Abstract
Background:
Realizing a dearth of data on this topic, especially in the Indian context, an epidemiological study was conducted in a south Indian rural population to identify the sexual activity patterns and sexual problems among the population above 60 years of age.
Objectives:
(1) Assessment of sexual activity patterns among individuals above 60 years. (2) Assessment of the prevalence of sexual disorders among individuals above 60 years.
Materials and Methods:
The study sample consisted of 259 participants, which included both males and females above 60 years of age. Subjects who were sexually active and fulfilled the study criteria were administered Arizona Sexual Experience Scale as a screening tool, for the presence of sexual problems. Those who were found to have sexual problems were interviewed further using appropriate questionnaires.
Results:
Only 27.4% of the individuals above 60 years were sexually active, and it progressively dropped as age advanced and none were sexually active after 75 years of age. Among the sexually active males, erectile dysfunction (ED) was prevalent in 43.5%, premature ejaculation in 10.9%, hypoactive sexual desire disorder (HSSD) in 0.77% and anorgasmia in 0.38% of the subjects. Among females, arousal disorder was prevalent in 28%, HSSD in 16%, anorgasmia in 20% and dyspareunia in 8% of the subjects.
Conclusion:
The study gives us an insight into the sexual problems of the elderly and brings home the point that sexual problems are very much common among both men and women in the older population. Among elderly males, ED is the most common sexual disorder whereas in elderly females, arousal disorder is the most prevalent female sexual dysfunction, implicating biology plays an important role in men, whereas psychology plays an important role in women sexual functioning.
Keywords: Epidemiological study, sexual disorders, geriatric sexuality, prevalence study, elderly sexuality, prevalence of sexual disorders in India, chronic medical disorders and sexual function
INTRODUCTION
Elderly sexuality and issues related to it have long been neglected not only from the treatment aspect but also from research point of view. The common misconception is that the elderly are asexual individuals and sexual activity is meant only for the young. Sexuality in older individuals cannot be seen through the lenses of the youth, primarily focusing on performance and erectile capacity, while overlooking psychological and interpersonal dimensions.[1,2,3]
With the advancement in the medical field, the life expectancy has increased; hence it becomes all the more important to address sexuality related issues in the elderly population.[4,5,6,7] Coming to terms with the fact that a large lacunae is there in this area of research, the current study was undertaken to access the sexual activity pattern and prevalence of sexual disorders among elderly above 60 years of age.
MATERIALS AND METHODS
An Exploratory study, was conducted using purposive sampling (sample size: n=259; 8.5 % of the selected rural population was above 60 years). Individuals above 60 years of age, who gave informed consent were included; however those with psychotic symptoms, dementia or mental retardation were excluded. Using descriptive and inferential statistics, contingency coefficient tests were applied to study the association using SPSS for Windows, Version 16.0. Chicago, SPSS Inc.
A door to door survey of the entire population residing at Suttur village (25 km from Mysore city; Population~4100; predominant Hindu population, with around 1000 families) was conducted. Of 311 subjects fulfilling the inclusion criteria, 259 subjects gave informed consent to participate in the study.
Sociodemographic data were collected as per the prepared standard questionnaire. In our study, we defined sexually active subjects as those who have at least one intercourse in the previous year. Those who were identified to be sexually active were administered Arizona sexual experience scale for screening the presence of sexual problems. Those who were found to be having sexual problems-based on Arizona sexual experience scale were further interviewed in detail to identify the type of sexual disorders. Male sexual disorders were assessed using International Index of Erectile Function (IIEF), premature ejaculation diagnostic tool (PEDT), a structured questionnaire prepared for the purpose of the study to assess male hypoactive sexual desire disorder (HSDD), postcoital dysphoria, anorgasmia, dyspareunia, paraphilias, sexual aversion disorder and gender identity disorders based on International Classification of Diseases 10 (ICD-10) and Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Text Revision (DSM-IV TR) diagnostic criteria. Female sexual disorders were assessed using female sexual functioning questionnaire and a structured questionnaire prepared for the purpose of the study to assess female postcoital dysphoria, anorgasmia, dyspareunia, paraphilias, sexual aversion disorder and gender identity disorders based on ICD-10 and DSM-IV diagnostic criteria.
Sociodemographic data and sexual activity proforma were used. Sociodemographic status assessment was based on modified Prasad's classification[8] Sexual functioning was assessed using Arizona sexual experience scale[9], IIEF for males[10], PEDT for males[11], Female sexual function questionnaire[12] and Structured interview schedule for diagnosing other sexual disorders based on DSM IV and ICD-10 criteria.[13,14]
RESULTS
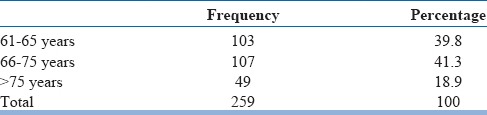
In our study sample of 259, majority of the subjects were between 66 and 75 years of age [Table 1]. Gender distribution was found almost to be equal with 55.2% being males and 44.8% being females. Most of the subjects (87.3%) were married and 12.7% of the subjects were single, either unmarried, divorced or their spouse had passed away. 98.5% of the subjects were illiterates. Most females continued to function as homemakers which constituted 31.7% of the study sample. 29% were unemployed, 21.2% were agriculturists and 17.8% worked as daily wage laborers. 46.3% of the subjects were residing in nuclear families, while 49% were residing in joint families and 4.6% were living alone. Majority of the study subjects belonged to either lower middle class (43.6%) or upper lower class (40.9%) according to modified Prasad classification for socioeconomic status. Diabetes mellitus (10.4%) and hypertension (7.3%) were found to be the most prevalent chronic medical conditions. 2.30% of the study population consumed alcohol and 6.2% used tobacco. Except for the distribution of the study population by gender, P value was significant for the distribution of study population by age, marital status, education, occupation, residing family structure, socioeconomic status, chronic medical condition, alcohol consumption and nicotine consumption.
Table 1.
Age distribution of the study sample
In our study, we defined sexually active subjects as those who had at least one intercourse in the previous year. Those who were sexually active were further interviewed to identify the presence of sexual disorders. Only 27.4% of the subjects were sexually active in our study sample [Table 2]. On analyzing the sociodemographic variables of subjects who were sexually active and sexually inactive, we found that there is a rapid decline in the sexual activity as the subjects grow older. Number of sexually active individuals dropped significantly from 47.6%, in 61-65 years age group to 0% in those above 75 years of age. Females were less sexually active when compared to males. Those subjects who were married and had a living spouse were more sexually active compared to those without a spouse. Subjects who were employed were more sexually active compared to those who were unemployed. Subjects living in a joint family had slightly lesser active sexual life compared to those living in a nuclear family. Subjects with diabetes mellitus were less sexually active compared to those without any chronic medical condition. However, other chronic medical conditions had no adverse influence on a subject's sexual activity. Subjects from the upper class were found to be less sexually active compared to those from lower socioeconomic classes [Table 3]. No significant difference was found among those who consumed alcohol and tobacco compared to those subjects who did not.
Table 2.
Distribution of sexually active and sexually not active subjects
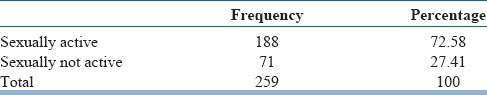
Table 3.
Distribution of sexually active and sexually not active subjects versus sociodemographic variables
Although we did not evaluate the various reasons for not being sexually active methodologically, during our study we learned that myths and misconceptions that sex is only for procreation, a perception that performing sexual activity after middle age is shameful or morally and spiritually incorrect for one or both the partners, self-declaration from one or both the partners to stop sexual intimacy once their kids grow above puberty, lack of privacy, lack of cooperation from one of the spouse, fear that if caught in a sexual act or any such suspicion among their children that their parents are having sexual activity is shameful were some of the reasons for not having sexual intercourse that are noted during our study.
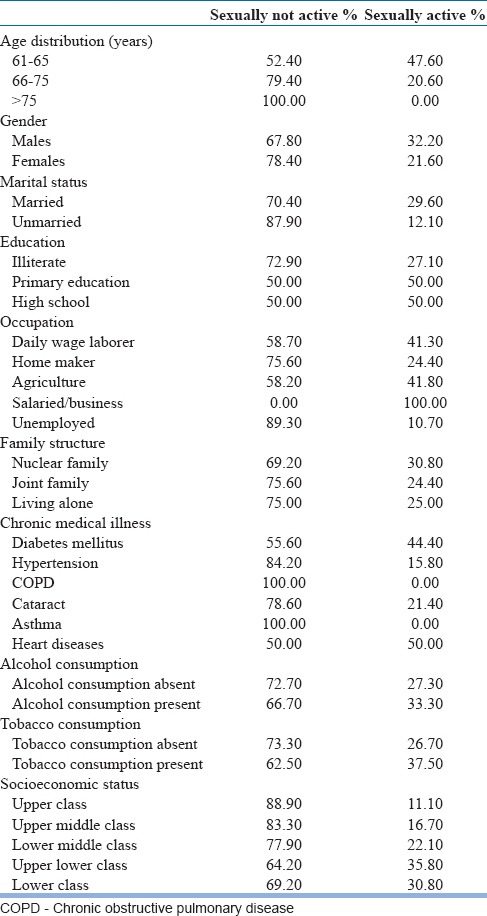
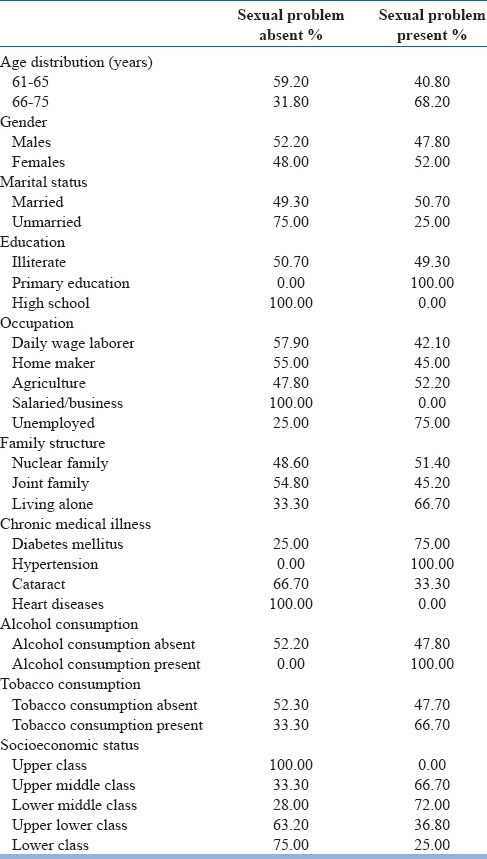
Among those who were sexually active, 49.3% of them were found to have one or more sexual disorder on using Arizona sexual experience screening questionnaire [Table 4]. These subjects were interviewed in detail to identify the various sexual disorders they were suffering from. On analyzing the sociodemographic variables of subjects who were sexually active and found to be having sexual problems we found the following results. Sexual problems increased with increasing age, 40.8% of those between 61-65 years had sexual problems compared with 68.2% among those between 66 and 75 years. We found none above 75 years to be sexually active; perhaps if we had sexually active individuals above 75 years in our sample it would have helped us in having more definite information about the impact of growing age on sexual activity. Females had slightly higher prevalence of sexual problems compared to males. Sexual problems were highly prevalent among the married and those who were unemployed. 100% of the subjects who were sexually active and were hypertensive had sexual problems, while 75% of those with diabetes mellitus had sexual problems. Those who consumed alcohol and tobacco had a higher prevalence of sexual problems compared to those who did not [Table 5].
Table 4.
Distribution of sexual problems based on Arizona sexual experience screening questionnaire
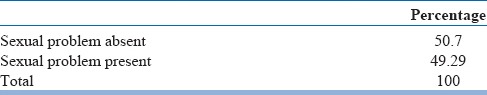
Table 5.
Distribution of sexual problems versus sociodemographic variables
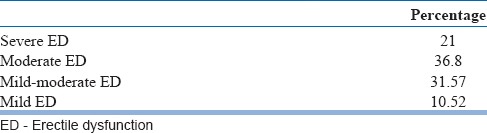
Among 259 subjects above 60 years, 71 were sexually active and were interviewed for identifying the prevalence of sexual disorders. 43.5% of the male subjects were diagnosed to have erectile dysfunction (ED), 10.9% premature ejaculation, 0.77% male HSSD and 0.38% of males had anorgasmia [Table 6]. Distribution of ED based on the severity of ED is given in Table 7. No cases of male postcoital dysphoria, gender identity disorder or paraphilias were found. Presence of male sexual disorders and chronic medical illness such as diabetes mellitus, hypertension and others was found to have a significant association. Age distribution above 60 years, occupation, education, sociodemographic status, domicile, family structure, alcohol and smoking were not found to have a significant association in causing sexual disorders among the elderly.
Table 6.
Prevalence of male sexual disorders among individuals above 60 years
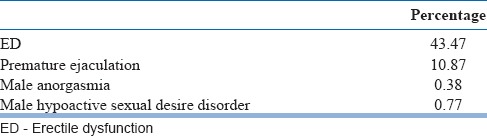
Table 7.
Distribution of ED by severity among individuals above 60 years
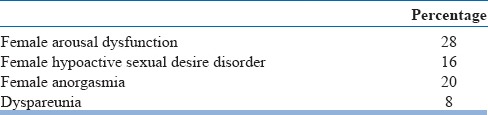
Prevalence of female arousal dysfunction was found to be 28%, female HSSD 16%, female anorgasmia 20% and dyspareunia in 8% of the female subjects [Table 8]. No cases of female postcoital dysphoria, female identity disorder or paraphilias were found. Differing from males, among females only socioeconomic status was found to have a significant association with the prevalence of sexual disorders. Age distribution above 60 years, occupation, education, chronic medical illness, domicile, family structure, alcohol and smoking were not found to have a significant association in causing sexual disorders among the elderly.
Table 8.
Prevalence of female sexual disorders among individuals above 60 years
DISCUSSION
The study found that only 27.4% of the subjects above 60 years were sexually active and there is a rapid decline in sexual activity with age. Studies have observed that decline in sexual activity with ageing is influenced more by culture and attitudes rather than by nature and physiology among the elderly.[15,16,17] The two most important influences on older age sexual interaction are the strength of the relationship and the physical condition of each partner. Individuals who had relationship issues with their partners earlier in life tend to report more sexual problems like lack of desire, dyspareunia and anorgasmia and eventually stop sexual activity. Many elderly lead a single life due to death of spouse, which itself curtails their sexual activity. Both the partners being healthy is another important aspect as they may not be able to enjoy an active sexual life if either is physically ailing which is common at older age.[16] Due to various physical ailments, either of the partners may be on medications which too may interfere with sexual activity. Supporting the notion that physical health plays an important role, our study found that subjects with chronic medical illness were less sexually active than those without medical illness.
We also noted that females were less sexually active compared to males. In the PRESIDE study, the prevalence of female HSSD above 65 years was 74.8%. The prevalence of sexual problems in women increased dramatically with age.[18,19] Long standing undiagnosed and untreated HSDD might be one of the reasons for females to stop sexual activity, in turn affecting the sexual activity of their male spouse. This stresses the need of early identification and treatment of sexual disorders among elderly.
There is paucity of research in the area of sexual disorders among the elderly; however studies in this area have reported a higher prevalence of sexual disorders among individuals above 60 years of age.[20,21,22] Data from the Massachusetts Male Aging Study showed that 34.8% of men aged 40-70 years had moderate to complete ED, which was strongly related to age, health status, and emotional function.[23] The current study found ED in 43.5% individuals above 60 years of age. Kinsey et al. found that ED occurs in <1% of the male population before age 19, increasing to 25% by age 75 suggesting that as age increases sexual disorders too increase.[24] Study by Laumann et al. observed the older cohort of men (ages 50-59 years) is more than 3 times as likely to experience erection problems and to report low sexual desire in comparison to men aged 18-29 years.[22] Community studies show an estimate of the 1 year prevalence of premature ejaculation range to be 4-5%.[25,26,27,28] Two other studies reported significantly higher rates of premature ejaculation estimating prevalence to be of 14% and 29%.[22,29] Panser et al. reported a significant positive correlation between age and HSSD (age 70 and over prevalence was 26%).[30] The current study found prevalence of premature ejaculation to be 10.9% and male HSSD to be 0.77% in individuals above 60 years. The reason for these discrepant estimates may be due to differing methodology adopted. The prevailing cultural beliefs in our country might discourage and inhibit the older individuals to consult a doctor and discuss about their sexual life leading to increased prevalence of sexual disorder among elder age groups. Also the age related physiological changes like andropause may explain higher prevalence rates of sexual problems.
In our study, male sexual disorders were more among subjects with chronic medical illness compared to those without chronic medical illness. Studies have shown that prevalence of sexual disorder increases with age, history of heart disease, diabetes, hypertension, untreated ulcer, arthritis, allergy, and smoking.[22,28,30,31] Some of these findings overlap with results in the current study. Study by Thomas et al. suggests that, although sexual dysfunction is more common in the aged, it is often related more to comorbid illness than aging alone.[32]
In our study prevalence of female arousal dysfunction was found to be 28%, female HSSD in 16%, female anorgasmia in 20% and dyspareunia in 8% of the female subjects. Discussions regarding female sexual functioning especially in the older population, have not been a routine part of our health care, hence the magnitude of female sexual disorders in geriatric age group is poorly understood. A meta-analysis of prevalence of female sexual disorders suggested that sexual dysfunctions are highly prevalent across cultures with prevalence increasing with age.[19,33] Women's International Study of Health and Sexuality, showed that overall female sexual problems increased with age and reported that the prevalence of sexual problems were 74.8% (desire), 65.3% (arousal) and 54.6% (orgasm).[34] The prevalence of dyspareunia is known to increase among postmenopausal women; estimates of rates vary widely between 12% and 45%.[18] Lack of vascularity, both lubrication and swelling response are affected due to decreased estrogen after menopause.[19,35]
No cases of postcoital dysphoria or paraphilias were found in our study. Other Indian studies by Bagadia et al. and Avasthi et al. also did not report any cases with these problems. This probably reflects the extremely rare prevalence of these disorders in the general population.[36,37]
CONCLUSION
Geriatric sexuality is one of the most neglected areas in research. As stated earlier, studies have shown that sexual dysfunctions increase with age and the prevalence increases further with the presence of co-morbidities like chronic medical illnesses. Our study shows that sexual problems are very much common among both men and women in the older population. However, more detailed evaluation of sexual dysfunction among the elderly is needed. Sex education among the elderly to correct the myths and misconceptions regarding sexuality, in general and elderly sexuality, in particular is much needed. Further research in elderly sexuality needs to be undertaken in an elaborate manner to improve their quality of life and benefit them in the long run.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Masters WH, Johnsons VE. Boston: MA Brown; 1966. Human Sexual Response. [Google Scholar]
- 2.Schiavi RC. Sexuality and aging in men. Annual Review of Sex Research. 1990;1:227–50. [Google Scholar]
- 3.Sigler IC, Novlin JB, Bumenthol JA. Health and behavior: Methodological consideration for adult development and aging. In: Poon, Leonard W, editors. Aging in the 1980s: Psychological issues. 1st ed. Washington, DC: 1980. pp. 599–612. [Google Scholar]
- 4.Nugartoen. Age groups in American society and the rise of young old. Ann AM Acad. 1984;48:187–98. [Google Scholar]
- 5.Speroff L, Glass RH, Kase NG. Clinical Gynecologic Endocrinology and Infertility. Maryland: Lippincott Williams and Wilkins; 1999. Menopause and the perimenopausal transition; pp. 643–724. [Google Scholar]
- 6.Traub ML, Peck AC, Santoro N. Jameson JL, DeGroot LJ. Endocrinology Adult and Pediatric. Philadelphia: Saunders; 2010. Menopause; pp. 2428–38. [Google Scholar]
- 7.Clayton AH, Hamilton DV. Female sexual dysfunction. Psychiatr Clin North Am. 2010;33:323–38. doi: 10.1016/j.psc.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Prasad BG. Social classification of Indian families. J Indian Med Assoc. 1961;37:250–1. [PubMed] [Google Scholar]
- 9.McGahuey CA, Gelenberg AJ, Laukes CA, Moreno FA, Delgado PL, McKnight KM, et al. The Arizona Sexual Experience Scale (ASEX): Reliability and validity. J Sex Marital Ther. 2000;26:25–40. doi: 10.1080/009262300278623. [DOI] [PubMed] [Google Scholar]
- 10.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–30. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 11.Symonds T, Perelman MA, Althof S, Giuliano F, Martin M, May K, et al. Development and validation of a premature ejaculation diagnostic tool. Eur Urol. 2007;52:565–73. doi: 10.1016/j.eururo.2007.01.028. [DOI] [PubMed] [Google Scholar]
- 12.Quirk FH, Heiman JR, Rosen RC, Laan E, Smith MD, Boolell M. Development of a sexual function questionnaire for clinical trials of female sexual dysfunction. J Womens Health Gend Based Med. 2002;11:277–89. doi: 10.1089/152460902753668475. [DOI] [PubMed] [Google Scholar]
- 13.Text Revision (DSM-IV-TR) 4th ed. Washington, DC: American Psychiatric Association; 1994. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 14.World Heath Organization. Geneva: WHO; 1992. The ICD-10 classification of mental and behavioural disorders: Clinical description and diagnostic guidelines. [Google Scholar]
- 15.Oswald I. Amsterdam: Elseiver; 1962. Sleeping and waking, Physiology and Psychology. [Google Scholar]
- 16.Shivananda M, Darshan MS, Tandon A. Male issues in elderly sexuality. Intimacy matters. In: Rao TSS, Gupta S, Tandon A, editors. Elderly Sexuality. Mysore: Published by Indian Association of Geriatric Mental Health; 2011. pp. 131–43. [Google Scholar]
- 17.Rao TSS, Darshan MS, Harsha GT, Kalaiah P, Krishna VS, Brahmbhatt R. Sexual disorders: General perspectives. Intimacy matters. In: Rao TSS, Gupta S, Tandon A, editors. Elderly Sexuality. Mysore: Published by Indian Association of Geriatric Mental Health; 2011. pp. 53–83. [Google Scholar]
- 18.Shifren JL, Monz BU, Russo PA, Segreti A, Johannes CB. Sexual problems and distress in United States women: Prevalence and correlates. Obstet Gynecol. 2008;112:970–8. doi: 10.1097/AOG.0b013e3181898cdb. [DOI] [PubMed] [Google Scholar]
- 19.Behl A. Female sexuality issues in the elderly population. Intimacy matters. In: Rao TS, Gupta S, Tandon A, editors. Elderly Sexuality. Mysore: Published by Indian Association of Geriatric Mental Health; 2011. pp. 143–58. [Google Scholar]
- 20.Spector IP, Carey MP. Incidence and prevalence of the sexual dysfunctions: A critical review of the empirical literature. Arch Sex Behav. 1990;19:389–408. doi: 10.1007/BF01541933. [DOI] [PubMed] [Google Scholar]
- 21.Simons JS, Carey MP. Prevalence of sexual dysfunctions: Results from a decade of research. Arch Sex Behav. 2001;30:177–219. doi: 10.1023/a:1002729318254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: Prevalence and predictors. JAMA. 1999;281:537–44. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 23.Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: Results of the Massachusetts Male Aging Study. J Urol. 1994;151:54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- 24.Kinsey AC, Pomeroy WB, Martin C. Philadelphia: W. B. Saunders; 1948. Sexual behavior in the human male. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ernst C, Földényi M, Angst J. The Zurich Study: XXI. Sexual dysfunctions and disturbances in young adults. Data of a longitudinal epidemiological study. Eur Arch Psychiatry Clin Neurosci. 1993;243:179–88. doi: 10.1007/BF02190725. [DOI] [PubMed] [Google Scholar]
- 26.Fugl-Meyer AR, Fugl-Meyer KS. Sexual disabilities, problems, and satisfaction in 18-74 year old Swedes. Scand J Sexol. 1999;3:79–105. [Google Scholar]
- 27.Schiavi RC, Mandeli J, Schreiner-Engel P, Chambers A. Aging, sleep disorders, and male sexual function. Biol Psychiatry. 1991;30:15–24. doi: 10.1016/0006-3223(91)90066-u. [DOI] [PubMed] [Google Scholar]
- 28.Ventegodt S. Sex and the quality of life in Denmark. Arch Sex Behav. 1998;27:295–307. doi: 10.1023/a:1018655219133. [DOI] [PubMed] [Google Scholar]
- 29.Solstad K, Hertoft P. Frequency of sexual problems and sexual dysfunction in middle-aged Danish men. Arch Sex Behav. 1993;22:51–8. doi: 10.1007/BF01552912. [DOI] [PubMed] [Google Scholar]
- 30.Panser LA, Rhodes T, Girman CJ, Guess HA, Chute CG, Oesterling JE, et al. Sexual function of men ages 40 to 79 years: The Olmsted County Study of Urinary Symptoms and Health Status Among Men. J Am Geriatr Soc. 1995;43:1107–11. doi: 10.1111/j.1532-5415.1995.tb07009.x. [DOI] [PubMed] [Google Scholar]
- 31.Mannino DM, Klevens RM, Flanders WD. Cigarette smoking: An independent risk factor for impotence? Am J Epidemiol. 1994;140:1003–8. doi: 10.1093/oxfordjournals.aje.a117189. [DOI] [PubMed] [Google Scholar]
- 32.Thomas M, Sheldon MR, Vernon MC, Cynthia BB. The role of aging and chronic disease in sexual dysfunction. J Am Geriatr Soc. 1988;36:520–4. doi: 10.1111/j.1532-5415.1988.tb04022.x. [DOI] [PubMed] [Google Scholar]
- 33.Derogatis LR, Burnett AL. The epidemiology of sexual dysfunctions. J Sex Med. 2008;5:289–300. doi: 10.1111/j.1743-6109.2007.00668.x. [DOI] [PubMed] [Google Scholar]
- 34.Leiblum SR, Koochaki PE, Rodenberg CA, Barton IP, Rosen RC. Hypoactive sexual desire disorder in postmenopausal women: US results from the Women's International Study of Health and Sexuality (WISHeS) Menopause. 2006;13:46–56. doi: 10.1097/01.gme.0000172596.76272.06. [DOI] [PubMed] [Google Scholar]
- 35.Gracia CR, Freeman EW, Sammel MD, Lin H, Mogul M. Hormones and sexuality during transition to menopause. Obstet Gynecol. 2007;109:831–40. doi: 10.1097/01.AOG.0000258781.15142.0d. [DOI] [PubMed] [Google Scholar]
- 36.Bagadia VN, Deve KP, Pradhan PV, Shah LP. A study of 258 male patients with sexual problems. Indian J Psychiatry. 1972;14:143. [Google Scholar]
- 37.Avasthi A, Arora A, Kulhara P, Banerjee ST. A study of Psychosexually disordered patients attending a special clinic. Arch Indian Psychiatry. 1998;4:92–6. [Google Scholar]


