Abstract
Objective:
to analyze and summarize knowledge concerning critical components of interventions that have been proposed and implemented by nurses with the aim of optimizing self-care by heart failure patients.
Methods:
PubMed and CINAHL were the electronic databases used to search full peer-reviewed papers, presenting descriptions of nursing interventions directed to patients or to patients and their families and designed to optimize self-care. Forty-two studies were included in the final sample (n=4,799 patients).
Results:
this review pointed to a variety and complexity of nursing interventions. As self-care encompasses several behaviors, interventions targeted an average of 3.6 behaviors. Educational/counselling activities were combined or not with cognitive behavioral strategies, but only about half of the studies used a theoretical background to guide interventions. Clinical assessment and management were frequently associated with self-care interventions, which varied in number of sessions (1 to 30); length of follow-up (2 weeks to 12 months) and endpoints.
Conclusions:
these findings may be useful to inform nurses about further research in self-care interventions in order to propose the comparison of different modalities of intervention, the use of theoretical background and the establishment of endpoints to evaluate their effectiveness.
Descriptors: Heart Failure, Self-Care, Nursing, Intervention, Review
Introduction
The context of heart failure (HF) exemplifies par excellence the critical role that nurses have to play in meeting health and social care challenges facing an aging population and an important increase in the prevalence of chronic diseases 1. HF is a global phenomenon. Nearly 6.5 million people in Europe, 5 million people in the USA and 2.4 million people in Japan currently suffer from heart failure (HF) and one million new cases are diagnosed every year worldwide. In Latin America, decompensated HF is the main cause of cardiovascular hospitalization. Indeed, Latin America is under the paradox of having the HF risk factors and HF epidemiology of developed countries with the added factors of Chagas Disease and rheumatic fever 2. Threequarters of all patients hospitalized for the first time with HF will die within 5 years, making its survival rate comparable to that of cancer 3. The syndrome has also a high prevalence of comorbidities and multiple chronic conditions 4, making these HF patients very complex, with a high risk of decompensation and frequent hospital admissions. Among patients aged 65 years or older, HF is the most frequent cause of hospitalization, and hospital care accounts for 65-75% of the expenditure on HF 5.
Continuous clinical follow-up of HF patients is recognized as a class 1 recommendation in the recent guideline for the management of HF 4and successful patient self-care is one of the strategies highlighted as imperative within their plan of care. According to the Self-care of Heart Failure Model 6, self-care is defined as "a naturalistic decision-making process involving the choice of behaviors that maintain physiologic stability (maintenance) and the response to symptoms when they occur (management)". Self-care encompasses a range of health-related behaviors and is influenced by several individual, social and environmental factors 7. Thus, the development of nursing interventions, targeting the patient's needs, demands careful planning (including an accurate evaluation of the needs), the choice for the best approach and0 a rigorous evaluation of its effectiveness in optimizing the practice of self-care and its translation into clinical outcomes.
A recent integrative review on self-care in HF aimed at identifying successfully implemented nursing interventions included only studies with experimental design 7, considering that the randomized controlled trial (RCT) is the gold standard for research into the effects of interventions. Despite the importance of such results, this review did not represent all nursing interventions that have been proposed in this context. Therefore, the purpose of the present study was to conduct a broader integrative review aimed at identifying the critical components of interventions that have been proposed and implemented by nurses with the aim of at optimizing self-care by HF patients. Finally, we intended to further refine propositions for research and clinical practice.
Methods
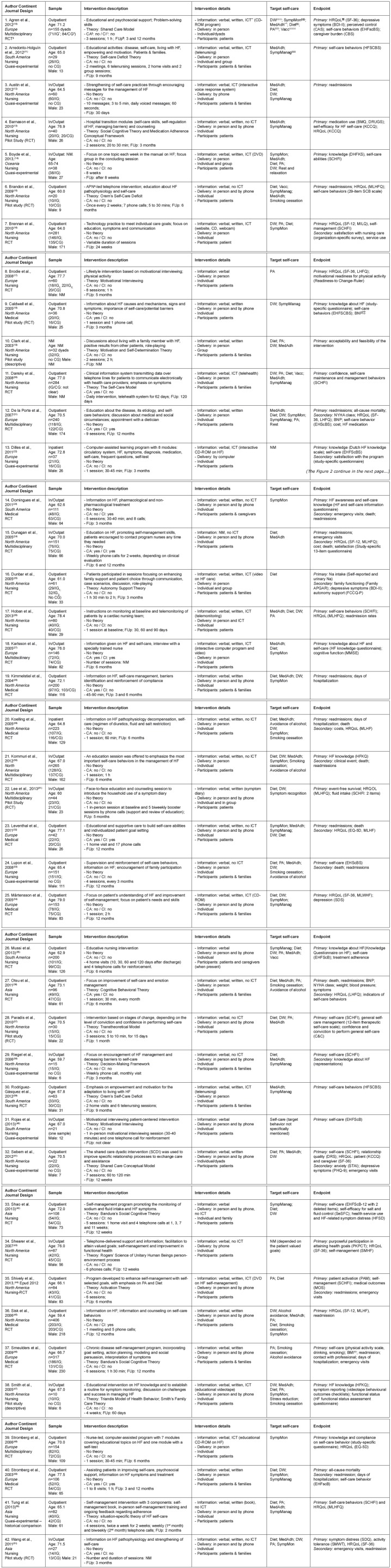
The steps for the integrative review used in this study were: problem identification (question formulation), literature search, data evaluation, data analysis and reporting 8. For question formulation in the first step, we were inspired by the PICO strategy, defining population as "HF patients" and intervention as "nursing intervention aimed at promoting self-care". The comparison criterion was not applied and outcome was analyzed in an exploratory perspective. Step 1 - Problem identification: the central question of this integrative review was: "What are the main attributes of nursing interventions that have been described to optimize self-care behaviors among HF patients?" The aspects analyzed were: comprehensiveness of the intervention; nature of the intervention (educational only or including clinical assessments/interventions); if they were theory-based; how they were applied (e.g., individually/in group; in person/by phone); who was the target population (patients only or patients and families/ caregivers); the targeted self-care behaviors and the primary and secondary endpoints used to evaluate the intervention. Step 2 - Literature search: an extensive electronic search of literature was conducted in the databases PubMed and Cumulative Index of Nursing and Allied Health Literature (CINAHL), from January 1, 2001 to December 31, 2013. The following key words were used: Heart Failure AND Self-Care AND Nursing Intervention. MeSH (Medical Subject Heading) Major Topics were used for the research in PubMed. Studies included met the following criteria: full peer-reviewed papers, describing experimental, quasi-experimental, descriptive and pilot studies that should necessarily present a clear proposition or implementation of a nursing intervention aimed at optimizing self-care, targeting patients or patients and families. Papers should be written in English, French, Spanish or Portuguese. Only published papers were considered. Reviews and dissertations or unpublished papers were not included(8-9). Step 3 - Data evaluation: 97 studies were found in PubMed and 45 in CINAHL. First, duplicate articles were discarded. Subsequently, title and abstracts were reviewed for content. Five independent reviewers validated the process of evaluation and retention of the studies. Finally, 42 studies were included in the review. For details, see the flowchart ( Figure 1).
Figure 1. Flowchart of the methodological steps undertaken in the integrative review.
Step 4 - Data analysis: a research instrument was developed for data extraction and analysis from the included studies. The instrument comprised the following items: (1) Data regarding article information; (2) Characteristics of the sample (outpatient/inpatient, age, sample size, gender); (3) Study design; (4) Intervention description (educational activity, theoretical background, clinical assessment/intervention; intervention dose and length of follow-up); (5) Strategy for intervention delivery (verbal/written/use of information and communication technology, in person/by phone, individual/group, patient/ dyad); (6) Targeted self-care behaviors; (7) Endpoints. This step was performed by four reviewers divided into two independent groups and revised by a fifth reviewer.
Results
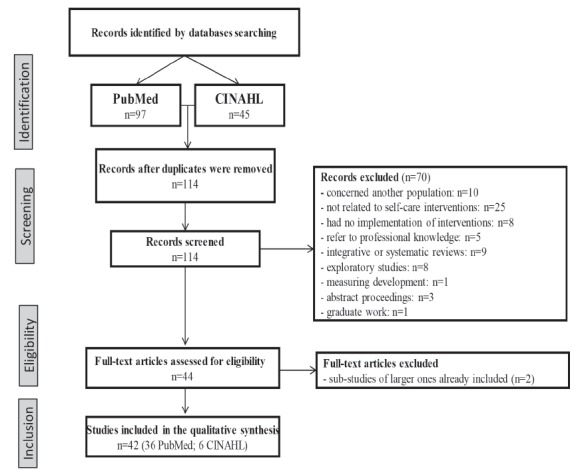
The reviewed articles were mostly published in nursing journals (64.3%). Medical and multidisciplinary journals accounted for 19.0% and 16.7% of the studies, respectively. The number of publications was distributed throughout the years, with a slight concentration in 2005 and 2012 (16.7% and 19.0%). North America was the continent with the greatest number of articles (50.0%), followed by Europe (26.2%); South America (11.9%); Asia (9.5%) and Oceania (2.4%). The 42 articles included a total of 4,799 patients, with sample sizes varying from 10 to 406 patients. Patients were in average 68.6 years old and mostly male (61.9%). In the 22 studies reporting New York Heart Association (NYHA) Functional Class specifically (n=2,562), it varied from I up to IV, but the majority of patients were in Class II (36.6%) or III (45.6%). Concerning the moment of transition, 26 studies targeted patients during their clinical followup, 2 studies targeted hospitalized patients, 13 studies targeted patients in the transition from hospital to home and 1 study did not mention it clearly. Most of the reviewed studies (31/42) adopted RCT design, but from those, 6 were pilot studies with small samples. The studies analyzed are summarized in Figure 2.
Figure 2. Síntesis de los artículos revisados.
* GI: grupo de intervención; † GC: grupo de control; ‡ ECA: ensayo clínico controlado aleatorio; § AC: evaluación clínica; ‖ IC: intervención clínica; ¶ FUp: seguimiento ( follow-up); ** TIC: tecnología de la información y comunicación; †† IMC: Índice de Masa Corporal; BNP: péptido natriurético tipo-B; §§ Dieta: restricción de sal y líquidos; ‖‖‖ PD: peso diario; ¶¶ CVRS: Calidad de Vida relacionada a la Salud; *** MedAdh: Adherencia a la medicación; ††† AF: Actividad física; ‡‡‡ GestSint: Gestión de síntomas; §§§ MonSint: Monitoreo de síntomas; ‖‖‖‖ Vac: vacunación.
Target participants: The majority of the studies targeted patients only (26/42), but 16 studies were centered also on the family or caregiver.
Target self-care: In general, studies targeted between 3 and 4 self-care behaviors (mean = 3.6; median = 4 behaviors). The behaviors most frequently targeted in descending order were diet(reduction of salt intake alone or associated with fluid restriction and/or healthy eating) mentioned in 31/42 studies; adherence to medication, in 27/42; daily weight (25/42); physical activity (19/42) as well as monitoring (17/42) and management (14/42) of signs and symptoms of HF decompensation. Less targeted behaviors were smoking (8/42) and alcohol cessation (6/42); vaccination (4/42) and stress control/relaxation (2/42).
Intervention activities: All the studies included educational/counselling activities in their interventions. In 14 studies, interventions used cognitive behavioral strategies: mastering the management of self-care behaviors, discussions and exchanges of experiences with self-care behaviors, action planning, modeling and social persuasion, awareness of physical and emotional states, motivational interviewing or empowerment and managing barriers. Finally, 10 studies mentioned a combination of information and cognitive behavioral strategies. In 18 studies, educational interventions were mostly based on information about the cardiovascular system, the HF pathophysiology, symptoms and treatment as well as expected self-care behaviors.
Theoretical background: The majority of the 18 studies focused on information did not use theoretical background to guide their intervention. Only two studies based on information mentioned the use of theoretical background, and the Self-Care Model and Orem's Self-Care Theory were used to define the concepts under study. As a rule, the 14 studies using cognitive behavioral strategies were based on a theoretical background. The models used were Activation Theory; Motivation and Self-Determination
Theory; Transtheoretical Model; Bandura's Social Cognitive Theory; Self-Determination Theory; Cognitive Behavior Theory; Orem's Self-Care Deficit Theory; Shared Care Conceptual Model; Motivational Interviewing; situation-specific theory of HF and Decision-Making Framework. Only one study did not use theoretical background for the intervention centered on behavior change. Among the 10 studies whose interventions included both information and changing behavior strategies, five used theories to guide the intervention: Rogers' Science of Unitary Human Being's Process; the Self-Care Deficit Theory; the Shared Care Model; the Autonomy Support Theory and the Triandis Model. Four studies did not use any theoretical background.
Type of intervention delivery: All studies used verbal information in their interventions. Twentyeight of them also used written information and 15 used information and communication technologies (ICT). Among ICT, the main tools were CD-ROM, DVD and video, alone or in combination. Fifty-four studies mentioned the use of telehealth or telenursing, and one study developed a website. Interventions were delivered individually (35/42), in group (2/42) or combining individual and group meetings (5/42). The majority of the interventions were delivered in person (39/42). From those, 19 combined in-person interventions with telephone calls. Two studies used only telephone calls and one used only CD-ROM to deliver the intervention.
Dose of intervention: The number of sessions to deliver the intervention varied from one to 30, with a mean of 5.6 sessions, but five articles did not clearly mention it. The duration of the sessions varied between five to 120 minutes, with a mean of 61.7 minutes, but again, 22 articles did not report this information. Finally, the duration of the followup ranged from 2 weeks up to 12 months, with an average of 5.8 months. Two studies were not clear about the length of the follow-up.
Inclusion of clinical assessment and intervention: In 12 studies, educational interventions were provided along with the clinical assessment of the patient, using anamnesis associated or not to physical examination (heart and lung auscultation and inspection of edema). In seven of these studies, the clinical evaluation was followed by therapeutic optimization, with management of the medication by the nurses involved in the study according to preestablished protocols and/or by referring to the cardiologist.
Endpoints: All studies established primary endpoints, with an average of 1.8 criteria (median=2). Self-care measures were the most frequent primary endpoints, measured in 57% of the studies (24/42). Different measures of self-care were used: self-care scales (19/24) or specific measures of the targeted behavior (5/24). Other primary endpoints were: readmissions (12/42); health-related quality of life (13/42); other psychosocial measures related to the strategies of intervention (10/42) and knowledge (9/42). The primary endpoints less frequently used were: clinical data regarding signs of decompensation/stabilization of HF (6/42), mortality (5/42), hospital days (3/42) and visits to the emergency department (2/42). Acceptability/feasibility was evaluated in one out of six pilot studies. Under half of the studies (18/42) used secondary endpoints. For those studies, in average 2.1 criteria were used (median=2). Secondary admission (6/18), HRQoL (6/18), visits to emergency departments (5/18), psychosocial variables (5/18), cost (2/18), knowledge (1/18), hospital days (1/18) and clinical data (1/18) were the criteria assessed.
Discussion
In this review, we aimed at evaluating the main features of the interventions implemented by nurses to promote self-care among HF patients. Our results confirmed the variety and the complexity of the interventions that have been proposed.
All the studies were founded on educational/ counselling activities and it is noteworthy that a significant number of interventions were based only on information. It is widely recognized that, despite the importance of knowledge about the health-related condition, it is not sufficient to help individuals change their behaviors. Moreover, the majority of the studies based only on information had not used theoretical background guiding the content and the strategy of educational intervention as well as the rational used to evaluate its results. The use of theoretical backgrounds is important to understand results and how inventions worked, enabling further improvements in the effectiveness of behavioral interventions 52.
In 28% of the studies, self-care interventions were combined with clinical assessment and therapeutic optimization, which is a troubling point for the evaluation of the effectiveness of self-care behaviors by themselves on clinical outcomes. The development and application of clear protocols as well the evaluation of the degree of adherence to each of them is essential to build a theoretical understanding of the process of change 53.
Self-care is defined as a set of health-related behaviors that can be divided in maintenance, monitoring and managing behaviors 6. Thus, interventions are anyhow often complex because more than one behavior is targeted. Behaviors contributing to the stability of the clinical profile, the maintenance behaviors diet, medication and physical activity, were the most frequently targeted, along with the monitoring behaviors of daily weight and observation of signs and symptoms of HF decompensation. Management behaviors are far less targeted in interventions.
Regarding the strategies used to deliver the intervention, it is important to note the frequent use of phone calls as well as ICT. These strategies may result in an increased accessibility to interventions, considering mainly the impaired and fragile health condition of HF patients. Research is needed to demonstrate the added value of such strategies. However, it is important to note that important information regarding intervention dose and length of follow-up were not mentioned in seven studies, while the duration of intervention sessions was not mentioned in 22. Studies on nursing interventions need to describe this information carefully, permitting further replication or comparison.
Interventions targeted patients or patients & families, individually or in group. Interventional strategies involving social referents are increasing in nursing studies, based on the assumption of the importance of social referents for the support of change and maintenance of health-related behaviors. Further studies must be done in order to explore if the inclusion of the caregivers optimizes the results of the intervention in this context. The demonstration of the cost-benefit ratio of this approach (considering the effectiveness of the intervention in terms of social and physical functioning and wellness) would be important, considering that the inclusion of dyads could result in more complex study design and higher costs.
Regarding the outcomes, all the studies established primary endpoints, and about half of them, secondary ones. Surprisingly, self-care was the primary endpoint of only 50% of them. Because behavior change is the aim of the interventions, behavior should always be the primary outcome 54. Clinical outcomes as endpoints are also important, because behavioral changes are intended to ameliorate the clinical profile. However, it is possible that interventions do not succeed in changing behavior and, even when they do, there are many reasons why they may be effective in achieving the desired behavior change but do not translate into desired clinical outcomes 55. Thus, the use of clinical endpoints only seems to be inadequate in this context. As complex interventions, it is interesting to consider their process of evaluation as having several distinct phases 55. The first phase must be the evaluation of behavioral change, and then the impact of self-care behavior changes on clinical or psychosocial outcomes.
Moreover, it is important to mention the difficulties in recruiting emotionally and physically vulnerable, life-limited participants such as those with HF in research activities 56. Usually, HF patients are older, presenting a number of comorbidities as well cognitive deficits. The attrition in the follow-up is considerable for many reasons: HF decompensation, readmissions, fatigue and death. This is even more important when considering patients in more advanced HF stages. As documented in this review, studies frequently recruit mostly patients in the NYHA Functional Classes II or III, not including those in Class IV. It means that this fragile part of the population of HF patients has not been addressed by self-care studies. The development of strategies is critical for people with advanced HF to have greater opportunity to participate in research that enables adequate service provision and development 56.
HF is a global phenomenon affecting people worldwide, and research in this setting must consider social, economic and cultural contexts. Nevertheless, the retrieved papers in this review pointed out that North America concentrates half the publication on nursing interventions about self-care in HF, followed by Europe. Countries in development that are increasingly susceptible to chronic non-communicable diseases have a small expression in the international literature, pointing to need of promoting research in these contexts. International literature is important to inspire interventions, but it does not necessarily mean that the interventions tested elsewhere will be effective in a certain culture. Research is needed to prove it. And the comparisons of the results among cultures could bring important insights to the understanding of the self-care phenomena.
Conclusions
Our results show that the nursing interventions proposed are diverse and complex. All of them are educational in nature but the use of cognitivebehavioral strategies was not considered in more than half of the studies, as well as the use of a theoretical background to guide the intervention. Most of the interventions were designed for patients only, and the targeted self-care behaviors varied largely, the most frequently targeted being those contributing to the stability of the clinical profile, the maintenance behaviors. Regarding the endpoints used to evaluate the effectiveness of the intervention, about 50% of the studies used only one measure of self-care. Our findings may be useful to inform nurses about further research in self-care interventions in order to propose the comparison of different intervention modalities, the use of theoretical background and the establishment of endpoints to evaluate their effectiveness.
Footnotes
Supported by Réseau de recherche en interventions en sciences infirmières du Québec (RRISIQ), Canada.
References
- 1.Richards DA, Borglin G. Complex interventions and nursing looking through a new lens at nursing research. International journal of nursing studies. 2011;48(5):531–533. doi: 10.1016/j.ijnurstu.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 2.Bocchi EA, Arias A, Verdejo H, Diez M, Gómez E, Castro P. The reality of heart failure in Latin America. J Am Coll Cardiol. 2013;62(11):949–958. doi: 10.1016/j.jacc.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 3.McMurray John JV, Stewart S. The burden of heart failure. European Heart Journal Supplements. 2002;4(D):D50–DD8. [Google Scholar]
- 4.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH. 2013 ACCF/AHA guideline for the management of heart failure a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147–e239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 5.Mejhert M, Kahan T, Persson H, Edner M. Predicting readmissions and cardiovascular events in heart failure patients. Int J Cardiol. 2006;109(1):108–113. doi: 10.1016/j.ijcard.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 6.Riegel B, Jaarsma T, Strömberg A. A middle-range theory of self-care of chronic illness. ANS Adv Nurs Sci. 2012;35(3):194–204. doi: 10.1097/ANS.0b013e318261b1ba. [DOI] [PubMed] [Google Scholar]
- 7.Barnason S, Zimmerman L, Young L. An integrative review of interventions promoting self-care of patients with heart failure. J Clin Nurs. 2012;21(34):448–475. doi: 10.1111/j.1365-2702.2011.03907.x. [DOI] [PubMed] [Google Scholar]
- 8.Whittemore R, Knafl K. The integrative review updated methodology. J Adv Nurs. 2005;52(5):546–553. doi: 10.1111/j.1365-2648.2005.03621.x. [DOI] [PubMed] [Google Scholar]
- 9.Whittemore R. Analysis of integration in nursing science and practice. J Nurs Scholarsh. 2005;37(3):261–267. doi: 10.1111/j.1547-5069.2005.00045.x. [DOI] [PubMed] [Google Scholar]
- 10.Ågren S, Evangelista LS, Hjelm C, Strömberg A. Dyads affected by chronic heart failure a randomized study evaluating effects of education and psychosocial support to patients with heart failure and their partners. J Card Fail. 2012;18(5):359–366. doi: 10.1016/j.cardfail.2012.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arredondo-Holguín E, Rodríguez-Gázquez MÁ, Higuita-Urrego L. Improvement of self-care behaviors after a nursing educational intervention with patients with heart failure. Invest Educ Enferm. 2012;30(2):188–197. [Google Scholar]
- 12.Austin LS, Landis CO, Hanger KH. Extending the continuum of care in congestive heart failure an interactive technology self-management solution. J Nurs Adm. 2012;42(9):442–446. doi: 10.1097/NNA.0b013e3182668342. [DOI] [PubMed] [Google Scholar]
- 13.Barnason S, Zimmerman L, Hertzog M, Schulz P. Pilot testing of a medication self-management transition intervention for heart failure patients. West J Nurs Res. 2010;32(7):849–870. doi: 10.1177/0193945910371216. [DOI] [PubMed] [Google Scholar]
- 14.Boyde M, Song S, Peters R, Turner C, Thompson DR, Stewart S. Pilot testing of a self-care education intervention for patients with heart failure. Eur J Cardiovasc Nurs. 2013;12(1):39–46. doi: 10.1177/1474515111430881. [DOI] [PubMed] [Google Scholar]
- 15.Brandon AF, Schuessler JB, Ellison KJ, Lazenby RB. The effects of an advanced practice nurse led telephone intervention on outcomes of patients with heart failure. Appl Nurs Res. 2009;22(4):e1–e7. doi: 10.1016/j.apnr.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Brennan PF, Casper GR, Burke LJ, Johnson KA, Brown R, Valdez RS. Technology-enhanced practice for patients with chronic cardiac disease home implementation and evaluation. Heart Lung. 2010;39(6 Suppl):S34–S46. doi: 10.1016/j.hrtlng.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brodie DA, Inoue A, Shaw DG. Motivational interviewing to change quality of life for people with chronic heart failure a randomised controlled trial. Int J Nurs Stud. 2008;45(4):489–500. doi: 10.1016/j.ijnurstu.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 18.Caldwell MA, Peters KJ, Dracup KA. A simplified education program improves knowledge, self-care behavior, and disease severity in heart failure patients in rural settings. Am Heart J. 2005;150(5):983–983. doi: 10.1016/j.ahj.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Clark PC, Dunbar SB. Family partnership intervention a guide for a family approach to care of patients with heart failure. AACN Clin Issues. 2003;14(4):467–476. doi: 10.1097/00044067-200311000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Dansky KH, Vasey J, Bowles K. Use of telehealth by older adults to manage heart failure. Res Gerontol Nurs. 2008;1(1):25–32. doi: 10.3928/19404921-20080101-01. [DOI] [PubMed] [Google Scholar]
- 21.de la Porte PW.Lok DJ.van Veldhuisen DJ.van Wijngaarden J.Cornel JH.Zuithoff NP Added value of a physician-and-nurse-directed heart failure clinic results from the Deventer-Alkmaar heart failure study. Heart. 2007;93(7):819–825. doi: 10.1136/hrt.2006.095810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dilles A, Heymans V, Martin S, Droogné W, Denhaerynck K, De Geest S. Comparison of a computer assisted learning program to standard education tools in hospitalized heart failure patients. Eur J Cardiovasc Nurs. 2011;10(3):187–193. doi: 10.1016/j.ejcnurse.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Domingues FB, Clausell N, Aliti GB, Dominguez DR, Rabelo ER. Education and telephone monitoring by nurses of patients with heart failure randomized clinical trial. Arq Bras Cardiol. 2011;96(3):233–239. doi: 10.1590/s0066-782x2011005000014. [DOI] [PubMed] [Google Scholar]
- 24.Dunagan WC, Littenberg B, Ewald GA, Jones CA, Emery VB, Waterman BM. Randomized trial of a nurse-administered, telephone-based disease management program for patients with heart failure. J Card Fail. 2005;11(5):358–365. doi: 10.1016/j.cardfail.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 25.Dunbar SB, Clark PC, Deaton C, Smith AL, De AK. O'Brien MC Family education and support interventions in heart failure a pilot study. Nurs Res. 2005;54(3):158–166. doi: 10.1097/00006199-200505000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Hoban MB, Fedor M, Reeder S, Chernick M. The effect of telemonitoring at home on quality of life and self-care behaviors of patients with heart failure. Home Healthc Nurse. 2013;31(7):368–377. doi: 10.1097/NHH.0b013e318291fd56. [DOI] [PubMed] [Google Scholar]
- 27.Karlsson MR, Edner M, Henriksson P, Mejhert M, Persson H, Grut M. A nurse-based management program in heart failure patients affects females and persons with cognitive dysfunction most. Patient Educ Couns. 2005;58(2):146–153. doi: 10.1016/j.pec.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 28.Kimmelstiel C, Levine D, Perry K, Patel AR, Sadaniantz A, Gorham N. Randomized, controlled evaluation of short- and long-term benefits of heart failure disease management within a diverse provider network the SPAN-CHF trial. Circulation. 2004;110(11):1450–1455. doi: 10.1161/01.CIR.0000141562.22216.00. [DOI] [PubMed] [Google Scholar]
- 29.Koelling TM, Johnson ML, Cody RJ, Aaronson KD. Discharge education improves clinical outcomes in patients with chronic heart failure. Circulation. 2005;111(2):179–185. doi: 10.1161/01.CIR.0000151811.53450.B8. [DOI] [PubMed] [Google Scholar]
- 30.Kommuri NV, Johnson ML, Koelling TM. Relationship between improvements in heart failure patient disease specific knowledge and clinical events as part of a randomized controlled trial. Patient Educ Couns. 2012;86(2):233–238. doi: 10.1016/j.pec.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 31.Lee KS, Lennie TA, Warden S, Jacobs-Lawson JM, Moser DK. A comprehensive symptom diary intervention to improve outcomes in patients with HF a pilot study. J Card Fail. 2013;19(9):647–654. doi: 10.1016/j.cardfail.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 32.Leventhal ME, Denhaerynck K, Brunner-La Rocca HP, Burnand B, Conca-Zeller A, Bernasconi AT. Swiss Interdisciplinary Management Programme for Heart Failure (SWIM-HF) a randomised controlled trial study of an outpatient inter-professional management programme for heart failure patients in Switzerland. Swiss Med Wkly. 2011;141:w13171–w13171. doi: 10.4414/smw.2011.13171. [DOI] [PubMed] [Google Scholar]
- 33.Lupon J, Gonzalez B, Mas D, Urrutia A, Arenas M, Domingo M. Patients' self-care improvement with nurse education intervention in Spain assessed by the European Heart Failure Self-Care Behaviour Scale. Eur J Cardiovasc Nurs. 2008;7(1):16–20. doi: 10.1016/j.ejcnurse.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 34.Mårtensson J, Strömberg A, Dahlström U, Karlsson JE, Fridlund B. Patients with heart failure in primary health care effects of a nurse-led intervention on health-related quality of life and depression. Eur J Heart Fail. 2005;7(3):393–403. doi: 10.1016/j.ejheart.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 35.Mussi CM, Ruschel K, de Souza EN, Lopes AN, Trojahn MM, Paraboni CC. Home visit improves knowledge, self-care and adhesion in heart failure: Randomized Clinical Trial HELEN-I. Rev. Latino-Am. Enfermagem. 2013;21(Spec No):20–28. doi: 10.1590/s0104-11692013000700004. [DOI] [PubMed] [Google Scholar]
- 36.Otsu H, Moriyama M. Effectiveness of an educational self-management program for outpatients with chronic heart failure. Jpn J Nurs Sci. 2011;8(2):140–152. doi: 10.1111/j.1742-7924.2010.00166.x. [DOI] [PubMed] [Google Scholar]
- 37.Paradis V, Cossette S, Frasure-Smith N, Heppell S, Guertin MC. The efficacy of a motivational nursing intervention based on the stages of change on selfcare in heart failure patients. J Cardiovasc Nurs. 2010;25(2):130–141. doi: 10.1097/JCN.0b013e3181c52497. [DOI] [PubMed] [Google Scholar]
- 38.Riegel B, Dickson VV, Hoke L, McMahon JP, Reis BF, Sayers S. A motivational counseling approach to improving heart failure self-care mechanisms of effectiveness. J Cardiovasc Nurs. 2006;21(3):23241–23241. doi: 10.1097/00005082-200605000-00012. [DOI] [PubMed] [Google Scholar]
- 39.Rodríguez-Gázquez MeL.Arredondo-Holguín E.Herrera-Cortés R Effectiveness of an educational program in nursing in the self-care of patients with heart failure randomized controlled trial. Rev. LatinoAm. Enfermagem. 2012;20(2):296–306. doi: 10.1590/s0104-11692012000200012. [DOI] [PubMed] [Google Scholar]
- 40.Rojas CM, Rojas DN, Reyes ÁM. La entrevista motivacional como intervención de enfermería para promover el autocuidado en pacientes con insuficiencia cardiaca en una institución de cuarto nivel en Bogotá, Colombia. Investig Enferm Imagen Desarr. 2013;15(1):31–49. [Google Scholar]
- 41.Sebern MD, Woda A. Shared care dyadic intervention outcome patterns for heart failure care partners. West J Nurs Res. 2012;34(3):289–316. doi: 10.1177/0193945911399088. [DOI] [PubMed] [Google Scholar]
- 42.Shao JH, Chang AM, Edwards H, Shyu YI, Chen SH. A randomized controlled trial of self-management programme improves health-related outcomes of older people with heart failure. J Adv Nurs. 2013;69(11):2458–2469. doi: 10.1111/jan.12121. [DOI] [PubMed] [Google Scholar]
- 43.Shearer NB, Cisar N, Greenberg EA. A telephone-delivered empowerment intervention with patients diagnosed with heart failure. Heart Lung. 2007;36(3):159–169. doi: 10.1016/j.hrtlng.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 44.Shively MJ, Gardetto NJ, Kodiath MF, Kelly A, Smith TL, Stepnowsky C. Effect of patient activation on self-management in patients with heart failure. J Cardiovasc Nurs. 2013;28(1):20–34. doi: 10.1097/JCN.0b013e318239f9f9. [DOI] [PubMed] [Google Scholar]
- 45.Sisk JE, Hebert PL, Horowitz CR, McLaughlin MA, Wang JJ, Chassin MR. Effects of nurse management on the quality of heart failure care in minority communities a randomized trial. Ann Intern Med. 2006;145(4):273–283. doi: 10.7326/0003-4819-145-4-200608150-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smeulders ES, van Haastregt JC, Ambergen T, Janssen-Boyne JJ, van Eijk JT, Kempen GI. The impact of a self-management group programme on health behaviour and healthcare utilization among congestive heart failure patients. Eur J Heart Fail. 2009;11(6):609–616. doi: 10.1093/eurjhf/hfp047. [DOI] [PubMed] [Google Scholar]
- 47.Smith CE, Koehler J, Moore JM, Blanchard E, Ellerbeck E. Testing videotape education for heart failure. Clin Nurs Res. 2005;14(2):191–205. doi: 10.1177/1054773804273276. [DOI] [PubMed] [Google Scholar]
- 48.Strömberg A, Dahlström U, Fridlund B. Computerbased education for patients with chronic heart failure A randomised, controlled, multicentre trial of the effects on knowledge, compliance and quality of life. Patient Educ Couns. 2006;64(1-3):128–135. doi: 10.1016/j.pec.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 49.Strömberg A, Mårtensson J, Fridlund B, Levin LA, Karlsson JE, Dahlström U. Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failure results from a prospective, randomised trial. Eur Heart J. 2003;24(11):1014–1023. doi: 10.1016/s0195-668x(03)00112-x. [DOI] [PubMed] [Google Scholar]
- 50.Tung HH, Lin CY, Chen KY, Chang CJ, Lin YP, Chou CH. Self-management intervention to improve self-care and quality of life in heart failure patients. Congest Heart Fail. 2013;19(4):E9–E16. doi: 10.1111/chf.12014. [DOI] [PubMed] [Google Scholar]
- 51.Wang SP, Lin LC, Lee CM, Wu SC. Effectiveness of a self-care program in improving symptom distress and quality of life in congestive heart failure patients a preliminary study. J Nurs Res. 2011;19(4):257–266. doi: 10.1097/JNR.0b013e318237f08d. [DOI] [PubMed] [Google Scholar]
- 52.Michie S. Changing behavior theoretical development needs protocol adherence. Health Psychology. 2005;24(4):439–439. doi: 10.1037/0278-6133.24.4.439. [DOI] [PubMed] [Google Scholar]
- 53.Leventhal H, Friedman MA. Does establishing fidelity of treatment help in understanding treatment efficacy Comment on Bellg et al. (2004) Health Psychol. 2004;23(5):452–456. doi: 10.1037/0278-6133.23.5.452. [DOI] [PubMed] [Google Scholar]
- 54.Michie S, Abraham C. Interventions to change health behaviours evidence-based or evidenceinspired? Psychol Health. 2004;19(1):29–49. [Google Scholar]
- 55.Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321(7262):694–696. doi: 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fitzsimons D, Strachan PH. Overcoming the challenges of conducting research with people who have advanced heart failure and palliative care needs. Eur J Cardiovasc Nurs. 2012;11(2):248–254. doi: 10.1016/j.ejcnurse.2010.12.002. [DOI] [PubMed] [Google Scholar]