W, Cardwell CR, Young T, Rao M. Workplace-based organisational interventions to prevent and control obesity by improving dietary intake and/or increasing physical activity (Protocol) Cochrane Database of Systematic Reviews 2010. Issue 6. Art. No.: CD008546. http://dx.doi.org/10.1002/14651858.CD008546.
- 137.Lemon SC, Pratt CA. Worksite environmental interventions for obesity control: an overview. J Occup Environ Med. 2010;52(Suppl 1):S1–3. doi: 10.1097/JOM.0b013e3181c8527e. http://dx.doi.org/10.1097/JOM.0b013e3181c8527e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Sorensen G, Barbeau EM. Integrating occupational health, safety and worksite health promotion: opportunities for research and practice. Med Lav. 2006;97(2):240–57. [PubMed] [Google Scholar]


