Abstract
Background:
Women's sexual dysfunction is found to be highly prevalent in western and Indian literature. Limited studies are available on drug naive depression in western literature and in Indian population.
Aim:
To determine the prevalence rate and symptom profile of female sexual dysfunctions in patients with untreated depression.
Design:
A cross-sectional study in the psychiatry out-patient department of general hospital in South India.
Materials and Methods:
Following written informed consent female sexual functioning index (FSFI) and Arizona Sexual Experience Scale (ASEX) – female version and Hamilton Depression Rating Scale (HAMD - 17 item) on 30 cases and 30 controls was administered. Sociodemographic data, pattern and type of sexual dysfunctions were enquired. Data were analyzed using descriptive statistics, contingency co-efficient analysis and stepwise multiple regression.
Results:
The mean score of HAMD 17 item in study group was 19.13. The study showed that female sexual dysfunction was 70.3% in study group compared to 43.3% in control FSFI scores above 16 in HAMD had dysfunction of 76% with FSFI in study group. With ASEX-F sexual dysfunction was 73.3% in study compared to 20% in control. Scores above 16 in HAMD had 80% of sexual dysfunction with ASEX-F in study group.
Conclusion:
The study found that ASEX-F co-related better with HAMD 17 item. Following the onset of depression, the incidence of sexual dysfunction started at an early age in women.
Keywords: Female sexual dysfunction, FSFI, drug naïve depression
INTRODUCTION
Depressive disorder is characterized by depressed mood, decreased energy and loss of interest in previously pleasurable activities. The somatic symptoms consist of lack of emotional reactivity, anhedonia, weight loss, terminal insomnia, psychomotor agitation or retardation, decreased appetite and marked loss of libido.[1] Worldwide studies have shown depression to be twice more common in women than men.[2,3,4] The prevalence of female sexual dysfunction in western countries is reported to be between 17% and 55%.[3,5] The high variability of the prevalence rates may be due to the different methods used in the studies-self rated or observer rated questionnaires, different tools used for assessment and the cultural differences in reporting sexual dysfunctions amongst women in different countries. Hardly any studies are available on sexual dysfunction in drug-naive depressed population. Hence, the prevalence of sexual dysfunction in women with depression is not really known.
In 1998 American foundation of urologic disease international conference modified the DSM IV criteria for female sexual dysfunction by suggesting sexually related personal distress before the manifestation of sexual dysfunction.[6] Lauman et al. in 1999 in United States studied data reported from the National health and social life survey conducted in 1992 on 1749 women aged 18-59 and found 43% with sexual dysfunction.[7] Reporting on a sample of 703 viennese women, using a questionnaire designed specifically for the study, Ponholzer et al. observed somewhat similar results.[8] Approximately 22% had low-sexual desire; 35% had arousal problems, 39% reported orgasmic difficulties and sexual pain disorders were reported by 12.8% of the sample. Age proved to be a substantial risk factor for increased rates of female sexual dysfunction. The Women's International Study of Health and Sexuality (WISHeS) was conducted in 1999 and 2000 via mail survey and personal interview on a large cross-sectional database of 4,517 women aged 20-70 years using validated self-report questionnaires, the profile of female sexual functioning (PFSF) and the personal distress scale (PDS)[3,9,10] in 5 countries. The women from the USA, UK, Germany, France, and Italy were included. Dennerstein et al.[11] reported on the prevalence of hypoactive sexual desire disorder (HSDD) in menopausal women from the four European countries. The PFSF desire scale were used to identify those individuals with low desire, while scores on the PDS determined women with high manifest distress. The sample was partitioned into premenopausal women, surgically menopausal women aged 20-49, surgically menopausal women aged 50-70, and naturally menopausal women. Rates of low sexual desire were 16%, 29%, 46%, and 42%, respectively. When distress levels were factored into determining cases of HSDD, the rates became 7%, 16%, 12%, and 9%. Contrast result was reported by Fugl-Meyer and Fugl-Meyer[12,13] on a Swedish sample, one-third indicated they suffered from low desire, but of that only 43% were distressed by it. The estimate of HSDD in that sample was 14%. Using the same database, Hayes et al.[14] analyzed the data looking at the relationship between HSDD and aging. Rates of low desire progressed from 11% among 20- to 29-year-old to 53% among women in the, 60-70 age group among Europeans and from 22% to 32% among comparable American samples. In both samples, there was a definite increase in rates of low sexual desire associated with age. Concomitantly, the nature of the relationship between age and distress was inverse, falling from 65% to 22% among Europeans, and 67-37% across the age range among American women. This disordinal relationship between low sexual desire and sexual distress resulted in a nonsignificant relationship between age and HSDD across the age range, with prevalence estimates ranging from 6% to 13% in Europe, and from 12% to 19% in the United States. Using the WISHeS dataset, Graziottin[15] estimated the prevalence of desire, arousal and orgasmic disorders based upon PFSF and PDS case definition criteria. She observed a significant inter country variation, with the highest rates of dysfunction in Germany and the United Kingdom and the lowest rates in Italy and France.
The ELIXIR conducted in France with 4557 patients of depression in 2003 showed the prevalence of disorders of sexual function was 35% for self-reported problems and 69% for problems identified by physician's questioning. A high score on the Arizona Sexual Experience Scale (ASEX) (mean overall score of 21.4) was seen. Frequency of sexual dysfunction was somewhat higher in patients treated with antidepressants than in untreated patients (71% and 65% respectively). Treatment with tianeptine was found to have lower incidence of sexual dysfunction than with tricyclic antidepressants or with selective serotonin reuptake inhibitors.[16] Various treatment modalities are available for female sexual dysfunction which include information and education about sexual intercourse, enhancement of stimulation by use of vibrators and masturbation, encouraging erotic and nonerotic fantasies, pelvic floor contraction and relaxation exercise, recommendation of sensual massage and sensate focus massage where the partner provides sensual message to nonsexual areas, use of testosterone for desire disorders (300 mcg trans dermal patch not approved by Food and Drug Administration [FDA]) has shown improvement in patients receiving hormone therapy. Topical and systemic estrogen had shown improvement in postmenopausal desire disorder. Another treatment option is the Eros Clitoral Therapy Device used for arousal disorder. The device is FDA-approved and is designed to improve arousal by increasing blood flow to the clitoris with gentle suction. Cognitive behavior therapy is used for orgasmic and pain disorder.[6,17]
A few Indian studies are available on sexual dysfunction.[18,19,20,21] Kar and Koola[21] conducted a postal survey among English-speaking persons from a south Indian town. They found orgasmic difficulties in 28.6% females, 40% of females had never masturbated. Avasthi et al. in 2008[19] conducted a study on 100 consecutive women attending the Department of Pediatrics for the care of noncritical children in a tertiary care teaching hospital in Chandigarh. They found 17% of the subjects encountered with difficulties in the form of headache after sexual activity (10%), difficulty reaching orgasm (9%), painful intercourse (7%), lack of vaginal lubrication (5%), vaginal tightness (5%), bleeding after intercourse (3%) and vaginal infection (2%). 14% subjects attributed these difficulties to their own health problems; further lack of privacy (8%), spouse's health problems (4%) and conflict with spouse (4%). None considered their sexual difficulty significant enough to demand a thorough clinical assessment.
A study done in Vellore (2009) by Singh et al. found 77.2% in desire domain; arousal 91.3%, lubrication in 96.6% orgasm 86.6% satisfaction 81.2%% and pain in 64.4%. Kalra et al.[22] A study done on elderly both male and female found 72% were sexually active below 60 years and 57% above 60 years. Above 50 years, 56.6% of women had stopped sexual activity due to various reasons when compared to men which was only16.6%.
Functional brain imaging studies BOLD and fMRI had shown healthy women had activation of middle occipital gyrus, middle temporal gyrus, inferior frontal gyrus, insula, hypothalamus, septal area, anterior cingulate gyrus, parahippocampal gyrus, thalamus, and amygdala by erotic visual stimulation. In comparison with the healthy women, the depressive women gave lower activity, especially in the brain regions of the hypothalamus, septal area, anterior cingulate gyrus, and parahippocampal gyrus.[23]
There is a need to explore the sexual functioning of women with depression as one part of sexuality is that it helps in developing intimate emotional and physical relationship to another person and this relationship may serve as a buffer against life stresses.[24,25,26] DSM 5 has included changes in premenstural dysphoric disorder. DSM 5 has suggested subtype of female sexual dysfunction into early onset (life long) and late onset (acquired) and has suggested specification like.
Generalized versus situational
Partner factors (partner's sexual problems, partner's health status)
Relationship factors (e.g. poor communication, relationship discord, discrepancies in desire for sexual activity)
Individual vulnerability factors (e.g. poor body image, history of abuse experience) or psychiatric comorbidity (e.g. depression or anxiety)
Cultural/religious factors (e.g. inhibitions related to prohibitions against sexual activity).
There is also a need to redefine and reconceptualize different components of female sexual dysfunction (desire, arousal, orgasm, vaginismus and pain) as they underlie various aspects of women's sexuality.[27]
MATERIALS AND METHODS
A cross-sectional study was done following institutional ethical committee clearance and written consent from the subjects. They were informed about the survey and were interviewed by lady doctor. Adequate privacy and confidentiality was ensured. Subjects both in study and control group were initially found to be hesitant and shy but once rapport was established they spoke freely about their sexual function. Subjects who were not comfortable were interviewed in subsequent sessions. They reported that no doctor had earlier enquired about their sexuality. It was not a self-reported scale as the dysfunction might had been over reported or under reported. The study group was diagnosed to have depressive disorder (mild, moderate or severe) for a duration of 6 months to 1-year according to ICD 10 criteria by a psychiatrist.
Cases n = 30.
Inclusion criteria
Female patients with untreated depression
Giving written informed consent
Married and completed 18 years
Staying with husband for the past 1-year and sexually active
Completed class 7.
Exclusion criteria
Not giving consent
Staying with husband, but sexually inactive in the past 1-year due to cultural taboo or other reasons
Psychotic symptoms, mental retardation
Husband having male sexual dysfunction.
Control n = 30.
Inclusion criteria
(1) Female relatives or accompanying person who came to the hospital with the patient who had given written consent. (2) Married and above 18 years, staying with husband for the past 1-year and sexually active. (3) Completed class 7.
Exclusion criteria
(1) Not given written consent (2) Associated with medical co-morbidity like HTN, DM or other illness, (3) Sexually inactive in the past 1-year, (4) Husband having sexual dysfunction, (5) Subjects who had overlapped symptoms scored more than 7 HAM D scale.
Tools
Arizona sexual experience scale for female.[33]
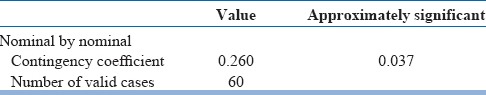
Hamilton Depression Rating Scale (17 item) – used for assessment of depression in study group. Subjects who score more than 7 in control group were excluded. The scoring of HAMD 17 item was applied for assessment.
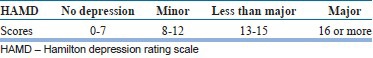
In the study the mean score of HAMD was 19.13 in the population under study.
Female sexual functioning index–has 19 questions with 6 domain-desire (2 questions), arousal (4 questions), lubrication (4 questions), orgasm, satisfaction and pain (3 question each). Evaluates sexual functioning in the past 4 weeks.
Total score below 26.55 denotes sexual dysfunction. Cut off for different domains are as follows.
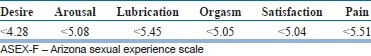
It is a 5 item scale with 5 domain – sex drive, arousal, lubrication, orgasm and satisfaction following orgasm. Evaluates sexual functioning in the past week including the day of interview.
A total ASEX score of ≥19, any one item with a score of ≥5, or any three items with a score of ≥4 would have sexual dysfunction.
RESULTS
After statistical analysis using SPSS for windows software, descriptive statistics and contingency co efficient analysis the following was obtained – ASEX-F was found to be better than FSFI and co-related with HAMD 17 item scale which was further proved by stepwise multiple regression.
P value was considered significant if values are ≤ 0.05.
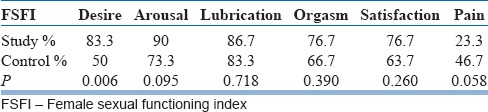
Tables 1 and 2 shows sexual dysfunction was significant with 70% in study group compared to 43.3% in control.
Table 1.
FSFI*group cross tabulation
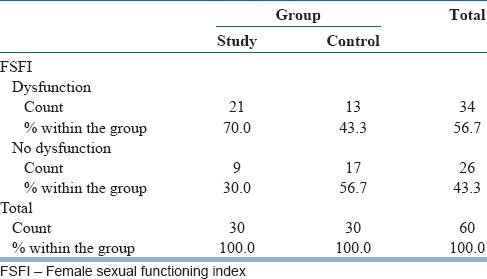
Table 2.
Symmetric measures
The Table 3 shows female sexual dysfunction is not significant in individual domain except desire.
Table 3.
Each domain score
Tables 4 and 5 shows ASEX-F was significant in determining sexual dysfunction 73.3% in study group compared to 20% in control.
Table 4.
ASEX-F
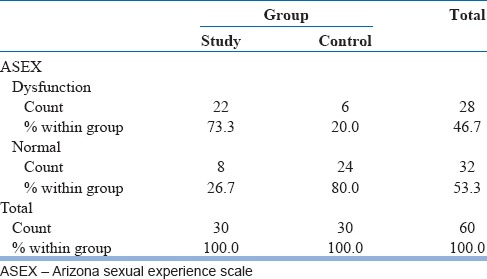
Table 5.
Symmetric measures
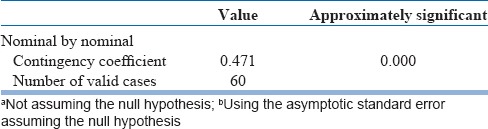
The Table 6 shows significant dysfunction in all domains as compared to control. 43.3% in sex drive, 50% compared to 6% in arousal, 43.3% compared to 6.7% in lubrication, 53.3% compared to 6.7% in orgasm and 56.7% compared to 6.7% in the study group and control group respectively.
Table 6.
Each domain score
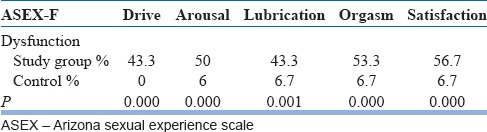
Table 7 shows that although the overall FSFI score did not co-relate with HAMD individual domains desire, lubrication, orgasm and satisfaction were significant [Figure 1].
Table 7.
FSFI to HAMD-crosstabulation in sexual dysfunction in the study group
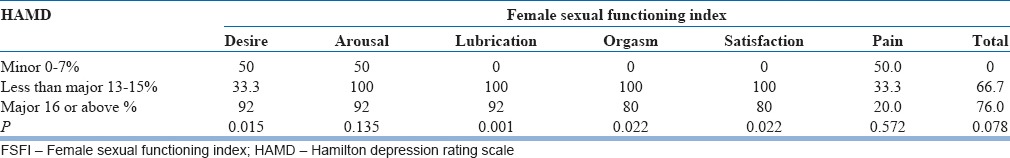
Figure 1.
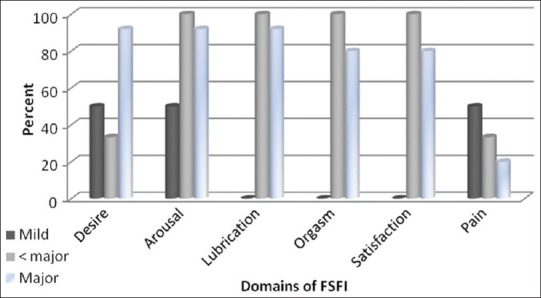
Depiction of dysfunction in various domains of FSFI
Table 8 shows correlation of HAMD and various domain and total ASEX-F % in the study group. Overall scores were significant as well as arousal, orgasm and satisfaction were significant.
Table 8.
ASEX-F to HAMD
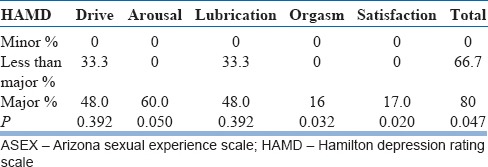
Comparing both FSFI and ASEX-F with HAMD significant impairment was found in orgasm and satisfaction co-relating with HAMD scale.
Sociodemographic pattern
Age
Age was divided into four subgroups
18-25
26-35
36-45 and 45 + years.
The age group was cross-matched with cases and control [Table 9].
Table 9.
Socio demographic pattern of case and control group
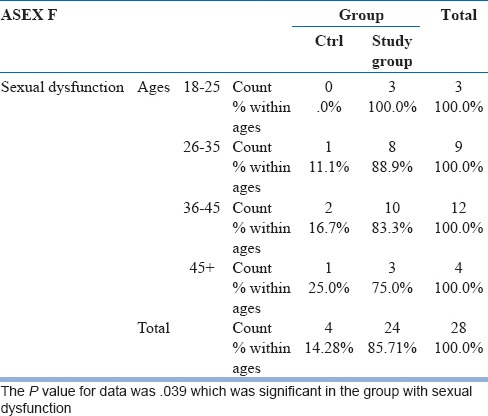
The study group data suggested early onset of sexual dysfunction in the domain of drive, arousal and satisfaction in 18-25 years group on the setting of depression compared to the control. The sex drive domain was 100% in study population to 0.0% in control group. In the study group difficulty in lubrication and orgasm started at earlier age group (26-35 years) as compared to control.
Education
Both the study group and control were class VII completed. No significant pattern found in co-relation to education.
Demographic data
About 60% were from urban background in the study group and approximately 73% in the control group no significant correlation between the pattern of dysfunction was found.
No relation was found in terms of sexual dysfunction to education, demography and foreplay (hug, kiss, touch) prior to sexual intercourse between the cases and controls. Although 6 in the study group reported that they wanted their husbands to do foreplay prior to intercourse.
DISCUSSION
This study was done on 60 female subjects to find the prevalence and symptom profile pertaining to sexual dysfunction in drug naive depression. The study showed that there was a high prevalence 70% in study group compared to 43.3% in the control group according to FSFI scale and 73.3% in study group compared to 20% in control according to ASEX-F group scores overall. Age matched control group showed (18-25) years 100%, (26-35) years 88.9%, (36-45) years 83.3%, 45 years and above 25% in cases compared to 0.0%, 11.1%, 16.7%, and 14.28% in controls respectively considering the overall score in ASEX-F. The study showed that though age did not have much significance in the individual domain between the study and the control group, there was an early age of onset of female sexual dysfunction in women with depression when compared to the control, and the dysfunction started as early as 18 years of age in study group compared to the control.
Two subjects with depression reported that although they loved their husbands emotionally, during the present episode of depression they were filled with rage when their husbands touched them. This hampered their sexual functioning, acted as a vicious cycle for interpersonal conflict and further increased their depression. One subject in the control group aged 55 years reported that though she had a desire she was not performing sexual relation from the past 8 years as advised by an astrologer for the well-being of her son. These three subjects were dropped out of the study as they did not fulfill the inclusion criteria. One subject, government employee, 55 years reported that she hardly made love with husband although she had a desire as she had to share a room with her grand-children which was one of the causes of depression. Some subjects with depression were excluded from the study reported of no sexual activity due to old age, children grown older, lack of privacy or husband's infidelity. There were also the unavailability of doors with lock in 12 couples’ bedroom (8 in cases and 4 in the control group) which inhibited their normal sexual functioning.
Fore-play prior to sexual intercourse was also very minimal in these population-6 in the study group and 10 in the control group. 12 of the study group and 7 of the control group did not have a separate bedroom with lock.
In the study group one subject with rheumatoid arthritis (RA+) married for 2 years on medication had less sexual dysfunction (score in FSFI – 21.8, ASEX-17, HAMD 16) One subject with hypothyroidism and one with diabetes mellitus had dysfunction in most of the domains, although their illnesses were controlled by medication. 3 in cases and 1 in control were postmenopausal. They had increased score in pain domain (3.6-4.8 in FSFI and 5 in ASEX-F).
The subjects were inhibited to report of their sexual dysfunction. However, on considerate enquiring they reported they wanted improvement in this area of functioning for the well-being of self and family.
Limitation
The sample size was small. However, with small sample we had compared the cases and the control and used observer-rater scale. Sexual functioning in relation to mood changes during menstrual cycle was not taken into account.
CONCLUSION
Our study found that there was a severe sexual dysfunction of sexual activity in depression in all domains of female sexual cycle. The study showed sexual dysfunction was 73.3% in study with ASEX-F compared to 20% in control and 70% in study to 43.3% in control group according to FSFI. The study found that there was an early age of onset of sexual dysfunction 18-25 years on the setting of depression. ASEX-F was found a better tool than FSFI in determining the female sexual dysfunction in depression. It also co-related with HAMD for depression. Sexual dysfunction was found very high with HAM D score of 16 and above (76% in FSFI and 80% in ASEX-F). On taking into account all three scales HAMD, FSFI and ASEX-F significant dysfunction was found in orgasm and satisfaction domain of female sexual dysfunction with depression. The study found women with difficulty in sexual functioning in the areas of drive, arousal, lubrication, orgasm, satisfaction and pain both in cases and control when enquired upon in a reassuring manner. Hence, every doctor should dutifully and empathetically assess the female sexual needs and functions ensuring privacy and confidentiality using rating scales which can aid in treatment and drug selection. If asked, assessed and addressed regularly, women will feel less hesitant and report more freely.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Geneva: World Health Organization; 1992. The ICD 10 Classification of Mental and Behavioural Disorders. F32 Depressive Episode; pp. 119–20. [Google Scholar]
- 2.Maier W, Gänsicke M, Gater R, Rezaki M, Tiemens B, Urzúa RF. Gender differences in the prevalence of depression: A survey in primary care. J Affect Disord. 1999;53:241–52. doi: 10.1016/s0165-0327(98)00131-1. [DOI] [PubMed] [Google Scholar]
- 3.Derogatis LR, Burnett AL. The epidemiology of sexual dysfunctions. J Sex Med. 2008;5:289–300. doi: 10.1111/j.1743-6109.2007.00668.x. [DOI] [PubMed] [Google Scholar]
- 4.Geneva: WHO Basic Documents; 1948. World Health Organization. Constitution of the World Health Organization. [Google Scholar]
- 5.Lewis RW, Fugl-Meyer K, Bosch R, Fugl-Meyer AL, Lauman EO, Lizz E, Marti-Morales A. Epidemiology:Risk factors for sexual dysfunction. J Sex Med. 2004;1:35–9. doi: 10.1111/j.1743-6109.2004.10106.x. [DOI] [PubMed] [Google Scholar]
- 6.Phillips NA. Female Sexual Dysfunction: Evaluation and Treatment. Am Fam Physician. 2000;62:127–36. [PubMed] [Google Scholar]
- 7.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: Prevalence and predictors. JAMA. 1999;281:537–44. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 8.Ponholzer A, Roehlich M, Racz U, Temml C, Madersbacher S. Female sexual dysfunction in a healthy Austrian cohort: Prevalence and risk factors. Eur Urol. 2005;47:366–74. doi: 10.1016/j.eururo.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Derogatis LR, Rust J, Golombok S, Bouchard C, Nachtigall L, Rodenberg C. Validation of the Profile of Female Sexual Function (PFSF) in surgically and naturally menopausal women. J Sex Marital Ther. 2004;30:25–36. doi: 10.1080/00926230490247183. [DOI] [PubMed] [Google Scholar]
- 10.Derogatis LR, Rust J, Golombok S, Kuznicki J, Rodenberg C, Horney Mc. Atlanta: International Society for the Study of Women's Sexual Health; 2004. A patient-generated multi-national inventory to measure distress associated with low desire. Proceedings of the Annual Meeting of the International Society for the Study of Women's Sexual Health; p. 206. [Google Scholar]
- 11.Dennerstein L, Koochaki P, Barton I, Graziottin A. Hypoactive sexual desire disorder in menopausal women: A survey of western European women. J Sex Med. 2006;3:212–22. doi: 10.1111/j.1743-6109.2006.00215.x. [DOI] [PubMed] [Google Scholar]
- 12.Fugl-Meyer AL, Fugl-Meyer K. Sexual disabilities, problems and satisfaction in 18–74 year old Swedes. Scand J Sexol. 1999;2:79–105. [Google Scholar]
- 13.Bancroft J, Loftus J, Long JS. Distress about sex: A national survey of women in heterosexual relationships. Arch Sex Behav. 2003;32:193–208. doi: 10.1023/a:1023420431760. [DOI] [PubMed] [Google Scholar]
- 14.Hayes RD, Dennerstein L, Bennett CM, Koochaki PE, Leiblum SR, Graziottin A. Relationship between hypoactive sexual desire disorder and aging. Fertil Steril. 2007;87:107–12. doi: 10.1016/j.fertnstert.2006.05.071. [DOI] [PubMed] [Google Scholar]
- 15.Graziottin A. Prevalence and evaluation of sexual health problems – HSDD in Europe. J Sex Med. 2007;4(Suppl 3):211–9. doi: 10.1111/j.1743-6109.2007.00447.x. [DOI] [PubMed] [Google Scholar]
- 16.Bonierbale M, Jean T. The ELIXIR study: evaluation of sexual dysfunction in 4557 depressed patients in France. Current Medical Research and Opinion. 2003;19:114–24. doi: 10.1185/030079902125001461. [DOI] [PubMed] [Google Scholar]
- 17.Frank JE, Mistretta P, Will J. Diagnosis and Treatment of Female Sexual Dysfunction. Am Fam Physician. 2008;77:635–42. [PubMed] [Google Scholar]
- 18.Prakash O, Rao TS. Sexuality research in India: An update. Indian J Psychiatry. 2010;52:S260–3. doi: 10.4103/0019-5545.69243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Avasthi A, Kaur R, Prakash O, Banerjee A, Kumar L, Kulhara P. Sexual behavior of married young women: A preliminary study from north India. Indian J Community Med. 2008;33:163–7. doi: 10.4103/0970-0218.39677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh JC, Tharyan P, Kekre NS, Singh G, Gopalakrishnan G. Prevalence and risk factors for female sexual dysfunction in women attending a medical clinic in south India. J Postgrad Med. 2009;55:113–20. doi: 10.4103/0022-3859.52842. [DOI] [PubMed] [Google Scholar]
- 21.Kar N, Koola MM. A pilot survey of sexual functioning and preferences in a sample of English speaking adults from a small South Indian town. J Sex Med. 2007;4:1254–61. doi: 10.1111/j.1743-6109.2007.00543.x. [DOI] [PubMed] [Google Scholar]
- 22.Kalra G, Subramanyam A, Pinto C. Sexuality: Desire, activity and intimacy in the elderly. Indian J Psychiatry. 2011;53:300–6. doi: 10.4103/0019-5545.91902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang JC, Park K, Eun SJ, Lee MS. Assessment of Cerebrocortical Areas Associated with Sexual Arousal in Depressive Women Using Functional MR Imaging. The Journal of Sexual Medicine. 2008;5:602–9. doi: 10.1111/j.1743-6109.2007.00737.x. [DOI] [PubMed] [Google Scholar]
- 24.Laumann EO, Gagnon JH, Michael RT, Michael S. Chicago: University of Chicago Press; 1994. The Social Organization of Sexuality: Sexual Practices in the United States. [Google Scholar]
- 25.Lauman EO, Paik A, Rosen RC. Sexual dysfunction in the United States; prevalence and predictors. JAMA. 1999;281:19–34. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 26.Segraves RT. Female sexual disorders: Psychiatric aspects. Can J Psychiatry. 2002;47:419–25. doi: 10.1177/070674370204700502. [DOI] [PubMed] [Google Scholar]
- 27.Basson R, Leiblum S, Brotto L, Derogatis L, Fourcroy J, Fugl-Meyer K, et al. Definitions of women's sexual dysfunction reconsidered: advocating expansion and revision. J Psychosom Obstet Gynaecol. 2003;24:221–9. doi: 10.3109/01674820309074686. [DOI] [PubMed] [Google Scholar]
- 28.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamilton M. Development of a rating scale for primary depressive illness. Br J Clin Psychol. 1967;4:561–71. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 30.Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): A multidimensional self report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 31.Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): Cross validation and development of clinical cutoff scores. J Sex Marital Ther. 2005;31:1–20. doi: 10.1080/00926230590475206. [DOI] [PubMed] [Google Scholar]
- 32.Meston CM. Validation of the Female Sexual Function Index (FSFI) in women with female orgasmic disorder and in women with hypoactive sexual desire disorder. J Sex Marital Ther. 2003;29:39–46. doi: 10.1080/713847100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McGahuey CA, Gelenberg AJ, Laukes CA, Moreno FA, Delgado PL, McKnight KM, et al. The Arizona Sexual Experience Scale (ASEX): Reliability and validity. J Sex Marital Ther. 2000;26:25–40. doi: 10.1080/009262300278623. [DOI] [PubMed] [Google Scholar]


